Abstract
For nearly a century, the heart was viewed as a terminally differentiated organ until the discovery of a resident population of cardiac stem cells known as cardiac progenitor cells (CPCs). It has been shown that the regenerative capacity of CPCs can be enhanced by ex vivo modification. Preconditioning CPCs could provide drastic improvements in cardiac structure and function; however, a systematic approach to determining a mechanistic basis for these modifications founded on the physiology of CPCs is lacking. We have identified a novel property of CPCs to respond to electrical stimulation by initiating intracellular Ca2+ oscillations. We used confocal microscopy and intracellular calcium imaging to determine the spatiotemporal properties of the Ca2+ signal and the key proteins involved in this process using pharmacological inhibition and confocal Ca2+ imaging. Our results provide valuable insights into mechanisms to enhance the therapeutic potential in stem cells and further our understanding of human CPC physiology.
1. Introduction
The heart was considered a postmitotic organ incapable of regeneration until the discovery of a resident population of cardiac stems cells brought about the potential for cardiac tissue regeneration [1]. Known as cardiac progenitor cells (CPCs) and primarily found in the myocardium, these cells have cardiogenic gene expression as well as the stem cell marker c-kit [2]. Since the first reports of c-kit+ CPCs, there has been controversy surrounding the ability of these cells to replace cardiac myocytes [1, 3–7]. Despite earlier reports that CPCs could replace damaged myocardium [1, 8], recent lineage tracking studies have provided compelling evidence that these cells do not become cardiac myocytes in vivo [4, 5, 7]. However, it has been shown that the regenerative capacity of these cells can potentially be enhanced by ex vivo modification. Several laboratories have demonstrated the feasibility and utility of ex vivo manipulation of adult stem cells modified by genetic engineering [9–13] or exposure to environmental, chemical, and biological treatments prior to delivery [9, 14–17]. The idea behind these strategies is to isolate a patient's CPCs and expand and modify them to create a more therapeutic phenotype.
Electrical stimulation is one treatment known to enhance cardiogenic potential of various stem cells via activation of calcium (Ca2+) signaling in adult cells [18–22]. Ca2+ is an integral second messenger in the heart, regulating the processes of excitation-contraction coupling (action potential-mediated Ca2+ entry triggers contraction) and excitation-transcription coupling (action potential-mediated Ca2+ entry triggers changes in gene expression). Previous reports showed that electrical stimulation of adult cardiac adipose tissue-derived progenitor cells caused changes in cell phenotype and genetic machinery, making them more suitable for cardiac regenerative approaches [19]. Furthermore, electrical stimulation of adult progenitor cells has been shown to induce a variety of responses, such as cytoskeletal rearrangements, migration, proliferation, and differentiation, as well as the de novo expression of the late cardiac sarcomeric proteins, troponin T and cardiac alpha actinin, and increase the expression of connexin 43 and its relocation to the cell membrane [19–22]. Recent data indicate that Ca2+ is involved in assembly of contractile apparatus and localization of key cardiogenic transcription factors, such as myocyte enhancer factor 2c, in CPCs [23]. Despite these results, the mechanisms behind the enhanced cardiospecific gene expression and the increased therapeutic potential of adult CPCs reported with electrical stimulation have not been elucidated [23–25]. Furthermore, these experiments have been conducted with very little knowledge of the basic composition of these cells to direct their efforts. Systematic studies of the regulation of Ca2+ handling in CPCs would substantially advance our knowledge of CPCs physiology and their potential in cardiac repair, providing fundamental information that could be used for developing new therapeutic approaches to improve myocardial repair and regeneration.
Toward that end, we aimed to characterize the mechanism of electrically induced Ca2+ handling in human c-kit+ cardiac progenitor cells. In this study, we have identified a novel property of CPCs to respond to electrical stimulation by initiating intracellular Ca2+ oscillations. CPCs were isolated from human atrial tissue and pooled from multiple donors to prevent patient-specific results in our experiments. These cells were loaded with the Ca2+-sensitive dye fluo-4/AM to measure the cytosolic and nuclear Ca2+ oscillations in response to acute electrical stimulation using live cell confocal microscopy. We characterized the Ca2+ signal by measuring the amplitude of cytosolic and nuclear Ca2+ oscillations elicited by electrical stimulation, identified the mechanism by which Ca2+ oscillations initiate and propagate throughout the cells, and also determined the key proteins involved in this process. This project may have implications on many stem cell therapies and provide us with valuable insights into mechanisms to enhance the therapeutic potential of stem cells and further our understanding of human CPC physiology.
2. Materials and Methods
2.1. Patient Aspects of the Proposed Research
Human cardiac progenitor cells (CPCs) used in this study were obtained under IRB approval which allows for isolation of CPCs from deidentified atrial waste tissue removed during surgical repair of congenital heart defects. Patients were not subject to any additional risks by involvement in this study. Confidentiality of patient information was assured as we did not record the patients' names or demographic information and did not contact the patients. A clinical research nurse obtained needed information such as age, gender, ethnicity, diagnosis, and drug therapy, but tissue samples were deidentified and data obtained from the biopsy were identified by an internal lab number only. No preference as to gender, race, or ethnicity was used for patient enrollment.
2.2. Reagents
All chemicals and reagents were purchased from Sigma-Aldrich (St. Louis, MO, USA), unless noted otherwise. Stock solutions of tetracaine and 2-aminoethoxydiphenyl borate (2-APB) were made in methanol and ethanol, respectively, and diluted to work concentrations in Tyrode's solution. The vehicle was added to Tyrode's solution for control experiments. Primary antibodies for the L-type Ca2+ channel and the inositol 1,4,5-trisphosphate receptor were obtained from Santa Cruz Biotechnology (Dallas, TX, USA), and primary antibody for the ryanodine receptor and secondary antibodies Alexa Fluor 488 and Alexa Fluor 647 were purchased from Thermo Fisher Scientific (Waltham, MA, USA).
