Abstract
Objective To identify variables within the patient‐oncologist communication pattern that impact overall patient comprehension and satisfaction within the breast cancer adjuvant therapy (AT) setting.
Setting and participants Fifty patients were recruited from a number of academic and community‐based oncology practices. Fifteen oncologists participated.
Main variables Three communication variables were identified: percentage of total utterances spoken by the patient, percentage of total physician utterances that were coded as affective (i.e. emotional), and total number of questions asked by the patient during the consultation. Knowledge and satisfaction were assessed by a variety of outcome measures, including knowledge items and satisfaction as measured by VASs, the satisfaction with decision scale and the decisional conflict scale.
Results The level of patient knowledge about breast cancer and satisfaction with the clinical encounter showed a tendency to correlate with the variables measuring aspects of patient‐physician communication style. Patients who spoke more or asked more questions tended to be more knowledgeable whilst patients whose physicians used more affective language tended to know less but to be more satisfied with their clinical encounter.
Conclusions In order to optimize patients’ degree of comprehension and satisfaction with their breast cancer adjuvant therapy, physicians need to increase their affective participation in clinical encounters whilst encouraging patients to ask questions and to actively participate in the decision‐making process.
Keywords: breast cancer, clinical communication, patient knowledge, patient satisfaction, RIAS
Introduction
The standards of communication between physicians and cancer patients have changed drastically in the last 20 years. Information as fundamental as the cancer diagnosis itself that was routinely withheld in the past 1 , 2, –3 is now conveyed to patients as a matter of course. 4 What still remain are wide variations in the communication practices of oncologists with respect to other types of information. Physicians may still hesitate to disclose details of treatment such as associated risks, prognostic information, and potential treatment alternatives. 3 , 5 , 6, –7
The communication process between physicians and cancer patients shares most of the general features of the standard doctor–patient interaction, but is burdened with additional problems. These problems emanate from a unique complement of factors that render the discussion of cancer emotionally charged. Most important amongst these factors are the stigma and fear associated with a diagnosis of cancer, 8 the complexity of the medical information itself and uncertainty regarding the course of disease and treatment benefits. 9 , 10, –11 Consequently, communication about cancer is often difficult, even where physicians and patients desire an open exchange of information. As a comprehensive discussion of treatment risks, benefits, and alternatives can be detailed and prolonged, suboptimal communication can very easily lead to information loss and misunderstandings. A review of the literature consistently corroborates the following findings: 12
• most patients continue to display significant gaps in their recall and understanding of treatment related information;
• physicians often do not relate information in a comprehensive or comprehensible way;
• providing detailed information has generally not been associated with adverse psychological sequelae and has, in some studies, been found to contribute to more positive treatment outcomes in the form of decreased patient anxiety and increased patient adherence to treatment regimens.
Improving the standards of doctor‐patient communication – including thorough discussion of the rationale for a proposed treatment or procedure, treatment related benefits and risks, and available treatment alternatives – is thought to offer many advantages to patients. 6 Ideally, such benefits are multifaceted and can be categorized broadly as follows: 5 , 12
• cognitive: improving recall and understanding of what physicians say and why they say it;
• affective: increasing patient and physician satisfaction and reducing patient anxiety;
• behavioural: assuring better patient adherence to drug protocols and appointment schedules;
• clinical: enhancing patient survival and quality of life.
A meta‐analysis of all published studies (n = 60) between 1965 and 1985 utilizing video or audiotaping of medical visits finds consistent relationships between patient outcomes and physician interview skills. 13 , 14 Of all outcome variables, satisfaction was best predicted by provider behaviour, quantity of communication overall, and social, partnership‐building communication in particular.
Discussing adjuvant therapy
Adjuvant therapy, the provision of treatment to stage I–III cancer patients with solid tumours after their primary surgical management, is the standard of care for most breast cancer patients. Patients who have no evidence of metastatic disease are now routinely considered for chemotherapy, hormonal therapy or both to prevent future recurrence. However, the use of adjuvant therapy in older patients continues to be less well accepted because of the modest benefits and significant potential toxicity. 15 This study examines how physicians make treatment decisions with breast cancer patients 50 years of age and older. Our study seeks to examine the relationship between patient‐oncologist communication patterns and overall patient comprehension and satisfaction. This paper presents and discusses data and findings from a preliminary set of 50 patients.
