Abstract
Background
Undernutrition remains highly prevalent in African children, highlighting the need for accurately assessing dietary intake. In order to do so, the assessment method must be validated in the target population. A triple pass 24 hour dietary recall with volumetric portion size estimation has been described but not previously validated in African children. This study aimed to establish the relative validity of 24-hour dietary recalls of daily food consumption in healthy African children living in Mbale and Soroti, eastern Uganda compared to simultaneous weighed food records.
Methods
Quantitative assessment of daily food consumption by weighed food records followed by two independent assessments using triple pass 24-hour dietary recall on the following day. In conjunction with household measures and standard food sizes, volumes of liquid, dry rice, or play dough were used to aid portion size estimation. Inter-assessor agreement, and agreement with weighed food records was conducted primarily by Bland-Altman analysis and secondly by intraclass correlation coefficients and quartile cross-classification.
Results
19 healthy children aged 6 months to 12 years were included in the study. Bland-Altman analysis showed 24-hour recall only marginally under-estimated energy (mean difference of 149kJ or 2.8%; limits of agreement -1618 to 1321kJ), protein (2.9g or 9.4%; -12.6 to 6.7g), and iron (0.43mg or 8.3%; -3.1 to 2.3mg). Quartile cross-classification was correct in 79% of cases for energy intake, and 89% for both protein and iron. The intraclass correlation coefficient between the separate dietary recalls for energy was 0.801 (95% CI, 0.429-0.933), indicating acceptable inter-observer agreement.
Conclusions
Dietary assessment using 24-hour dietary recall with volumetric portion size estimation resulted in similar and acceptable estimates of dietary intake compared with weighed food records and thus is considered a valid method for daily dietary intake assessment of children in communities with similar diets. The method will be utilised in a sub-study of a large randomised controlled trial addressing treatment in severe childhood anaemia.
Trial Registration
This study was approved by the Mbale Research Ethics committee (Reference: 2013-050). Transfusion and Treatment of severe Anaemia in African Children: a randomized controlled Trial (TRACT) registration: ISRCTN84086586.
Keywords: dietary assessment, validation, children, portion size estimation, Uganda, undernutrition
Background
Undernutrition, estimated to affect 100 million children in the developing world, is implicated in approximately 45% of childhood mortality globally1 2 and its reduction has been one of the United Nations Millennium Development Goals since 2000s3. Aside from affecting mortality, poor nutrition in the first 1,000 days of life is also associated with impaired cognitive ability, and reduced school and work performance4. Nutritional intake is fundamentally important to the health of the child and there is an intimate relationship between nutritional intake, nutritional status and infection. In order to develop and assess nutritional strategies and policies aimed at reducing childhood undernutrition, evaluation and validation of reliable methods of quantifying an individual’s macro- and micronutrient intakes are therefore of critical importance.
Several studies in African countries have used single methods for assessing diet including household consumption surveys5, weighed food records6, food frequency questionnaires7 8, and 24-hour dietary recall (24hDR)5–7 9 with variable success. Common methodologies, such as food frequency questionnaires and retrospective information on dietary history, are largely qualitative and considered as poor barometers of daily intake due to their imprecision10–12. Quantitative methods, measuring individual foods consumed (weighed food records, WFR) are the most precise methods for providing quantitative dietary data13. These are, however, time-consuming to conduct that results often in a small sample size, as they have been found to be burdensome and disruptive to the respondents. Interactive dietary recall is a potential substitute for a weighed food record. This has been investigated in Ghanaian children14 and in Malawian children15 in studies using a single 24hDR the day following independent weighed food assessment. This method of dietary recall could only be considered partially validated in the study groups due to some biases and imprecision. The Ghanaian study reported that averaged 24hDR assessments tended to underestimate energy and nutrient intake compared with WFR, while the Malawian study reported the opposite. The over- and under-estimation of energy and nutrients may be reduced by the modifying the triple pass method for 24hDR, which has been shown to maximise recall accuracy for quantitation16–18 by including volumetric portion size estimation, but this has yet to be evaluated in African children.
The current pilot study sought to establish the relative validity of an interactive 24hDR method with volumetric portion size estimation, compared to concurrent WFR in children in rural Uganda. The tool is intended for future use to assess the impact of daily dietary intake on outcome for a controlled trial of children hospitalised with severe anaemia (Transfusion and Treatment of severe anaemia in African children: a randomised controlled Trial (TRACT), ISRCTN84086586)19.
Methods
Aim
The study’s aims were first, to establish the relative validity of a 24hDR method compared to a weighed food record in estimating intakes of macro- and selected micro-nutrients in children in rural Uganda. Second, to ensure the recall method is feasible and culturally acceptable in this population.
