Introduction
Rupture of uterus is a potentially catastrophic event in which the integrity of the myometrial wall is breached. It can be of two types, incomplete and complete. Spontaneous rupture in early pregnancy is rare to occur. Incidence of rupture in unscarred uterus is about 1 in 17,000–20,000 deliveries [1], while that in scarred uterus is 5.1 per 10,000 deliveries [2]. Here we are presenting our experiences with 3 cases of rupture of uterus in early pregnancy.
Case 1
A young 22-year-old multipara G4P3L3 came to our emergency with complaints of amenorrhea 5 months, pain abdomen and vaginal bleeding for 1 day. Her past obstetrics history consisted of three full-term vaginal deliveries. She had neither visited any antenatal clinic nor gone through any antenatal investigations before coming to us. She had undergone minilaparotomy ligation two and half years back. There was no history of trauma, MTP pills intake, dilation and evacuation, previous uterine surgery and instrumentation. On general physical examination, she was conscious, oriented and pale. Her pulse rate was 100/min, and BP was 100/60 mmHg. There was a small vertical scar present at suprapubic region with minimal lower abdomen distension. A mass of 14-week size was palpable with tenderness more on right side. On per speculum (P/S) examination, bleeding was seen through cervical os. On per vaginum (P/V) examination, uterus was bulky, and a mass of 14-week size was felt through right fornix. It was firm and tender with restricted mobility.
Her investigations showed low hemoglobin level (7 gm%). Ultrasound showed single 15-week extra uterine pregnancy in right adnexa with normal-sized uterus. Free fluid was seen in pouch of Douglas (POD). Ruptured ectopic pregnancy was suspected, and emergency laparotomy was performed. There was hemoperitoneum, and 1000 ml blood was drained out. Vertical rent was seen on the postero-lateral wall of uterus, extending up to vault (Fig. 1). Part of placenta was seen hanging out of the rent, and fetus and placenta were lying in the POD. As tissues were very friable and weak and bleeding could not be controlled so, total hysterectomy was done. Postoperative period was uneventful. Histopathology report showed gravid uterus with evidence of rupture, fetus measuring 15 cm in length and placenta with chorionic villi.
Fig. 1.
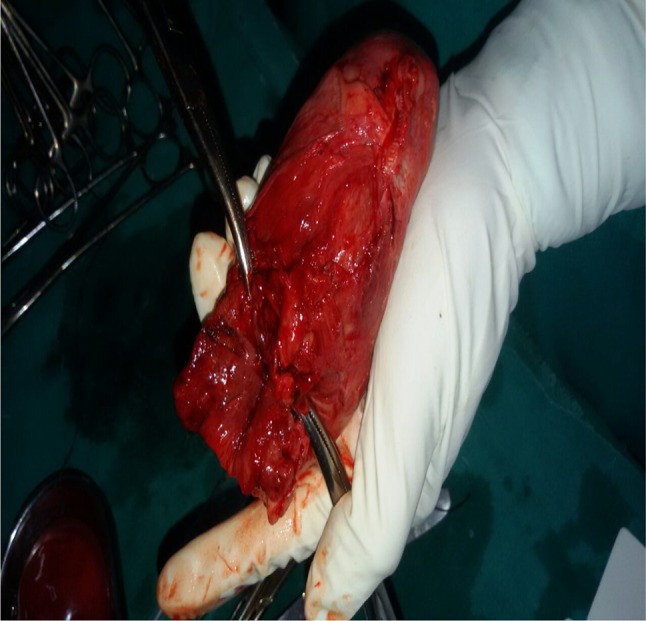
Specimen of uterus after hysterectomy with vertical rent on postero-lateral surface
Case 2
A 27-year-old G4P2L2 with 17-week pregnancy came to our emergency with complaints of severe pain abdomen for 1 day and bleeding per vaginum. She had previous one cesarean section 5 years back followed by vaginal delivery 2 years back. There was no history of intake of MTP pills intake and trauma. On examination, her pulse rate was 120/min, and BP was 100 systolic. Lower abdomen tenderness and guarding were present. On P/S examination, bleeding was seen coming through cervical os. On P/V examination, cervical os was 3 cm dilated and a rent of 4 cm was felt in the anterior wall of the uterus. No products of conception were felt through cervical os. Scar dehiscence was suspected. No emergency ultrasound was available. Exploratory laparotomy was performed, and 500 ml blood was drained from peritoneal cavity. Dead fetus was seen inside peritoneal cavity with placenta. Complete rupture was present at previous scar site which was repaired. One unit of blood was transfused in postoperative period.