Methods
Sample
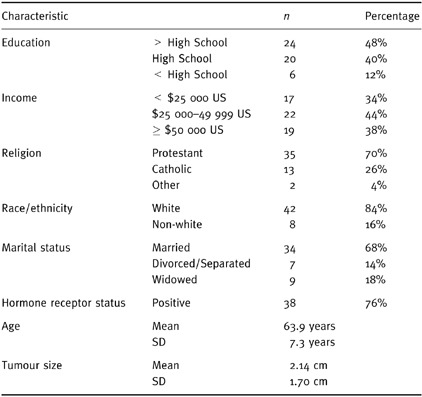
The study is being conducted at 14 practices in two large American metropolitan communities in two states. The practices consist of four academic oncology practices and 10 community‐based practices. A total of 49 oncologists are participating in the study. Patients are eligible for the study if they are post‐menopausal, candidates for adjuvant therapy, and at least 50 years of age with no prior history of breast cancer. All patients who are eligible for the study are asked to participate prior to seeing the medical oncologist for the first time. The study acceptance rate is 85%. Written informed consent was obtained from all patients and physicians participating in this study. The first 50 patients from our study are included in these analyses. Each patient was seen by one of 15 enrolled physicians. Table 1 details the demographic data for this study sample.
Table 1.
Patient demographic and disease characteristics (n = 50)
Data collection
Patients were enrolled at the time of their first visit to the medical oncologist to discuss post‐surgical care and consider adjuvant therapy. Most adjuvant care decisions are made at the time of this first visit. Patients who required a second visit were followed until the decision was made. Thirty‐six patients made their decisions based upon the first encounter with the physicians. Fourteen patients saw or spoke to their oncologist more than one time before they were able to make a decision. The patients who interacted with their oncologists on numerous occasions may have experienced somewhat different encounters than patients who only saw their oncologist once. However, due to the small sample size we are unable to evaluate the impact of this potential variable at this time.
The clinical encounter was tape‐recorded and coded using the Roter Interaction Analysis System (RIAS) to determine communication patterns. Patients were interviewed immediately before and after their clinical encounter with their oncologists using a semi‐structured questionnaire. We conducted these interviews to establish each patient’s overall comprehension of adjuvant therapy and satisfaction with her clinical encounter. A similar questionnaire was utilized in a follow‐up interview conducted 3 months after the initial consultation and initiation of treatment. At this time we obtained a measure of decisional regret. In this study sample, there was no loss to follow‐up at 3 months.
Measurement
The Roter Interaction Analysis System is a computer application designed for use in medical encounters to code and subsequently analyze dyadic exchanges. It allows coders to record each complete thought, or utterance, directly from an audiotape to a database. Each utterance is coded into one of 40 mutually exclusive and exhaustive categories reflective of the structure and content of the doctor‐patient exchange. Each utterance entered into the database may be coded with either a content code, which can distinguish between utterances that may be purely informational in character on the one hand, and affective codes that reflect emotional content such as empathy, reassurance or criticism. Also coded is the relationship of the speaker to the listener as well as specific types of informational categories of interest in this setting such as prognosis, treatment rationale, or risks and benefits of treatment. Using this system, one can objectively quantify the extent to which both patients and physicians participate in the consultation, and better pinpoint the role played by each.
As part of the coders’ process of learning the RIAS coding system, all 50 initial interviews were double coded. Kendall’s Tau B was calculated for each pair of coded interviews in order to obtain a measure of global agreement between coders. Six interviews needed to be recoded. Final Tau B scores ranged from 0.6087 to 0.7749.
RIAS variables
Three variables were extracted from the RIAS data. The database has been coded to yield much more detailed information but this initial analysis is part of a hypothesis generating stage of the analysis and thus is fairly limited in scope. A more detailed analysis of the data will allow us to examine the amount of information exchanged on specific topics such as risks, benefits, treatment rationale and prognosis, as well as the amount of time spent on these and other topics of interest. Each of the variables we selected is a measure of one aspect of the doctor‐patient communication pattern. These or similar variables have been used in previous analyses of RIAS coded data. 16 , 17, 18, 19, –20 The variables we utilized were:
1) Percentage of total utterances spoken by the patient (median = 38.1%, range 14.0 to 53.0%);
2) Percentage of total physician utterances that were coded as affective (i.e. emotional) (median = 8.4%, range 1.2 to 21.1%);
3) Total number of questions asked by the patient during the consultation (median = 13.0, range 2 to 65).
