Abstract
Background: Postoperative pain is managed with opioids, which are associated with adverse effects. The efficacy of intravenous (IV) acetaminophen in reducing opioid consumption has been studied with inconsistent results. The primary outcome of this study was to assess the effect of IV acetaminophen on opioid consumption 24 hours postoperatively. Secondary outcomes included the opiate consumption at 48 hours after the operation, opioid-related side effects 72 hours after the operation, discharge disposition, and length of stay.
Methods: This was an IRB-approved, retrospective cohort study including adult patients who underwent an elective total knee arthroplasty (TKA). Patients were stratified into IV and no IV acetaminophen groups; patients who had received at least one dose of IV acetaminophen were included in the IV acetaminophen group. Total opioids were collected, converted to morphine equivalents, and compared between groups. Patients were excluded for alcohol abuse, substance abuse treatment, non-elective TKA, or medication mischarting.
Results: Of the 161 patients evaluated, 148 patients were included: 86 in the IV acetaminophen and 62 in the no IV acetaminophen group. There were no differences in mean morphine equivalents between groups postoperatively at 24 hours (54.2 ± 35.9 mg vs 45.4 ± 30.2 mg; p = .12) and 48 hours (99.2 ± 68.7 mg vs 79.5 ± 49.1 mg; p = .06). There were no differences in secondary outcomes (administration of bowel regimen medications, antiemetics, naloxone, discharge disposition, or length of stay) between the groups.
Conclusion: The use of IV acetaminophen was not associated with a decrease in opiate use, opiate-related side effects, or any secondary outcomes in patients who underwent TKA.
Keywords: acetaminophen, intravenous, IV, opiate, opioid, orthopedic, surgery
Adequate pain control is an important aspect of hospital care, particularly in the postoperative setting, due to the increase in morbidity and mortality associated with uncontrolled pain.1 Conventionally, postoperative pain is managed with a combination of opioids; however, multimodal pain management is widely used and recommended.2 Such modalities include the use of 2 or more medications with different mechanisms, such as the combination of local anesthetics and opioids.2 Opioids are frequently associated with adverse effects, such as constipation, nausea, vomiting, and sedation.3 Therefore, adjunctive pain management medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), are often added to opioid therapy.2 More recently, combination therapy with intravenous (IV) acetaminophen and opioids for postoperative pain management has been studied in an attempt to reduce the amount of opioids used postoperatively and minimize opioid-related adverse effects.4,5 IV acetaminophen has been shown to have a faster onset and reach higher peak levels when compared to oral or rectal administration.6
Although, the effect of IV acetaminophen has been evaluated in a variety of surgical settings, including cardiac; abdominal; spinal; ear, nose, and throat (ENT); dental; and orthopedic procedures, there is inconsistent evidence regarding its effectiveness in reducing postoperative opioid consumption. In abdominal laparoscopic procedures, IV acetaminophen was shown to reduce the amount of hydromorphone, morphine, and oxycodone consumed by 12% of patients during the first 12 hours after surgery. However, the reduction in opioid consumption was not statistically significant greater than 12 hours after the operation.7 In patients after lumbar laminectomy and discectomy, IV acetaminophen reduced the morphine requirements in the first 24 hours, but this difference was not statistically significant.8 Similar findings have been reported in other surgical settings.9 Conversely, IV acetaminophen use has been associated with a 13% to 21% decrease in opioid consumption 24 hours after coronary artery bypass graft (CABG) surgery.10,11 Patients who received IV acetaminophen post orthopedic procedures also demonstrated a 29% to 39% reduction in opioid consumption when compared to placebo.12–14 Lastly, there are inconsistent reports on the effectiveness of IV acetaminophen in reducing opioid-related adverse effects (ie, nausea/vomiting, constipation, respiratory depression, and sedation), discharge disposition, length of stay, pain scores, or patient satisfaction scores.8,10–12,14,15
At our institution, the use of IV acetaminophen perioperatively is provider-based, with the main purpose of improving pain management among surgery patients. The purpose of this study was to evaluate the effect of IV acetaminophen on postoperative opioid consumption in adult TKA patients in a tertiary care teaching hospital.
