Introduction
Primary leiomyosarcomas of the ovary are very rare tumors with only few cases having been reported so far and represent less than 0.1 % of all ovarian malignancies. These are highly aggressive tumors and have a very poor prognosis. Pathogenesis of this tumor is still uncertain. These cases mostly present in peri- and postmenopausal women aged 45–60 years. Leiomyosarcomas are usually unilateral and grow to a very large size making wide excision often impossible. These tumors are well circumscribed, large and often with necrosis, hemorrhage, and cystic degeneration. Marked cellular pleomorphism and brisk mitotic activity are frequent findings in such tumors. Most patients present with advanced disease having distant metastases to lungs and liver at presentation. Overall 5-year survival is reported as only 20–30 %. Because of its extreme rarity and low survival rate, we present this case of ovarian neoplasm in a young woman of 27 years with disease-free survival of 47 months after surgery and adjuvant chemotherapy.
Case Report
A 27-year-old female presented to the Gynecological OPD with complaints of pain in right lower abdomen and abdominal distension. Her past medical and surgical history was uneventful. She had one full term normal vaginal delivery. A soft to firm lump of about 8 × 6 cms was palpable in the right iliac fossa, and on vaginal examination, the lump was found with restricted mobility and tenderness. Ultrasound examination revealed a complex mass in the right adnexal region measuring 9.7 × 5.2 cm. The left ovary, uterus, and cervix were normal. Routine preoperative investigations were normal except for mild anemia. Serum Beta HCG was 5 mIU/mL, and CA125 was 5.2 IU/mL. Initially, the patient underwent simple right cystectomy as malignancy was not suspected. The patient was referred to Gynecological Oncology Department as histopathology of sample revealed a high grade pleomorphic sarcoma. Chest X-ray and a CT scan of whole abdomen done to look for primary tumor were found normal. Laparotomy revealed a residual mass originating from the right ovary and adherent to the bladder. The uterus and left ovary appeared normal, the omentum was adhered to the uterus, ovaries, and the abdominal wall. The mass was separated from the bladder with some difficulty, and hysterectomy with bilateral salpingo-oophorectomy, total omentectomy, and pelvic and para aortic lymph node dissection was done, and tissue was sent for histopathological examination. Histopathology reported more than ten mitotic figures per ten high power fields, fascicles of brightly eosinophilic spindle cells with ovoidal- to cigar-shaped nuclei intersecting each other at wide angles with marked atypia which contained pleomorphic nucleus with prominent nucleoli (Fig. 1). Immunohistochemistry revealed intense cytoplasmic positivity for desmin and smooth muscle actin in all the cells. CD 10 and CD 34 were negative so the final diagnosis of high grade Pleomorphic Leiomyosarcoma was made.
Fig. 1.
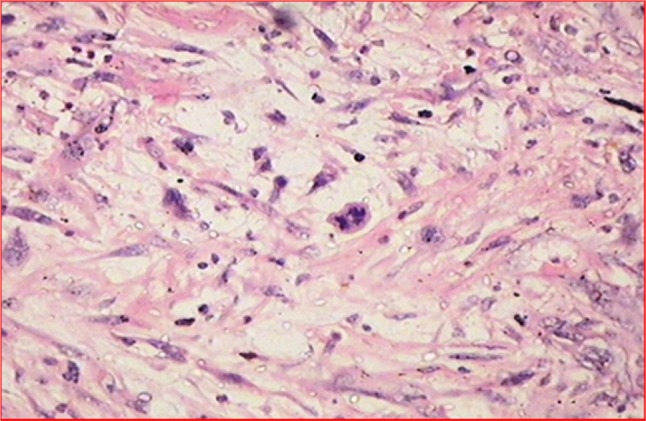
HPE showing spindle cells
The patient was referred to medical oncology and received adjuvant chemotherapy comprising 6 cycles of docetaxel (80 mg/m2) and gemcitabine (1000 mg/m2). Chemotherapy was uneventful and response to therapy was evaluated by CT scan according to WHO response criteria. Serum CA 125 was within normal limits. Patient is on regular follow-up and is doing well after 47 months of surgery. She is leading a normal life with no evidence of relapse or recurrence.
Discussion
Primary leiomyosarcoma of the ovary usually affects postmenopausal women with very few cases having been reported in the younger age group, as in the present case of a 27-year-old female [1]. Pure primary sarcomas originating in the ovary are rare (<1 %), and only a few cases of fibrosarcoma, leiomyosarcoma, angiosarcoma, and other histologic types of sarcoma have been reported [2]. On gross examination, these tumors are found to be similar to any other sarcomas. Controversy exists in the management of leiomyosarcoma of ovary with no established treatment for these tumors other than surgery [3]. Debulking surgery, consisting of total abdominal hysterectomy, bilateral salpingo-oophorectomy, and removal of the tumor masses, is the recommended surgery. In patients with primary ovarian sarcoma, optimal debulking surgery appears to be of prognostic significance [4]. Various adjuvant therapies have been proposed, including radiotherapy and chemotherapy, but with no additional benefits.