Case 3
A 28-year-old G4P3L3 with 2-month amenorrhea came to our emergency with complain of sudden onset of severe pain abdomen with bleeding per vaginum. She had previous 2 full-term vaginal deliveries followed by one lower segment cesarean section 4 years back. She had not done any routine antenatal checkup and investigation in this pregnancy. On examination, she was severely pale, her pulse rate was 130/min, and blood pressure was 90/60. Her urine pregnancy test was positive. On per abdomen examination, at scar site tenderness was present. On P/S examination, bleeding was seen through cervical os. On P/V examination, uterus was about 8- to 10-week size with tenderness, and bilateral fornices were clear. Ultrasound of pelvis was done which showed hemoperitoneum, and intrauterine pregnancy of 9 weeks was seen in lower segment. Emergency laparotomy was performed which revealed 1500 ml of hemoperitoneum. Amniotic sac with fetus inside and placenta were present inside peritoneal cavity. Small rupture of 3 cm was present in lower segment near right angle (Fig. 2). Small bits of membrane adhered to it. It was cesarean scar site ectopic pregnancy, which got ruptured. Repair was done, tissue sent for histopathology. Two unit of blood was transfused in perioperative period, and rest of the postoperative period was uneventful. Histopathology report confirmed the above finding.
Fig. 2.
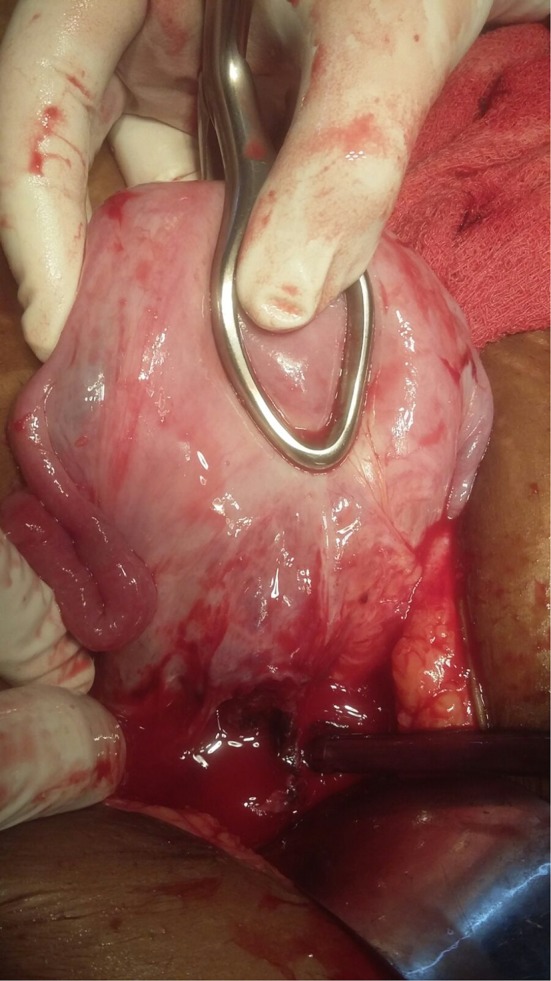
Small 3-cm rent seen at lateral angle (ruptured scar site ectopic pregnancy)
Discussion
Rupture of uterus is one of the life-threatening obstetrics emergencies. It is associated with high maternal and fetal morbidity. Rate of maternal death from uterine rupture is 0–1 % in developed nations, but in developing countries, it is 5–10 % [3]. Although rupture in early pregnancy is rare compared to term pregnancy, it is one of the challenging situations both to diagnose and to manage. Diagnosis is often delayed in early gestation because signs and symptoms are nonspecific as pain abdomen, vaginal bleeding and contour of small uterus are difficult to assess as compared to term uterus.