Design
Dietary data from a weighed food record carried out by an independent researcher in the home of the subject was compared to estimated intakes from 24hDR assessments carried out by two other independent researchers the following day, to assess the relative validity of 24hDR. These researchers (clinicians and nurses) were not aware of the outcome of either the weighed food record or the other dietary recall. We opportunistically recruited 24 well children aged 6 months to 12 years attending Mbale and Soroti Regional Referral Hospitals over a two-week period in May 2014. We excluded infants who were entirely breastfed and children currently unwell. Prospective consent was sought from parents or guardians.
Pre-study training involved role-play simulations of data collection including recall and weighed food interviews with non-study child-parent pairs attending hospital to consolidate clinician and nurse training.
Portion size estimation
In developing the 24hDR method for this population, issues specific to East African diets emerged such as the estimation of portion sizes for semi-solid foods since much of the diet is a semi-solid consistency (such as a maize flour-based paste known as ‘posho’ or ‘ugali’) and eaten by hand, often from one communal family bowl20. Thus, it was problematic to estimate by volume using standard household measures (bowlfuls, spoonfuls). We developed a number of novel approaches to estimate portion sizes (see Table 1). We considered an alternative method of estimating portions of semi-solid foods by utilising play dough and volume displacement, previously proposed16 but not yet validated. Estimated volumes or number of items eaten were then converted into grams. For this a database of local foodstuffs was generated with weight per 100mls or weight of a whole food item. Local reference sizes were used where appropriate (for example small/medium/large mango) or for certain foods including cassava chips or sugar cane three using representative lengths to which they were closest. Consensus approaches were agreed for other items, for example loaves of bread were classified by price, since these are consistently sized in this community.
Table 1. Methodology of dietary data collection and portion size estimation.
| Stage | Methodology | Person conducting | Portion Size Estimation | |
|---|---|---|---|---|
| 1 2 3 |
Weighed food record 24-hour dietary recall 24-hour dietary recall |
First researcher Second researcher Third researcher |
{ | Weighing Volume of play dough* Household measures** Standardised food item size† |
for foods eaten by hand;
cups, bowls, table- and teaspoons of water or dry uncooked rice;
for example 1 egg, half of 1 medium onion
Dietary data collection
Dietary data collection occurred in three stages: weighed food record (WFR) and two dietary recalls (DR) each carried out by a separate member of the research team following published protocols14, 15. Each researcher completed only one stage with each child and guardian in the home of the child and were blinded to details recorded by other observers. The details of each stage are summarised in Table 1.
For all measures the specific time frame was from the time the child awoke in the morning to the time they slept at night. Any food taken after this time was not included in either WFR or DR since it was not realistic to expect researchers to remain in participants’ houses overnight.
The triple pass 24-hour recall, shown to maximise recall accuracy for quantitation18, used the following algorithm. The first pass encourages the respondent (guardian/parent) to freely report all food and drink intake for the prior day uninterrupted; in the second pass the interviewer probes for greater details on the exact time, type and quantity of food or drink taken; in the third and final pass the interviewer reviews all food reported in order, prompting for omissions and clarifying ambiguities. Completion of both DR used the same methodology and the same guardian and child to provide information about inter-assessor reliability and reproducibility. Interviews and assessments were carried out English or local languages to ensure accuracy.
Calculation of estimated requirements
Total daily energy and protein requirements were estimated using the methods recommended by the relevant World Health Organization (WHO), Food and Agriculture Organisation of the United Nations (FAO), United Nations University (UNU) or joint publications21 22. Iron requirements were based on the age and gender specific recommended daily allowances presented by Food and Nutrition Board of the US Institute of Medicine23.
Data entry and analysis
Data from WFR, DR1 and DR2 were entered into Dietplan 6 (Forestfield Software Limited), and energy, macro- and micronutrient intakes were automatically computed for most foods using McCance and Widdowstone’s ‘The Composition of Foods (Food Standards Agency)’24. These were supplemented, when recipes or foods were not available, by the Ugandan Food Tables (UFT)25 which are derived from the United States Department of Agriculture National Nutrient Database for Standard Reference. For food items, such as milk, meat and flour, where composition may vary geographically, both UFT and The Composition of Foods values were compared, and generally the lower of the two values used. Some foods such as oil, and maize and wheat flours are fortified in Uganda with vitamin A, and iron respectively, however this does not appear to be consistent26. Since the current study is concerned with method validation only and as such, unfortified values have been used.
We could find no data of direct nutrient analysis of food in Uganda or East Africa therefore some uncertainty remains regarding the accuracy of food composition data in this setting. It is recognised that neither US based UFT values25, nor the UK Composition of Foods24 may reflect actual nutrient composition of Ugandan foods.
