Abstract
For most adults, sleep is a dyadic behavior. Only recently have studies explored the dynamic association between sleep and relationship functioning among bedpartners. The current study is the first to examine bidirectional associations between changes in insomnia and changes in marital quality over time, in the context of a marital therapy trial. Among husbands, improvements in marital satisfaction were associated with a 36% decreased risk of insomnia at follow-up. Regarding the reverse direction, counter-intuitively, wife baseline insomnia was associated with improvements in husbands’ marital satisfaction, but only among the non-treatment seeking comparison group. Results are discussed in terms of implications for sleep and marital therapy, and suggest that improving sleep may be an added benefit of improving the marital relationship.
Introduction
Sleep is a critically important health behavior, reliably and prospectively associated with diverse indicators of health outcomes including general well-being, risk for psychiatric disorders, and risk for chronic health conditions, including cardiovascular diseases (Knutson, 2010; Troxel et al., 2010). A similarly robust body of research has found prospective associations between the quality of close relationships—in particular, marital or intimate partner relationships—and a host of mental and physical health outcomes (Gallo et al., 2003; Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002; Robles, 2014). Among health behaviors, sleep is uniquely associated with couple functioning because it typically occurs within a shared couple context. Indeed, emerging research has begun to highlight the interdependent nature of couple sleep (Gunn, Buysse, Hasler, Begley, & Troxel, 2015; Meadows, Arber, Venn, Hislop, & Stanley, 2009). However, sleep science has traditionally assessed sleep at the level of the individual, largely neglecting the influence of the partner and the quality of the bedpartners’ relationship (Troxel, Robles, Hall, & Buysse, 2007). In the present study, we seek to explore sleep in a dyadic context by exploring the association between sleep and relationship quality using a longitudinal approach that allows for an examination of whether sleep predicts marital quality, whether marital quality predicts sleep, or whether these relationships are bidirectional.
Until recently, there has been scant research on the impact of close relationships on sleep. However, there are likely to be dynamic and bidirectional associations between sleep and relationship quality, via psychological, behavioral, and physiological pathways (Troxel et al., 2007). For instance, given known effects of sleep disruption on mood, frustration tolerance, and cognitive functioning (Robles, Slatcher, Trombello, & McGinn, 2014), a poor night of sleep can lead to greater marital strife the next day. The reverse direction is also plausible—feelings of safety and security which are largely derived from close interpersonal connections (Feeney & Kirkpatrick, 1996), are considered critical for optimizing restorative and high quality sleep by facilitating down-regulation of physiological and emotional arousal. In contrast, insecurity in close relationships are purported to increase sleep disturbance by increasing vigilance and anxiety, and upregulating arousal (Dahl, 1996). Such feelings of safety and security (or its absence) are likely to be particularly important for optimizing sleep quality in the context of couple relationships. In fact, several studies have shown that insecurity in close relationships (i.e., attachment anxiety)is an independent correlate of poor subjective sleep quality and decreased sleep depth (as measured by polysomnography) in both women and men (Carmichael & Reis, 2005; Hicks & Diamond, 2011; Scharfe & Eldredge, 2001; Sloan, Maunder, Hunter, & Moldofsky, 2007; Troxel et al., 2007; Verdecias, Jean-Louis, Zizi, Casimir, & Browne, 2009). However, most of the extant research on relationship quality and sleep has utilized cross-sectional designs and has not considered the potential for bidirectional associations that unfold over time.
Among the handful of studies that have employed longitudinal designs, the findings support the contention that sleep and relationship quality are bidirectional (Gordon & Chen, 2013; Hasler & Troxel, 2010; Kane, Slatcher, Reynolds, Repetti, & Robles, 2014; Rauer, Kelly, Buckhalt, & El-Sheikh, 2010); however, the direction of effects may be gender-dependent. For instance, in a 10-day daily experience study of heterosexual cohabitating couples, Hasler and Troxel (2010) found that higher levels of female relationship satisfaction during the day predicted better sleep for both herself and her partner that night. However, for males, better sleep at night predicted higher male (but not female) relationship satisfaction the next day. Similarly, Kane and colleagues (2014) found that greater self-disclosure predicted better sleep for wives, but not for husbands. Finally, in a large community sample of 241 couples, Rauer and colleagues (2010) investigated the longitudinal association between psychological abuse and subjective sleep quality over a 3-year follow-up period. The findings showed that for both men and women, higher initial levels of psychological abuse and increases in psychological abuse over time predicted greater sleep problems at the 3-year follow-up. However, the analyses were stratified by sex rather than being examined dyadically, which precludes an examination of whether cross-partner effects were present, as observed in the Hasler and Troxel (2010) study.