These variables are based on logical groupings of the utterance categories. The percentage of total utterances spoken by the patient was used as a measure of patient participation and verbal dominance in the encounters. The percentage of total physician utterances that were coded as affective was used as a measure of the emotional quality and responsiveness of the physician during the encounter. The total number of questions asked by the patients was used as a measure of patients’ active participation in the encounters. Of interest in this analysis was the correlation between the interactional components of the consultation and patient outcomes of subsequent comprehension about adjuvant therapy, immediate satisfaction with the treatment decision made, and long‐term satisfaction with the adjuvant therapy decision (decisional regret).
Each of the three interaction variables was categorized into two groups for the analysis – high and low utterance groups (the n for each group is listed in Tables 2 and 4). The group determination was based upon a qualitative examination of the distributions of the variables. For each variable, the difference between the means of the high and low groupings was statistically significant. The relationship between these variables and the outcome variables of interest were analyzed using Chi‐square for categorical level data and student’s t‐test for interval level data.
Table 2.
Effect of interaction characteristics on patient comprehension*
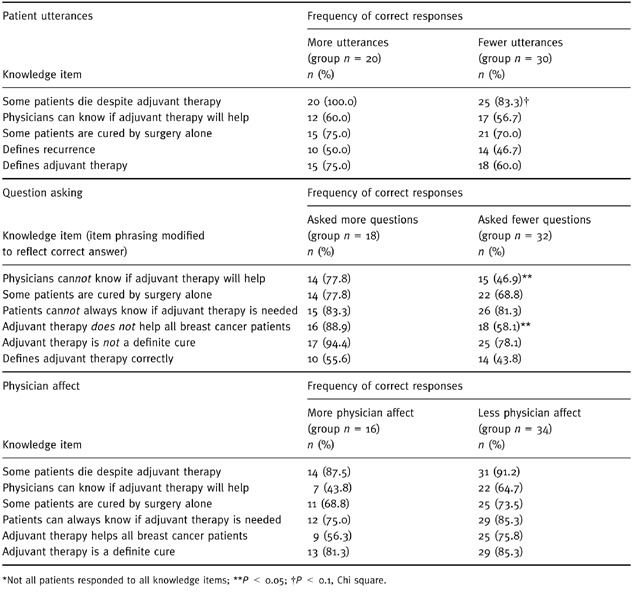
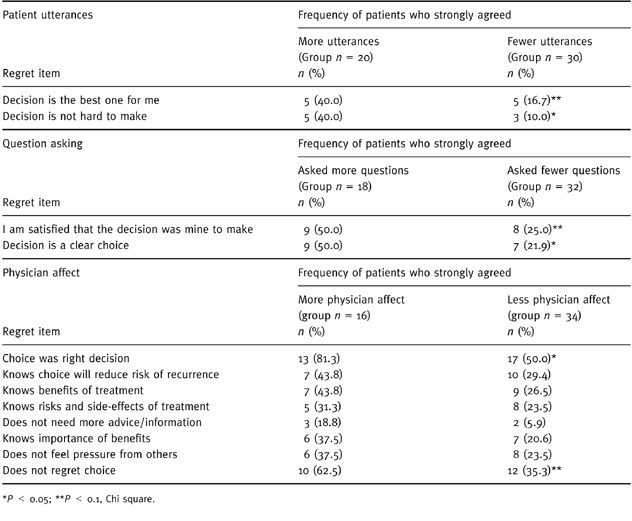
Table 4.