2.3. Culturing of Human Cardiac Progenitor Cells
Human child (aged 1–5 years) cardiac progenitor cells were isolated from biopsied tissue using c-kit antibody-conjugated magnetic beads and propagated in culture as previously described [26]. Briefly, tissue was minced and digested with type 2 collagenase (1 mg/mL) in Hank's balanced salt solution and passed through a 70 μm filter. Cells were incubated with Dynabeads (Thermo Fisher Scientific, Waltham, MA, USA) conjugated to a c-kit antibody (Santa Cruz Biotechnology, Dallas, TX, USA) prior to magnetic sorting. Sorted cells were plated in a T-75 tissue culture flask and expanded to confluence. Cells were pooled from 4–6 donors to reduce variability. CPC culture media consisted of Ham's F-12 basal media (Mediatech, Manassas, VA, USA) along with 10% fetal bovine serum (Atlanta Biologicals, Flowery Branch, GA, USA), 1% penicillin, 1% streptavidin, 1% L-glutamine, and 0.1 μg/mL basic fibroblast growth factor. Prior to experiments, cells were plated on glass coverslips and allowed to attach overnight at 37°C.
2.4. Intracellular Calcium Measurements
Cells were loaded with 10 μM fluo-4/AM for 20 min followed by a 20 min wash in Tyrode's solution for deesterification of the dye. Electrical field stimulation was applied using an IonOptix MyoPacer Cell Stimulator (10 ms duration, 32 V; Westwood, MA, USA) and fluo-4 was excited at 488 nm and emission collected at 515 ± 15 nm using laser scanning confocal microscopy (FV1000, Olympus, Melville, NY, USA). Calcium oscillation measurements were acquired from CPCs during 0.5 or 1 Hz stimulation bathed in Tyrode's solution, which contained (in mM) 130 NaCl, 4 KCl, 2 CaCl2, 1 MgCl2, 10 D-glucose, and 10 Hepes, pH 7.4 with NaOH. All experiments were performed at room temperature (20–24°C). Data were analyzed using Olympus FV1000 FluoView software and Fiji [27].
2.5. Membrane Staining
Cell membranes and transverse tubular structures were visualized with the membrane-bound fluorescent probe Di-8-ANEPPS (Thermo Fisher Scientific, Waltham, MA, USA) by 2-dimensional confocal microscopy. Cells were loaded for 15 min with Di-8-ANEPPS (5 μM) in Tyrode's solution and the indicator was excited at 488 nm, and emission was measured at >600 nm.
2.6. Immunocytochemistry
CPCs were plated on glass coverslips, fixed in 4% paraformaldehyde, permeabilized with 0.1% Triton, and blocked with 3% BSA/PBS for 2 hrs. Cells were treated with the appropriate primary (Cav2.1, type 2 IP3R, and RyR2) and secondary antibodies for 2 hrs at dilution of 1 : 500. After washing with PBS, VECTASHIELD HardSet Antifade Mounting Medium containing DAPI (Vector Laboratories, Burlingame, CA, USA) was used to mount the coverslips onto glass slides for visualization.
2.7. Long-Term Electrical Stimulation
CPCs were seeded at a density of 4 × 105 cells/well in a 6-well C-dish (IonOptix, Westwood, MA, USA) and incubated in stimulation media. CPC stimulation media consisted of Ham's F-12 basal media along with 10% fetal bovine serum, 1% penicillin, 1% streptavidin, 1% L-glutamine, and 2 mM CaCl2. The C-Pace EP Culture Pacer (IonOptix, Westwood, MA, USA) was used for culture stimulation at 0.5 Hz, 10 ms duration, 32 V for 72 hrs. Media were changed every 24 hrs.
2.8. Cell Alignment Quantification
After 72 hours of electrical stimulation, cells were immediately fixed in 4% paraformaldehyde for 20 minutes at room temperature. Unstimulated cells cultured in stimulation media for 72 hrs or cells stimulated in Ca2+-free media for 72 hrs were also processed and stained as described below for basal and Ca2+-dependent alignment quantification. Following three washes in 1x PBS, the cells were permeabilized with 0.1% Triton in 1x PBS. Cells were again washed and then blocked in 3% bovine serum albumin for 1 hour at room temperature. Cells were then stained with 10 μg/mL fluorescein-5-maleimide for 1 hour at room temperature in the absence of light, followed by washing. Cells were washed prior to imaging on an Olympus IX70 inverted fluorescent microscope (Melville, NY, USA). Two-dimensional fluorescent images were acquired using the 20x objective and analyzed with Fiji software using the directionality function to obtain the primary angle of the cells and the percent of cells within one standard deviation of the direction of the applied electrical field [27].
2.9. Data Presentation
Fluorescence traces and confocal line scan data are presented as individual observations representative of multiple recordings or as the average of multiple recordings. Fluorescence traces were background subtracted and plotted as F/F 0, where F 0 is the basal fluorescence in resting cells prior to electrical stimulation (for initial oscillation) or the diastolic fluorescence just before an oscillation (for subsequent oscillations). Fluorescent cellular images are presented as two-dimensional images representative of multiple trials. Summary data are presented as the mean ± SD of n measurements, where n is the total number of cells from 4 different pools of cells. Statistical comparisons between groups were performed with Student's t-test. Differences were considered statistically significant at p < 0.05.