Collectively, these findings provide support for the contention that relationship quality and sleep quality are reciprocally linked, with some evidence that associations may be gender-dependent. However, there is still a scarcity of data on how these processes unfold over time. Moreover, the existing literature involves observational studies using healthy, convenience samples of couples, which may result in a restriction of range in marital quality. Observational designs may be less informative for understanding whether intervening on sleep or relationship quality has an impact on the other behavior. A handful of studies have shown that treating a sleep disorder (i.e., obstructive sleep apnea) is associated with improvements in bedpartner sleep and the couples’ relationship functioning (as reviewed in Troxel et al., 2007). To our knowledge, however, no prior research has examined the impact of a relationship intervention on sleep in couples.
The current study builds on the scant existing research by being the first to study the bidirectional associations between sleep and relationship as they unfold over time in a sample of distressed couples assigned to a marital therapy intervention and a comparison sample of non-distressed couples who did not receive the marital intervention. By utilizing an intervention design that included both distressed and non-distressed couples, our study may provide a more robust test of the interface between relationship functioning and sleep. By increasing variability in both constructs and by intervening on one of the key study constructs, we will not only examine these constructs without the restriction of range that limits previous research, but we may also observe whether improvements in relationship quality can also improve sleep. Recognizing the interdependence of sleep and relationship functioning within couples, we utilized actor-partner interdependence models to examine how relationship quality affects one’s own sleep and one’s partner’s sleep over time. We also examined how earlier actor and partner sleep influences changes in relationship quality over time. Specifically, we examined whether changes in marital satisfaction over a 3-month follow-up period are associated with initial (i.e., baseline) insomnia while statistically adjusting for other factors which are known to covary with insomnia and/or relationship functioning, including participant age, number of children1 in the home, depressive symptoms, and body mass index (BMI). Finally, based on Hasler and Troxel’s findings which showed gender-dependent effects in the magnitude of the direction of effects, and consistent with the broader literature suggesting that women may be more sensitive physiologically, behaviorally, and emotionally, to relational cues than are men (Kiecolt-Glaser et al., 2002), we hypothesized that there would be stronger associations from relationship quality leading to insomnia over time for women, whereas for men, the reverse direction would evidence stronger associations.
Methods
Participants
The sample consisted of 216 participants—108 married couples—taking part in a larger marital intervention study (see Table 1). Participants were generally physically healthy based on specific exclusionary criteria. For example, exclusionary criteria included: chronic disease with a cardiovascular component, currently taking medications that influence blood pressure (as the parent study focused on cardiovascular outcomes), pregnant, or may become pregnant within the timeframe of our study (i.e., not preventing pregnancy). To ensure that we included distressed couples, we recruited from a community mental health clinic among those seeking marital therapy. Thus, among the total sample of 216, 60 couples were actively seeking therapy. We used a multi-method approach (e.g., newspaper advertisements, flyers, internet, referral, etc.) to recruit a comparison group of well-adjusted couples from the community, who were not seeking marital therapy. All couples were screened to assess actual level of marital distress (see details below). Those seeking marital therapy were offered marital therapy at no cost and all couples received monetary compensation for completing the procedures of the study. Only those who were seeking marital therapy were assigned to the treatment arm of our study. Thus, our study is not a randomized clinical trial, but rather a comparison of treatment-seeking versus non-treatment seeking couples. This project received IRB approval by the Human Subjects committee at Brigham Young University.
Table 1.
Sample Characteristics
| Tx Seeking (N = 119) | No-Tx Controls (N = 96) | |
|---|---|---|
|
|
||
| Relationship Duration In Years | 6.1 (6.6) | 4.5 (8.9) |
| Number of children | 1.84 (2.23) | .81 (1.68) |
| T1 DAS | 96.9 (19.0) | 118.9 (13.9) |
| T2 DAS | 107.8 (15.4) | 119.2 (14.0) |
| Percent reporting Insomnia at T1 | 48% | 44% |
| Percent reporting Insomnia at T2 | 35% | 29% |
| Age | 30.5 (8.7) | 26.9 (9.4) |
| Race | 80% White (Caucasian) | 87% White (Caucasian) |
| 8% Hispanic | 5% Hispanic | |
| 1% African American | 2% African American | |
| 2% Asian | 0% Asian | |
| 1% Native American | 1% Native American | |
| 8% Other | 5% Other | |
| Median Income | 16% < $10k | 21% <$10k |
| 31% 10–25k | 46% 10–25k | |
| 18% 25–40k | 11% 25–40k | |
| 9% 40–55k | 8% 40–55k | |
| 8% 55–70k | 3% 55–70k | |
| 6% 70–85k | 4% 70–85k | |
| 6% 85–99k | 3% 85–99k | |
| 6% 100k+ | 4% 100k+ | |
Procedure
Couples were first pre-screened over the phone to ensure they met the inclusion criteria. In addition to the criteria listed above, participants were also excluded if they were already receiving marital therapy, and if addiction and/or physical abuse were comorbid issues. If criteria were met, and after informed consent was obtained, participants completed a series of questionnaires that assessed general demographics variables (i.e. age, ethnicity, income, years married, number of children in the home), physical health (i.e. health history, sleep), mental health (i.e. depressive symptoms, general stress), and psychosocial measures (i.e. marital adjustment, social support). Participants completed the psychosocial and lifestyle assessments using a computerized survey tool (i.e., Qualtrics). Participants were also weighed and measured to assess body mass index (BMI) and waist circumference. The identical procedures were repeated 12-weeks later, with the exception of BMI assessment which was assessed at baseline only.
