Abstract
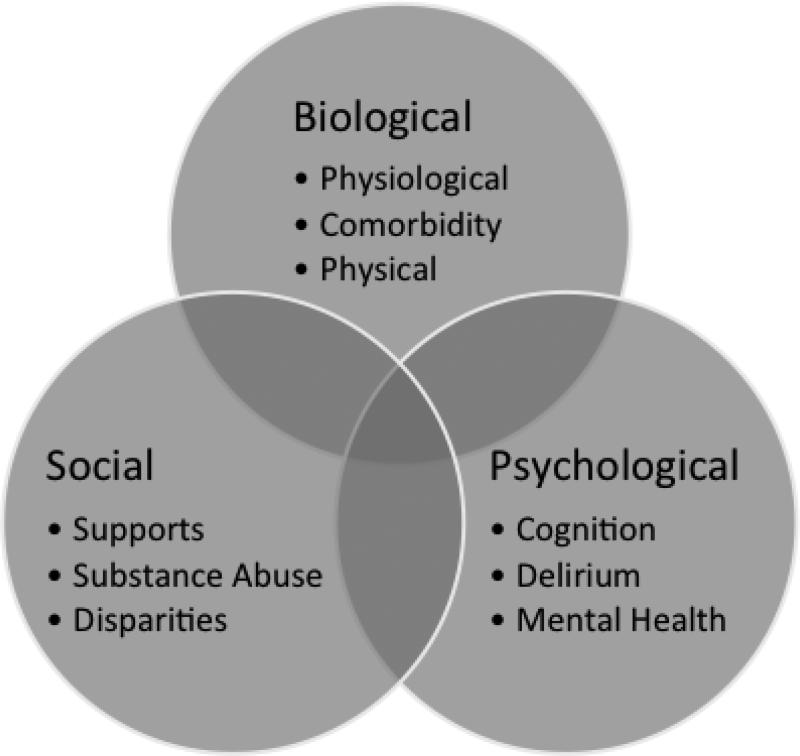
In an aging population, recovery and restoration of function are critical to maintaining independence. Over the past 50 years, there have been dramatic improvements made in cardiac surgery processes and outcomes that allow for procedures to be performed on an increasingly older population with the goal of improving function. Although improved function is possible, major surgical procedures are associated with substantial stress, which can severely impact outcomes. Past literature has identified that frail patients, who are vulnerable to the stress of surgery, are more likely to have postoperative major adverse cardiac and cerebrovascular events (OR 4.9, 95% confidence interval 1.6, 14.6). The objective of this manuscript is to examine preoperative frailty in biological, psychological, and social domains using cardiac surgery to induce stress. We systematically searched PubMed for keywords including “cardiac surgery, frailty, and aged” in addition to the biological, psychological, and social keywords. In the biological domain, we examine the association of physiological and physical vulnerabilities, as well as, the impact of comorbidities and inflammation on negative surgical outcomes. In the psychological domain, the impact of cognitive impairment, depression, and anxiety as vulnerabilities were examined. In the social domain, social structure, coping, disparities, and addiction as vulnerabilities are described. Importantly, there is substantial overlap in the domains of vulnerability. While frailty research has largely focused on discrete physical vulnerability criteria, a broader definition of frailty demonstrates that vulnerabilities in biological, psychological, and social domains can limit recovery after the stress of cardiac surgery. Identification of vulnerability in these domains can allow better understanding of the risks of cardiac surgery and tailoring of interventions to improve outcomes.
Keywords: Frailty, aged, cardiac surgery, biopsychosocial, delirium
1. Introduction
Frailty has been defined as a vulnerability to stressors.1,2 Preoperative frailty predisposes a patient to negative consequences after the stress of surgery. Recent work has identified that frailty is a major risk factor for negative outcomes after cardiac surgery3-7, with a systematic review demonstrating a five-fold increase in postoperative major adverse cardiac and cerebrovascular events (OR 4.9, 95% confidence interval 1.6, 14.6).6 While the literature has largely focused on the biological aspects of frailty as a risk factor8,9, psychological and social frailty can also result in negative postoperative outcomes. This is particularly important in the context of cardiac surgery being offered in an increasingly older and frailer population.10-13
Frailty has also been defined as a geriatric syndrome,14 a broader concept where accumulated deficits15 on many pathophysiologic pathways can lead to a similar constellation of symptoms (or phenotype). For example, when an older adult suffers femoral fracture following a fall, the phenotype and risk of negative outcomes are clear. However, the cause of the phenotype is multifactorial with the physical environment, sensation, cognition, the emotional state, and social factors all contributing to the fall and fracture. Importantly, focusing on a pre-emptive treatment of a single cause is unlikely to modify the risk (e.g. removing throw rugs does not compensate for reduced muscle strength, poor eyesight, or post-prandial hypotension).16 Additionally, the literature supporting biological underpinnings is limited with respect to the phenotypic expression of frailty.