Statistical analysis
Weight-for-age z-scores (WAZ) were calculated with WHO Anthro using the WHO reference population27 and compared to the Uganda Demographic and Health Survey (UDHS), which use the median of the National Centre for Health Statistics28, Centres for Disease Control and Prevention (CDC)29, and WHO reference populations27. All other statistical analysis was completed using IBM SPSS Statistics for Windows v22 (IBM). Prior to statistical tests, Kolmogorov-Smirnov statistic and Q-Q plots were used to assess data distribution. Only estimated energy requirements were non-normally distributed, therefore Wilcoxon signed-rank test was used when comparing estimated energy requirements and estimated intakes and variability was assessed using interquartile range (IQR, 25-75th centiles). Bland-Altman analysis was conducted for a range of macro- and micronutrients, to compare each individual assessment of 24hDR (DR1 and DR2) and then to compare these with WFR30. Mean difference and standard deviation of the difference between each DR, and DR and reference method were generated for energy, protein and iron consumption, and reported as mean difference and limits of agreement (i.e. ± 1.96*standard deviation of mean difference).
The relationship between estimated intakes of energy, protein and iron were explored using intraclass correlation coefficients (ICC) and by quartile cross-classification. ICCs compared absolute agreement of average measures, using a two-way random model. Classification was defined as correct (same quartile), adjacent (±1 quartile), or grossly misclassified by 2 or more quartiles. Differences between estimated requirements and estimated intakes by WFR, DR1, and DR2 were analysed using paired t-tests. Initial analysis was completed between WFR, DR1 and DR2 in pairs. Statistical significance was defined as p < 0.05.
Results
Demographics and anthropometry
Of 24 children recruited (14 in Mbale and 10 in Soroti), two did not complete the dietary assessment and three were excluded due to recurring or new illness. Of the remaining 19, 12 were female (61.9%), mean age (±SD) was 3.4 years (±2.6), and mean weight (±SD) was 14.0kg (±5.6). The mean WAZ score (±SD) was -0.19 (±1.75). Three children were moderately or severely underweight defined as WAZ scores ≤ -2.0. The majority (n=13) had WAZ scores between -2 and 2. Three children had high WAZ scores ≥2. Four children were partially breastfed therefore were not included in comparisons with estimated requirements as determining a reliable ‘portion size’ was impossible. A post hoc power analysis showed that with 19 participants, this study has 80% power to detect a difference of 16.7% or 1097kJ in energy intake at a significance level of 0.05, using the mean energy consumption of 6563kJ and SD of 1706kJ.