Distressed couples seeking therapy received either the therapists preferred method of couple’s therapy (un-standardized method; n = 35) or emotion focused therapy (EFT, n = 25) during the 12-week period. EFT is a short term, structured approach to couples therapy with demonstrated efficacy, which focuses on restructuring key emotional responses (Denton, Burleson, Clark, Rodriguez, & Hobbs, 2000). We found no evidence that clustering within treatment type explained significant variance in outcomes, thus data from these groups were combined in analyses. The well-adjusted comparison group of couples received no treatment.
Measures
Distress Screening
The Revised Dyadic Adjustment Scale (RDAS; Busby, Christensen, Crane, & Larson, 1995) was used to assess level of marital quality at screening. The RDAS is an abbreviated 14-item version of the Dyadic Adjustment Scale that can reliably distinguish between distressed and non-distressed samples (Busby et al., 1995). The RDAS has demonstrated excellent test-retest reliability. For the Total RDAS Cronbach’s Alpha was.90, Guttman Split-Half = .94 and Spearman-Brown Split-Half reliability = .95. Based on prior research, scores on the RDAS < 48 (±5) are considered the clinical cutoff for distressed marital satisfaction (Anderson et al., 2014). Given that the RDAS has a 5 point margin of error, only cases where both members of the couple scored above 53 were excluded from the therapy group. As expected from recruitment, the non-treatment seeking couples recruited from the community were indeed more well-adjusted and less distressed (M=52.9; SD=4.8) relative to those recruited from clinic intake (M=43.54; SD=7.6).
Marital Quality
In our analysis, the full 32-item version of the Dyadic Adjustment Scale (DAS; Spanier, 1976) was used to assess marital relationship quality using 4 sub-scales (dyadic satisfaction, cohesion, consensus, and affection expression) as well as total score. The DAS is a psychometrically sound instrument (Graham, Liu, & Jeziorski, 2006; Spanier, 1976) that is perhaps the most widely used measure adjustment in couples in both clinical and research settings, and has been used widely in the marriage and health literature (Robles, 2014; Robles et al., 2014). The average score on the DAS for control couples was 118.91 (SD = 13.93), the average score for intervention couples was 96.87 (SD = 19.01), where higher scores indicate better relationship quality (d = 1.30, 95% CI [1.00, 1.60]). At T2, couples continued to be significantly different from one another (with those in the control group having higher DAS scores than those in the intervention group); however, the difference between groups was smaller than at baseline (d = .78, 95% CI [.45, 1.10]). To account for these differences, we controlled for whether participants were in the intervention group or not and used the reliable change index (RCI, described in more detail below) to examine changes in marital satisfaction as a predictor of insomnia.
Insomnia
Three items drawn from the Pittsburgh Sleep Quality Index (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989)were used to assess the presence or absence of insomnia: sleep quality (on a 4-point scale ranging from Very Good to Very Bad), sleep latency (minutes to fall asleep), and minutes of wakefulness after sleep onset (WASO). Given that each of the sleep measures were correlated and that isolated sleep symptoms are prevalent in the general population, for parsimony, we created a composite, binary insomnia measure using clinical cutpoints that have been used in insomnia research (Edinger et al., 2004; Lichstein, Durrence, Taylor, Bush, & Riedel, 2003). Specifically, participants were coded as 1 if they endorsed that their sleep quality was Very Bad or Fairly Bad or if their sleep latency or WASO was greater than 30 minutes; those who did not endorse any of the sleep symptoms at or above these threshold levels were coded as 0. Using this criterion, 47 husbands and 53 wives reported insomnia at baseline and 24 husbands and 26 wives reported insomnia at follow up. Analyses (not shown) examining symptom counts (i.e., 0, 1,2, or 3 or more symptoms at or above the defined thresholds) revealed the same pattern of associations as with the binary measure. Therefore, we elected to present findings according to the binary outcome, as this is consistent with diagnostic criteria for insomnia.
