Introduction
Ovarian stromal tumor with minor sex cord elements is a rare entity among the unclassified sex cord stromal tumor first described in 1983 by Young and Scully as a predominantly fibromatous or thecomatous tumor with minor sex cord elements comprising less than 10 % of the tumor area [1]. Typically, ovarian stromal tumors are hormonally inactive but sometimes secrete estrogen stimulating the endometrium to proliferate. The additional sources of estrogen from sex cord elements further predispose these patients to endometrial carcinoma. To the best of our knowledge, only three cases of ovarian stromal tumor with minor sex cord elements coexisting with endometrial carcinoma have been reported in the literature [1–3]. However, none of these cases were of uniformly fibromatous type. We report a case of ovarian fibroma with minor sex cord elements in a 55-year-old postmenopausal female who presented with heaviness in the lower abdomen and bleeding per vagina. The patient also had focal well-differentiated endometrioid adenocarcinoma and complex atypical endometrial hyperplasia of the uterus indicating the hormone overproduction by the ovarian tumor. This is the first case report describing the ovarian fibroma with minor sex cord elements, showing evidence of estrogenic manifestation in the form of endometrioid adenocarcinoma.
Case Report
A 55-year-old female, gravida 4, para 4, sought consult for the assessment of heaviness in the lower abdomen and postmenopausal bleeding. She had attained menopause 5 years back and had no significant past or family history. On examination, a 12 × 10 cm firm mass was palpable in the hypogastrium extending to right iliac, lumbar, and umbilical regions. Vaginal examination revealed a uniformly enlarged uterus of 10–12 weeks and a right adnexal mass. Ultrasound abdomen showed a right adnexal mass and a bulky uterus with thickened endometrium. Magnetic resonance imaging showed a T1 hypointense and T2 mixed-intense (solid and cystic) lobulated mass involving the right ovary of 9.1 × 7.6 cm in size. Bulky uterus showing grossly thickened endometrium with breach in junctional zone was also noted (Fig. 1a). Post-contrast study showed significant enhancement of right ovarian mass and uterine endometrium, and a diagnosis of neoplastic lesion was made from imaging studies (Fig. 1b). Endometrial aspiration revealed endometrioid adenocarcinoma. On staging laparotomy, a 10 × 11-cm-sized solid right ovarian tumor and a bulky uterus were seen. The left ovary, fallopian tube, intestines, liver, biliary tract, pancreas, and omentum were normal with minimal ascites. Total abdominal hysterectomy with bilateral salphingoopherectomy, infracolic omentectomy, and pelvic lymphadenectomy was performed.
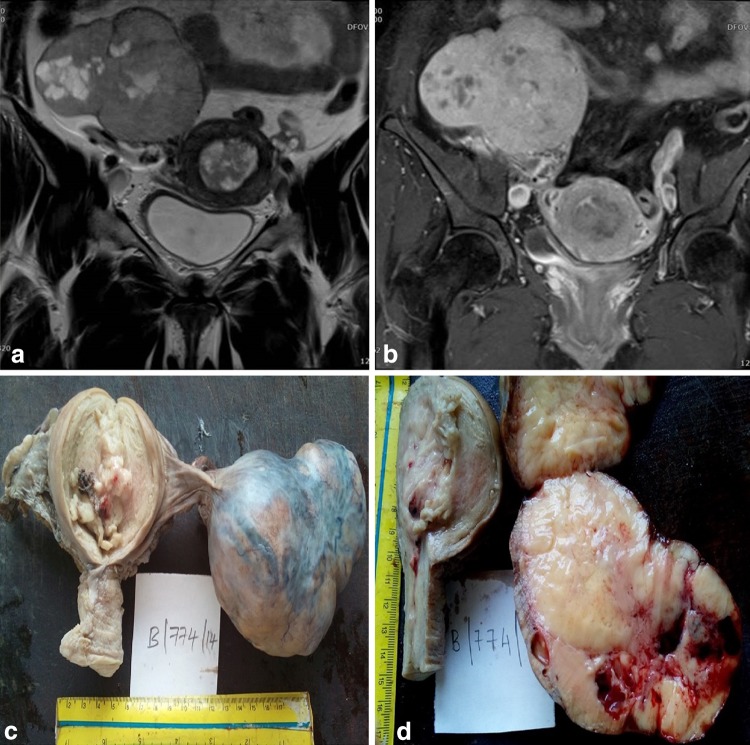
Fig. 1.
