Abstract
Objective An exploratory study has been carried out to examine decision‐making role preferences and information needs for a sample of people with colorectal cancer (n=48). The work replicated a larger study carried out for women with breast cancer (n=150), and this paper compares and contrasts findings for both disease groups.
Design A cross‐sectional design was employed, involving structured interviews. The main variables investigated were decision‐making preference (using a decisional role preference card sort), perceived decisional role and information need (using an information needs questionnaire).
Results The majority (78%) of the colorectal cancer patients preferred to play a passive role in decision making, in contrast to 52% of women with breast cancer in previous work. Eighty per cent of the colorectal sample and 61% of the women with breast cancer perceived that the doctor had made treatment decisions. Priority information needs for both groups related to cure, spread of disease and treatment options.
Conclusions The two most striking findings from the comparison between the two disease groups relate to the differences in decision‐making role preferences and the similarities in information needs. The process of involving people with colorectal cancer in treatment decision making warrants further investigation. The similarity in information needs of the two disease groups has implications for health care professionals providing information to people with cancer.
Keywords: breast cancer, colorectal cancer, decision making, information needs, patient participation
Background
Colorectal cancer is the second most common cause of cancer death in the UK, but the disease has not achieved as high a public or political profile as other conditions, such as breast cancer, and as yet the UK has no national screening programme for early detection. Recent guidelines on the management of colorectal cancer acknowledge that there is less clarity of research evidence for effective management than for breast cancer. 1 Breast cancer presents to health services via easy‐to‐define routes, normally by GP referral or breast screening, and primary management is almost always surgical. However, colorectal cancer presents in more varied ways, including emergency admissions, and in‐patient and GP referrals. Current management of colorectal cancer primarily involves surgery (in approximately 80% of cases) aimed at improving long‐term survival and reducing recurrence. 1 Radiotherapy and chemotherapy are also given as adjuvant or palliative treatments, although it is reported that they are offered to only a minority of patients. 1
While colorectal cancer guidelines support patients being involved in treatment decisions and being given full information, they are less clear‐cut than the more definitive guidelines for involving women with breast cancer in decision making. 1 , 2 For breast cancer the treatment options centre primarily around the type of surgery, and may be fairly well defined with no impact on survival. Guidelines state that surgical options can include mastectomy or breast‐conserving surgery, that all patients should be fully informed of all the options and their potential risks, and that choices should be made jointly between the surgeon and the patient. 2 If the management of colorectal cancer is not clearly defined, then there may be difficulties in clearly articulating the various options available, the different outcomes that may ensue and the potential impact on quality of life. However, it has been argued that in this situation there is an even stronger case for incorporating patients’ preferences in the decision‐making process. 3
Presenting patients with treatment choices has been shown to have positive benefit in reducing psychological morbidity. 4 , 5 If it is accepted that patient participation in decision making is beneficial and to be encouraged, with a shift away from paternalism towards sharing partnerships, then it is important to discover how patients feel about their involvement in the decision‐making process. Despite recommendations that people with colorectal cancer be given clear information about their disease and treatment options, 1 and the increasing trend for involving service users in the decision‐making process, there is little in the literature to indicate the preferences for involvement in decision making for this patient group.
To date there is some evidence, mainly from the USA, that patients do want to be actively involved in decisions concerning their care and treatment. 6 , 7, –8 However, more recent evidence from the UK and Canada indicates that active engagement in the decision‐making process is not a role that all patients feel comfortable adopting, and certainly for women with breast cancer, men with prostate cancer and renal patients, the doctor has been preferred as the primary decision maker. 9 , 10, –11 For Canadian women with breast cancer a shared partnership with the doctor has been indicated as the preferred decision‐making role. 12
In engaging service users in the decision‐making process, it may be acceptable to view a preference for a passive role as an autonomous choice in that individuals may be deciding not to decide. Alternatively, it may be that individuals who are not presented with choices and who do not have expectations of being involved in decision making may well prefer a passive role because they are unaware of alternative roles.