Center for Epidemiological Studies Depression Scale (CES-D)
The CES-D includes 20 clinically derived items and has been shown to be a reliable and valid measure of depression (Radloff, 1977). In a nationwide survey of 2,500 participants, the scale’s reliability showed high consistency, with Cronbach’s alpha ranging from .75–.95 and in our sample, α = .87. We removed the sleep item from the CES-D scale to avoid redundancy with the sleep measure.
Results
Analytic Strategy
To analyze our data, we used the Actor-Partner Interdependence Model (APIM), a dyadic data analytic approach that not only accounts for the nestedness of couple data but also explicitly models the dynamic, interdependent processes that characterize couple relationships. Unlike composite scores or analyzing partners separately, the APIM allows one to model the dynamic, interdependent influence of partners on one another. For example, one can model the impact of changes in wife’s marital satisfaction on husband insomnia (a partner effect) while accounting for the longitudinal stability of the husband’s insomnia over time (an actor effect). We conducted our analysis in Stata 13.1 (StataCorp, 2013) using generalized structural equation modeling (GSEM) which allows for analysis of dependent variables that are not normally distributed. This flexibility was necessary because we had a binary outcome (i.e., insomnia present versus absent). We reported odds ratios (OR) when insomnia was the outcomefor ease of interpretation.
Our central research question was whether changes in marital satisfaction predicted insomnia at follow-up, after controlling for baseline insomnia and other covariates. To most directly answer this question, we included our treatment condition variable (0 = no-treatment group, 1 = treatment group) and the reliable change index (RCI) for marital satisfaction. In this case, the RCI is a pre-post change score that indicates how much people’s marital satisfaction changed during the course of study (Jacobson & Truax, 1991). Assignment to treatment group is a comparatively less sensitive measure of improvement, whereas the RCI offers a clearer measurement of how much participants’ relationship satisfaction changed over the course of the study, and thus more clearly answered the question of whether or not improvements in marital satisfaction predict changes in insomnia. We controlled for factors that are known to covary with both relationship functioning and insomnia, including baseline insomnia, body mass index, depressive symptoms (with the sleep item removed), age, and number of children in the home. Establishing a strong, unique relationship between variables and establishing the temporal ordering of an effect are key criteria in establishing causality (Hill, 1965). Observing a significant association between changes in marital quality when controlling for established covariates provides evidence of a strong, unique relationship between these variables, and the time lag between our two time points provides evidence for the direction of these effects (i.e. temporal ordering).
Descriptive Statistics
Descriptive statistics, including means, standard deviations and correlations within and between partners can be seen in Table 2 and our model can be seen in Figure 1. The average age of the sample was 28.86 (SD = 9.20). The ethnic breakdown of participants was as follows: 82% White (Caucasian), 7% Hispanic, 4.5% “Other”, 1.5% African American, 1.5% Native American, 1.5% “Mixed”, 1% Asian, and 1% did not disclose their ethnicity. On average, couples had been together 5.4 years (SD = 7.8). Those in the intervention group had higher RCI values than those in the no-treatment group, indicating greater changes in marital satisfaction during the 3-month follow-up period (dHusbands = .60, 95% CI [.15, 1.05]; dWives = .87, 95% CI [.40, 1.33]). Those in the intervention group were also older (dHusbands = .39, 95% CI [.01, .78]; dWives = .41, 95% CI [.03, .79]) and had more children (dCouple = .48, 95% CI [.09, .87]). Husbands in the intervention group, but not wives, reported more depressive symptoms (dHusbands = .46, 95% CI [.07, .84]). There were no differences between groups for BMI or baseline insomnia.
Table 2.
Descriptive Statistics
| Condition | T1 Age | # of Children | BMI | T2 CES-D | RCI | T1 Insomnia | T2 Insomnia | |
|---|---|---|---|---|---|---|---|---|
| Husband Mean (SD) | 0.56 (.50) | 29.8 (9.5) | 1.34 (2.03) | 25.45 (5.38) | 31.77 (5.15) | .58 (1.75) | .44 (.50) | .30 (.46) |
| Wife Mean (SD) | 0.56 (.50) | 27.9 (8.8) | 1.42 (2.11) | 24.82 (5.60) | 33.85 (4.91) | .70 (1.75) | .49 (.50) | .33 (.47) |
|
|
||||||||
| Condition | 1.00 | 0.13 | 0.15 | 0.05 | −0.07 | 0.40*** | 0.21 | 0.17 |
| T1 Age | 0.17 | 0.96*** | 0.75*** | 0.19 | 0.07 | 0.14 | 0.23* | 0.23* |
| # of Children | 0.24* | 0.58*** | 0.93*** | 0.12 | 0.02 | 0.28* | 0.27* | 0.20 |
| BMI | 0.01 | 0.04 | 0.05 | 0.42*** | 0.02 | 0.05 | 0.18 | 0.18 |
| T2 CES-D | −0.15 | −0.08 | −0.03 | −0.01 | −0.03 | −0.07 | 0.18 | 0.28* |
| RCI | 0.28* | 0.14 | 0.19 | −0.02 | −0.06 | 0.45*** | 0.19 | 0.18 |
| T1 Insomnia | −0.14 | −0.17 | −0.03 | 0.15 | 0.05 | 0.01 | −0.04 | 0.56*** |
| T2 Insomnia | −0.07 | −0.07 | −0.09 | 0.11 | −0.05 | −0.22 | 0.46*** | −0.02 |
Note. Wife correlations are above the diagonal, husband correlations are below the diagonal and intra-dyad correlations are bolded on the diagonal,
p<0.05,
p<0.01,
p<0.001
Figure 1.