3. Results and Discussion
3.1. Global Ca2+ Oscillations in Electrically Stimulated Human Cardiac Progenitor Cells
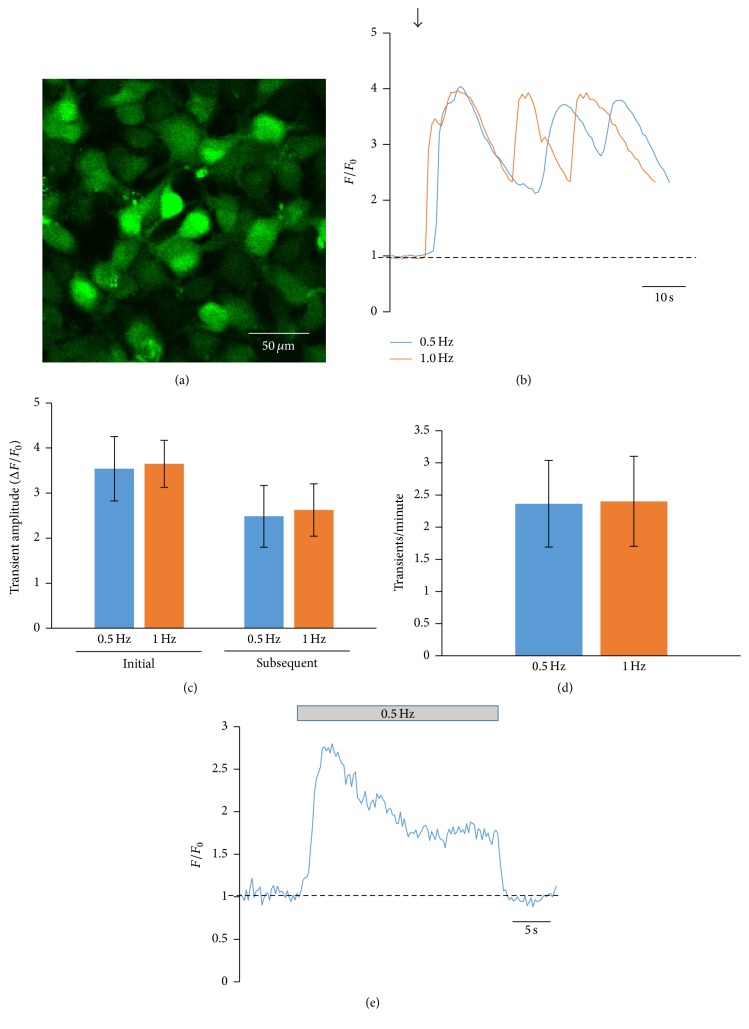
We have obtained human cardiac tissue from children undergoing repair for congenital heart defects and utilized these samples for isolation of human c-kit+ CPCs by a method previously described by our laboratory [26, 28–31]. Our technique results in a population of cells that are ~94% positive for the stem cell marker c-kit [26]. CPCs were loaded with the Ca2+ dye fluo-4/AM and stimulated at 0.5 or 1 Hz. Figure 1 shows representative Ca2+ oscillations in CPCs elicited by electrical stimulation. A rapid rise in cytosolic Ca2+ was observed followed by frequency-independent cytosolic Ca2+ oscillations (Figure 1(b)). After the initial oscillation, subsequent oscillations did not decline back to baseline levels but instead came to a new level of cytosolic “diastolic” Ca2+ presumably due to loading of the cell with Ca2+. We then quantified the amplitude of these Ca2+ oscillations and compared them based on the frequency of electrical stimulation (0.5 or 1 Hz). Quantification of the amplitude of the Ca2+ oscillations showed no significant difference between the initial oscillation amplitudes at 0.5 or 1 Hz or the subsequent oscillation amplitudes (Figure 1(c)). Furthermore, the stimulation frequency did not affect the rate at which Ca2+ oscillations were observed in these cells (Figure 1(d)). Despite the subsequent Ca2+ oscillations not being dependent on the stimulation frequency, it is clear that electrical stimulation initiates the Ca2+ oscillations and also plays a part in maintaining cytosolic Ca2+ in these cells, as cessation of electrical stimulation caused a decrease in cytosolic Ca2+ back to baseline levels and abolished the Ca2+ oscillations (Figure 1(e)). Additionally, all cells recorded displayed an increase in cytosolic Ca2+ in response to electrical stimulation. We did not observe spontaneous Ca2+ oscillations in these cells under our recording conditions as has been previously reported, and the amplitude of our electrically induced oscillations is approximately 4–6 times greater than that reported for spontaneous Ca2+ oscillations [32].
Figure 1.
Whole-cell Ca2+ oscillations in electrically stimulated CPCs. (a) 2D fluorescent image of child CPCs loaded with fluo-4/AM. Fluo-4/AM-loaded hcCPCs were electrically stimulated at 0.5 Hz (blue) or 1 Hz (orange). Representative recordings of Ca2+ oscillations are shown in (b). The arrow indicates the start of electrical stimulation. The amplitude (ΔF/F 0) and frequency (oscillations/minute) of the oscillations are summarized in (c) and (d), respectively. (e) Representative recording of cytosolic Ca2+ before, during, and after 0.5 Hz electrical stimulation. The bar above the trace shows the time during the recording when electrical stimulation was applied. Data in (e) represent mean ± SD. No significance was found by Student's t-test. n = 14 cells from 4 different pools of cells for all measurements.
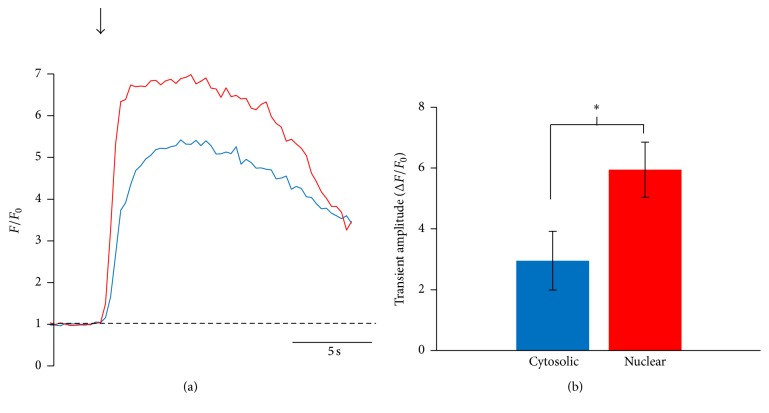
The amplitude of nuclear Ca2+ oscillations was also measured in electrically stimulated CPCs and these oscillations were of significantly higher amplitude than the corresponding cytosolic Ca2+ oscillations. Figure 2(a) shows representative traces of nuclear and cytosolic Ca2+ oscillations taken from the same cell and aligned in time. These data are summarized in Figure 2(b). Our finding that nuclear Ca2+ oscillations were of significantly higher amplitude than cytosolic Ca2+ oscillations may indicate a possible role for the increased nuclear Ca2+ in regulation of Ca2+-dependent proteins and transcription factors leading to differentiation and lineage commitment of CPCs. Activation of Ca2+ signaling by electrical stimulation has been shown to cause changes in the phenotype and genotype in multiple types of adult progenitor cells [19–22]. We did not observe spontaneous Ca2+ release events (Ca2+ waves or Ca2+ sparks) in unstimulated cells under our experimental conditions nor did the imaging laser activate Ca2+ release events. Together, these data show that electrical stimulation of CPCs elicits a robust cytosolic and nuclear Ca2+ response from these cells.
Figure 2.