Any decisions that patients make about treatment can only be as sound as the information on which they are based. Individuals may want information but may not wish to use that information to make decisions. Wanting information is a rather vague expression of need, which does not aid the busy health care professional with limited time to discuss care and treatment. It may be helpful to know the specific types of information that are required at a particular point in time: that is, priority information needs. Previous work with women with breast cancer, conducted in the UK and Canada, has indicated the priority information needs around the time of diagnosis and at follow‐up stages. 12 , 13, –14 However, there is little in the literature to indicate the priority information needs of people with colorectal cancer.
It may be hypothesized that people with colorectal cancer will have different information needs from women with breast cancer, owing to differences in the nature of the illness. Although risk factors such as age, genetic inheritance, early menarche and nulliparity have been indicated in breast cancer, these factors are essentially non‐preventable. The situation is rather different for colorectal cancer, for which a diet high in fat and calories and low in fibre has been implicated as a causal factor. It may be expected that information on diet and lifestyle would be of interest to people with colorectal cancer in terms of preventing further disease.
Taking into account these potential differences, it seemed important to explore the concepts of decision‐making role preferences and information needs in this under‐researched group, and to compare and contrast the findings to those of previous work with women with breast cancer, in order that health care professionals can more usefully tailor information to individual need.
Objectives
The aim of the study was to determine the decision‐making role preferences and information needs for a sample of people with colorectal cancer, and to compare the findings to previous work conducted with women with breast cancer. 9 , 13 , 14 This was a small exploratory study, which also aimed to investigate whether measures utilized in previous work with women with breast cancer could be transferred and used successfully with people with colorectal cancer.
Design
A cross‐sectional design was employed, and a convenience sample of people diagnosed with colorectal cancer was taken from one consultant’s practice at a large university teaching hospital. Following ethical committee approval, suitable individuals were approached in an out‐patient clinic that catered for a range of disease stages from pre‐diagnosis to post‐treatment follow‐up, and asked to consent to one interview. Individuals were identified by reference to medical notes, the specialist consultant and a specialist nurse who provided information on individuals who met the entry criteria. The entry criteria included: an adult (at least 18 years old) with a known first‐time diagnosis of colorectal cancer and an understanding of written and spoken English. Resources were not available to provide interpreters and translations for the measures. Individuals were not approached if physical or psychological impairment was considered to be such that it would make the interview process stressful for the participant. A researcher attended out‐patient clinics each week and approached individuals who met the entry criteria in a consecutive manner: that is, the next available person was asked to consent to interview. Unfortunately, this entailed some individuals who met the entry criteria being lost to the researcher, but it was considered insensitive to ask people to delay their departure from the clinic in order to wait for the researcher to conclude an interview that was in progress. In total 48 patients participated in the study.
An interview schedule was designed for the study, which included socio‐demographic questions such as age, gender, education and occupation (used to derive social class), and included questions on the type of treatment planned or received.
Decision‐making role preferences
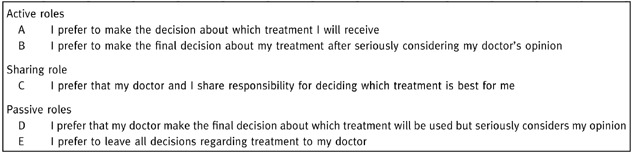
To establish decision‐making role preferences, a card‐sort technique was used that had been developed in Canada 15 and used successfully in British and Canadian women with breast cancer. 9 , 12 The role preferences card sort consists of five cards, each representing a potential role that can be played in treatment decision making (Box 1). The roles range from preferring active involvement (cards A and B), through sharing (card C) to more passive roles where the doctor is the decision maker (cards D and E). A random order presentation was utilized and cards were presented two at a time. On each occasion individuals were asked to state a preference between the two presented cards. This continued until a preference order over all five roles was established. For example, someone with the preference order ABCDE would want a very active role in decision making, whereas someone who chose EDCBA would want a very passive role. A sample size estimation was made using the arcus © (Medical Computing, UK), statistical package based on current numbers of people with colorectal cancer being treated at the study site and previous findings for decision‐making role preferences in which 48% of women with breast cancer preferred some degree of involvement in treatment decision making. 9 To detect a difference of 10% from previous findings (95% power, 5% significance level), the arcus © program indicated that a minimum sample size of 44 would be required.