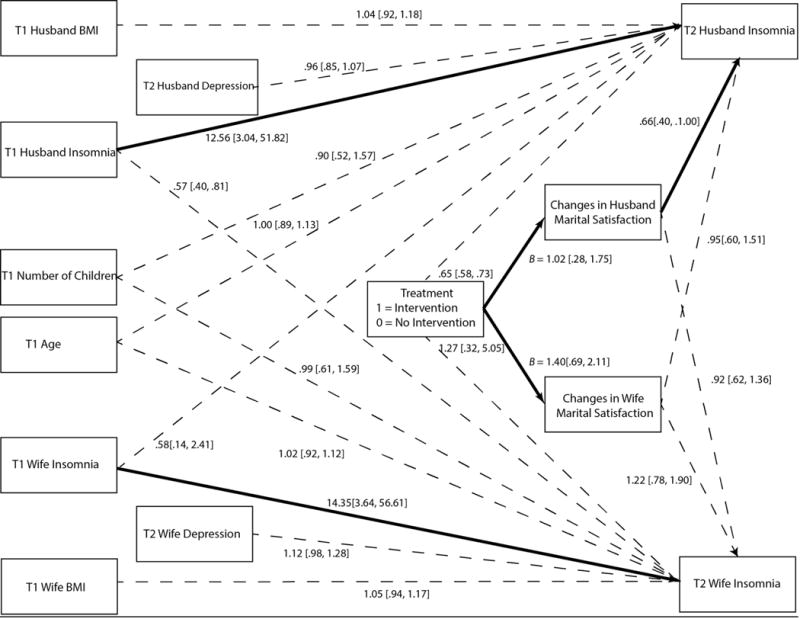
Actor-partner interdependence model with parameter estimates and 95% confidence intervals. All parameter estimates are expressed as odds ratios, with the exception of of paths from “Treatment” to “Changes in Husband/Wife Marital Satisfaction” which are expressed as unstandardized regression weights. Solid lines indicate a parameter estimate with a confidence interval that does not include B = 0 or OR = 1. Correlations between exogenous variables and disturbance terms for endogenous variables are not pictured for ease of interpretation but were included in the statistical model.
Do Changes in Marital Satisfaction Predict Changes in Insomnia?
As expected, husbands (B = 1.02, 95% CI [.28, 1.75]) and wives (B = 1.40, 95% CI [.69, 2.11]) who received treatment experienced more improvement in their marital satisfaction than those in the no-treatment group. Treatment seeking did not have a direct effect on either husband or wife insomnia. However, improvements in husband marital satisfaction over the 3-month follow-up period were associated with lower odds of husband insomnia (OR = .64, 95% CI [.40, 1.002]) at follow-up, even after controlling for both partners’ baseline insomnia and other covariates; indicating that for each standard deviation improvement in husband marital satisfaction, there was a 36% decrease in the odds of husband insomnia. For wives, improvements in their own marital satisfaction were not associated with wife insomnia at follow-up. A Wald test revealed that the difference in these parameter estimates was significantly larger for men than for women (χ2 (1) = 3.96, p < .05). We did not find evidence for partner effects (i.e., wife changes in marital satisfaction influencing husbands’ insomnia and vice versa).
To determine whether marital therapy influenced husband insomnia via the mechanism of improved relationship satisfaction, we examined this meditational path using the RMediation package (Tofighi & MacKinnon, 2011). Our results suggest that changes in marital satisfaction mediated the influence of marital therapy on husband insomnia (indirect effect = −.46, 95% CI [−1.16, 0.01]). Although the upper limit of the confidence interval just included zero, the vast majority of plausible estimates for the indirect effect fell below zero providing evidence that an effect is present.
Does Insomnia Predict Changes in Marital Satisfaction?