Inter-assessor variation
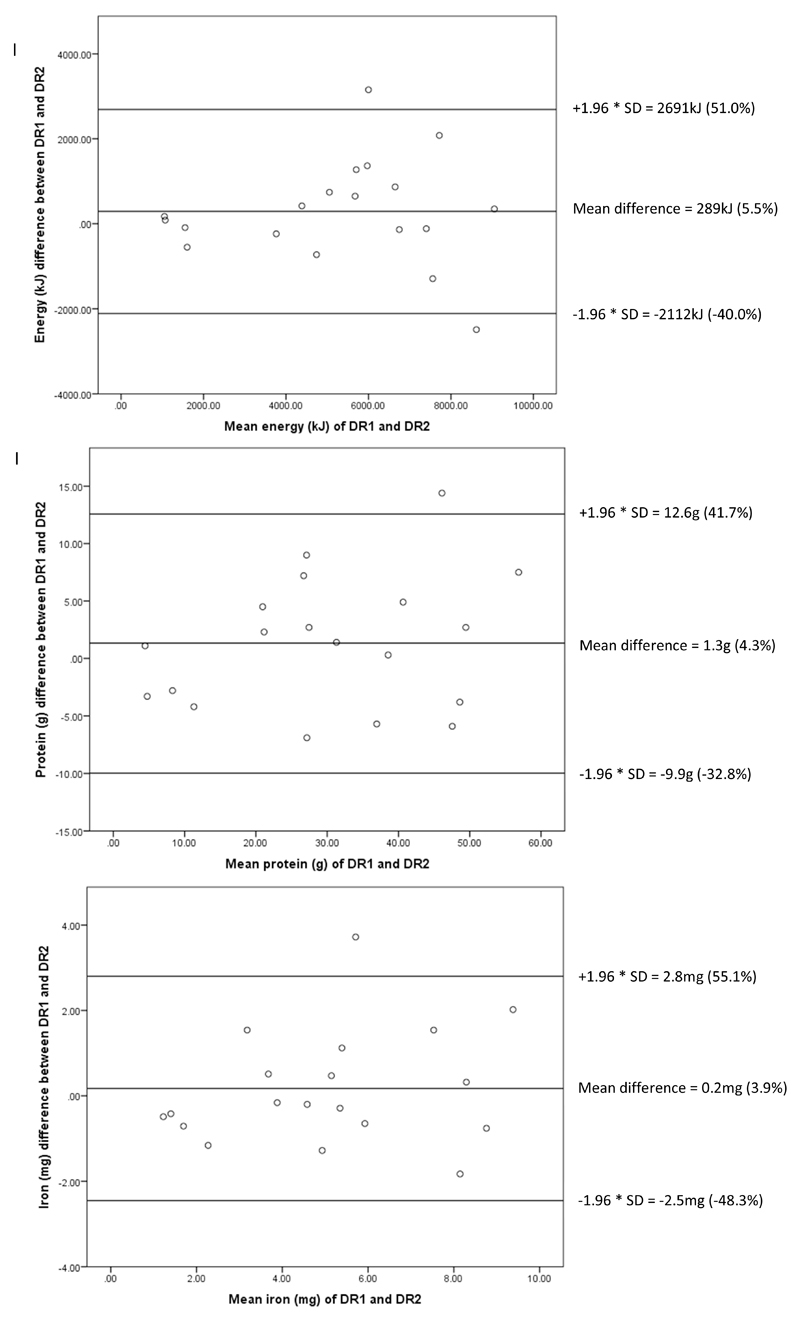
Figure 1 shows Bland-Altman analysis with mean difference, absolute limits of agreement and percentage (%) between DR1 and DR2 for energy 289.4kJ, -2111.9 to 2690.6kJ (-40.0 to 51.0%); protein 1.3g, -9.93 to 12.6g (-32.8 to 41.7%); and iron 0.2mg, -2.5 to 2.8mg (-48.3 to 55.1%). The intraclass correlation coefficient for the two 24-hour dietary recalls for energy was 0.802 (95% CI, 0.429-0.933), for protein 0.925 (95% CI, 0.779-0.975), and for iron 0.868 (95% CI, 0.618-0.955) suggesting high inter-assessor reliability. Since the estimates by DR1 and DR2 for each of these parameters were comparable as assessed by cross-validation and Bland-Altman analyses, we therefore used the global mean of these estimates to compare with WFR data for conciseness.
Figure 1.
Bland-Altman plots of first and secondary dietary recalls: (I) energy, (II) protein, (III) iron
Legend: DR, dietary recall; SD, standard deviation
Comparability of WFR and 24-hour dietary recall methods
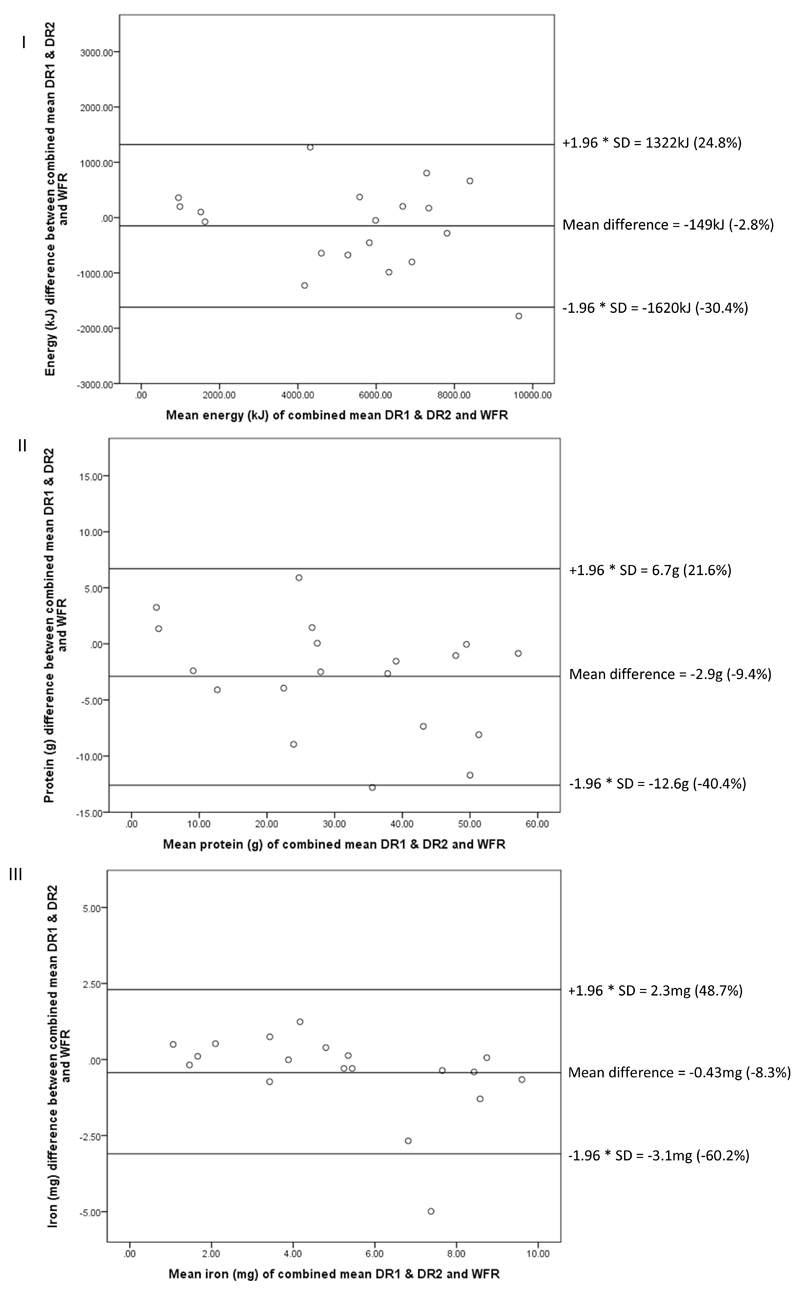
Figure 2 shows the mean difference for energy was -149.1kJ with limits of agreement of -1619 to 1321kJ (-30.4 to 24.8%), mean difference for protein was -2.9g with limits of agreement of -12.6 to 6.7g (-40.4 to 21.6%) and mean difference for iron was -0.4mg with limits of agreement of -3.1 to 2.3mg (-60.2 to 43.7%). Mean differences with associated upper and lower limits of agreement comparing WFR and combined DR1 and DR2 are displayed for all nutrients included in Supplementary Table 1.
Figure 2.
Bland-Altman plots of combined dietary recalls and weighed food records: (I) energy, (II) protein, and (III) iron
Legend: DR, dietary recall; SD, standard deviation; WFR, weighed food record
Intraclass correlation coefficients for WFR and combined 24-hour dietary recall estimates of nutritional intake were 0.979 (95% CI, 0.899-0.984) for energy, 0.972 (95% CI, 0.903-0.990) for protein, and 0.936 (95% CI, 0.837-0.975) for iron, summarized in Table 2.
Table 2. Intraclass and bivariate correlation coefficients comparing estimated intakes by weighed food records and 24-hour dietary recalls†.