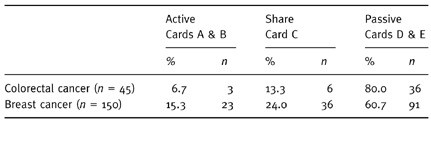
Table 1.
Box 1 The five decision‐making roles
Perceived role in decision making
The decision‐making card sort was also used to establish what role individuals perceived they had played in decision making. Individuals were asked to choose the one card that came closest to their actual involvement in the treatment decision‐making process. In this way, comparisons could be made between preferred and actual roles, indicating the discrepancy between what a person wanted and what they received in terms of decision‐making preference.
Information needs
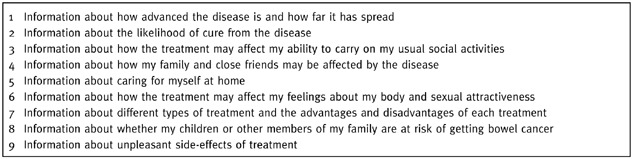
To establish priority information needs, nine items of information were presented to individuals in pairs in the form of an information needs questionnaire (INQ). The nine items represented physical, psychological and social aspects of care and treatment, and had been derived from a literature search. 16 Each of the nine items was seen with every other item to give a total of 36 pairs [n(n − 1)/2]. The pairs were presented such that selection bias was avoided. 17 Individuals were asked to state, for each pair of items, which of the two items had the greater importance at that particular moment in time. The measure had been used successfully in women with breast cancer in both the UK and Canada, 12 , 13, –14 , 18 but had not been used in colorectal cancer. It was therefore important to establish, following completion of the measure, whether individuals had information needs that were not included in the INQ. The INQ was adapted so that ‘bowel cancer’ replaced ‘breast cancer’. The nine items in the INQ are shown in Box 2 2.
Table 2.
Box 2 The nine items of information represented in the Information Needs Questionnaire (INQ)
Analysis
All data were initially entered into the data entry component of spss (SPSS, Chicago, IL, USA). Computer programs developed in Canada for SAS (SAS Institute, Cary, NC, USA) software were used to carry out the analysis on the decision‐making role preferences and INQ, working on portable files transferred from spss. 19 , 20
As the decision‐making card sort had not previously been used with a UK sample of people with colorectal cancer, it was important to revalidate the measure using the model that had been applied to the breast cancer data, 9 , 12 that is Coombs’ Unfolding Theory. 21 This psychological scaling model is based on the theory of preferential choice (i.e. one item is preferred over another item). The entire preference order (e.g. ABCDE) is used in the analysis to determine the amount of control over the decision‐making process that is preferred by each individual. The model aims to show an underlying dominant dimension of control, ranging from keeping control (active, cards A and B) through collaboration (sharing, card C) to giving away control (passive, cards D and E). There are 120 possible permutations of the five decisional role cards, but only 11 of these preferences are consistent with the main hypothesized dimension, ranging from ABCDE to EDCBA (ABCDE, BACDE, BCADE, BCDAE, CBDAE, CDBAE, CDBEA, CDEBA, DCEBA, DECBA, EDCBA). Coombs stated that 50% plus one of the preference orders would need to fall on to this main psychological dimension to establish validity and evidence of a unidimensional model. 21 By chance alone, 13% of preference orders could have fallen on to the hypothesized dimension. 15 Other necessary criteria include the presence of both ends of the dimension. For example, in the active–share–passive dimension the preference orders ABCDE and EDCBA would need to have been chosen by participants. Distributions of preferences are also reported based on the first choice of card in the preference order. For example, in the preference order ABCDE the first choice of card, and most preferred, is A (active).
To investigate the difference between preferred role (using the first choice of card in the preference order) and actual role, a discrepancy score was computed. Each decision‐making card from A to E was given a corresponding number from 1 to 5 (A=1, B=2, C=3, D=4, E=5) and the discrepancy score was equal to the preferred role minus the perceived role. Discrepancy scores ranged from –4 to +4 with a score of 0 indicating that an individual had achieved their preferred role (e.g. preferred E and received E, 5 − 5=0). Any score in the negative range indicated that an individual received a more passive role than they would have preferred, while any score in the positive range indicated that an individual received a more active role than they would have preferred.