For our secondary research question, we examined whether insomnia at baseline predicted change in marital satisfaction over the 3-months of the study. To address this aim, we reversed the model showed in Figure 1, omitting T2 Insomnia and replacing it with T1 Insomnia and examining husband and wife RCIs as our dependent variables. We tested for group interactions (no-treatment vs. intervention) and report different values for each group only when they were significantly different from one another; otherwise we collapsed across groups. As expected, the intercepts were different across groups such that both husbands (χ2 (1) 8.53, p < .01) and wives (χ2 (1) 13.66, p < .01) in the intervention group experienced more change over the course of the study than those in the no-treatment group.
Insomnia had no significant impact on changes in ones’ own marital satisfaction for either husbands or wives (i.e., actor effects). However, we did find evidence for a partner effect, but only in the no-treatment comparison group; the influence of wife insomnia on changes in husband marital satisfaction was different between groups (χ2 (1) 6.30, p = .01). Specifically, in the no-treatment group, wife baseline insomnia predicted improvements in husband marital satisfaction (B = 1.14, 95% CI [.45, 1.84] whereas for those in the intervention group, there was not a significant association (B = −.75, 95% CI [−2.04, .55]). Regarding partner effects, there were no differences between groups nor did partner insomnia predict changes in marital satisfaction for either husbands or wives.
Discussion
These results add to an emerging literature that recognizes the dyadic nature of sleep for most adults. It is the first to study longitudinal sleep-marital functioning associations in a sample of treatment-seeking, maritally distressed couples and a non-treatment-seeking comparison group. Improvements in marital satisfaction were associated with lower risk of insomnia at the 3-month follow-up; however, contrary to our expectations and prior work, we found that this effect was only statistically significant for husbands—for each standard deviation increase in husband’s marital satisfaction, there was a 36% reduction in the risk of insomnia. Although these findings are in conflict with prior research and theory that suggest that women are more physiologically and emotionally responsive to marital distress than men, there is only limited data suggesting gender-dependent associations between marital distress and sleep. These findings highlight the importance of considering the impact of marital distress on both husbands’ and wives’ sleep.
Although the treatment group experienced greater improvement in marital satisfaction as compared to the no-treatment group, there was not a direct effect of treatment on insomnia symptoms at follow-up. However, our data suggest that marital therapy improved husband insomnia indirectly by improving marital quality. This effect was not isolated to those who received marital therapy; rather, improvement in husband marital satisfaction had a direct effect on insomnia irrespective of condition. Thus, these findings are intriguing in that they are the first to demonstrate that improving marital quality can have a measurable impact on insomnia. Importantly, the significant associations reported herein were independent of risk factors that are known to covary with both insomnia and marital distress, are consistent with the hypothesis that reducing marital distress may have an independent positive effect on sleep.
Regarding the reverse association where we examined whether insomnia predicted changes in marital satisfaction, we found only one significant effect; counter-intuitively, wife baseline insomnia predicted improvements in husband’s marital satisfaction, but only in the no-treatment group. Perhaps wives in non-distressed marriages who experience more sleep loss at night (either at onset or after onset) are engaging in conversation or sexual activity with their husbands, thus increasing husband marital satisfaction. More research is needed that examines not only sleep disturbance, but also related dyadic activities such as late night conflict, conversations, or sexual activity, as each of these could manifest as sleep disturbance on sleep measures such as those that we used, but that may reflect other relational processes. The lack of significant associations overall for the pathway from insomnia to changes in marital satisfaction is in contrast to the handful of other studies using observational designs (Gordon & Chen, 2013; Hasler & Troxel, 2010) which have shown that poor sleep predicts subsequent marital functioning. This inconsistency with the prior literature may be due to the context of the study (i.e., as part of a marital intervention trial) or may be due to differences in the nature and timing of the assessments of sleep and marital functioning. Specifically, whereas our study evaluated insomnia as a predictor of changes in marital satisfaction over a 3-month period, both the Gordon and Chen study (2013) and the Hasler and Troxel study (2010) examined more proximal associations between sleep and next day’s marital functioning. Further research is needed to determine whether the proximal associations between poor sleep and marital distress cumulatively contribute to changes in marital distress over more extended periods of time.