Nuclear Ca2+ increases more than cytosolic Ca2+ in response to electrical stimulation. Fluo-4/AM-loaded hcCPCs were stimulated at 0.5 Hz and the amplitudes of the nuclear and cytosolic Ca2+ oscillations were analyzed. Representative traces of nuclear (red) and cytosolic (blue) Ca2+ oscillations are shown in (a), and amplitudes are summarized in (b). Data represent mean ± SD. ∗ p < 0.05; Student's t-test. n = 16 cells from 4 different pools of cells for all points.
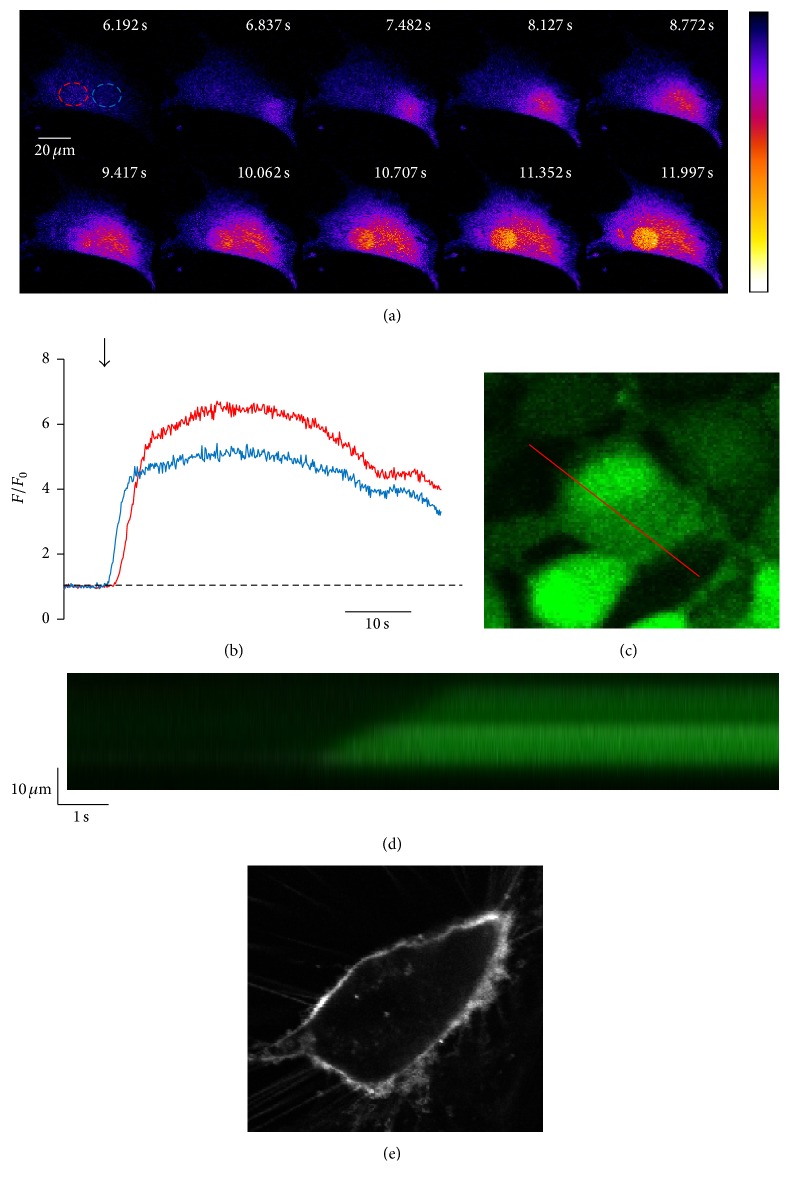
3.2. Ca2+ Oscillations Propagate in a Wave-Like Fashion in CPCs
The Ca2+ oscillations were further analyzed by two-dimensional and high-speed line scan confocal imaging to determine the spatiotemporal properties of Ca2+ oscillations in CPCs. Figure 3(a) shows a representative 2D high-speed confocal image montage of the activation of a Ca2+ oscillation in a CPC. Interestingly, Ca2+ release begins in a focal region in the periphery of the cell and then propagates in a wave-like fashion through the cytosol and the nucleus. Fluorescent traces from a cytosolic region (blue) and the nucleus (red) are shown in Figure 3(b). As shown in the traces, the cytosolic Ca2+ in the region near the site of Ca2+ release activation increases first (blue trace), and the Ca2+ signal propagates outward through the cytosol and eventually reaches the nucleus and an increase in the nuclear Ca2+ is seen (red trace). Again, a larger nuclear Ca2+ oscillation compared to the cytosolic Ca2+ oscillation can be seen in these traces, with the red nuclear trace reaching a higher amplitude than that of the blue cytosolic trace. These traces show the spatiotemporal heterogeneity of Ca2+ release activated by electrical stimulation in CPCs and show that the Ca2+ oscillations in these cells propagate in a wave-like fashion, initiating at the periphery of the cell and propagating through the cytosol and nucleus.
Figure 3.
Ca2+ oscillations in electrically stimulated CPCs show spatial heterogeneity and propagate in a wave-like fashion. ((a) and (b)) Representative 2D high-speed confocal image montage of the activation of a Ca2+ oscillation in a CPC loaded with fluo-4/AM. ROIs (red: nuclear, blue: cytosolic) indicated in (a) are graphed in (b). ((c) and (d)) Measured from the red line shown in (c), the confocal line scan in (d) shows that initiation of Ca2+ release at one edge of the cell propagates through the cell to the other side. (e) Representative image of a CPC stained with Di-8-ANEPPS.