Thurstone scaling techniques were applied to the information needs data as the INQ is compatible with Thurstone’s paired comparison approach, where individuals are asked to state a preference between only two items at any one time. 22 , 23 Analysis involves the construction of a series of matrices to reflect how often each individual item is preferred over another item. Frequency, proportions and unit deviate matrices are produced from the data and scale values are derived from the mean of the unit deviate scores, so allowing each item of information to be ranked in order of perceived importance. T‐tests can be used to compare scale values from the information needs profiles across the two disease groups, colorectal and breast cancer.
Results
Findings are presented for the study involving people with colorectal cancer, and a comparison is made with previous work involving women with breast cancer. 9 , 13 , 14
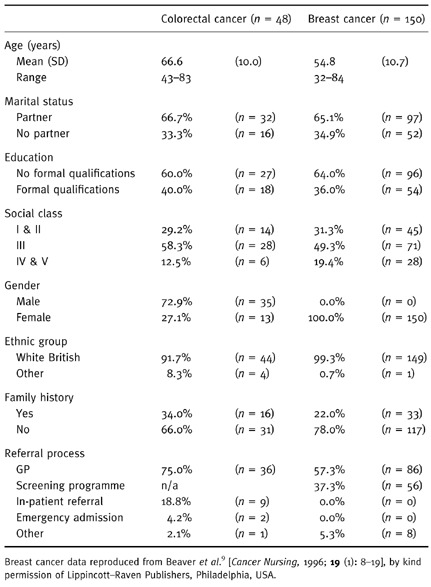
Sample characteristics are presented in Table 1. The mean age of the colorectal cancer group was higher (66.6 years) than that of the breast cancer group (54.8 years). In both disease groups a typical participant had a partner, had no formal qualifications, and was white British, from social class III, with no known family history of the disease. The referral process for the women with breast cancer had been via the GP and the national screening programme. For the colorectal cancer group, referral had been primarily by the GP with a small number of in‐patient referrals and two emergency admissions. One obvious difference between the groups relates to gender. All participants in the breast cancer study were women, while the majority of the colorectal cancer group were male (72.9%, n=35/48).
Table 1.
Characteristics of the colorectal cancer study group compared with the breast cancer group from previous work
Decision‐making role preferences
Forty‐six people completed the decision‐making card sort. For the colorectal cancer group 52.2% (24/46) of preference orders fell on the ABCDE–EDCBA dimension, just over the 50% plus one required to establish validity. However, 14 individuals (29%) had chosen the preference order EDCBA, the most passive order, and the opposite end of the dimension, ABCDE, was not represented.
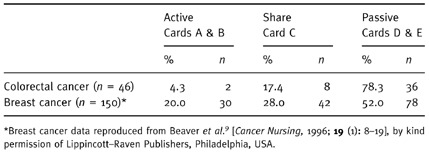
An examination of the distribution of preferences based on the first choice of card in the preference order indicated that 78.3% of the participants preferred the doctor to make the treatment decisions, compared with 52.0% for women with breast cancer (Table 2). Card E was the most popular first choice of card for 52.2% (n=24/46) of the individuals, and no individual chose card A as their most preferred role.
Table 2.
Distribution of decision making role preferences
Owing to the small sample sizes in the active and share cohorts, it was not possible to examine the impact of demographic variables on decision‐making role preferences.
Preferred and perceived decisional role
Forty‐five individuals completed the measure of perceived decision‐making role. The majority of the colorectal cancer group perceived that they had played a passive role in decision making (80.0%, n=36/45). This was also the perception of women with breast cancer, although not to the same extent (Table 3).
Table 3.
Perceived role
Findings indicated that the majority of the colorectal cancer group achieved their preferred role (60.0%, n=27/45) ( Fig. 1), whereas only 38.7% of women with breast cancer achieved their preferred role ( Fig. 2). There were a substantial number of women with breast cancer who would have preferred more involvement in the treatment decision‐making process (39.3%), whereas only 22.2% of the colorectal cancer group wanted more involvement.
Figure 1.