METHODS
Design and Setting
This was a retrospective cohort study, conducted at an urban academic medical center, to analyze the difference in mean amount of opioids administered perioperatively for patients after elective total knee arthroplasty (TKA). This study was approved by the institutional review board/human subjects research committee.
Patient Identification
The United Health Consortium Clinical Database (UHC-CDB) was used to identify adult orthopedic surgical patients who received an elective TKA procedure between July 1, 2013 and June 30, 2014 based on diagnosis-related group codes for TKA (0080 and 8154). Patients who were pregnant at the time of surgery, had known or suspected alcohol or drug abuse, were administered buprenorphine-containing products or methadone for addiction management, received an epidural postoperatively, were hospitalized for less than 24 hours, or for whom any medication mischarting was noted were excluded. Medication mischarting was defined as charting of doses that were considerably outside the range of doses ordered and were implausible to have been administered (eg, fentanyl 50 mg, hydromorphone 50 mg). Patients were stratified into 2 groups: those who received IV acetaminophen perioperatively and those who did not. The decision to administer IV acetaminophen was based on provider preference.
Outcomes
The primary outcome of this study was the effect of IV acetaminophen on opioid consumption 24 hours postoperatively. Secondary outcomes included the effect of IV acetaminophen on opioid consumption 48 hours following the procedure, opioid-related side effects 72 hours after the procedure, discharge disposition (home, skilled nursing facility, rehab facility, etc), and length of hospital stay.
Data Collection
Data were abstracted from the electronic medical record (EMR; Cerner Millennium, Kansas City, MO) and included baseline demographics, such as age, weight, gender, race/ethnicity, history of kidney or liver disease, and outpatient use of opioids and adjuvant pain medications. Acetaminophen, baclofen, carisprodol, celecoxib, cyclobenzaprine, diclofenac, duloxetine, gabapentin, ibuprofen, indomethacin, ketorolac, meloxicam, methocarbamol, naproxen, nabumetone, piroxicam, prednisone, pregabalin, tizanidine, tramadol, or tricyclic antidepressants were all considered adjuvant pain medications. Outpatient opioids and outpatient adjuvant pain medications were evaluated from the patients' medication list provided by the EMR for 6 months prior to and up to 48 hours after the operation. The administration of IV acetaminophen, hospital length of stay, and discharge disposition were also collected. For the primary outcome, the total amount of each opioid administered was collected and converted to morphine equivalents using standard opioid conversion calculators.16,17 The number of doses of scheduled or as-needed (PRN) bowel regimen medication, antiemetics, opioid-reversal agents, and occurrences of re-intubation 72 hours after the operation were also collected.
Statistical Analysis
All data were entered and analyzed in the Statistical Package for the Social Sciences (SPSS) version 19 (IBM Inc., Somers, NY). Descriptive statistics were used to identify differences in baseline characteristics between the 2 groups (independent t test and chi-square for continuous and categorical variables, respectively). The mean milligrams of morphine equivalents for patients who received IV acetaminophen versus those who did not were analyzed using an independent t test. Multiple linear regression was used to compare mean morphine equivalents between the study groups after controlling for potential confounders. Only variables with a p value less than .2 in the univariate analysis were included in the multivariate analysis. Based on the mean amount of opioids reported in previous literature (35.1 mg in the placebo group; 25.1 mg in the IV acetaminophen group),5,7,10–14 it was estimated that 60 patients were needed in each group in order to detect a 20% decrease in the amount of morphine equivalents used in the 24-hour postoperative period (α = 0.05, power = 80%).
RESULTS
Demographics
During the study period, 161 patients received an elective TKA; a total of 148 patients met the inclusion criteria. There were 86 patients in the IV acetaminophen group and 62 patients in the no IV acetaminophen group. The most common reasons for study exclusion included history of ethanol abuse, substance abuse treatment, non-elective TKA, and medication mischarting (Figure 1).
Figure 1.