| Nutrient | Weighed Food Record | Combined Dietary Recalls | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ICC (95% CI) | r (p-value) | |
| Energy (kJ) | 6563 | 1706 | 6335 | 1537 | 0.98 (0.90-0.98) | 0.96* |
| Protein (g) | 40.0* | 12.9 | 36.4* | 11.4 | 0.97 (0.90-0.99) | 0.985* |
| Iron (mg) | 6.6 | 2.6 | 6.0 | 2.0 | 0.94 (0.84-0.98) | 0.91* |
SD, standard deviation; ICC, intraclass correlation coefficient; CI, confidence interval; r, correlation coefficient
p<0.001
*p=0.02
ICCs compared absolute agreement of average measures, using a two-way random model
Classification into quartiles of intake and assessment of this agreement by Cohen’s Kappa (κ) statistic is displayed in Table 3. This showed that in the majority of cases WFR and dietary recalls agreed on classification, in 79% of cases for energy and 89% for protein and iron. The remainder were classified adjacently, with none being grossly misclassified. Agreement of classification in quartiles was substantial (κ 0.61-0.80) or almost perfect (κ 0.81-1.00) for all nutrients tested34.
Table 3. Cross-classification of children to quartiles according to intake estimates.
| Nutrient | Classified correctly (%) | Classified adjacently (%) | Grossly misclassified (by ≥2 quartiles) (%) | Cohen’s Kappa κ (p-value) |
|---|---|---|---|---|
| Energy | 15 (79) | 4 (21) | 0 | 0.719 (<0.001) |
| Protein | 17 (89) | 2 (11) | 0 | 0.859 (<0.001) |
| Iron | 17 (89) | 2 (11) | 0 | 0.859 (<0.001) |
Estimated requirements and intake
The median estimated requirement for energy was 4602kJ/day (IQR 25-75th centile = 3836-5208kJ), and intake was estimated at 6544kJ (IQR 25-75th centile = 5330-7448kJ) by the WFR, showing a significant surplus of 1942kJ (p=0.001). Mean estimated protein requirement was 14.2g (±5.1), while WFR-estimated intake was 40.0g (± 12.9)/day, 26.8g in excess of requirements (p<0.001). Mean iron requirement was 8.3mg (±1.6)/day, while WFR-estimated intake was 6.6mg (± 2.6) (p=0.004).
Discussion
The 24-hour multi-pass recall method described compared favourably to a weighed food records, with regards to energy, protein and iron intakes. Bland-Altman analyses showed overall agreement for energy, protein and iron intakes between two separate interviewers, suggesting high inter-assessor reproducibility, which is further reinforced by high intraclass correlation coefficients. Classification of energy intake into quartiles showed substantial agreement for energy and almost perfect agreement for protein and iron intakes.