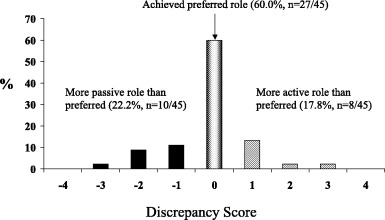
Discrepancy scores: colorectal cancer.
Figure 2.
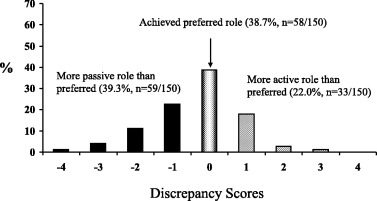
Discrepancy scores: breast cancer.
Information needs
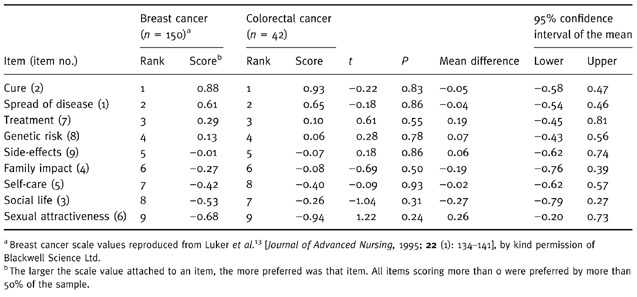
Although the INQ was presented to all 48 participants, some individuals were not able to complete the measure or only completed part of the measure. Those individuals who omitted more than five information needs pairs (n=6) were not included in subsequent analysis of the information needs data. Thurstone scaling analysis for 42 individuals indicated that the top three priority information needs related to likelihood of cure, spread of disease and treatment options. The item on sexual attractiveness was ranked in last place. Scale values for the two patient groups (breast and colorectal cancer) are compared in Table 4, indicating that for seven of the nine items the rankings were identical. The normal deviate scores from the Thurstone scaling analysis for the two patient groups were compared, and no significant differences between the rankings of the two patient groups were apparent (Table 4). The type of cancer did not have an impact on priority information needs.
Table 4.
Scale values derived from the INQ for colorectal and breast cancer
When the colorectal cancer group were asked if there were any other items of information that were important but had not been included in the INQ, seven individuals gave an affirmative response, although three comments related to treatment and one comment related to the impact on the family, items that were already included in the INQ. The remaining three comments included a need for information on support groups, finances and what foods to eat to prevent diarrhoea.
Discussion
The two most striking findings from the comparison between the two disease groups relate to the differences in decision‐making role preferences and the similarities in information needs. In previous work the Coombs Unfolding Model had shown the decision‐making card sort to be a valid and reliable measure of preferences. 9 , 12
However, it appeared that the colorectal cancer group were so passive in their preferences that the active end of the dimension was inappropriate. In contrast, while the majority of the women with breast cancer (52%) had preferred a passive role, there were still 20% who wanted active involvement and 28% who wanted to share the decision‐making responsibility. The facts that breast cancer has a high public and media profile and many women with breast cancer in the western world are activists may explain these findings to some extent.
It is interesting that a minority, in both disease groups, perceived that they had been involved in treatment choices. However, for the colorectal cancer group 60% had achieved their preferred role, primarily because they had wanted to play a passive role and that is the role they were allowed to play. While it is of course the right of an individual not to be involved in decision making if they do not wish to do so, in this situation the majority perceived that they had not been presented with treatment options. In contrast, only 39% of women with breast cancer had achieved their preferred role, with 39% wanting more involvement in the treatment decision‐making process. These findings may indicate that many women with breast cancer may benefit from being encouraged to be involved in the decision‐making process. However, for people with colorectal cancer the situation appears to be more complex.
Unfortunately, small sample sizes in the colorectal cancer group did not allow for an analysis of the impact of demographic factors on decision‐making role preference. Future work with larger samples would provide useful information on whether variables such as gender and age impacted on decision‐making role preference for this patient group. In addition, more exploratory work on the choices that are available to people with colorectal cancer and the way in which treatments are explained to individuals would enable a greater understanding of the treatment decision‐making process in this area. The studies described relied on the patients’ perceptions of choices being presented, and did not include the perception of the health care professionals involved. It would be interesting to know whether health care professionals also perceive that people with colorectal cancer are not involved in treatment choices.