Successful surgical correction of cardiac disease has the potential to restore biologic function and provide substantial benefit for older, symptomatic patients.17,18 However, while many older adult patients survive surgery and return to preoperative functional levels, the perioperative risk of mortality and morbidity from cardiac surgery is higher than in younger patients undergoing similar procedures.3-7 While the techniques and processes of cardiac surgery have progressed to allow older adult patients to be considered as surgical candidates, the surgery remains a physiological, psychological, and social stressor.19-21
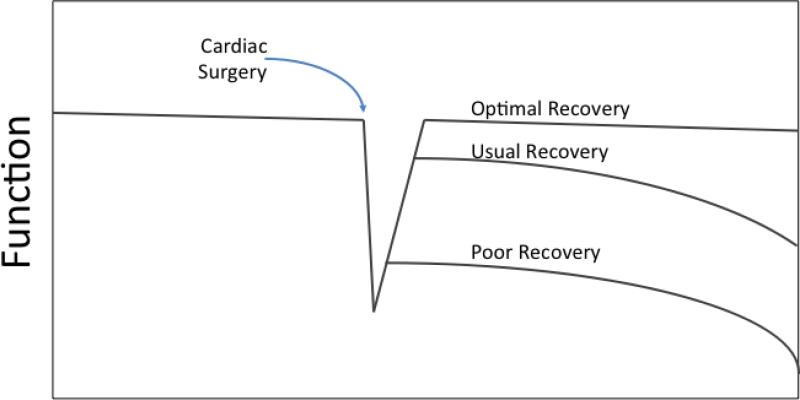
Any surgery, including cardiac surgery, is a stressor to the patient. This manuscript examines frailty by using cardiac surgery as a “stressor” event in the older adult population. A vulnerable patient, who is more susceptible to the complexity of surgical process, will be at-risk for complications of the surgery and will be less likely to return to function postoperatively (Figure 1). The process of cardiac surgery is typically very structured: a) there is a baseline assessment; b) the surgical procedure (i.e. stressor) most commonly occurs a predetermined time and place; c) there is measurable systemic response; and d) there is anticipated survival and recovery course. (Box 1 describes stressors associated with Cardiac Surgery). By expanding the scope of vulnerability within the construct of the biopsychosocial model after cardiac surgery, we acknowledge that the surgical process includes factors that are outside of the control of the peri-operative team and may influence outcomes.
Figure 1. Response to Stressors.
When a frail patient is subjected to a stressor, such as cardiac surgery, there is a reduced ability to return to the prior level of functioning and frequently negative outcomes. They tend to attend a new “baseline”. As these stressors become more severe or more often, the baseline status continues to trend down. Patients with pre-existing vulnerabilities may undergo cardiac surgery at lower functional levels (i.e. cardiac surgery stress is shifted right).
1.1 The Biopsychosocial Model and Frailty
This Biopsychosocial Model has been applied in multiple conditions to understand the impact of illness22, particularly complex diseases. The syndrome of frailty has been applied to the Biopsychosocial Model using the stressor of cardiac surgery in this review. In the biological, psychological, and social domains, the literature supports frailty as a vulnerability to the stress of cardiac surgery. In the following sections, the association of frailty in each of the biopsychosocial domains with negative health outcomes after cardiac surgery will be reviewed. Importantly, there is a substantial overlap among the domains. For example, cognitive frailty has biological, psychological, and social underpinnings that contribute to negative outcomes after surgery. Describing the overlap of domains is not possible within the scope of this manuscript.
1.2 Age, Vulnerability, and Frailty
One of the critical areas of overlap – age deserves mention. Age is inextricably linked to frailty, but not causally related.14,23 In the case presented, the patient's age is a risk factor for perioperative morbidity and mortality. However, the acuity of the patient's cardiac illness24, physiology as well as the underlying comorbid disease25 and functional24 status, should be considered in the decision for cardiac surgery. Chronological age alone cannot be the sole factor in determining operative vulnerability.
2. Biological Frailty
2.1 Case Continued
Mr P. has many chronic medical conditions including hypertension, hyperlipidemia, benign prostatic hypertrophy, osteoarthritis of the knees and hands, gastroesophageal reflux, and constipation. He takes 8 different medications and a multivitamin every day. He is able to walk about 100 meters before the chest pain causes him to stop. Mr P. develops chest pain during the climbing of one flight of stairs to his bedroom. He frequently complains of fatigue and takes an afternoon nap daily. He has had an unintentional 4-kilogram weight loss in the 12 months.
When considering the biological domain, there is a significant body of evidence that the contribution of physiological function26,27, comorbidity27,28, and inflammation29,30 contribute to a patient's vulnerability for negative outcomes after cardiac surgery.31 The case presented identifies multiple comorbid conditions and treatments, each with a molecular underpinning that can contribute to a negative response to stress. For example, the osteoarthritis of the knees, in addition to limited mobility, is associated with an increase in baseline inflammation and subsequently treated with an agent (nonsteroidal anti-inflammatory drugs) that affects platelet function thereby increasing the risk for bleeding after surgery. Each factor has a separate biological underpinning and cumulatively contributes to a propensity for adverse events after cardiac surgery, yet each is dependent on the others.