a T2 coronal magnetic resonance sequence shows uterus with grossly thickened endometrium and breach of junctional zone. Large right ovarian mass with solid and cystic areas is also appreciated. b T1 fat sat coronal post-contrast magnetic resonance sequence shows heterogenous enhancement of endometrial cavity and diffuse enhancement of right ovarian mass with few non-enhancing cystic areas. c Gross photograph of uterus and cervix with enlarged right ovarian mass having nodular surface. Cut section of the uterus showing exophytic growth in endometrial canal. d Cut section of the right ovary showing gray white nodules with cystic areas with compressed normal parenchyma at the periphery
On gross examination, the right ovary was found to be enlarged and measured about 9 × 7.5 × 5 cm with nodular surface and no capsular breech (Fig. 1c). The cut section revealed a solid gray white tumor with areas of hemorrhage, cysts, and compressed ovarian parenchyma at the periphery (Fig. 1d). An exophytic growth of 4 × 2 cm in size was seen at the fundal and posterior walls of the endometrial canal with no gross invasion of the myometrium (Fig. 1c). Left ovary, omentum, and bilateral fallopian tubes were grossly unremarkable. Microscopy sections from the right ovarian mass showed a cellular tumor composed of multiple nodules of interlacing spindle-shaped cells in fascicles with no atypia, and a mitotic count ranging from 0 to 1 per 10 high-power fields consistent with fibroma. No thecomatous elements were found in the tumor even on performing fat stain. Interspersed among the bland stromal cells were small nests of cells with grooved oval nucleus and minimal cytoplasm, comprising <5 % of total tumor area (Fig. 2a). These cells were strongly immunoreactive for inhibin (Fig. 2b). The endometrial growth showed features of endometrioid adenocarcinoma (Grade 1) (Fig. 2c) and multiple foci of complex hyperplasia with atypia of endometrial glands (Fig. 2d). Focal invasion into the myometrium involving less than 2 % of the thickness was noted. The omentum, lymph nodes, right ovary, and both fallopian tubes were free from tumor. A final diagnosis of well-differentiated endometrioid adenocarcinoma (Grade I) of the uterus with fibroma and minor sex cord elements of right ovary was made. The patient did not receive radiotherapy postoperatively and is free from recurrence or distant metastasis since one year.
Fig. 2.
a Microphotograph showing fibroma with small aggregates of sex cord type cells in tubular structure (H&E ×400). b Inhibin-intense cytoplasmic staining in the minor sex cord element cells (Immunohistochemistry ×400). c Well-differentiated endometrioid adenocarcinoma of uterus showing back-to-back glands and stromal disappearance (H&E ×100). d Complex atypical hyperplasia showing glandular overcrowding with loss of polarity and cytological atypia (H&E ×200)
Discussion
Ovarian stromal tumor with minor sex cord elements was first described by Young and Scully in a series of seven cases [1]. These patients present with bleeding per vagina or abdominal mass. The average age of presentation is 16–65 years with a mean age of 59 years [1]. Most tumors ranges from 1 to 10 cm; however, a case with a tumor of 20-cm size is also reported in the literature [2]. These tumors are solid, firm, gray white, and in cases of fibrothecoma yellow-white, in color. Microscopy shows a predominantly fibromatous or thecomatous tumor and a minor component of sex cord elements occupying less than 10 % or not more than 0.45 mm of the tumor area. These cell nests may be of well-differentiated granulosa cells or tubular structures, resembling immature sertoli cells, sharply demarcated from the surrounding stroma. But in some cases, the indifferent sex cord cells may be seen intermingling with the stromal component [1, 2]. The sex cord elements will be immunoreactive to inhibin, calretinin, CD99, CD 56, antikeratin antibody KL1, and MIC, while negative for smooth muscle actin, cytokeratin, and epithelial membrane antigen [4].
Ovarian stromal tumor with minor sex cord elements has to be properly identified as this tumor in many instances has been mistaken for ovarian fibromatosis, Brenner tumor, and adenofibroma. Spindle-shaped cells with abundant collagen and edema with preserved follicular structures of the ovary are evident in ovarian fibromatosis [2]. In our case, the presence of compressed ovarian tissue was only seen in the periphery. Brenner tumor shows transitional cells or mucinous cells as the epithelial aggregates. Adenofibroma shows varying sized numerous tubular glands when compared to sex cord elements of ovarian stromal tumor [1].