High intraclass correlation coefficients, and low mean differences for energy, protein and iron with weighed food records suggest the triple-pass 24 hour recalls are comparable for assessing daily intakes. The method suggested by Gibson & Ferguson16 was adapted to the local setting and validated in this pilot. Using play-dough and volume displacement generally worked well, and was intuitive for both researchers and subjects. The estimated nutrient intakes must be interpreted with caution owing to wide limits of agreement; in the case of iron particularly, only gross differences in intake can be inferred. For iron one extreme outlier was noted with 4.99mg lower estimated intake by recalls compared to WFR. The cause of this large discrepancy was found to be due to inaccuracy in the portion size estimation of a ready-to-use nutrient-dense nutritional supplement, which contributed over 6mg of iron alone to intake, the only instance in this pilot where this supplement was noted. Studies involving severely malnourished children are likely to encounter ready-to-use feed or calorie enhanced milks, and particular care in estimating the portion size is advised due to nutrient density, for the future study (TRACT), where it is intended to be used the numbers of children with severe malnutrition are anticipated to be few.
Although inter-assessor variability was assessed, this study did not address intra-observer repeatability, which must be borne in mind when the method is used. One limitation of only assessing the preceding 24-hour period is that a habitual identical intake cannot be assumed. Both dietary recalls were undertaken on the same day, which may have introduced bias in parental recall, for example memory of information provided during the first recall may have been reinforced for the second recall, whether accurate or not, thus artificially reducing the inter-assessor variability. Noteworthy, is that whilst the results presented using the mean of two 24-hour dietary recalls will technically reduce the observed variability, the inter-assessor variability was low, therefore conducting a single recall should not have a substantive effect.
Although method validation was the main aim of this study, it is prudent to comment on the intakes observed. Energy intake was higher than in previous reported studies, at 6563kJ compared to 5606kJ31. Intakes of energy and protein were also in excess of requirements by a factor of 1.39 for energy and 2.97 for protein. Similar high protein intakes of 41.0g/day have been reported in children in other regions of Uganda31. Another potential reason for the difference is variation over the week in energy consumption, which is not reflected on a single day recall assessment. Two reasons are suggested for this observation. Firstly, although it was explained to participants that the priority was to observe the children’s intake unbiased, the effect of the researchers’ presence is difficult to estimate. Secondly, while these were healthy children, all had had recent contact with healthcare services, and as such may be experiencing catch-up growth and provided with additional food for recuperation. Indeed, WAZ scores observed showed that 16% were severely or moderately underweight, and is similar to the most recent UDHS 2011 census for the Eastern Uganda region32, where prevalence was 15.4%. In contrast to the UDHS results which showed only 0.1% had WAZ scores >2, compared to 15.8% (n=3) of subjects in this pilot.
The methods we have described and validated in children in Uganda appear consistent and correlate satisfactorily with quantitative assessment of dietary intake. A study comparing a single pass 24DR to assess dietary intake with a subsequent 7-day weighed food record in Sri Lankan adults found that 24DR tended to underestimate mean energy levels and macronutrients however the difference in the energy percentages were not statistically different33. Underestimation using single pass 24DR has been previously reported and is improved by triple-pass 24DR17 18. We consider that the method we have assessed to be valid for an on going a factorial treatment trial of African children presenting to hospital with severe anaemia (TRACT trial)19. The method will be used to assess nutritional intake as a surrogate marker of general wellbeing and the association of acute nutritional intake with severity of anaemia, impaired gut barrier function and susceptibility to infection. The TRACT study combines sequential dietary intake assessment using the multi-pass method at each follow-up visit to estimate macro and micro nutrient intake and will be subsequently linked to biomarkers of gut barrier function, gut microbiome, immunity and hormonal appetite control.
Supplementary Material
Supplementary table summarising Bland-Altman analysis results for all nutrients. Results presented in absolute and percentage values. Legend: DR: dietary recall; LOA: limit of agreement; WFR: weighed food record
Associated dataset in Excel format to enable validation of results and statistical interpretation. Gender has been removed to limit indirect identifiable information, but can be made available on request.
Acknowledgments
Funding: This research was funded by a grant (MR/J012483/1) from the Medical Research Council, United Kingdom (provided through the MRC DFID concordat). The MRC was not involved in the study design, collection, analysis, interpretation, or manuscript preparation.