Effect of interaction characteristics on patient regret
Knowledge and satisfaction variables
Knowledge items
Patient comprehension was measured by testing patients on several discrete knowledge items. The following items/questions were included:
• whether or not one can know for certain that adjuvant therapy cures an individual patient;
• ability to define the concept of recurrence or relapse;
• whether or not breast cancer patients taking adjuvant therapy might die despite receiving treatment;
• whether or not a doctor can know for certain if a breast cancer patient will be helped by taking more treatment for her breast cancer;
• whether or not some breast cancer patients who take additional therapy would have lived just by having had the surgery;
• whether or not they will know for sure if they needed to take the additional therapy;
• whether or not additional breast cancer treatment will cure the cancer with certainty and;
• the ability to define adjuvant therapy
Satisfaction
Patient satisfaction with the clinical encounter was measured using Visual Analogue Scales (VAS) to rate satisfaction with the encounter. 21 , 22 Siminoff and Fetting have made extensive use of VASs with this patient population and have found them to be valid and reliable. 23 , 24 The specific items used included:
• satisfaction with the rationale provided by physicians for their treatment recommendations;
• satisfaction with their physician’s understanding of their treatment needs;
• overall satisfaction with the information actually received;
• satisfaction with the amount of time the physician spent with them;
• satisfaction with the concern the physician exhibited about the patient’s fears and;
• overall satisfaction with the visit itself.
A composite satisfaction score taking the arithmetic mean of these six items was also calculated.
Three instruments were used to measure short‐term satisfaction regarding treatment decisions and decisional regret: the decisional conflict scale (DCS), the satisfaction with decision scale (SWD), and a five‐point Likert scale assessing overall regret with the final decision. The DCS was developed by O’Connor 25 to measure patients’ uncertainty in making health‐related decisions, the factors contributing to uncertainty, and patients’ perceived effectiveness in decision making. The scale quantifies the factors contributing to uncertainty during the process of deliberation and following a treatment decision. 25 The DCS was evaluated in two decision‐making contexts, including 360 women aged 50–69 years, about breast cancer screening and influenza immunization decisions. The DCS has 16 items and uses a five‐point Likert scale with a reported internal consistency coefficient of 0.92 and a test‐retest coefficient of 0.81. 25
The SWD is a measure developed by Holmes‐Rovner et al. 26 The patient satisfaction with decision is a six‐item scale with excellent reliability (Cronbach alpha = 0.86) and good discriminate ability as evaluated using principal components analysis. The instrument was validated using a sample of post‐menopausal women specifically to evaluate the utility of patient decision aids. 26 The strength of the SWD is that it measures satisfaction with the decision made regardless of how good or bad the prognosis or health outcome might be for the individual patient.
The five‐point Likert scale was developed for this study specifically to measure overall regret asked about the following items:
• whether or not the decision was the right one for them;
• whether the patient does or does not regret the decision made;
• whether the patient would make the same choice if she had it to do over again;
• whether the choice did or did not do the patient harm, and;
• whether the decision was a wise one
Results
The results of this analysis are preliminary in nature and will help us generate hypotheses to test once the study is completed. We do expect that the patterns we have identified in the data will become significant as the size and power of the database increases assuming that the direction of the patterns holds constant. For illustrative purposes, we have included discussion of items which are either not statistically significant or are only marginally significant, but which show consistent directional patterns of responses.
Patient comprehension
Measures of patient comprehension were found to be positively associated with patients who spoke more, asked more questions, or had oncologists who used fewer affective utterances. In general, patients who spoke more during the consultation tended to provide more accurate responses to questions probing their comprehension about adjuvant therapy (see Table 2). Specifically, they were marginally more likely to correctly recognize that some patients die despite adjuvant therapy (P < 0.1). In addition, they tended to be more likely to understand that their medical oncologists cannot know whether or not adjuvant therapy will help, report that some patients live with surgery alone, and could correctly define recurrence or adjuvant therapy.
Patients who asked more questions were significantly more likely than patients who asked fewer questions to correctly recognize that adjuvant therapy will not help all breast cancer patients (P < 0.05) and that physicians cannot always know if adjuvant therapy will help them (P < 0.05). These patients also tended to be more likely than patients who asked fewer questions to know that some patients live with surgery alone, to recognize that patients cannot know for certain whether adjuvant therapy is needed, to define adjuvant therapy correctly, or to know that treatment does not necessarily cure everyone.