The striking similarity between the information needs profiles for the two study groups implies that a diagnosis of cancer may bring with it information needs that are not specific to different disease conditions. Information on the likelihood of cure, spread of disease and treatment options was a priority for both groups. These information items have also been shown to be a priority for Canadian women with breast cancer and men with prostate cancer. 10 , 12
Information on sexual attractiveness was ranked in last place, an interesting finding in that both conditions can involve mutilating surgery in terms of mastectomy or stoma. Talking about such intimate subjects may be difficult for patients and health care professionals alike, and this may account for the low ranking of this item: that is, patients may wish to avoid a discussion of such sensitive subject matter. It may also be that information is not what is required, but rather some type of supportive care. It is not the intention to suggest that sexual attractiveness is not an important issue, but it may be that individuals are more concerned about other aspects of their care and treatment. Further investigation into why this item of information was ranked in last place is warranted.
Only three comments were made by the colorectal group on other items of information that should have been included in the INQ. This may indicate that the INQ may be used successfully with different cancer disease groups, and that there is a common element to cancer in terms of information needs that cuts across different disease conditions.
It is acknowledged that the profiles of information need relate to general profiles for the total study samples and not to individual profiles of need. It is not the intention to state that certain items of information were not important. All nine information needs were important, as evidenced by their presence in the INQ. The priority order was the issue, and obviously individual rankings will differ from the average overall ranking. The generation of individualized profiles would be a useful guide for health care professionals in enabling the communication process, and work on evaluating a touch‐screen computer system for establishing individual decision‐making role preferences and individual information needs profiles is currently underway in Canada. 24
Limitations
Small sample sizes in the colorectal cancer group do not allow the findings to be generalized. The colorectal cancer group were a cross‐section of people from early diagnosis to many years from diagnosis, whereas a longitudinal approach was adopted in the breast cancer study. This should be borne in mind when considering comparisons between the two studies. The colorectal cancer group was from one consultant’s practice, and this may have had an impact on decision‐making role preference. Individuals may have developed a trusting relationship with particular health care professionals, and may have deferred decision‐making responsibility for this reason.
In addition, provider styles were not considered. Interactions between patients and health care professionals were not directly observed, and it is not possible to comment on whether health care professionals perceived that choices were presented. Although observation‐based studies tend to be expensive and are usually small‐scale, the data from such studies could make a valuable addition to work in this area.
Conclusions
It may be rhetoric to talk about involving all patients in treatment decision making if some people do not want to make choices or if treatment choices are not presented. Involving patients in decision making is most certainly on the policy agenda, but it has been stated that implementation of this policy will need a sound research base. 3 There is a need for more research into the ways in which choices are presented to service users generally, and the actual choices available. If involving users in decision making, and encouraging their involvement, is to be advocated as best practice, because it has positive benefits, then more work will be needed to design innovative ways of enabling more active involvement.
Acknowledgements
We would like to express our thanks to Mr Paul Rooney and Ms Jane Randells for their co‐operation and advice during the course of this study.
References
- 1. NHS Executive. Improving Outcomes in Colorectal Cancer: The Manual. London: Cancer Guidance Sub‐group of the Clinical Outcomes Group, Department of Health, 1997.
- 2. NHS Executive . Improving Outcomes in Breast Cancer: The Manual. London: Cancer Guidance Sub‐group of the Clinical Outcomes Group, Department of Health, 1996.