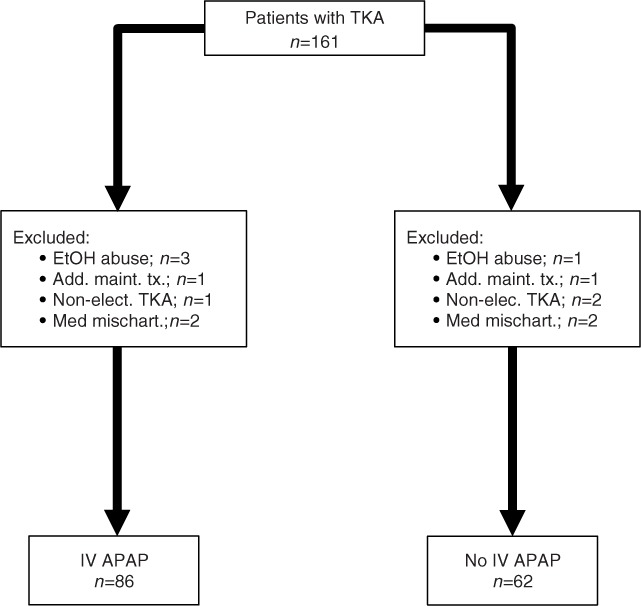
Patient selection process. Add. main. tx = addiction maintenance treatment; EtOH = ethanol; IV APAP = intravenous acetaminophen; Non-elec. = non-elective; Med mischart = medication mischarting; TKA = total knee arthroplasty.
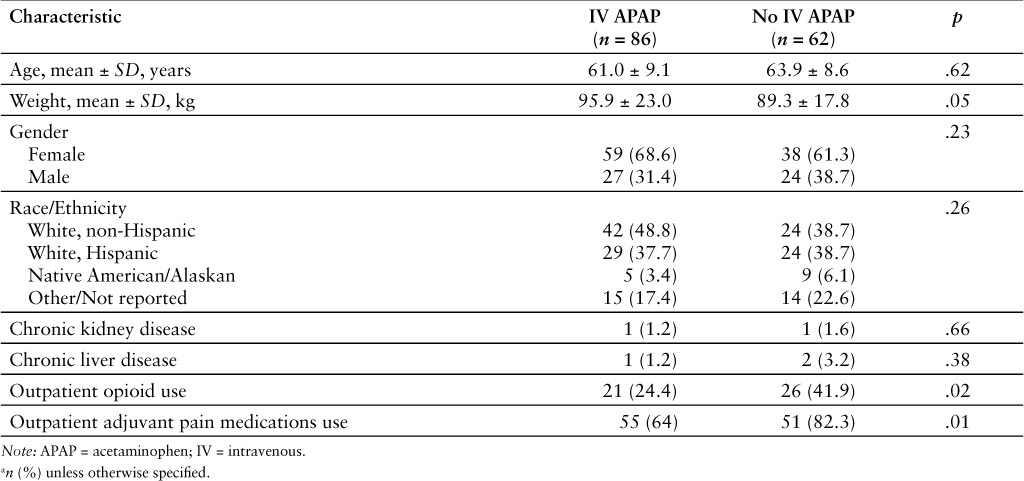
The demographic characteristics of both treatment arms were similar as shown in Table 1. Patients weighed slightly more in the IV acetaminophen group; however this difference was not statistically significant (p = .05). The patients who received IV acetaminophen were less likely to have received a prescription for outpatient opioids (24.4% vs 41.9%; p = .02) or adjuvant pain medications (64% vs 82.3%; p = .01).
Table 1.
Baseline characteristics a
The use of patient-controlled analgesia devices was similar in patients who received IV acetaminophen as compared to those who did not (79.1% vs 74.2%; p = .49). Likewise, the IV acetaminophen group received similar amounts of non-IV acetaminophen at 24 hours and 48 hours postoperatively when compared to patients who did not (24 hours: 642.4 ± 171.2 mg vs 687.1 ± 699.6 mg; p = .83; 48 hours: 1,553.2 ± 1,171.7 mg vs 1,651.6 ± 959.1 mg; p = .58).