There are many risk factors for rupture of scarred and unscarred uterus. Because unscarred uterus multiparity is one of the most important, it is often associated with other causes also. Stretching, tearing or bruising of repeated childbirth makes uterine wall very weak, so chances of rupture increase with every subsequent pregnancy. Schrinsky and Benson [4] found 32 % women who had unscarred uterine rupture were multipara. Other risk factors are uterine anomaly, uterine curettage, uterine diverticula, malpresentation, chronic corticosteroid use, cocaine abuse, direct or indirect uterine trauma, placenta percreta, increta, adenomyosis, fibroid uterus, external uterine maneuver, collagen matrix disorder as Ehlers–Danlos syndrome (type 4). For rupture of scarred uterus, risk factors are previous cesarean section, myomectomy. In case of previous cesarean section, risk of rupture increases with classical incision or low vertical incision than lower uterine segment and short interconceptional interval (<18 months). Some authors also believe that single-layer closure with locking also increases the risk [5, 6]. Regarding the myomectomy scar, there is no significant difference in the risk of rupture between the laparoscopy and open myomectomy surgery. Most obstetricians believe that entry into uterine cavity at the time of surgery is associated with increased risk of rupture in future pregnancy. There is no definite evidence about the risk of rupture related to the number, location or size of fibroid and suture technique at time of surgery [7]. With increasing cesarean rate worldwide, incidence of rupture has also increased, even midtrimester rupture is not uncommon. Incidence of cesarean scar site ectopic pregnancy has also increased. It can be diagnosed early by transvaginal ultrasonography. It can be managed conservatively by sonography-guided injection of methotrexate in gestational sac.
Clinical scenario of rupture of uterus in early pregnancy usually mimics the picture of, ruptured heterotrophic or ectopic pregnancy, ruptured corpus leuteal cyst, abruption placenta, molar pregnancy with secondary invasion. Most critical step for management is timely diagnosis. Surgical management depends on type of rupture (lower segment and upper segment rupture), extent of rupture, condition of women at time of surgery, degree of shock, desire of fertility and amount of blood loss. Rupture can be managed by repair of rupture site, but many a times hysterectomy is required. Indications of repair are low transverse rupture, desire of future fertility, no extension of tear to the broad ligament, cervix or paracolpos, good general physical condition of mother, easily controllable hemorrhage and no clinical or laboratory evidence of coagulopathy.
Complication of rupture includes anemia, infection, disseminated intravascular coagulation, bladder injury, maternal death, fetal hypoxia, fetal acidosis, low APGAR score, severe blood loss and fetal or neonatal death. Risk of rerupture in future pregnancy with lower segment rupture is 6 % and with upper segment rupture is 32 % [8]. So in future pregnancy, it is advisable to do elective LSCS when fetal lung maturity is assured and before onset of labor [8].
So far very few cases have been reported for rupture of uterus of early pregnancy. Largest case series which is available in the literature is of 3 cases of midtrimester rupture. Other cases are reported in the form of case report only. Park et al. [9] reported a case of rupture of unscarred uterus at 10 weeks of gestation, and the only risk factor in their case was multiparity. In developing countries like India, low female literacy rate has negative impact on the use of family planning methods and contraception. This increases the number of multipara and grand multipara pregnancy and short interconceptional period, so risk of rupture increases. Women also become anemic and undernourished which increases the morbidity and mortality associated with this condition.
Conclusion
Rupture of uterus is life-threatening emergency. Proper antenatal care is important for each and every patient. Early referral of high-risk patients as grand multipara, anomaly uterus, previous uterine surgery to higher center where 24 h obstetrician, anesthetist and operation facility is available. Institutional delivery should be promoted. Awareness program about family planning methods should be encouraged. In cases of pain abdomen with amenorrhea with tachycardia and low and borderline low BP, rupture should be ruled out.