Strengths and Limitations
These findings must be interpreted within the study strengths and limitations. Notably, this was the first study to examine the role of sleep in the context of a marital intervention. As such, these findings extend the limited, extant literature on bidirectional associations between sleep and marital functioning, by examining these pathways in a sample of distressed couples seeking marital therapy and a control group of couples that were not seeking therapy, which may enhance the variability in key study constructs, as opposed to prior work which has focused on convenience, community-based samples. Nevertheless, our sample was relatively small and consisted primarily of young, Caucasian couples, some of whom were seeking therapy in a low-income community clinic, some of whom were not. Also, given that there was some overlap in the marital satisfaction scores, there is clearly some heterogeneity in level of marital distress in both the treatment-seeking group and the non-treatment seeking group, which may have attenuated group differences. Furthermore, by design, the study was not a randomized clinical trial. Another strength of the study was the use of a well-validated instrument for assessing marital distress (DAS) and use of actor-partner models to assess the dyadic and bidirectional associations between marital functioning and insomnia. However, the use of self-reports for both marital distress and insomnia may have introduced common method variance. Nevertheless, findings are supported by the fact that significant associations were observed even after controlling for depressive symptoms. It is also worth noting that we used specific items drawn from the PSQI to assess sleep, rather than the fully validated scale, which may limit the reliability and validity of the measure. On the other hand, as a measure of insomnia complaints, the measure used herein is consistent with frequency and symptom criteria used for the diagnosis of insomnia, with the exception that it does not assess daytime dysfunction (Edinger et al., 2004). Related to sleep assessment, given that the original intent of the study was not focused on examining sleep in couples, we did not have measures of diagnosed or undiagnosed sleep disorders, and did not directly assess whether or not participants were actually sleeping with their spouse on a regular basis. However, given that couples in this sample were relatively young and healthy, we would not expect a high prevalence of sleep disorders, such as obstructive sleep apnea (OSA), and we controlled for baseline BMI which is a key risk factor for OSA.
Summary
This study highlights the important but understudied interface between changes in marital functioning in the context of marital therapy and insomnia. Given that sleep is a dyadic behavior for most adults and is critically important for health and well-being, it is surprising that very little marital research has focused on the role of sleep in the context of marital interventions. By the same token, only recently have sleep researchers focused on the social nature of sleep (Rogojanski, Carney, & Monson, 2013; Troxel et al., 2007). To our knowledge, this is the first study to demonstrate that improvements in marital functioning are associated with improvements in sleep, although the findings were only significant among husbands. Clearly, these findings must be replicated with larger and more diverse samples, and using objective as well as subjective measures of sleep. Nevertheless, findings from this preliminary research add to the growing literature on the dyadic role of sleep, and suggest that improving sleep may be an added benefit of improving marital functioning within couples. Recognizing the dyadic nature of sleep is critical to inform the comprehensive assessment and treatment planning in the context of marital and sleep interventions.
Acknowledgments
This work was supported by a grant given to JHL from the Netherlands Institute for Advanced Study in the Humanities and Social Sciences (NIAS). JHL was supported by funding from the Family Studies Center at Brigham Young University, and the Mary Lou Fulton Young Scholar Award. WMT was supported by K23 HL093220 and HL112646.
Footnotes
The authors have no conflicts of interest to disclose.
Number of children and age were entered as couple level variables because of the correlations between partners approached 1 (see Table 2), which is problematic statistically. We elected to use wife report for both of these variables.
Having the upper limit of the 95% confidence interval include an odds ratio of 1.00 is analogous to having p = .05
References
- Anderson SR, Tambling RB, Huff SC, Heafner J, Johnson LN, Ketring SA. The development of a reliable change index and cutoff for the revised dyadic adjustment scale. Journal of Marital and Family Therapy. 2014;40(4):525–534. doi: 10.1111/jmft.12095. [DOI] [PubMed] [Google Scholar]
- Busby DM, Christensen C, Crane DR, Larson JH. A revision of the dyadic adjustment scale for use with distressed and nondistressed couples – construct hierarchy and multidimensional scales. Journal of Marital and Family Therapy. 1995;21(3):289–308. doi: 10.1111/j.1752-0606.1995.tb00163.x. [DOI] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carmichael CL, Reis HT. Attachment, sleep quality, and depressed affect. Health Psychology. 2005;24(5):526–531. doi: 10.1037/0278-6133.24.5.526. [DOI] [PubMed] [Google Scholar]
- Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development & Psychopathology. 1996;8:3–27. [Google Scholar]