Primary Outcome
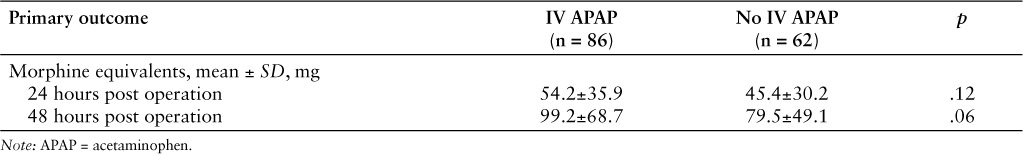
Eighty-five of the 86 patients in the IV acetaminophen group received one dose, with one patient receiving 2 doses in the first 24 hours after the operation. All doses administered were 1,000 mg. Patients who received IV acetaminophen and those who did not (controls) received a similar dose of total morphine equivalents at 24 hours (54.2 ± 35.9 mg vs 45.4 ± 30.2 mg; p = .12) and 48 hours (99.2 ± 68.7 mg vs 79.5 ± 49.1 mg; p = .06) postoperatively (Table 2).
Table 2.
Primary outcomes
Multivariate Analysis
Baseline characteristics were compared to mean morphine equivalents to identify potential covariates. During the univariate analysis, age and outpatient opioid use were significantly associated with morphine-equivalent doses at 24 hours (p < .001 and p = .01, respectively) (Table 3). These characteristics were included in the multivariate analysis along with other baseline characteristics that demonstrated a trend toward significance (p ≤ .2).
Table 3.
Analysis of factors contributing to postoperative opioid use following TKA a
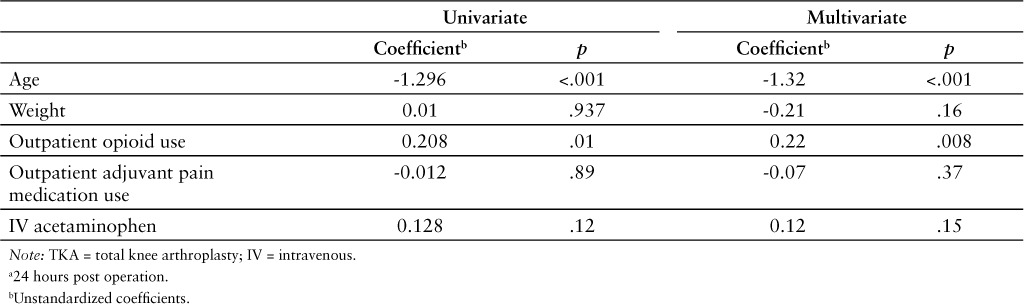
The multivariate analysis demonstrated that with an increase in age, there was a decrease in mean morphine equivalents administered (p < .001). Furthermore, the use of outpatient opioids was associated with an increased amount of mean morphine equivalents consumed postoperatively (p = .008). After adjusting for identifiable covariates, there was no significant difference in mean morphine equivalents with the use of IV acetaminophen.
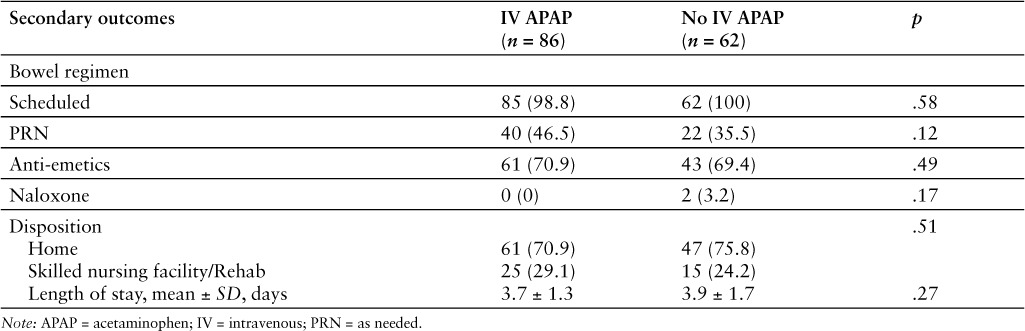
Secondary Outcomes
Data on the results of the variables evaluated for secondary outcomes are reported in Table 4. There was no statistically significant difference in the administration of scheduled or PRN bowel regimen medications, antiemetics, or naloxone. Additionally, there were no differences in discharge disposition or length of stay.
Table 4.
