Abstract
Background of the Study
In India, although a number of contraceptive choices are available, the usage of contraceptive methods among postpartum women is rather low. The current study intended to determine the impact of “structured contraception counseling” on women’s decision making on selection of contraceptive methods and the reasons behind the selection of a contraceptive method.
Methods
One-hundred-and-seventeen postpartum women in the age group of 18–35 years, requesting contraception, were enrolled in the study. “Structured contraception counseling” was provided using a standardized protocol with balanced and comprehensive education material on the available hormonal and nonhormonal contraceptive methods. Questionnaires with information on the women’s pre- and post-counseling contraceptive choice, her perceptions, and the reasons behind her postcounseling decision were filled by the participating women.
Results
Maximum women enrolled for the study were in the age group of 21–25 years. In pre-counseling, 36 % postpartum women selected a contraceptive method, 23.1 % a nonhormonal method, and 12.8 % a hormonal method. After “structured contraception counseling,” 92.25 % of women chose a contraceptive method. There were significant differences between the women’s choices of contraceptive methods in the pre- and post-counseling sessions, respectively [progesterone-only pills (POP): 5.1 vs. 38.46 %, (p < 0.001); injectable-depot medroxy progesterone acetate (DMPA): 2.56 vs. 21.356 %, (p < 0.01); and intra uterine device (IUD): 10.28 vs. 23.92 %, (p < 0.001). 38.46 % chose a POP, 21.36 % injectable-DMPA, and 23.9 % the IUD].
Conclusion
“Structured contraception counseling” using standardized protocol resulted in significant improvements in the selection of contraceptive methods by postpartum women.
Keywords: Postpartum women, Contraception, Counseling, Progesterone-only pills
Introduction
The Indian family planning program, although successful in increasing contraceptive use among couples who have achieved their desired family size, has not been equally successful in educating postpartum women about the use of contraceptive methods for birth spacing [1–4]. An increase in contraceptive use during the postpartum period should substantially reduce rates of maternal and infant mortality by preventing unplanned and unwanted pregnancies, and judicious spacing between new pregnancies [5, 6].
Contraceptive use may be depressed immediately after childbirth and delayed postpartum because of the dependence of postpartum women on less-reliable contraceptive practices such as breast feeding, withdrawal, and fertility-based awareness techniques. Studies suggest that only about one quarter of women with a baby younger than 6 months old is protected by lactational amenorrhea method as they are not exclusively breast feeding [6]. Perhaps the most important concern is that contraceptive use is no more than 17 % among the women immediately and within 6 months postpartum, and around 33 % between 6 and 12 months after delivery [3–7]. Most women are at risk of unintended pregnancy in the postpartum and extended postpartum period [8, 9]. To address this issue, efforts should be directed to educate postpartum women regarding contraception and healthy pregnancy spacing [9]. One such approach worthy of adoption: ‘Counseling and sharing information’ on various available contraceptives can provide postpartum women with the information they need to make an informed decision about contraception [10–12].
This study primarily aimed to evaluate the role of structured contraceptive counseling on the decision-making process among postpartum women and the changes it brought about in their contraceptive choice and selection post counseling. Other objectives of the study were to determine the reasons behind the women’s selection of a particular contraceptive method, and the social and demographic variables (age, highest educational level, employment status, breast feeding, and number of children) among the postpartum women.
Materials and Methods
Necessary approval from the Institutional Ethics Committee was obtained before initiating the study.
Study Design
Cross-sectional, interventional study.
Study Site
The Department of Obstetrics and Gynecology, Pediatrics, MGM Medical College, Kalomboli, Navi Mumbai, and the Deparment of Pharmacology, MGM Medical College, Kamothe, Navi Mumbai.
Study Duration
May 2014–August 2014.
Sample Size
One hundred and seventeen Postpartum women within 8 weeks of delivery were counseled for the hormonal and nonhormonal methods of contraception.