Meanwhile, patients whose oncologists used more affective utterances tended to exhibit lower degrees of comprehension than patients whose physicians used less affect. A pattern was seen for these patients as follows: they were somewhat more likely to report that patients would not die if they took adjuvant treatment; to think that physicians can know whether or not adjuvant therapy will help them; to fail to realize that some patients live with surgery alone; to believe that they can know with certainty whether or not adjuvant therapy is needed; to allege that adjuvant therapy will help all patients who take it and to assert that adjuvant therapy would definitely cure them.
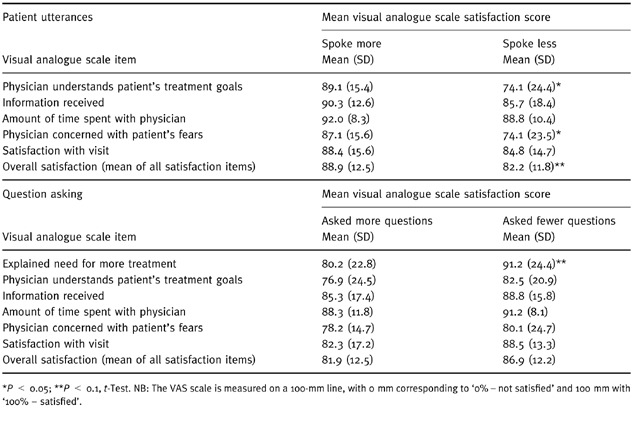
Patient satisfaction
Immediate patient satisfaction also was found to be related to communication variables. Patients who spoke more during their oncology appointment exhibited a generally higher mean level of satisfaction overall (P < 0.1 on the VAS items). Such patients were significantly more likely to be satisfied that their physician understood their treatments goals and that s/he was concerned about their fears (P < 0.05) (see Table 3). These patients also tended to be more satisfied with the information they received, the amount of time they spent with their oncologist, and their visit overall.
Table 3.
Effect of interaction characteristics on patient satisfaction
Of significant interest is evidence suggesting that asking more questions is associated with lower levels of patient satisfaction. Patients who asked more questions were marginally less likely to believe their physician adequately explained the need for more treatment than patients who asked fewer questions (P < 0.1). They also tended to be less satisfied with the information they received, the amount of time they spent with their oncologist and their overall visit. They reported less satisfaction that their physician understood their treatment goals or was concerned about their fears. No significant relationship or trend was identified between physicians’ use of affect and patient satisfaction.
Decisional regret
Finally, measures of regret were found to vary with communication variables (see Table 4). Patients who spoke more were significantly less likely to feel conflicted or regretful about their treatment decisions. These patients were more likely to strongly agree that the decision was the best one for them (P < 0.1) and did not agree that it was a hard decision (P < 0.05). On the other hand, patients who asked more questions were significantly less likely to be satisfied that the decision was theirs to make (P < 0.1) or to find treatment decisions to be clear‐cut (P < 0.05). This finding is in agreement with the relationship between patient question asking behaviour and satisfaction levels measured by VAS.
Meanwhile, patients of physicians who exhibited more affect were less conflicted and regretful about their decisions. They were significantly more likely to strongly agree that their decision was the right one (P < 0.05) and marginally more likely to strongly agree that they did not regret their choice (P < 0.1). They also tended to be more likely to strongly agree that they knew adjuvant therapy could reduce the risk of recurrence, knew the benefits of taking adjuvant therapy, knew the risks and side‐effects of adjuvant therapy, felt they did not need more information or advice than what they had already received, knew the importance of the benefits of treatment, and did not feel pressure from others concerning the decision they made.
Patient demographics: communication, comprehension, satisfaction and regret
The plurality (48%) of the sample had more than a high school diploma, were Protestant (70%), white (84%), and were married (68%). Their mean age was 63.9 years. Most patients were hormone receptor positive and had moderately size tumours (2.14 cm) (see Table 1 for more detailed information regarding the patients’ characteristics). Associations between patient demographic characteristics and the major independent and dependent variables were identified but the sample size limits any conclusions. Race appeared to be the most consistent factor, having the strongest overall effect on communication and comprehension. However, it must be noted that there were only eight non‐white patients in this sample. We found that white patients were more proactive during the consultation, being significantly more likely to speak more often (P < 0.01) and were able to answer more comprehension questions correctly (P < 0.01). White patients were also marginally more likely to exhibit lower overall satisfaction than non‐white patients (P < 0.1).