Secondary outcomes
DISCUSSION
Although opioids traditionally have been the medication of choice for postoperative pain, multimodal approaches are gaining favor as the mainstay for pain management.18,19 In this retrospective cohort study, the administration of IV acetaminophen did not demonstrate a reduction in opioid consumption in adult patients who underwent an elective TKA. Additionally, there was no difference in opioid-related side effects, discharge disposition, or length of stay between the 2 groups, which is consistent with previous literature.7,11–14,20
Results from other trials have noted that significant decreases in opioid consumption occurred with the administration of multiple doses of IV acetaminophen postoperatively (ie, 1,000 mg every 6 hours for 24 hours for a total dose of 4,000 mg).5,7,12–14 In the current study, all patients received a total dose of 1,000 mg with the exception of one patient who received 2 doses (2,000 mg). Additionally, opioid-sparing effects may be related to the amount of IV acetaminophen received, which could also explain the aforementioned findings of the current study. However, other literature in orthopedic patients suggested that a single dose is sufficient to reduce postoperative opioid consumption.21 Therefore, single dose administration of IV acetaminophen may be appropriate for postoperative opioid reduction. Another potential reason that our study was unable to demonstrate a decrease in opioid consumption was that IV acetaminophen was simply added onto other pain medication orders without any organized or concerted effort to use a multimodal pain regimen to reduce opioid consumption.
As expected, history of opiate use prior to surgery was associated with a higher use of opioids postoperatively. There was also an association with lower total doses of opioids in older patients in our study population. Evidence suggests that there are fluctuations in pain perception with age progression. Lautenbacher et al22 found that elderly patients had higher thresholds for somatosensory sensations and lower thresholds for pressure pain in comparison to younger patients. Although the average age in the Lautenbacher's trial was slightly higher than the average age in the current trial, these variations in pain perception suggest that elderly patients may experience different levels of pain and may require different amounts of opioids for pain management.
Though the current findings suggest that IV acetaminophen may not have an opioid-reducing effect in TKA patients, there may be some utility for IV acetaminophen regarding patient satisfaction. According to a pooled analysis conducted by Apfel et al, patients who received IV acetaminophen after hip/knee arthroplasty or abdominal/gynecological surgery were more likely to rate their quality of pain control as excellent as compared to patients who did not receive IV acetaminophen.15 Additionally, a reduction in pain scores was seen on days 1 and 2 in patients who received IV acetaminophen for open reduction internal fixations in comparison to those who did not.23 Pain scores were not evaluated in the current study, but rather opioid consumption was evaluated as a surrogate marker making it difficult to compare the effect of IV acetaminophen on patient pain scores and patient satisfaction.
Despite data supporting improved patient satisfaction with IV acetaminophen, the acquisition cost has recently been the area of focus. The average wholesale price of one vial of IV acetaminophen has nearly tripled over the 3 years prior to completion of the study ($13 per vial vs $32.90 per vial).24 Alternative dosage forms, such as rectal or oral, are available at a lower cost per unit. However, they lack the advantage of IV acetaminophen's quick onset of action and higher peak concentration, which have been associated with its benefit for postoperative pain management.6 Nonetheless, cost plays a major role in the decision about which medications to include and maintain on hospital formularies especially with budgetary restrictions.
Limitations
There are some limitations to be noted with this study. First, as a retrospective analysis, use of IV acetaminophen was made at the discretion of the providers. This is subject to selection bias as we were unable to randomize which patients received IV acetaminophen and control for additional factors that may have contributed to the physicians' decision to order the medication.
Additionally, 3 patients in this study received TKA surgeries on both knees at separate occasions. The first patient received IV acetaminophen for both procedures and received similar dose of opioids during both procedures (17.2 vs 20 mg). The second patient did not receive IV acetaminophen for either procedure and received a similar amount of opioids 24 hours postoperatively (118.3 vs 125.3 mg). The last patient received IV acetaminophen during both procedures, but received more morphine equivalents 48 hours postoperatively during the second surgery when compared to the first surgery (64 vs 30 mg, respectively).
Patient experiences during previous TKA surgeries may have influenced providers to offer more pain control with IV acetaminophen or opioids during the second TKA. Patients may have also requested more pain medications during their second TKA to better manage their pain based on prior experiences. However, this study design did allow for analysis of IV acetaminophen in naturalistic settings rather than in a controlled clinical trial.