The sample size with 80 % power was calculated based on the assumption that the survey will detect at least a 25 % increase in the proportion of women choosing a method {the more reliable contraceptive methods: progesterone-only pill (POP), injectable contraceptive, intrauterine system (IUS), intrauterine device (IUD)/condoms/lactation amenorrhea} after counseling compared to that before counseling. (Underlying assumption was that 25 % of women switch from less-reliable contraceptive methods {e.g., withdrawal, fertility-based awareness techniques, improper lactation amenorrhea method} or no-contraception choice to more-reliable contraceptive methods (e.g., POP, injectable contraceptive, IUD, IUS, condoms/proper lactation amenorrhea) after counseling. The Type I error probability associated with this test of this null hypothesis is 0.05. The uncorrected Chi squared statistic to evaluate this null hypothesis was used.
Study Population
Postpartum women within 8 weeks of delivery who conformed to the specified inclusion and exclusion criteria were enrolled for the study.
Inclusion Criteria
Postpartum women within 8 weeks of delivery
Women who agree to sign an informed consent form
Exclusion Criteria
Postpartum women choosing permanent method of contraception (sterilization)
Postpartum women more than 8 weeks post delivery
Counseling
Counseling was provided using a standardized protocol with balanced and comprehensive education material on the available contraceptive methods. Counseling card for Hormonal Contraceptive methods developed by Federation of Obstetric and Gynecological Societies of India (FOGSI) was used for the study [11]. Counseling card for nonhormonal methods was developed specifically for the study. In addition, a tray displaying the various hormonal and non-hormonal contraceptives methods was also used for counselling of the post partum women (Fig. 1).
Fig. 1.
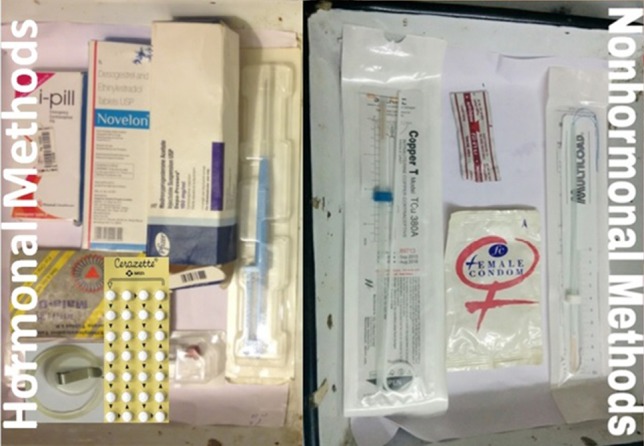
Tray demonstration the various hormonal and non-hormonal contraceptive methods used during counselling
Questionnaire
A questionnaire was prepared to record information on the women’s pre- and post-counseling contraceptive choice, and the reasons behind her post-counseling decision. The demographic variables (age, religion, community, highest educational level, employment status, breast feeding, and number of children) were also included in the questionnaire.
Study Procedure
The gynecologist and the medical student involved in the study underwent training regarding the counseling process and resources based on a counseling kit developed by FOGSI. All postpartum women within 8 weeks of delivery, during their post-natal checkup or while attending immunization clinic for vaccination of the infant, were enrolled in the study. The medical student under the supervision of the treating gynecologist provided comprehensive information and counseled the study subjects with regard to the advantages and disadvantages of various hormonal and nonhormonal methods of contraception.
After obtaining informed consent, the participating women were asked about contraceptive usage and their choice of contraceptive method prior to counseling. The social and demographic data of the participating women were recorded in the same questionnaire (Part A of the questionnaire). Subsequently, the postpartum women were counseled about the available contraceptives methods. In the same session, participating women’s choice of contraceptive method post-counseling and the criteria for choosing the specific contraceptive were documented and recorded in questionnaire (Part-B of the questionnaire).
Statistical Methods
The contraceptive methods opted by women pre- and post-counseling program was represented as a shift table and was analyzed using Mc Nemar’s Chi square test. Pre- and post-counseling, proportions of women opting for any one of contraceptive methods were recorded and compared.