- 3. Coulter A. Partnerships with patients: the pros and cons of shared clinical decision‐making. Journal of Health Services Research and Policy, 1997; 2 (2): 112 121. [DOI] [PubMed] [Google Scholar]
- 4. Davison BJ & Degner LF. Empowerment of men newly diagnosed with prostate cancer. Cancer Nursing, 1997; 20 (3): 187 196. [DOI] [PubMed] [Google Scholar]
- 5. Fallowfield LJ, Hall A, Maguire P, Baum M, A’Hern RP. Psychological effects of being offered a choice of surgery for breast cancer. British Medical Journal, 1994; 309 : 448 448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Blanchard CG, Labreque MS, Ruckdeschel JC, Blanchard EB. Information and decision‐making role preferences of hospitalized adult cancer patients. Social Science and Medicine, 1988; 27 : 1139 1145. [DOI] [PubMed] [Google Scholar]
- 7. Cassileth BR, Zupkis RV, Sutton‐Smith K, March V. Information and participation preferences among cancer patients. Annals of Internal Medicine, 1980; 92 : 832 836. [DOI] [PubMed] [Google Scholar]
- 8. Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making? Journal of the American Medical Association, 1984; 252 : 2990 2994. [PubMed] [Google Scholar]
- 9. Beaver K, Luker KA, Owens RG, Leinster SJ, Degner LF, Sloan JA. Treatment decision making in women newly diagnosed with breast cancer. Cancer Nursing, 1996; 19 (1): 8 19. [DOI] [PubMed] [Google Scholar]
- 10. Davison J, Degner LF, Morgan TR. Information and decision‐making preferences of men with prostate cancer. Oncology Nursing Forum, 1995; 22 (9): 1401 1408. [PubMed] [Google Scholar]
- 11. Caress AL & Luker KA. Patient‐sensitive treatment decision‐making? Preferences and perceptions in a sample of renal patients. Nursing Times Research, 1998; 3 (5): 364 372. [Google Scholar]
- 12. Degner LF, Kristjanson LJ, Bowman D et al. Information needs and decisional preferences in women with breast cancer. Journal of the American Medical Association, 1997; 277 (18): 1485 1492. [PubMed] [Google Scholar]
- 13. Luker KA, Beaver K, Leinster SJ, Owens RG, Degner LF, Sloan JA. The information needs of women newly diagnosed with breast cancer. Journal of Advanced Nursing, 1995; 22 (1): 134 141. [DOI] [PubMed] [Google Scholar]
- 14. Luker KA, Beaver K, Leinster SJ, Owens RG. The information needs of women with breast cancer: a follow up study. Journal of Advanced Nursing, 1996; 23 : 487 495. [DOI] [PubMed] [Google Scholar]
- 15. Degner LF & Sloan JA. Decision making during serious illness: what role do patients really want to play? Journal of Clinical Epidemiology, 1992; 45 : 941 950. [DOI] [PubMed] [Google Scholar]
- 16. Degner LF, Farber JM, Hack TF. Communication Between Cancer Patients and Health Care Professionals: an Annotated Bibliography. Winnipeg, Manitoba: National Cancer Institute of Canada, 1989.
- 17. Ross RT. Optimal orders in the method of paired comparisons. In: Maranell GM (ed.) Scaling: a Sourcebook for Behavioral Scientists. Chicago: Aldine Publishing Company, 1974: 106–109.
- 18. Bilodeau BA & Degner LF. Information needs, sources of information and decisional roles in women with breast cancer. Oncology Nursing Forum, 1996; 23 : 691 696. [PubMed] [Google Scholar]
- 19. Sloan JA, Doig W, Yeung A. A Manual to Carry Out Thurstone Scaling and Related Analytic Procedures. Manitoba Nursing Research Institute Technical Report #11. Manitoba, Canada: University of Manitoba, 1994.
- 20. Sloan JA & Yeung A. A Manual for Implementing Coombs’ Unidimensional Unfolding Model for Paired Comparisons Data. Manitoba Nursing Research Institute Technical Report #12. Manitoba, Canada: University of Manitoba, 1994.
- 21. Coombs C. A Theory of Data. New York: John Wiley & Sons Inc., 1964.
- 22. McIver JP & Carmines EG. Unidimensional Scaling. London: Sage Publications Ltd, 1991.
- 23. Thurstone LL. Psychophysical Analysis. In: Maranell GM (ed.) Scaling: a Sourcebook for Behavioral Scientists. Chicago: Aldine Publishing Company, 1974: 59–80.
- 24. Degner LF, Goodwin C, Carriere KC, Davison J. Clinical trial of a computer assisted intervention for women with breast cancer: a study in progress. Canadian Oncology Nursing Journal, 1997; 7 (2): 120 120. [PubMed] [Google Scholar]