Confocal line scans were used to confirm our 2D data described above. Figure 3(c) shows the placement of the line for recording, and Figure 3(d) is the resulting line scan. This scan is representative of 12 trials. As shown, the Ca2+ release activated by electrical stimulation starts at the periphery of the cell and propagates across the line in a wave-like fashion over time. We also looked for cell membrane invaginations that may identify preferential sites in the CPC similar to transverse tubules (T-tubules) in adult ventricular myocytes. T-tubules are invaginations of the sarcolemmal membrane in cardiac myocytes that bring the surface membrane in close proximity to the sarcoplasmic reticulum (SR) membrane allowing for efficient coupling of Ca2+ entry through sarcolemmal L-type Ca2+ channels and activation of intracellular Ca2+ release by ryanodine receptors on the SR [33]. Staining of CPCs with the membrane dye Di-8-ANEPPS did not reveal any invaginations of the surface membrane indicating that this feature did not contribute to Ca2+ release activation in CPCs (Figure 3(e)). In summary, the electrically induced Ca2+ release in CPCs very much resembles Ca2+ wave propagation in adult ventricular myocytes [34]. Despite their activation in the general periphery of the cell, they do not appear to be activated in any more localized preferential sites within the cell or at the same region in the periphery in subsequent Ca2+ oscillations. Consistent with the finding that there were no preferential sites of Ca2+ release during electrical stimulation, we did not find evidence of T-tubules which have been shown to be preferential release sites in ventricular myocytes [33]. We hypothesize that Ca2+ release initiation occurs at the periphery of the cell where the cell membrane and endoplasmic reticulum may be closest together to facilitate effective coupling Ca2+ entry to activation of intracellular Ca2+ release.
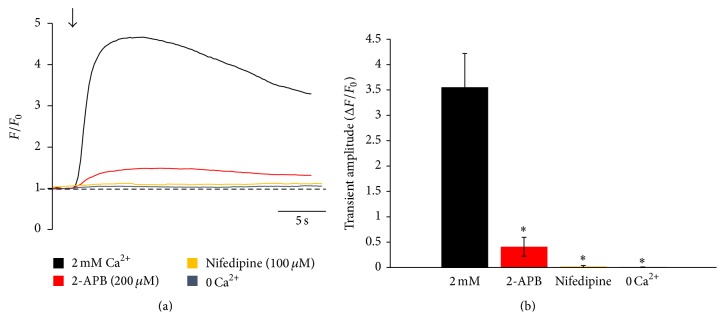
3.3. The L-Type Ca2+ Channel and the Inositol 1,4,5-Trisphosphate Receptor Are Implicated in Ca2+ Release in CPCs in Response to Electrical Stimulation
In order to determine the proteins involved in the activation of Ca2+ release in CPCs, we used specific inhibitors of key Ca2+ handling proteins prior to electrical stimulation and also performed immunocytochemistry to confirm the expression of these proteins. Due to the fact that these cells readily responded to electrical stimulation, the voltage-dependent L-type Ca2+ channel (LTCC) was our first candidate for the protein mediating the response of CPCs to electrical stimulation. Pretreatment of cells for 5 min with the LTCC inhibitor nifedipine nearly abolished electrically induced increases in cytosolic Ca2+ in all cells recorded, suggesting that electrically induced Ca2+ oscillations in CPCs are dependent on the activity of the voltage-dependent LTCC (Figure 4). In adult cardiac myocytes, entry of Ca2+ into the cytosol through the LTCC in response to electrical stimulation initiates massive Ca2+ release from sarcoplasmic reticulum Ca2+ store through the ryanodine receptor (RyR). To determine whether the same process was present in CPCs, we first tested the necessity of extracellular Ca2+ for electrically induced Ca2+ oscillations in CPCs. Bathing the cells for 5 min prior to recording in an external solution without Ca2+ (0 Ca2+) prevented electrically induced Ca2+ release in CPCs (Figure 4). Pretreatment of the cells for 5 min with tetracaine, a RyR inhibitor, did not prevent electrically induced Ca2+ release in our CPCs (data not shown); however, pretreatment for 5 min with 2-aminoethoxydiphenyl borate (2-APB), an inositol 1,4,5-trisphosphate receptor (IP3R) inhibitor, significantly decreased the amplitude of electrically induced Ca2+ release (Figure 4). The IP3R is another intracellular Ca2+ release channel found in adult cardiac myocytes and has also been shown to mediate spontaneous Ca2+ release in multiple types of stem cells including CPCs [32, 35], and 2-APB has been shown to be an inhibitor of IP3R function, albeit a nonspecific one.
Figure 4.
Cycling of Ca2+ in CPCs in response to electrical stimulation is dependent on the LTCC, IP3R, and external Ca2+. (a) Representative Ca2+ oscillations recorded from fluo-4/AM-loaded CPCs at 0.5 Hz electrical stimulation in 2 mM Ca2+ Tyrode's solution, pretreated with nifedipine or 2-APB to inhibit the LTCC or IP3R, respectively, or in 0 Ca2+ Tyrode's solution. Traces have been aligned in time based on when electrical stimulation was applied for comparison. Arrow indicates the start of stimulation. (b) Summary bar graph of Ca2+ oscillation amplitudes under the various recording conditions in (a). Data represent mean ± SD. ∗ p < 0.05; Student's t-test. n = 16 cells from 4 different pools of cells for all points.
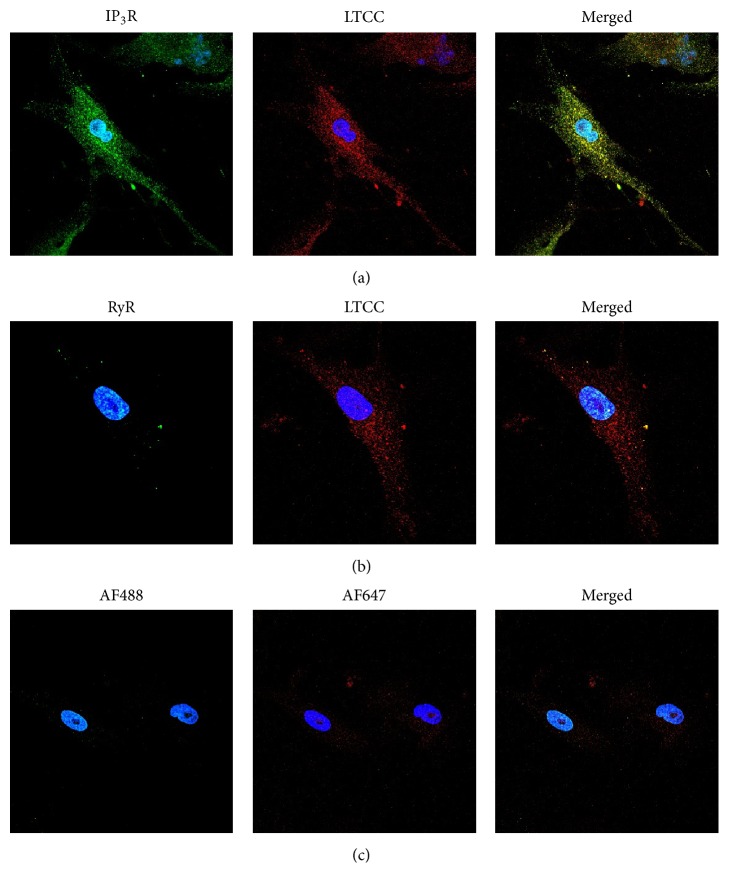
Immunocytochemistry confirmed the presence of the LTCC and the IP3R in CPCs, while no RyR was detected consistent with our functional studies (Figure 5). In summary, these data suggest that the LTCC and the IP3R are key proteins in electrically induced Ca2+ oscillations from human CPCs and represent a previously undescribed pathway for the activation of Ca2+ signaling in these cells; however, more experiments are necessary to confirm these results in human CPCs.