Results
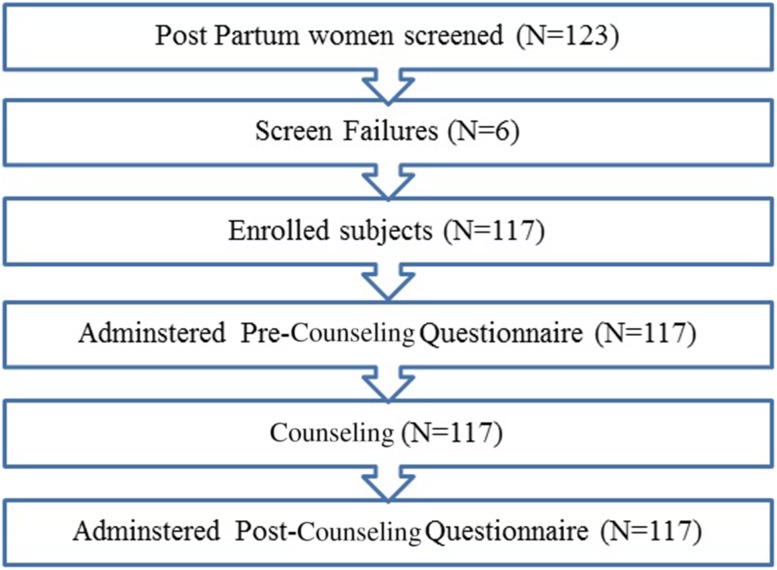
One-hundred-and-twenty-three (123) women were screened for the eligibility criteria of the study. Of these, six were excluded. Major reasons for exclusions were not meeting the study eligibility criteria and not filing the study questionnaire completely. This resulted in a total of 117 eligible women who were included in the final analysis and counselled using hormonal and non-hormonal contraceptive cards and trays (Figs. 1, 2).
Fig. 2.
Disposition summary of women
Demography
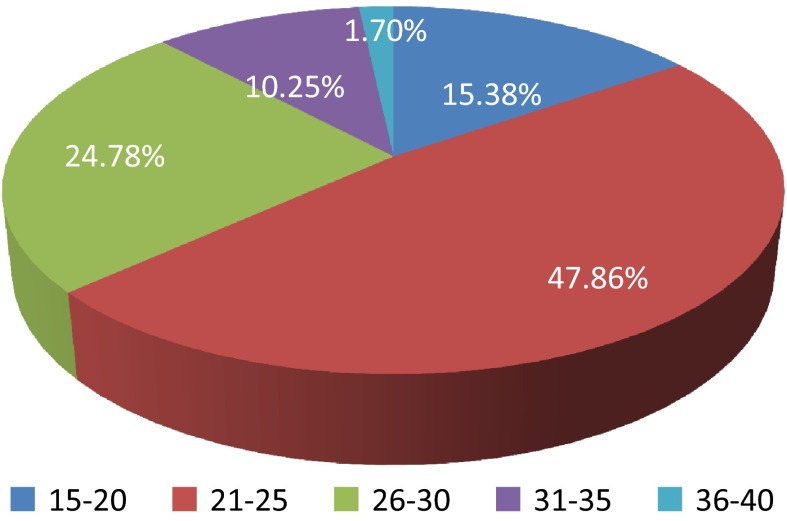
The age distribution of the postpartum women who were counseled is depicted in Fig. 3. Maximum (47.8 %) postpartum women were in the age group of 21–25 (Fig. 3). Demographic characteristics of these women are presented in Table 1. History of unplanned pregnancies was reported by 25.6 % (30) of the postpartum women. Women were counseled for a mean duration (SD) of 24 (8) min. Women’s ratings of the counseling and contraceptive information they received were largely positive. Majority of women rated the information received through counseling as “very” useful (89.2 %), “very” complete (81.1 %), and “very” fair and balanced (83.3 %).
Fig. 3.
Age distribution of postpartum women
Table 1.