List of abbreviations
- 24hDR
24 hour dietary recall
- CDC
Centres for Disease Control and Prevention
- DR
dietary recall
- FAO
Food and Agricultural Organisation of the United Nations
- ICC
intraclass correlation coefficient
- IQR
interquartile range
- LOA
Level of Agreement
- SD
standard deviation
- TRACT
Transfusion and Treatment of severe anaemia in African children: a randomised controlled Trial
- UDHS
Ugandan Demographic and Health Survey
- UFT
Ugandan Food Tables
- UNU
United Nations University
- WAZ
weight-for-age z-score
- WFR
weighed food record
- WHO
World Health Organisation
Footnotes
Ethics approval and consent to participate: This study was approved by the Mbale Research Ethics committee (Reference: 2013-050). Verbal consent was sought from parents or guardians for researchers to measure the child’s weight, observe and weigh the child’s food intake over one day, and for two separate 24 hour dietary recalls to be undertaken the following day. The child’s assent and ongoing verbal parental/guardian consent was also sought prior to each activity.
Consent for publication of individual data: Not applicable
Availability of Data and Materials
The dataset supporting the conclusions of this article is included within the article and its additional files.
Competing interests: None.
Authors’ contributions: HN, GF, KM, POO, and CE designed and planned the study. HN, TS, JN, CM, MN, MA, DA developed the method and carried out data collection. KJW analysed and interpreted the data. HN and KJW drafted the manuscript, and all authors commented on the manuscript.
Contributor Information
Helen Nightingale, Email: h.c.nightingale@gmail.com.
Kevin J Walsh, Email: k.walshk13@imperial.ac.uk.
Peter Olupot-Olupot, Email: polupotolupot@yahoo.com.
Charles Engoru, Email: charlesengoru@yahoo.co.uk.
Tonny Ssenyondo, Email: tssenyondo@gmail.com.
Julius Nteziyaremye, Email: jntezi@gmail.com.
Denis Amorut, Email: damorut@gmail.com.
Margaret Nakuya, Email: nakuyamarg@yahoo.com.
Margaret Arimi, Email: ariimim@yahoo.co.uk.
Gary Frost, Email: g.frost@imperial.ac.uk.
Kathryn Maitland, Email: k.maitland@imperial.ac.uk.
References
- 1.Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–60. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 3.The Millennium Development Goals. New York: United Nations; 2010. [Google Scholar]
- 4.Improving Child Nutrition: The achievable imperative for global progress. New York: United Nations Children's Fund (UNICEF); 2011. [Google Scholar]
- 5.Jariseta ZR, Dary O, Fiedler JL, et al. Comparison of estimates of the nutrient density of the diet of women and children in Uganda by Household Consumption and Expenditures Surveys (HCES) and 24-hour recall. Food Nutr Bull. 2012;33(3 Suppl):S199–207. doi: 10.1177/15648265120333S208. [DOI] [PubMed] [Google Scholar]
- 6.Kigutha HN. Assessment of dietary intake in rural communities in Africa: experiences in Kenya. Am J Clin Nutr. 1997;65(4 Suppl):1168S–72S. doi: 10.1093/ajcn/65.4.1168S. [DOI] [PubMed] [Google Scholar]
- 7.Amare B, Moges B, Moges F, et al. Nutritional status and dietary intake of urban residents in Gondar, Northwest Ethiopia. BMC Public Health. 2012;12:752. doi: 10.1186/1471-2458-12-752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin CA, Boslaugh S, Ciliberto HM, et al. A prospective assessment of food and nutrient intake in a population of Malawian children at risk for kwashiorkor. J Pediatr Gastroenterol Nutr. 2007;44(4):487–93. doi: 10.1097/MPG.0b013e31802c6e57. [DOI] [PubMed] [Google Scholar]
- 9.Alemayehu AA, Abebe Y, Gibson RS. A 24-h recall does not provide a valid estimate of absolute nutrient intakes for rural women in southern Ethiopia. Nutrition. 2011;27(9):919–24. doi: 10.1016/j.nut.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Block G, Thompson FE, Hartman AM, et al. Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. Journal of the American Dietetic Association. 1992;92(6):686–93. [PubMed] [Google Scholar]
- 11.Block G, Woods M, Potosky A, et al. Validation of a self-administered diet history questionnaire using multiple diet records. Journal of clinical epidemiology. 1990;43(12):1327–35. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 12.Kipnis V, Subar AF, Midthune D, et al. Structure of dietary measurement error: results of the OPEN biomarker study. American journal of epidemiology. 2003;158(1):14–21. doi: 10.1093/aje/kwg091. discussion 22-6. [DOI] [PubMed] [Google Scholar]
- 13.Ferguson EL, Gadowsky SL, Huddle JM, et al. An interactive 24-h recall technique for assessing the adequacy of trace mineral intakes of rural Malawian women; its advantages and limitations. European journal of clinical nutrition. 1995;49(8):565–78. [PubMed] [Google Scholar]