Figure 5.
Immunostaining of CPCs shows expression and localization of the LTCC and IP3R. CPCs were fixed, permeabilized, and incubated with primary antibodies against the L-type Ca2+ channel (LTCC, Cav2.1 subunit), type 2 inositol 1,4,5-trisphosphate receptor (IP3R), or type 2 ryanodine receptor (RyR). Cells were then incubated with either Alexa Fluor 488 (IP3R and RyR; green) or Alexa Fluor 647 (LTCC; red). Nuclei are stained with DAPI (blue). Expression of the IP3R and LTCC is shown in (a), while expression of the LTCC and the RyR is shown in (b). Cells were also incubated with only secondary antibodies to determine nonspecific binding in (c). Images are representative of 3 replicates.
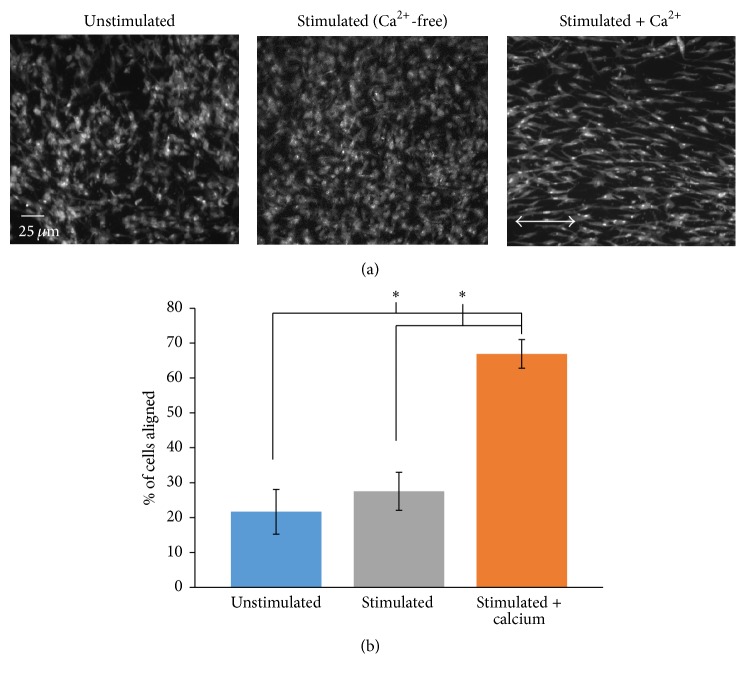
3.4. Long-Term Culture Stimulation Induces CPC Alignment
Anisotropy of cardiac tissue is a key characteristic of the structure and function of the heart that facilitates electrical and mechanical activation of the myocardium. Alignment of cells organizes them into a tissue-like structure and has been shown to improve the differentiation of stem cells [36]. Therefore, we sought to determine whether long-term culture stimulation would induce this phenotypic change in CPCs. CPCs were cultured in stimulation media and subjected to 72 hrs of electrical stimulation. CPCs were also plated in stimulation media and cultured for 72 hrs without electrical stimulation to serve as an unstimulated control or stimulated in Ca2+-free media to serve as a stimulation control. Cells were fixed, permeabilized, incubated with 10 μg/mL fluorescein-5-maleimide, and imaged. Representative images of unstimulated and stimulated CPCs are shown in Figure 6(a) and a summary graph of the quantified alignment scores is shown in Figure 6(b). Nearly 50% increase in the percent of cells aligned parallel to the electrical field was seen after 72 hrs of electrical stimulation compared to unstimulated cells or compared to stimulated cells in Ca2+-free media. These data illustrate an important phenotypic change induced in CPCs with chronic electrical stimulation and also indicated that this change is dependent on the presence of extracellular Ca2+. Our results showing that long-term culture stimulation induces Ca2+-dependent anisotropy in CPCs are important for the tissue architecture necessary for proper alignment of the cells in a tissue-like structure to prevent electrical conduction abnormalities, impaired pump function, or arrhythmias upon CPC implantation.
Figure 6.
Electrically induced alignment of CPCs. CPCs were plated in stimulation media and subjected to electrical stimulation in culture for 72 hrs (stimulated + Ca2+). As controls, CPCs were plated in stimulation media and cultured for 72 hrs without electrical stimulation (unstimulated) or in Ca2+-free media and subjected to electrical stimulation (stimulated). All groups were fixed, permeabilized, and incubated with fluorescein-5-maleimide. Representative images of cells from the three groups are shown in (a). Summary bar graph of cellular alignment for the three culture conditions is shown in (b). Arrow in (a) (stimulated + Ca2+) is the direction of the electrical field. Data in (b) represent mean ± SD. ∗ p < 0.05; Student's t-test; n = 8 replicates.