Characteristics of participating women in the study (n = 117)
| S. no. | Characteristics (N = 117) | Number | Percentage |
|---|---|---|---|
| 1. | Education | ||
| Uneducated | 18 | 15.38 | |
| Less than 10th pass | 35 | 29.91 | |
| 10th pass | 30 | 25.64 | |
| 12th pass | 21 | 17.94 | |
| Graduate | 10 | 8.54 | |
| Post graduate | 2 | 1.70 | |
| 2. | Employment | 9 | 7.69 |
| Unemployed | 108 | 92.30 | |
| 3. | State | ||
| Maharashtrian | 71 | 60.68 | |
| Non-Maharashtrian | 46 | 39.31 | |
| 3. | Religion | ||
| Hindu | 102 | 87.18 | |
| Muslim | 13 | 11.12 | |
| Christian | 2 | 1.70 | |
| 5. | Un planned pregnancy | 30 | 25.64 |
| 6. | No of children | ||
| Nil | 3 | 2.56 | |
| One | 65 | 55.56 | |
| Two | 34 | 29.05 | |
| Three and more | 15 | 12.82 | |
| 7. | Breast feeding | 108 | 92.30 |
| Exclusive breast feeding | 90 | 83 | |
| No breast feeding | 9 | 7.69 | |
Contraceptive Choices Among Participating Postpartum Women
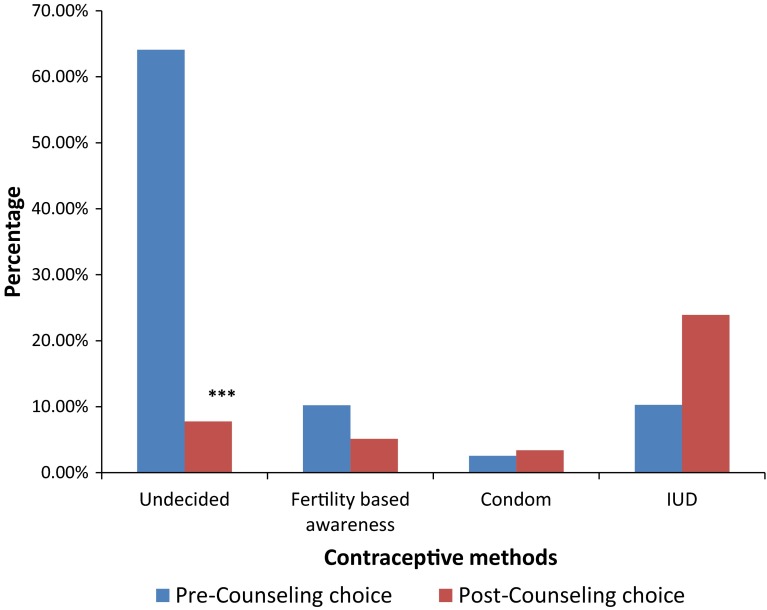
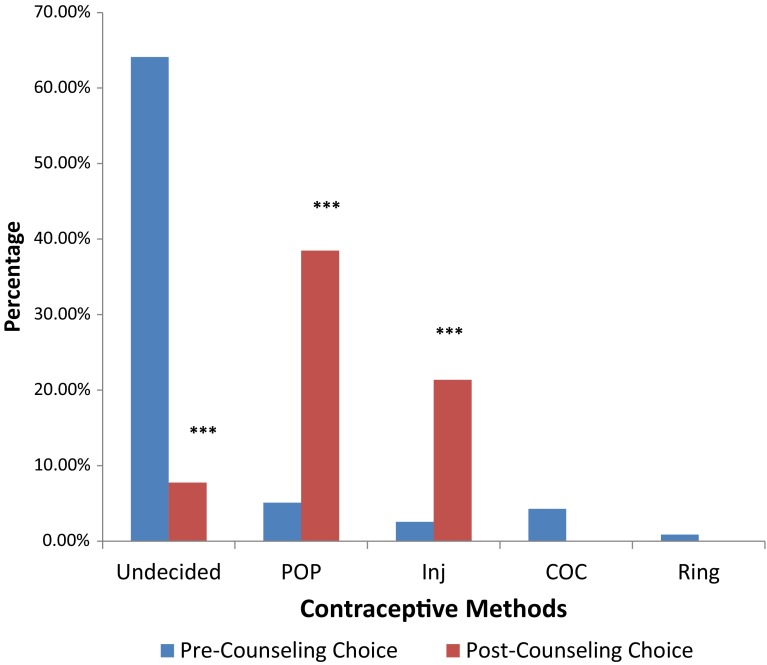
Pre-counseling, 12.8 % women selected a hormonal method, 23.1 % nonhormonal method, and 64.1 % were undecided for any contraceptive method. After “structured contraception counseling,” 59.85 % of women chose a hormonal contraceptive method and 31.5 % nonhormonal method. Contraceptive counseling provided to women resulted in statistically significant (***p value <0.0001, Mc Nemar’s test) differences between proportions of women opting each contraceptive method before and after the counseling (Fig. 4). Post-counseling, POPs were chosen by 38.46 %, vaginal ring by 0.85 %, injectable-DMPA by 21.36 %, IUD by 23.07 % women. In addition, Post-counseling, nonhormonal methods were selected by 31.5 % women (Natural methods 5.1 %, Condoms 3.4 5 and IUD by 23.07 %). Around, 7.75 % women remained indecisive about any method of contraception (Figs. 4, 5).