Only three cases of ovarian stromal tumor with minor sex cord elements coexisting with endometrial carcinoma have been reported in the English literature. Young and Scully reported one such case in a series of seven cases, wherein the major component was of stromal leydig cell type. Another case of luteinized thecoma showed only endometrial hyperplasia. The other five cases of fibroma did not show any evidence of hormonal function [1]. Kumar et al. reported one case of fibrothecoma, and Lee and Ahmed reported a case of fibrothecoma with focal fibrosarcomatous change associated with endometrial carcinoma [2, 3]. In these two cases, the thecoma cells were identified by light microscopy. Androgenic manifestation of fibrothecoma with minor sex cord elements was also reported by Sood et al. which was seen in a 13-year-old patient [4]. In all of these cases, the endocrine function was due to luteinized thecoma cells or Leydig cells. In our case, extensive search and fat stains did not reveal any thecoma cells. Hence, the functional activity was attributed to the ovarian fibroma and minor sex cord elements, which was evident by endometrioid adenocarcinoma and complex atypical hyperplastic endometrium resulting in postmenopausal bleeding.
Conclusion
Ovarian fibroma with minor sex cord elements is an uncommon tumor and its coexistence with endometrioid adenocarcinoma has been presented. The presence of estrogenic manifestations should alert a clinician of this entity and meticulous histopathological examination of the tumor is necessary to identify additional sources of hormonally active elements in ovarian stromal tumor, such as sex cord elements.
Acknowledgments
Funding
No funding was received for conducting the study.
Dr. G. Shilpa
is working as an Assistant Professor in the Department of Pathology, Sri Devraj Urs Medical College since 2013 till date. She did her under graduation from Kempegowda Institute of Medical Sciences and Post MD Pathology from Mysore Medical College in 2010 and won a Gold medal from Rajiv Gandhi University of Health Sciences. She has also done a certificate course in Cytological techniques from St. John’s Medical College. She has been always involved in many research activities since her undergraduate course. She has keen interest in gynecology with special interest in cervical cytology. She has presented many research papers in national and international conferences. She has also published many papers in international and national journals. She was involved in many projects in the Department of Pathology and Obstetrics and Gynecology at Sri Devraj Urs Medical College. She was also involved in undergraduate research activity and had been a resource person for DEMEDCON 2014 and Pathology Postgraduate quiz conducted in the year 2014 in Sri Dev Ra Urs Academy of Higher Sciences. She was the organizing secretary of National CME on Gastrointestinal Pathology conducted by SDUAHER in 2014.
Compliance with Ethical Standards
Conflict of Interest
All authors declare that they have no conflict of interest.
Footnotes
Dr. G. Shilpa is an Assistant Professor in the Department of Pathology; Dr. E. Gomathy is a Professor in the Department of Obstetrics and Gynecology; Dr. M. L. Harendra Kumar is a Professor in the Department of Pathology; Dr. M. Anil Kumar Sakalecha is a Professor in the Department of Radiodiagnosis, Sri Devraj Urs Medical College, Kolar, India
References
- 1.Young RH, Scully RE. Ovarian stromal tumor with minor sex cord elements; a report of seven cases. Int J Gynecol Pathol. 1983;2:227–234. doi: 10.1097/00004347-198303000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Kumar S, Mathur S, Subbaiah M, et al. Ovarian stromal tumor with minor sex cord elements with coexistent endometrial carcinoma. Indian J Med Paediatr Oncol. 2013;34:44–46. doi: 10.4103/0971-5851.113432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee HY, Ahmed Q. Fibrosarcoma of the ovary arising in a fibrothecomatous tumor with minor sex cord elements. A case report and review of literature. Arch Pathol Lab Med. 2003;127:81–84. doi: 10.5858/2003-127-81-FOTOAI. [DOI] [PubMed] [Google Scholar]
- 4.Sood N, Nigam JS, Goyal G, et al. Virilizing ovarian fibrothecoma with minor sex cord elements in a 13 year old girl: a rare case. Pediatr Rep. 2014;6(3):5447. doi: 10.4081/pr.2014.5447. [DOI] [PMC free article] [PubMed] [Google Scholar]