Education also had an effect on specific measures of comprehension and satisfaction. Patients with a higher educational level were significantly more likely to know that physicians cannot know for certain whether or not adjuvant therapy will help a particular patient (P < 0.05) and to be able to correctly define the term adjuvant therapy (P < 0.05). They were also significantly more likely to feel that their treatment choice did them no harm at 3 months post decision (P < 0.01). It may be that our sample is an unusually well‐educated group of women when compared to the general public. It also may be that the high educational level reflects a higher socio‐economic level amongst women who are able to access oncology care after a breast cancer diagnosis, the dependency on employer based health care benefits in the United States, and the link between education and employment status. This issue may be further complicated by the fact that in our sample, race, income, and education were found to covary, with higher education, higher income, and white race forming one cluster and lower education, lower income, and non‐white race forming the other.
Discussion
The findings point to the importance of specific characteristics of the physician–patient encounter. The fact that patients who participated more in their clinical encounter were more knowledgeable and had higher levels of satisfaction may indicate that these patients were better able to extract the information they needed or wanted from their oncologists. It will be of interest to assess whether patients who spoke more during their clinical encounters also spent more time interacting with their oncologists at a personal level, asking questions, or receiving information on particular topics that they queried.
Of particular interest is the finding that women who asked more questions were less satisfied with their visit. This pattern has been reported elsewhere. 18 These women may be coming into the encounter having done more independent research into their condition and having higher expectations of the physician and/or the information to be provided during the encounter. These relationships can be assessed once the database is complete since we have collected data assessing the extent of women’s knowledge about breast cancer prior to their appointment with their oncologist as well as their expectations for the visit.
The fact that women whose physicians used more affective utterances seemed to be both less well informed and more satisfied is striking. These women may be receiving less information from physicians who are spending a greater amount of their clinical time addressing the patients’ perceived psychosocial needs. This finding, if sustained in the final analysis, should be of great interest to physicians interested in meeting the psychosocial and information needs of their patients.
Conclusions
Although the findings from this study are intriguing, we stress that they are preliminary. The study is limited by the small sample size and the exploratory nature of the analyses. The findings may be confounded by demographic factors, however, with a small initial sample such as this one, that question will have to await further data collection and analysis. Nonetheless, we expect that if these same patterns hold with the remainder of our data, more of the associations will become statistically significant, supporting the preliminary conclusions we have drawn.
Given this caveat, there are some findings of interest. Patient comprehension, satisfaction, and regret associated with adjuvant therapy discussions and decisions appear to have been influenced by the manner in which patients and doctors communicated during clinical encounters. In the breast cancer setting, where information is complex and where the discussions can be emotionally charged, it is important for physicians to communicate optimally with their patients. Our findings provide a starting point toward identifying the critical components of these conversations that physicians need to consider when planning how to approach informing patients about their prognosis and treatment options. Assuming that our variables are indeed measuring components of the communication process that are characteristics of the conversations rather than of the participants, there are implications for clinical practice that physicians dealing with breast cancer patients may want to consider. In order to optimize patients’ degree of comprehension and satisfaction with their breast cancer adjuvant therapy, physicians need to consider increasing their affective participation in clinical encounters whilst encouraging and enabling patients to ask more questions, giving consideration to how responsive one is being to those queries, and offering encouragement of patients’ active participation in the decision‐making process.