Fig. 4.
Women’s pre- and postcounseling contraceptive choice of the nonhormonal contraceptive methods. IUD intrauterine device. ***p > 0.001 Difference between pre- and post-counseling is statistically significant (p value >0.0001, Mc Nemar’s test)
Fig. 5.
Women’s pre- and postcounseling contraceptive choice of the hormonal contraceptive methods.COC combined oral contraceptive pill, Injectable-DMPA injectable-depot medroxyprogesterone acetate, POP progestogen-only pill. Difference between pre- and post-counseling is statistically significant (p value >0.0001, Mc Nemar’s test)
Maximum difference (33.3 %; p value <0.001) was noted in the proportion of women who chose POP after counseling compared to that before counseling. Differences in proportions of women who opted for injectable-DMPA and IUD post-counseling and pre-counseling were 18.7 and 12.7 %, respectively (Table 2). In the present study, counseling helped women arrive at a decision. After counseling, the highest decrease was observed in the proportion of women indecisive about method to be opted (difference in proportions = 56.35 %, p value <0.0001) (Figs. 4, 5).
Table 2.
Reasons for selection of contraceptive methods by postpartum women
| S. no. | Contraceptive method | Reasons for choice of the contraceptive method | Percentage |
|---|---|---|---|
| 1. | Injectable-DMPA | 3 monthly use | 86 |
| Convenience | 82 | ||
| Will not forget | 65 | ||
| 2. | IUD | Long acting | 91 |
| Will not forget | 76 | ||
| Convenience | 72 | ||
| 3. | POP | Breast feeding | 82 |
| Easy to use | 77 | ||
| My friends use it | 61 |
Injectable DMPA injectable-depot medroxyprogesterone acetate, IUD Intrauterine device, POP progestogen only pill
Reasons for Contraceptive Method Selection
Post-counseling perceptions of postpartum women about the hormonal contraceptive methods are shown in Table 2. The top three reasons cited for the selection of various contraceptive methods were injectable-DMPA-3: monthly use, convenience, and will not forget; IUD: long acting, will not forget, and convenience of use; and POP: breast feeding, my friends use it, and convenience. Across all the age groups, most frequent reason reported by women for nonselection of any contraceptive method was “discussion with partner” (Table 2).
Discussion
A large number of pregnancies in India are unintended and associated with inadequate birth spacing. The postpartum period is an important, yet underutilized, time to initiate contraception. Evidence shows that closely spaced pregnancies pose health risks to mothers and newborns. An analysis of data from the Demographic and Health Survey (DHS) for various years shows that babies born less than two years after the next oldest sibling were more than twice as likely to die in the first year compared with babies born after an interval of three years [13]. Also, women with short inter-pregnancy intervals (less than 6 months) were at higher risk of maternal death (OR = 2.54), third trimester bleeding (OR = 1.73), premature rupture of membranes (OR = 1.72), and anemia (OR = 1.30) [14].
Adequate spacing—24 months from delivery to the next pregnancy—could save the lives of mothers and newborns. Family planning could prevent up to one third of all maternal deaths by allowing women to delay motherhood, space births, avoid unintended pregnancies and unsafe abortions, and stop childbearing when they have reached their desired family after size [15]. National-level surveys show that the adoption of contraceptive methods for spacing has remained low in India, despite the fact that many women (50 %) desire at least a 3-year gap between two births. NFHS-3 data (2005–2006) show that among the married women aged 15–34 years, only 20 % were using any contraceptive method for spacing. Therefore, postpartum contraception is vital to the reduction of short interval pregnancies, which is a significant source of neonatal morbidity and medical care costs [16].