Zeepee Godha
has done postgraduation in Obstetrics and Gynecology from Aligarh Muslim University, India. She has been working as Senior Resident in Deen Dayal Upadhaya Hospital, New Delhi, India. She has keen interest in management of abnormal uterine bleeding in women. She has keen interest in academic research of clinical interest.
Conflict of interest
None.
Informed Consent
Informed consent was taken from all patients and hospital ethical board for study and publication.
Footnotes
Dr. Shashi Lata Kabra, M.S. (Obs & Gynae), is a specialist in Department of Obstetrics and Gynaecology, Deen Dayal Upadhaya Hospital, New Delhi, India; Dr. Poonam Laul, M.S. (Obs & Gynae), is a specialist in Department of Obstetrics and Gynaecology, Deen Dayal Upadhaya Hospital, New Delhi, India; Dr. Zeepee Godha, M.S., is a Senior Resident in Department of Obstetrics and Gynaecology, Deen Dayal Upadhaya Hospital, New Delhi, India; Dr. V. K. Kadam, M.S.(Obs & Gynae), is a specialist in Department of Obstetrics and Gynaecology, Deen Dayal Upadhaya Hospital, New Delhi, India.
Contributor Information
Shashi Lata Kabra, Email: drshashikabra@rediffmail.com.
Poonam Laul, Email: poonamlaul@rediffmail.com.
Zeepee Godha, Email: zeepee_dr@yahoo.co.in.
V. K. Kadam, Email: dr.jiteshajmera@yahoo.com
References
- 1.Gueye M, Baye MM, Ndiaye-Gueye MD, et al. Spontaneous rupture of an unscarred uterus before labor. Hindawi Publ Corp Case Rep Obstet Gynaecol. 2012;2012:231–232. doi: 10.1155/2012/598356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Zirqi I, Stray-Pedersen B, Forsén L, et al. Uterine rupture: trends over 40 years. BJOG. 2015 doi: 10.1111/1471-0528.13394. [DOI] [PubMed] [Google Scholar]
- 3.Bhaskar Rao K. Obstructed labor. In: Ratnam SS, Bhaskar Rao K, Arulkumaran S, editors. Obstetrics and gynecology for postgraduates. 1. Madras: Orient Longman; 1992. pp. 130–132. [Google Scholar]
- 4.Schrinsky DC, Benson RC. Rupture of the pregnant uterus: a review. Obstet Gynecol Surv. 1978;33(4):217–232. doi: 10.1097/00006254-197804000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Bujold E, Goyet M, Marcoux S, et al. The role of uterine closure in the risk of uterine rupture. Obstet Gynecol. 2010;116(43–50):61. doi: 10.1097/AOG.0b013e3181e41be3. [DOI] [PubMed] [Google Scholar]
- 6.Roberge S, Chaillet N, Boutin A, et al. Single- versus double-layer closure of the hysterotomy incision during cesarean delivery and the risk of uterine rupture. Int J Gynecol Obstet. 2011;115:5–10. doi: 10.1016/j.ijgo.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Weibel HS, Jarcevic R, Gagnon R, et al. Perspectives of obstetricians on labour and delivery after abdominal or laparoscopic myomectomy. J Obstet Gynaecol Can. 2014;36(2):128–132. doi: 10.1016/S1701-2163(15)30658-7. [DOI] [PubMed] [Google Scholar]
- 8. Cunningham F, Leveno K, Bloom S, et al. Williams Obstetrics. 23rd ed. McGraw Hill; 2009. p. 569.
- 9.Park Y-J, Ryu K-Y, Lee J-I, et al. Spontaneous uterine rupture in the first trimester: a case report. J Korean Med Sci. 2005;20(6):1079–1081. doi: 10.3346/jkms.2005.20.6.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]