- Denton WH, Burleson BR, Clark TE, Rodriguez CP, Hobbs BV. A randomized trial of emotion-focused therapy for couples in a training clinic. Journal of Marital and Family Therapy. 2000;26(1):65–78. doi: 10.1111/j.1752-0606.2000.tb00277.x. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Bonnet MH, Bootzin RR, Doghramji K, Dorsey CM, Espie CA, Stepanski E. Derivation of research diagnostic criteria for insomnia: Report of an American academy of sleep medicine work group. Sleep. 2004;27:1567–1596. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- Feeney BC, Kirkpatrick LA. Effects of adult attachment and presence of romantic partners on physiological responses to stress. Journal of Personality and Social Psychology. 1996;70(2):255–270. doi: 10.1037//0022-3514.70.2.255. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Troxel W, Kuller L, Sutton-Tyrrell K, Edmundowicz D, Matthews KA. Marital status, marital quality and subclinical atherosclerosis in postmenopausal women. Psychosomatic Medicine. 2003 doi: 10.1097/01.psy.0000097350.95305.fe. [DOI] [PubMed] [Google Scholar]
- Gordon AM, Chen S. The role of sleep in interpersonal conflict: Do sleepless nights mean worse fights? Social Psychological and Personality Science. 2013 doi: 10.1177/1948550613488952. [DOI] [Google Scholar]
- Graham JM, Liu YJ, Jeziorski JL. The dyadic adjustment scale: A reliability generalization meta-analysis. Journal of Marriage and the Family. 2006;68(3):701–717. doi: 10.1111/j.1741-3737.2006.00284.x. [DOI] [Google Scholar]
- Gunn HE, Buysse DJ, Hasler BP, Begley A, Troxel WM. Sleep concordance in couples is associated with relationship characteristics. Sleep. 2015 doi: 10.5665/sleep.4744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Troxel WM. Couples’ nighttime sleep efficiency and concordance: Evidence for bidirectional associations with daytime relationship functioning. Psychosomatic Medicine. 2010;72(8):794–801. doi: 10.1097/PSY.0b013e3181ecd08a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks AM, Diamond LM. Don’t go to bed angry: Attachment, conflict, and affective and physiological reactivity. Personal Relationships. 2011;18(2):266–284. doi: 10.1111/j.1475-6811.2011.01355.x. [DOI] [Google Scholar]
- Hill AB. The environment and disease: Association or causation? Proceedings of the Royal Society of Medicine. 1965;58(5):295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kane HS, Slatcher RB, Reynolds BM, Repetti RL, Robles TF. Daily self-disclosure and sleep in couples. Health Psychology. 2014;33(8):813–822. doi: 10.1037/hea0000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- Knutson KL. Sleep duration and cardiometabolic risk: A review of the epidemiologic evidence. Best Practice & Research Clinical Endocrinology & Metabolism. 2010;24(5):731–743. doi: 10.1016/j.beem.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichstein K, Durrence H, Taylor D, Bush A, Riedel B. Quantitative criteria for insomnia. Behaviour Research and Therapy. 2003;41(4):427–445. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- Meadows R, Arber S, Venn S, Hislop J, Stanley N. Exploring the interdependence of couples’ rest-wake cycles: An actigraphic study. Chronobiology International. 2009;26(1):80–92. doi: 10.1080/07420520802678452. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rauer AJ, Kelly RJ, Buckhalt JA, El-Sheikh M. Sleeping with one eye open: Marital abuse as an antecedent of poor sleep. Journal of Family Psychology. 2010;24(6):667–677. doi: 10.1037/a0021354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles TF. Marital quality and health: Implications for marriage in the 21 century. Current Directions in Psychological Science. 2014;23(6):427–432. doi: 10.1177/0963721414549043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: A meta-analytic review. Psychological Bulletin. 2014;140(1):140–187. doi: 10.1037/a0031859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogojanski J, Carney CE, Monson CM. Interpersonal factors in insomnia: A model for integrating bed partners into cognitive behavioral therapy for insomnia. Sleep Medicine Reviews. 2013;17(1):55–64. doi: 10.1016/j.smrv.2012.02.003. [DOI] [PubMed] [Google Scholar]
- Scharfe E, Eldredge D. Associations between attachment representations and health behaviors in late adolescence. Journal of Health Psychology. 2001;6(3):295–307. doi: 10.1177/135910530100600303. [DOI] [PubMed] [Google Scholar]
- Sloan E, Maunder R, Hunter J, Moldofsky H. Insecure attachment is associated with the alpha-EEG anomaly during sleep. BioPsychoSocial Medicine. 2007;1(1):20. doi: 10.1186/1751-0759-1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage & the Family. 1976:15–28. [Google Scholar]
- StataCorp. Stata statistical software (Version 13.1) College Station, TX: StataCorp LP; 2013. [Google Scholar]
- Tofighi D, MacKinnon DP. Rmediation: An r package for mediation analysis confidence intervals. Behavior Research Methods. 2011;43(3):692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Buysse DJ, Matthews KA, Kip KE, Strollo PJ, Hall M, Reis SE. Sleep symptoms predict the development of the metabolic syndrome. Sleep. 2010;33(12):1633–1640. doi: 10.1093/sleep/33.12.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews. 2007;11(5):389–404. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdecias RN, Jean-Louis G, Zizi F, Casimir GJ, Browne RC. Attachment styles and sleep measures in a community-based sample of older adults. Sleep Medicine Reviews. 2009;10(6):664–667. doi: 10.1016/j.sleep.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