The variety of contraceptive methods available for postpartum women includes hormonal contraception (POP, Inj-DMPA), intrauterine device, lactational amenorrhea, barrier contraception, natural family planning, and sterilization. The present study was designed to explore the impact of a balanced and comprehensive structured counseling session on increasing contraceptive acceptability among postpartum women. Several studies have reported the need and utilization of contraceptives in India [5–8]. However, there is a lack of studies evaluating the impact of contraceptive counseling on the selection of contraceptive methods among postpartum women. A study conducted by Goel et al. [17] shows that women who received advice on family planning were more likely to adopt postpartum contraception (unadjusted OR = 1.63 p < 0.001) than those who were not advised at all. The present study was the first of its kind as it provides a complete perspective on contraceptive use among postpartum women on hormonal and nonhormonal methods in India. In the present study, overall, the hormonal contraceptive methods were found to be the preferred contraceptive method selected by postpartum women in India. This is in conformity with the results for India in the world contraceptive use pattern survey [17].
Contraceptive choices were found to be significantly influenced by the time-bound counseling sessions, as evident by the change in proportions of postpartum women choosing a particular method pre- versus post-counseling [18]. In the present study, structured contraception counseling of an average duration of 24 min about various available hormonal and nonhormonal contraceptive methods helped most women (92.8 %) to choose a contraceptive method. Although not conducted among postpartum women, similar observations regarding contraceptive counseling selection were reported in studies conducted in different countries. The effect of counseling on the selection of combined hormonal contraceptive methods in 11 countries was reported by others [19].
The poor usage of contraceptives as observed in the present study may be linked to the low education status of the postpartum women. Only 9.5 % of the postpartum women surveyed were graduates. This may partly explain the poor accessibility and information among these women regarding the various available contraceptive methods. Therefore, through counseling, the knowledge imparted to these postpartum women, regarding the advantages as well as disadvantages of each contraceptive method helped them make well-informed contraceptive choices catering to their specifications and requirements. The results of the present study emphasize the importance of communication (counseling) interventions in educating the postpartum women. The results are in conformity with the study conducted by Goel et al. [17]. Those authors concluded that the women’s background characteristics such as educational attainment (secondary or higher education; OR = 1.29, p < 0.05) and high standard of living (OR = 1.63, p < 0.001) facilitate the adoption of the desired practice [17]. Another study result that needs to be highlighted is that one fourth of the postpartum women enrolled, reported unplanned pregnancies. This is a matter of concern and needs to be addressed adequately. Communication Intervention as evaluated in the present study has the potential to educate the postpartum women and reduce the burden of unplanned pregnancies, abortions, maternal and infant morbidities, and mortalities.
In contrast to counseling provided on hormonal methods reported in the European CHOICE study, and recently in India, the present study included counseling on hormonal as well as nonhormonal methods among postpartum women [19]. In the present study, counseling provided to women resulted in statistically significant differences between contraceptive methods marked by women in pre- and post-counseling questionnaires. Among hormonal contraceptive methods, maximum difference in proportions was observed for women who chose the POP after counseling compared to pre-counseling. This was probably the most chosen method awareness of which was also low during the pre-counseling session.
After counseling, a significant switch after counseling was observed from nonhormonal methods to hormonal methods of contraception. Counseling helped a majority of the women who were indecisive about any contraceptive method to make a choice. The number of the women who opted for hormonal methods was the highest in the selection of POPs followed by those who selected Injectable DMPA. This pattern for switching is consistent with previous findings of a comprehensive study conducted across five European countries, where changes in women’s pre-counseling and post-counseling choices were statistically significant after counseling sessions [19–21]. However, this is the first-ever report of such choices being made by postpartum women pre- and post-counseling.
Availability of a variety of contraceptive methods is important if individual needs are to be met, and to choose a method that optimally fits with their life stages and requirements [22]. In conformity with many studies, there were varied reasons reported by women for selecting a contraceptive method. The most common reasons reported by postpartum women for selecting contraceptive methods were “breast feeding” for POP, “long action” for IUD, and “3-monthly use” for injectable-DMPA [22].
This study highlights the importance of utilizing the postpartum period to initiate contraceptive use among reproductive aged women, in order to decrease the risk of unintended pregnancy. Ideally, counseling should begin early in the antenatal period and include provider-initiated discussions. With a little time and effort on the part of the physician, the patients can be guided to decide on an effective and appropriate method of contraception.