References
- 1. Oken D. What to tell cancer patients: a study of medical attitudes. Journal of the American Medical Association, 1961; 175 : 1120 1128. [DOI] [PubMed] [Google Scholar]
- 2. McIntosh J. Processes of communication, information seeking and control associated with cancer: a selective review of the literature. Social Science and Medicine, 1974; 8 : 167 187. [DOI] [PubMed] [Google Scholar]
- 3. Silva MC & Sorrell JM. Enhancing comprehension of information and informed consent. Institutional Review Boards, 1988; 10 : 1 5. [PubMed] [Google Scholar]
- 4. Novack DH, Plumer R, Smith RL, Ochitill H, Morrow GR, Bennett JM. Changes in physicians’ attitudes toward telling the cancer patient. Journal of the American Medical Association, 1979; 241 : 897 900. [PubMed] [Google Scholar]
- 5. Fitts W & Ravdin I. What Philadelphia physicians tell patients with cancer. Journal of the American Medical Association, 1953; 153 : 901 904. [DOI] [PubMed] [Google Scholar]
- 6. Tuckett D & Williams A. Approaches to the measurement of explanation and information‐giving in medical consultations: a review of empirical studies. Social Science and Medicine, 1984; 18 : 571 580. [DOI] [PubMed] [Google Scholar]
- 7. Wu WC & Perlman RA. Consent in medical decision‐making. Journal of General Internal Medicine, 1988; 3 : 9 14. [DOI] [PubMed] [Google Scholar]
- 8. Liberati A. What doctors tell patients with breast cancer about diagnosis and treatment. British Journal of Cancer, 1986; 54 : 319 326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brewin TB. The cancer patient: communication and morale. British Medical Journal, 1977; 2 : 1623 1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sontag S. Illness as Metaphor New York (NY): Farrar, Straus & Grioux, 1978.
- 11. Frei E. The National Cancer Program. Science, 1982; 217 : 600 606. [DOI] [PubMed] [Google Scholar]
- 12. Siminoff LA. Improving communication with cancer patients. Oncology (Huntington), 1992; 6 : 83 87. [PubMed] [Google Scholar]
- 13. Roter D, Hall J, Katz N. Patient‐physician communication: a descriptive summary of the literature. Patient Education and Counselling, 1988; 12 : 99 119. [Google Scholar]
- 14. Hall JA, Roter DL, Katz NR. Meta‐analysis of correlates of provider behavior in medical encounters. Medical Care, 1988; 26 : 657 675. [DOI] [PubMed] [Google Scholar]
- 15. Desch C, Hillner B, Smith T et al. Should the elderly receive chemotherapy for node‐negative breast cancer? Journal of Clinical Oncology, 1993; 11 : 777 782. [DOI] [PubMed] [Google Scholar]
- 16. Bensing JM & Dronkers J. Instrumental and affective aspects of physician behavior. Medical Care, 1992; 30 : 283 297. [DOI] [PubMed] [Google Scholar]
- 17. Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Satisfaction, gender and communication in medical visits. Medical Care, 1994; 32 : 1216 1231. [DOI] [PubMed] [Google Scholar]
- 18. Roter DL. Patient participation in the patient–provider interaction: the effects of patient question asking on the quality of interaction, satisfaction and compliance. Winner of the 1977 Beryl J. Roberts Memorial Award. Health Education Monographs, 1977; 5 : 281 315. [DOI] [PubMed] [Google Scholar]
- 19. Roter D, Lipkin M, Korsgaard A. Sex differences in patients’ and physicians’ communication during primary care medical visits. Medical Care, 1991; 29 : 1083 1093. [DOI] [PubMed] [Google Scholar]
- 20. Roter DL, Stewart M, Putnam SM, Lipkin M, Stiles W, Inui TS. Communication patterns of primary care physicians. Journal of the American Medical Association, 1997; 277 : 350 356. [PubMed] [Google Scholar]
- 21. Like R & Zyzanski SJ. Patient satisfaction with the clinical encounter: social psychological determinants. Social Science and Medicine, 1987; 24 : 351 357. [DOI] [PubMed] [Google Scholar]
- 22. Like R & Zyzanski SJ. Patient requests in family practice: a focal point for clinical negotiations. Family Practice, 1986; 3 : 216 228. [DOI] [PubMed] [Google Scholar]
- 23. Siminoff LA & Fetting JH. Factors affecting treatment decisions for a life‐threatening illness: the case of medical treatment of breast cancer. Social Science and Medicine, 1991; 32 : 813 818. [DOI] [PubMed] [Google Scholar]
- 24. Siminoff LA, Fetting JH, Abeloff MD. Doctor‐patient communication about breast cancer adjuvant therapy. Journal of Clinical Oncology, 1989; 7 : 1192 1200. [DOI] [PubMed] [Google Scholar]
- 25. O’Connor AM. Validation of a decisional conflict scale. Medical Decision Making, 1995; 15 : 25 30. [DOI] [PubMed] [Google Scholar]
- 26. Holmes‐Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Medical Decision Making, 1996; 16 : 58 64. [DOI] [PubMed] [Google Scholar]