4. Conclusions
With Ca2+ handling linked, directly or indirectly, to almost all properties of cardiomyocytes including excitation-contraction coupling and excitation-transcription coupling, a solid understanding of this process in CPCs is crucial for fully realizing the cardiac therapeutic potential of these cells given recent studies that have shown that these cells do not significantly contribute to cardiac myocyte replenishment in vivo [4–6]. In this study, we have identified a novel property of human c-kit+ cardiac progenitor cells to respond to electrical stimulation by initiating intracellular Ca2+ oscillations. CPCs were isolated from human pediatric patients and pooled from multiple donors to diminish the effects of patient variability in our experiments. The use of human CPCs gives relevance to our findings for translation into a novel therapeutic strategy for clinical use, and our ability to perform live cell recordings of cytosolic Ca2+ in electrically stimulated CPCs represents a novel approach to understanding the physiology of these cells. As we have shown in this work, pediatric CPCs possess a broad spectrum of functional molecular elements of Ca2+ signaling. Ca2+-dependent regulatory mechanisms can be supposed to influence their differentiation potential, and we speculate that electrical stimulation activates a Ca2+-dependent signaling pathway in which the increased intracellular Ca2+ activates transcription of cardiospecific genes. In summary, we have characterized the electrically induced Ca2+ signal in CPCs by measuring the amplitude of cytosolic and nuclear Ca2+ oscillations elicited by electrical stimulation, identified the mechanism by which Ca2+ oscillations initiate and propagate throughout the cells, and also determined the key proteins involved in this process. Since our experiments were done in human pediatric CPCs, our results may be specific to that population of cells, and further experiments will be necessary to determine whether our results are species- or age-dependent [37]. To our knowledge, this is the first study to have reported the functional effect of acute ex vivo electrical stimulation on human CPCs. This study furthers our understanding of CPC physiology and may be used to direct future therapeutic strategies with these cells.
Acknowledgments
The authors wish to acknowledge the support of the Children's Miracle Network gift to Children's Healthcare of Atlanta. The authors also wish to acknowledge the generous support of Ms. Katrina Ceccoli and the Darryll M. Ceccoli Research Fund, as well as Keilani and Brian Betkowski and the Betkowski Pediatric Research Fund. This work was also supported by federal funds from the National Heart, Lung, and Blood Institute HL088488 to Mary B. Wagner as well as American Heart Association Grant 11GRNT7490000 to Mary B. Wagner.
Abbreviations
- CPC:
Cardiac progenitor cell
- Ca2+:
Calcium
- LTCC:
L-type Ca2+ channel
- RyR:
Ryanodine receptor
- IP3R:
Inositol 1,4,5-trisphosphate receptor.
Competing Interests
The authors declare no potential competing interests.
Authors' Contributions
Joshua T. Maxwell and Michael E. Davis were responsible for conception and design of the experiments. Collection, analysis, and interpretation of data were carried out by Joshua T. Maxwell, Mary B. Wagner, and Michael E. Davis. Joshua T. Maxwell drafted the article. All authors have approved the final version of the manuscript.
References
- 1.Beltrami A. P., Barlucchi L., Torella D., et al. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell. 2003;114(6):763–776. doi: 10.1016/S0092-8674(03)00687-1. [DOI] [PubMed] [Google Scholar]
- 2.Magenta A., Avitabile D., Pompilio G., Capogrossi M. C. c-kit-positive cardiac progenitor cells: the heart of stemness. Circulation Research. 2013;112(9):1202–1204. doi: 10.1161/circresaha.113.301317. [DOI] [PubMed] [Google Scholar]
- 3.Keith M. C. L., Bolli R. ‘String theory’ of c-kitpos cardiac cells: a new paradigm regarding the nature of these cells that may reconcile apparently discrepant results. Circulation Research. 2015;116(7):1216–1230. doi: 10.1161/circresaha.116.305557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Q., Yang R., Huang X., et al. Genetic lineage tracing identifies in situ Kit-expressing cardiomyocytes. Cell Research. 2016;26(1):119–130. doi: 10.1038/cr.2015.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sultana N., Zhang L., Yan J., et al. Resident c-kit+ cells in the heart are not cardiac stem cells. Nature Communications. 2015;6, article 8701 doi: 10.1038/ncomms9701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Berlo J. H., Kanisicak O., Maillet M., et al. C-kit+ cells minimally contribute cardiomyocytes to the heart. Nature. 2014;509(7500):337–341. doi: 10.1038/nature13309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Berlo J. H., Kanisicak O., Maillet M., et al. c-kit+ cells minimally contribute cardiomyocytes to the heart. Nature. 2014;509(7500):337–341. doi: 10.1038/nature13309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orlic D., Kajstura J., Chimenti S., et al. Bone marrow cells regenerate infarcted myocardium. Nature. 2001;410(6829):701–705. doi: 10.1038/35070587. [DOI] [PubMed] [Google Scholar]
- 9.Dai Y., Xu M., Wang Y., Pasha Z., Li T., Ashraf M. HIF-1α induced-VEGF overexpression in bone marrow stem cells protects cardiomyocytes against ischemia. Journal of Molecular and Cellular Cardiology. 2007;42(6):1036–1044. doi: 10.1016/j.yjmcc.2007.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fischer K. M., Cottage C. T., Wu W., et al. Enhancement of myocardial regeneration through genetic engineering of cardiac progenitor cells expressing pim-1 kinase. Circulation. 2009;120(21):2077–2087. doi: 10.1161/CIRCULATIONAHA.109.884403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haider H. K., Sim E. K. W., Lei Y., Ashraf M. Cell-based ex vivo delivery of angiogenic growth factors for cardiac repair. Arteriosclerosis, Thrombosis, and Vascular Biology. 2005;25(12, article e144) doi: 10.1161/01.atv.0000190665.72652.d7. [DOI] [PubMed] [Google Scholar]
- 12.Mangi A. A., Noiseux N., Kong D., et al. Mesenchymal stem cells modified with Akt prevent remodeling and restore performance of infarcted hearts. Nature Medicine. 2003;9(9):1195–1201. doi: 10.1038/nm912. [DOI] [PubMed] [Google Scholar]