Medication charting times may have been inconsistent given that charting does not always occur immediately after medication administration. This could have affected which doses of opioids were included in the 24- and 48-hour total dose calculations. We were also unable to assess the accuracy of documented outpatient medications and information included in the history and physical clinical notes. Documentation of outpatient medications does not necessarily confirm that the patients were taking the medications listed.
As previously mentioned, we did not analyze pain scores or patient satisfaction with pain management, but rather used milligrams of morphine equivalents as a surrogate indicator. This may have been an inaccurate marker for pain control as there many factors that influence administration of opioid medications. Some nurses may have been more diligent in assessing patients' pain and administering opioids than others. Similarly, some patients may have requested opioids more frequently than others to stay ahead of their pain. Alternatively, some patients may have not requested as many opioids as others due to fear of addiction. In 2012, 1.9 million people ages 12 and older used pain relievers for nonmedicinal purposes.25 This type of information is readily accessible via social media and internet sources, which may deter patients from seeking appropriate pain management.
Conclusions
The current study did not demonstrate a difference in opioid consumption in patients who received IV acetaminophen compared to those who did not during the TKA postoperative period. Moreover, there were no statistically significant differences in opioid-related adverse effects, discharge disposition, or length of stay between the 2 groups. Factors that were significantly associated with overall opioid use included age and use of outpatient opioids 6 months prior to surgery. Further studies in other surgical settings are warranted to reach a definitive conclusion on the efficacy of IV acetaminophen for reduction in opioid consumption and opioid-related adverse effects postoperatively.
ACKNOWLEDGMENTS
The authors report no conflicts of interests or financial support. They acknowledge Audrey Dettwiller, student pharmacist, for her contribution to data collection for this study.
REFERENCES
- 1. Sharrock NE, Cazan MG, Hargett MJL, Williams-Russo P, Wilson PD. Changes in mortality after total hip and knee arthroplasty over a ten-year period. Anesth Analg. 1995; 80: 242– 248. [DOI] [PubMed] [Google Scholar]
- 2. Apfelbaum JL, Ashburn MA, Connis RT, Gan TJ, Nichinovich DG. Practice guidelines for acute pain management in the perioperative setting. Anesthesiology. 2012; 116( 2): 248– 273. [DOI] [PubMed] [Google Scholar]
- 3. Benyamin R, Trescot AM, Datta S. et al. Opioid complications and side effects. Pain Physician. 2008; 11( 2 suppl): S105– S120. [PubMed] [Google Scholar]
- 4. Buvanendran A, Kroin JS, Tuman KJ. et al. Effects of perioperative administration of a selective cyclooxygenase 2 inhibitor on pain management and recovery function after knee replacement: A randomized controlled trial. JAMA. 2003; 290( 18): 2411– 2418. [DOI] [PubMed] [Google Scholar]
- 5. Memis D, Turan Inal M, Kavalci G. et al. Intravenous paracetamol reduced the use of opioids, extubation time, and opioid-related adverse effects after major surgery in intensive care unit. J Crit Care. 2010; 25: 458– 462. [DOI] [PubMed] [Google Scholar]
- 6. Singla NK, Parulan C, Samson R. et al. Plasma and cerebrospinal fluid pharmacokinetic parameters after single-dose administration of intravenous, oral, and rectal acetaminophen. Pain Pract. 2012; 12( 7): 523– 532. [DOI] [PubMed] [Google Scholar]
- 7. Winniger SJ, Miller H, Minkowitz HS. et al. A randomized, double-blind, placebo-controlled, multicenter, repeatdose study of two intravenous acetaminophen dosing regimens for the treatment of pain after abdominal laparoscopic surgery. Clin Ther. 2010; 32( 14): 2348– 2369. [DOI] [PubMed] [Google Scholar]