The prognosis of ovarian leiomyosarcoma is very poor, and dependent on the tumor size, stage, and mitotic index. Taskin et al. reported that 63 % of stage-1 patients survived with no evidence of the disease after a mean follow-up period of 41.7 months, while 81.25 % of patients at a higher stage died after a mean follow-up period of only 14.7 months. The 5-year survival rate was 32 % overall, 63 % for endometrial stromal sarcoma, 30 % for mixed mesodermal sarcomas, and 18 % for leiomyo-myosarcoma [5].
We report disease-free survival of 47 months in our patient who is still alive and healthy. E J Goodall et al. presented a case of ovarian leiomyosarcoma with reported disease-free survival of 22 months after surgery alone [3]. In a 58-year-old postmenopausal woman with Stage Ia leiomyosarcoma of ovary, Zygouris et al. reported no evidence of recurrence 21 months after initial surgery, without any postoperative adjuvant therapy [6]. In another report of primary leiomyosarcoma of the ovary, adjuvant treatment with ifosfamide and doxorubicin was used, achieving progression-free survival of 24 months and overall survival of 36 months [7].
Further studies are needed to understand the details about the nature, clinical behavior, and treatment of this very rare tumor.
The overall prognosis of leiomyosarcoma of ovary is poor, but if diagnosed in early stage and managed with optimal surgery and chemotherapy, there might be significant improvements in survival as seen in our case.
Dr. Sangeeta Pankaj
is interested in the areas of Gynecological Oncology, teaching, and research work. She is regularly doing screening for cervical and breast cancers. She has dedicated her services solely to prevent and alleviate sufferings of women with Gynecological Malignancies.
Conflict of Interest
Dr. Syed Nazneen, Dr. Anjili Kumari, Dr. Vijayanand Choudhary, Dr. Simi Kumari, and Dr. Sangeeta Pankaj declare that they have no conflicts of interest and they have not received any grant.
Ethical approval
Study has been approved by Departmental Research committee.
Footnotes
Syed Nazneen is a Senior Resident with an area of interest in Gynecological Oncology; Anjili Kumari is a Senior Resident with an area of interest in Gynecological Oncology; Simi Kumari is a Senior Resident with an area of interest in Gynecological Oncology; Sangeeta Pankaj is an Associate Professor with an area of interest in Gynaecological Oncology in the Regional Cancer Centre, Indira Gandhi Institute of Medical Sciences, Patna, India; Vijayanand Choudhary is a, Associate Professor with area of interest in Pathology at Indira Gandhi Institute of Medical Sciences, Patna, India.
References
- 1.Vijaya Kumar J, Khurana A, Kaur P. A rare presentation of primary leiomyosarcoma of ovary in a young woman. ecancer. 2015;9:524. doi: 10.3332/ecancer.2015.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouie SM, Cracchiolo B, Heller D. Epithelioidleiomyosarcoma of the ovary. Gynecol Oncol. 2005;97:697–699. doi: 10.1016/j.ygyno.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 3.Goodalla EJ, Madhuria T, Manuela SB. The management dilemma of leiomyosarcoma of the ovary. World J Oncol. 2011;2(5):265–266. doi: 10.4021/wjon362w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai Y, Shen K, Lang JH. Primary sarcoma of the ovary: clinicopathological characteristics, prognostic factors and evaluation of therapy. Chin Med J (Engl) 2011;124(9):1316–1321. [PubMed] [Google Scholar]
- 5.Taşkin S, Taşkin EA, Uzüm N. Primary ovarian leiomyosarcoma: a review of the clinical and immunohistochemical features of the rare tumor. Obstet Gynecol Surg. 2007;62:480–488. doi: 10.1097/01.ogx.0000268629.16151.71. [DOI] [PubMed] [Google Scholar]
- 6.Zygouris D, Androutsopoulos G, Grigoriadis C. Primary ovarian leiomyosarcoma. Eur J Gynaecol Oncol. 2012;33(3):331–333. [PubMed] [Google Scholar]
- 7.Rivas G, Bonilla C, Rubiano J. Primary leiomyosarcoma of the ovary: a case report. Case Rep Clin Med. 2014;3:192–196. doi: 10.4236/crcm.2014.34045. [DOI] [Google Scholar]