- 13.Noiseux N., Gnecchi M., Lopez-Ilasaca M., et al. Mesenchymal stem cells overexpressing Akt dramatically repair infarcted myocardium and improve cardiac function despite infrequent cellular fusion or differentiation. Molecular Therapy. 2006;14(6):840–850. doi: 10.1016/j.ymthe.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Christoforou N., Gearhart J. D. Stem cells and their potential in cell-based cardiac therapies. Progress in Cardiovascular Diseases. 2007;49(6):396–413. doi: 10.1016/j.pcad.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Deb K., Sarda K. Human embryonic stem cells: preclinical perspectives. Journal of Translational Medicine. 2008;6, article 7 doi: 10.1186/1479-5876-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gnecchi M., He H., Noiseux N., et al. Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. FASEB Journal. 2006;20(6):661–669. doi: 10.1096/fj.05-5211com. [DOI] [PubMed] [Google Scholar]
- 17.Haider H. K., Ashraf M. Strategies to promote donor cell survival: combining preconditioning approach with stem cell transplantation. Journal of Molecular and Cellular Cardiology. 2008;45(4):554–566. doi: 10.1016/j.yjmcc.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gautam M., Fujita D., Kimura K., et al. Transplantation of adipose tissue-derived stem cells improves cardiac contractile function and electrical stability in a rat myocardial infarction model. Journal of Molecular and Cellular Cardiology. 2015;81:139–149. doi: 10.1016/j.yjmcc.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 19.Llucià-Valldeperas A., Sanchez B., Soler-Botija C., et al. Electrical stimulation of cardiac adipose tissue-derived progenitor cells modulates cell phenotype and genetic machinery. Journal of Tissue Engineering and Regenerative Medicine. 2015;9(11):E76–E83. doi: 10.1002/term.1710. [DOI] [PubMed] [Google Scholar]
- 20.Llucià-Valldeperas A., Sanchez B., Soler-Botija C., et al. Physiological conditioning by electric field stimulation promotes cardiomyogenic gene expression in human cardiomyocyte progenitor cells. Stem Cell Research and Therapy. 2014;5(4, article 93) doi: 10.1186/scrt482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pietronave S., Zamperone A., Oltolina F., et al. Monophasic and biphasic electrical stimulation induces a precardiac differentiation in progenitor cells isolated from human heart. Stem Cells and Development. 2014;23(8):888–898. doi: 10.1089/scd.2013.0375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Serena E., Figallo E., Tandon N., et al. Electrical stimulation of human embryonic stem cells: cardiac differentiation and the generation of reactive oxygen species. Experimental Cell Research. 2009;315(20):3611–3619. doi: 10.1016/j.yexcr.2009.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hotchkiss A., Feridooni T., Zhang F., Pasumarthi K. B. S. The effects of calcium channel blockade on proliferation and differentiation of cardiac progenitor cells. Cell Calcium. 2014;55(5):238–251. doi: 10.1016/j.ceca.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 24.Che H., Li G., Sun H.-Y., Xiao G.-S., Wang Y., Li G.-R. Roles of store-operated Ca2+ channels in regulating cell cycling and migration of human cardiac c-kit+ progenitor cells. American Journal of Physiology—Heart and Circulatory Physiology. 2015;309(10):H1772–H1781. doi: 10.1152/ajpheart.00260.2015. [DOI] [PubMed] [Google Scholar]
- 25.Quijada P., Hariharan N., Cubillo J. D., et al. Nuclear calcium/calmodulin-dependent protein kinase II signaling enhances cardiac progenitor cell survival and cardiac lineage commitment. The Journal of Biological Chemistry. 2015;290(42):25411–25426. doi: 10.1074/jbc.m115.657775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.French K. M., Davis M. E. Isolation and expansion of C-Kit-positive cardiac progenitor cells by magnetic cell sorting. Methods in Molecular Biology. 2014;1181:39–50. doi: 10.1007/978-1-4939-1047-2_4. [DOI] [PubMed] [Google Scholar]
- 27.Schindelin J., Arganda-Carreras I., Frise E., et al. Fiji: an open-source platform for biological-image analysis. Nature Methods. 2012;9(7):676–682. doi: 10.1038/nmeth.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boopathy A. V., Che P. L., Somasuntharam I., et al. The modulation of cardiac progenitor cell function by hydrogel-dependent Notch1 activation. Biomaterials. 2014;35(28):8103–8112. doi: 10.1016/j.biomaterials.2014.05.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gray W. D., French K. M., Ghosh-Choudhary S., et al. Identification of therapeutic covariant microRNA clusters in hypoxia-treated cardiac progenitor cell exosomes using systems biology. Circulation Research. 2015;116(2):255–263. doi: 10.1161/CIRCRESAHA.116.304360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Padin-Iruega M. E., Misao Y., Davis M. E., et al. Cardiac progenitor cells and biotinylated insulin-like growth factor-1 nanofibers improve endogenous and exogenous myocardial regeneration after infarction. Circulation. 2009;120(10):876–887. doi: 10.1161/CIRCULATIONAHA.109.852285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pendergrass K. D., Boopathy A. V., Seshadri G., et al. Acute preconditioning of cardiac progenitor cells with hydrogen peroxide enhances angiogenic pathways following ischemia-reperfusion injury. Stem Cells and Development. 2013;22(17):2414–2424. doi: 10.1089/scd.2012.0673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferreira-Martins J., Rondon-Clavo C., Tugal D., et al. Spontaneous calcium oscillations regulate human cardiac progenitor cell growth. Circulation Research. 2009;105(8):764–774. doi: 10.1161/CIRCRESAHA.109.206698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franzini-Armstrong C., Protasi F., Ramesh V. Comparative ultrastructure of Ca2+ release units in skeletal and cardiac muscle. Annals of the New York Academy of Sciences. 1998;853:20–30. doi: 10.1111/j.1749-6632.1998.tb08253.x. [DOI] [PubMed] [Google Scholar]
- 34.Maxwell J. T., Blatter L. A. Facilitation of cytosolic calcium wave propagation by local calcium uptake into the sarcoplasmic reticulum in cardiac myocytes. The Journal of Physiology. 2012;590(23):6037–6045. doi: 10.1113/jphysiol.2012.239434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kapoor N., Maxwell J. T., Mignery G. A., Will D., Blatter L. A., Banach K. Spatially defined InsP3-mediated signaling in embryonic stem cell-derived cardiomyocytes. PLoS ONE. 2014;9(1) doi: 10.1371/journal.pone.0083715.e83715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pijnappels D. A., Schalij M. J., Ramkisoensing A. A., et al. Forced alignment of mesenchymal stem cells undergoing cardiomyogenic differentiation affects functional integration with cardiomyocyte cultures. Circulation Research. 2008;103(2):167–176. doi: 10.1161/CIRCRESAHA.108.176131. [DOI] [PubMed] [Google Scholar]
- 37.Agarwal U., Smith A. W., French K. M., et al. Age-dependent effect of pediatric cardiac progenitor cells after juvenile heart failure. Stem Cells Translational Medicine. 2016;5(7):883–892. doi: 10.5966/sctm.2015-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]