The Indian National Family Health Survey data show that the chances of infant and maternal survivals would be 2.5 times as high with birth intervals of 3–5 years as with intervals of fewer years. In this context, the postpartum period is particularly significant as in India, a large proportion of women with an unmet need for contraception are within their first year after childbirth. Therefore, concerted efforts to educate postpartum women on available contraceptive methods could have a proportionally bigger impact on increasing postpartum contraception usage and reducing maternal and infant mortalities. The prevalence of postpartum contraceptive use, including the use of more effective methods, was highest when contraceptive counseling was provided during both prenatal and postpartum time periods [23]. Hence consideration should be given to counseling at both pre-natal and post-partum time so that there is greater acceptance of contraceptive methods among post-partum women. Recently, the role of task shifting (from physicians to health workers and para medicals) to expand the accessibility to family planning methods has been emphasized. Hence appropriate training and guidelines should be provided for dissemination of family planning methods and as well as optimization of the resources in health centers [24].
Although the study has significant findings, limitation of the study includes no follow-up visit to assess participant’s actual choice and compliance, and no direct involvement of male partners in counseling. The strengths of this study were the use of a unique standard structured counseling material (developed by FOGSI) as well as the in-house development of a nonhormonal counseling card and the inclusion of both hormonal and nonhormonal contraceptive methods in the educational material of counseling.
Conclusions
In conclusion, this study showed that POPs are the most frequently preferred contraceptive method among postpartum women followed by Inj-DMPA and then IUD. Using standardized protocol “Structured contraception counseling” resulted in a significant increase in selection of contraceptive methods by postpartum women.
Acknowledgments
This study is part of an Indian Council of Medical Research short-term studentship (ICMR STS -2014) Project. (Ref ID: 2014-00084).
Harpreet Kaur Chhabra
is a budding third-year UG-MBBS student at MGM Medical College, Navi Mumbai. She has attended two undergraduate conferences, MEDSICON 2K14 and ILLUMINATI 2K14, organized by VMMC Delhi and AFMC Pune, respectively. She has completed the following ICMR STS project successfully with due approval of the report by ICMR. Harpreet is looking forward to doing various research projects in her formative years of medical education and contributing toward patient care and welfare of the society. Besides her keen interest in exploring different aspects of academics and life, she enjoys writing occasionally and traveling.
Compliance with Ethical Standards
Conflict of interest
The authors declare that there is no Conflict of Interest in the present study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Harpreet Kaur Chhabra is a student at MGM Medical College; Dr. Ipseeta Ray Mohanty is a Professor of Pharmacology at Mahatma Gandhi Mission.
References
- 1.World Health Organization (WHO) Maternal mortality in 2005: estimates developed by WHO, UNICEF, UNFPA and the World Bank. Geneva: WHO; 2007. [Google Scholar]
- 2.Shah IH, Say L. Maternal mortality and maternity care from 1990 to 2005: uneven but important gains. Reprod Health Matter. 2007;15(30):17–27. doi: 10.1016/S0968-8080(07)30339-X. [DOI] [PubMed] [Google Scholar]
- 3.Vernon R. Meeting the family planning needs of postpartum women. Stud Fam Plan. 2009;40(3):235–245. doi: 10.1111/j.1728-4465.2009.00206.x. [DOI] [PubMed] [Google Scholar]
- 4.Kunwar S, Faridi MM, Singh S, et al. Pattern and determinants of breast feeding and contraceptive practices among mothers within six months postpartum. Biosci Trends. 2010;4(4):186–189. [PubMed] [Google Scholar]
- 5.Whitworth A, Stephenson R. Birth spacing, sibling rivalry and child mortality in India. Soc Sci Med. 2002;55(12):2107–2119. doi: 10.1016/S0277-9536(02)00002-3. [DOI] [PubMed] [Google Scholar]
- 6.Nath DC, Land KC, Singh KK. The role of breast-feeding beyond postpartum amenorrhoea on the return of fertility in India: a life table and hazards model analysis. J Biosoc Sci. 1994;26(2):191–206. doi: 10.1017/S0021932000021234. [DOI] [PubMed] [Google Scholar]
- 7.Sebastian MP, Khan ME, Kumari K, et al. Increasing postpartum contraception in rural India: evaluation of a community-based behavior change communication intervention. Int Perspect Sex Reprod Health. 2012;38(2):68–77. doi: 10.1363/3806812. [DOI] [PubMed] [Google Scholar]
- 8.Arora YL, Sharma GD. Family planning through post-partum communication in Dufferin Hospital, Lucknow. POPCEN News Lett. 1977;3(4):9–14. [PubMed] [Google Scholar]
- 9.Hingorani V. Methods of birth control. Choice is yours. Yojana. 1984;28(19):33–34. [PubMed] [Google Scholar]
- 10.Machado RB, Pompei LM, Giribela A, et al. Impact of standardized information provided by gynecologists on women’s choice of combined hormonal contraception. Gynecol Endocrinol. 2013;29(9):855–858. doi: 10.3109/09513590.2013.808325. [DOI] [PubMed] [Google Scholar]
- 11.Sheriar N, Joshi R, Mukherjee B, et al. Impact of counseling on selection of hormonal contraceptive among Indian women, vol. 57. In: 18th world congress on controversies in obstetrics, gynecology and infertility, Vienna, 2013; pp. 24–27.