- 14.Ferguson EL, Gibson RS, Opare-Obisaw C. The relative validity of the repeated 24 h recall for estimating energy and selected nutrient intakes of rural Ghanaian children. European journal of clinical nutrition. 1994;48(4):241–52. [PubMed] [Google Scholar]
- 15.Thakwalakwa CM, Kuusipalo HM, Maleta KM, et al. The validity of a structured interactive 24-hour recall in estimating energy and nutrient intakes in 15-month-old rural Malawian children. Maternal & child nutrition. 2012;8(3):380–9. doi: 10.1111/j.1740-8709.2010.00283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gibson R, Ferguson E. An interactive 24-hour recall for assessing the adequacy of iron and zinc intakes in developing countries. Washington: International Food Policy Research Institute (IFPRI) and International Centre for Tropical Agriculture (CIAT); 2008. [Google Scholar]
- 17.Bingham SA, Cassidy A, Cole TJ, et al. Validation of weighed records and other methods of dietary assessment using the 24 h urine nitrogen technique and other biological markers. Br J Nutr. 1995;73(4):531–50. doi: 10.1079/bjn19950057. [DOI] [PubMed] [Google Scholar]
- 18.Ma Y, Olendzki BC, Pagoto SL, et al. Number of 24-hour diet recalls needed to estimate energy intake. Ann Epidemiol. 2009;19(8):553–9. doi: 10.1016/j.annepidem.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mpoya A, Kiguli S, Olupot-Olupot P, et al. Transfusion and Treatment of severe anaemia in African children (TRACT): a study protocol for a randomised controlled trial. Trials. 2015;16(1):593. doi: 10.1186/s13063-015-1112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nutrition Country Profile: The Republic of Uganda. Food and Agricultural Organization of the United Nations; 2010. Available at: ftp://ftp.fao.org/ag/agn/nutrition/ncp/uga.pdf: [Google Scholar]
- 21.Joint WHO/FAO/UNU Expert Consultation. Protein and amino acid requirements in human nutrition. World Health Organ Tech Rep Ser. 2007;935:1–265. [PubMed] [Google Scholar]
- 22.Human energy requirements: report of a joint FAO/ WHO/UNU Expert Consultation. Food Nutr Bull. 2005;26(1):166. [PubMed] [Google Scholar]
- 23.Food and Nutrition Board. Institute of Medicine. Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc: a report of the panel on micronutrients. Washington DC: National Academy Press; 2001. [Google Scholar]
- 24.Food Standards Agency. McCance and Widdowson's The Composition of Foods. Sixth Summary Edition. Cambridge: The Royal Society of Chemistry; [Google Scholar]
- 25.Hotz C, Abdelrahman L, Sison C, et al. A food composition table for central and eastern Uganda. Washington DC: HarvestPlus; 2011. [Google Scholar]
- 26.Quality of Fortified Foods in Uganda, Ministry of Health Food Fortification Program. National Monitoring Report. [Accessed 07/07, 2015]; Available at: http://www.ffinetwork.org/monitor/Documents/Uganda.pdf.
- 27.WHO child growth standards: methods and development: length/height-for-age, weight-for-age, weight-for-length, weight-for-height, body mass index-for-age. [Accessed 14/12, 2014]; Available at: http://www.who.int/childgrowth/publications.
- 28.National Center for Health Statistics. Growth curves for children birth to 18 years: United States Department of Health Education and Welfare, Vital and Health Statistics. 1977;11 Series. [PubMed] [Google Scholar]
- 29.National Health and Nutrition Examination Survey: CDC Growth Charts. [Accessed 12/14, 2014]; Available at: http://www.cdc.gov/growthcharts.
- 30.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–60. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 31.Bridge A, Kipp W, Raine K, et al. Nutritional status and food consumption patterns of young children living in Western Uganda. East Afr Med J. 2006;83(11):619–25. doi: 10.4314/eamj.v83i11.9478. [DOI] [PubMed] [Google Scholar]
- 32.Uganda Demographic and Health Survey. Kampala, Uganda: Uganda Bureau of Statistics; 2011. Available at: http://www.ubos.org/publications/health/ [Google Scholar]
- 33.Jayawardena R. Comparison dietary assessment methods in Sri Lankan adults: use of 24-hour dietary recall and 7-day weighed intake. BMC Nutrition. 2016;2(1) [Google Scholar]
- 34.McHugh ML. Inter-rater reliability: the kappa statistic. Biochem Med. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary table summarising Bland-Altman analysis results for all nutrients. Results presented in absolute and percentage values. Legend: DR: dietary recall; LOA: limit of agreement; WFR: weighed food record
Associated dataset in Excel format to enable validation of results and statistical interpretation. Gender has been removed to limit indirect identifiable information, but can be made available on request.