- 8. Cakan T, Inan N, Culhaoglu S. et al. Intravenous paracetamol improves the quality of postoperative analgesia but does not decrease narcotic requirements. J Neurosurg Anesthesiol. 2008; 20( 3): 169– 173. [DOI] [PubMed] [Google Scholar]
- 9. Aubrun F, Kalfon F, Mottet P. et al. Adjunctive analgesia with intravenous propacetamol does not reduce morphinerelated adverse effects. BJA. 2003; 90( 3): 314– 319. [DOI] [PubMed] [Google Scholar]
- 10. Petterson PH, Jakobsson J, Öwall A. Intravenous acetaminophen reduced the use of opioids compared with oral administration after coronary artery bypass grafting. J Cardiothorac Vasc Anesth. 2005; 19( 3): 306– 309. [DOI] [PubMed] [Google Scholar]
- 11. Lahtinen P, Kokki H, Hendolin H. et al. Propacetamol as adjunctive treatment for postoperative pain after cardiac surgery. Anesth Analg. 2002; 95: 813– 819. [DOI] [PubMed] [Google Scholar]
- 12. Sinatra RS, Jahr JS, Reynolds LW. et al. Efficacy and safety of single and repeated administration of 1 gram of intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology. 2005; 102( 4): 822– 831. [DOI] [PubMed] [Google Scholar]
- 13. Peduto VA and the Italian Collaborative Group on Propacetamol, Ballabio M Stefanini S.. Efficacy of propacetamol in the treatment of postoperative pain: Morphine-sparing effect in orthopedic surgery. Acta Anaesthesiol Scand. 1998; 42: 293– 298. [DOI] [PubMed] [Google Scholar]
- 14. Delbos A, Boccard E. The morphine-sparing effect of propacetamol in orthopedic postoperative pain. J Pain Symptom Manage. 1995; 10( 4): 279– 286. [DOI] [PubMed] [Google Scholar]
- 15. Apfel CC, Souza K, Portillo J, Dalal P, Bergese SD. Patient satisfaction with intravenous acetaminophen: A pooled analysis of five randomized, placebo-controlled studies in the acute postoperative setting. J Healthc Qual. 2015; 37( 3): 155– 162. [DOI] [PubMed] [Google Scholar]
- 16. Opioid Agonist Conversion. Lexicomp. http://online.lexi.com/lco/action/calc/calculator/70050. Accessed December 1, 2014.
- 17. Opioid Analgesic Converter. Globalrph: The clinician's ultimate references. http://globalrph.com/narcoticonv.htm. Accessed December 1, 2014.
- 18. Kehlet H, Dahl JB. The value of multimodal or balanced analgesia in postoperative pain treatment. Anesth Analg. 1993; 77: 1048– 1056. [DOI] [PubMed] [Google Scholar]
- 19. American Society of Anesthesiologists Task Force on Acute Pain Management. . Practice guidelines for acute pain management in the perioperative setting. Anesthesiology. 2012; 116( 2): 248– 273. [DOI] [PubMed] [Google Scholar]
- 20. Kelly JS, Opsha Y, Costello J, Schiller D, Hola ET. Opioid use in knee arthroplasty after receiving intravenous acetaminophen. Pharmacotherapy. 2014; 34( 12 pt 2): 22S– 26S. [DOI] [PubMed] [Google Scholar]
- 21. Singla NK, Hale ME, Davis JC. et al. IV acetaminophen: Efficacy of a single dose for postoperative pain after hip arthroplasty: Subset data analysis of 2 unpublished randomized clinical trials. Am J Ther. 2015; 22: 2– 10. [DOI] [PubMed] [Google Scholar]
- 22. Lautenbacher S, Kunz M, Strate P, Nielson J, Arendt-Nielson L. Age effects on pain threshold, temporal summation and spatial summation of heat and pressure pain. Pain. 2005; 115: 410– 418. [DOI] [PubMed] [Google Scholar]
- 23. Schug SA, Sidebotham DA, McGuinnety M, Thomas J, Fox L. Acetaminophen as an adjunct to morphine by patientcontrolled analgesia in the management of acute postoperative pain. Anesth Analg. 1998; 87: 367– 372. [DOI] [PubMed] [Google Scholar]
- 24. Lewis AN. IV acetaminophen (Ofirmev). Pharmacy Times. 2012. http://www.pharmacytimes.com/publications/health-system-edition/2012/Jan-2012/-IV-Acetaminophen-Ofirmev-. Accessed March 26, 2015.
- 25. Center for Behavioral Health Statistics and Quality. . Results from the 2012 National Survey on Drug Use and Health: Summary of national findings (HHS Publication No. SMA 13-4795, NSDUH Series H-46). Substance Abuse and Mental Health Services Administration website. September 2013. http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/Index.aspx. Accessed June 9, 2015.