- 12.International Institute for Population Sciences (IIPS) and Macro International, National Family Health Survey (NFHS-3), 2005–2006. India, vol. 1, Mumbai: IIPS, 2007.
- 13.Smith R, Ashford L, Gribble J, et al. Family planning saves lives. Washington, DC: Population Reference Bureau; 2009. [Google Scholar]
- 14.Conde-Agudelo A, Belizan JM. Maternal morbidity and mortality associated with inter-pregnancy interval: cross sectional study. Br Med J. 2000;321(7271):1255–1259. doi: 10.1136/bmj.321.7271.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collumbien M, Gerressu M, Cleland J. Non-use and use of ineffective methods of contraception. In: Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization, Chapter 2004; 15:1255–320.
- 16.Sheriar N, Joshi R, Mukherjee B, et al. Impact of structured counseling on the selection of hormonal contraceptive methods: results of a multi-centric, observational study in India. J Obstet Gynecol India. 2014;64(4):241–250. doi: 10.1007/s13224-014-0560-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goel S, Bhatnagar I, Khan ME, et al. Increasing postpartum contraception in rural Uttar Pradesh. J Fam Welf. 2010;56:57–64. [Google Scholar]
- 18.Cross2. United Nations, Department of Economic and Social Affairs, Population Division. 2011. World Contraceptive Use 2010 (POP/DB/CP/Rev2010). http://www.un.org/esa/population/publications/wcu2010/WCP_2010/Data.html. Accessed 2 June 2013.
- 19.Yeshaya A, Ber A, Seidman DS, Oddens BJ. Influence of structured counseling on women’s selection of hormonal contraception in Israel: results of the CHOICE study. Eur J Contracept Reprod Health Care. 2012;17:65–78. doi: 10.3109/13625187.2011.637586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomaszewski J, Paszkowski T, Dębski R, et al. CHOICE (Contraceptive Health Research of Informed Choice Experience) Ginekol Pol. 2012;83:417–423. [PubMed] [Google Scholar]
- 21.Baveja R, Buckshee K, Das K, et al. Evaluating contraceptive choice through the method-mix approach. An Indian Council of Medical Research (ICMR) task force study. Contraception. 2000;61:113–119. doi: 10.1016/S0010-7824(00)00089-5. [DOI] [PubMed] [Google Scholar]
- 22.Lete I, Doval JL, Perez-Campos E, et al. Factors affecting women’s selection of a combined hormonal contraceptive method: the TEAM-06 Spanish: sectional study. Contraception. 2007;76:77–83. doi: 10.1016/j.contraception.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 23.Zapata LB, Murtaza S, Whiteman MK, Jamieson DJ, Robbins CL, Marchbanks PA, D’Angelo DV, Curtis KM. Contraceptive counseling and postpartum contraceptive use. Am J Obstet Gynecol. 2015;212(2):171. [DOI] [PMC free article] [PubMed]
- 24.Polus S, Lewin S, Glenton C, Lerberg PM, Rehfuess E, Gülmezoglu AM. Optimizing the delivery of contraceptives in low- and middle-income countries through task shifting: a systematic review of effectiveness and safety. Reprod Health. 2015;12(1):27. [DOI] [PMC free article] [PubMed]