2.2 Physiological frailty
There are, presently, two major scoring systems that are commonly utilized to predict the risk of negative outcomes following cardiac surgery. Both the Society of Thoracic Surgeons (STS)27,32 and the European System for Cardiac Operative Risk Evaluation II 26 (EuroSCORE II) risk prediction tools are sophisticated models used for prediction of morbidity and mortality following cardiac surgery. As a result, the physiological variables entered into the models meet the broad definition of frailty. While these tools have incorporated age, both in their current iteration, focus on “traditional” physiology variables and thus provide information limited to the patient's physiological vulnerability. It is becoming increasing evident that a more comprehensive assessment that involves the psychological and social frailty assessments as part of their algorithm is necessary for the contemporary cardiac surgery patient.4,33
2.3 Comorbidities
On a fundamental level, medical conditions reduce an organ system's ability to respond to stressors and multiple comorbidities should increase vulnerability to the stress of cardiac surgery.34 While both the STS and EuroSCORE II risk prediction scores incorporate a collection of co-morbid disease, listing diseases provides a basic measure of organ function and does not account for the range in organ function. Additionally, many chronic medical conditions such as inflammatory, cognitive, or oncologic conditions are not included as these are not presently routinely collected as part of the preoperative evaluation as the majority of currently utilized assessments did not consider the aging population that is now being referred for cardiac surgery procedures. Therefore, as the incidence of comorbid medical conditions grows in an older and complex operative population, there is a need to have a deeper understanding how the additional factors increase a patient's vulnerability to the anticipated stress of their surgical procedure. Past work identified that comorbidity was a risk factor for frailty.35 With increasing comorbidities, comes increased preoperative medication utilization and potentially altered drug metabolism.36 The potential for interactions, reactions, and adverse events increases when baseline polypharmacy is combined with the perioperative medications.37
2.3 Inflammation
In studies of sepsis38, trauma39, surgical complications40, and exercise41, those patients with higher baseline circulating inflammatory cytokines had an heightened and prolonged inflammatory response compared to those with lower baseline inflammation. Importantly, preoperative levels of inflammatory markers have been shown to be higher in frail versus non-frail individuals, 35 and has suggested that chronic low-level inflammation makes one prone to frailty.42,43 During cardiac surgery, there is a dramatic rise in inflammatory markers with levels that can be over 100 times the baseline level.40,44 Therefore, when primed with pre-existing low level inflammation, the response to stressors following cardiopulmonary bypass can be significantly amplified.45,46 As a result, frail patients with low levels of inflammation may have more of an inflammatory response which might contribute to negative postoperative outcomes such as vasoplegia, atrial fibrillation and delirium.47,48
2.4 Physical Frailty
With the description of Fried's Frailty Phenotype35, there is a growing body of literature on the interrelationship of physical frailty and multiple negative consequences. Fundamentally, this physical frailty model can be utilized to further our understanding of responses to the stress of cardiac surgery. In the sections below, we examine the components of this frailty phenotype with relationship to cardiac surgery stress.
2.4.1 Decreased activity
The presence of underlying chronic disease further contributes to the limitation of physical activities in older adults, leading to acceleration of catabolic process.49,50 Importantly, preoperative gait speed is developing as a marker of morbidity and mortality after cardiac surgery.51 In the case outlined above, the presence limits of preoperative physical activity combined with osteoarthritis, hormonal imbalance/deficiency such as testosterone imbalance, compounds the problem. Instrumental activities of daily living (IADLs) dependence and the use of walking device were independent predictors of the outcome of cardiac surgery in the older patients.52
2.4.2 Sarcopenia
Sarcopenia, a loss of muscle mass, is associated with adverse clinical outcome after cardiac surgery.53 The loss of muscle mass associated with sarcopenia represents not only a risk in physical capabilities for recovery, but an unknown impact on cardiac muscle function. In a healthy older adult population, the loss of 70% of basal muscle power was associated with physical frailty.54
2.4.3 Weight loss
There are extremes of weight that can lead to vulnerability after cardiac surgery. Both malnutrition from protein deficiency and obesity are associated with poor wound healing and multiple complications55 and low albumin associated with operative mortality.56 Further complicating the picture are dietary restrictions57, difficulties in chewing and swallowing58, medication and their side effects37, and comorbidities.34 Importantly, the value of weight loss is a marker of morbidity and mortality after cardiac surgery.59
2.4.4 Exhaustion
Exhaustion was the defining feature of frailty in patients with CVD.3 In combination with the psychological domain below, the exhaustion component represents the overlap of physical and psychological frailty.
3. Psychological Frailty
3.1 Case Continued
Mr. P had difficulty maintaining the house after the death of his wife 2 years ago as she managed many of the household activities. Currently, he drives to the store, prepares his meals, and is able to perform housework. He depends on his neighbors for maintaining the exterior of his home which the chest pain has proven limiting. He is frustrated by the physical limitations, but thankful that he is able to continue driving. He states that he has no problems with memory besides forgetting where he put his keys. He denies having symptoms of depression.
The relationship between atherosclerosis and psychological disease, including cognitive impairments60,61 and psychiatric disease62, has been well established. We used the psychological domain of frailty to examine how the stressor of cardiac surgery impacts the recovery. While psychological frailty lacks the definitive criteria and measurement ability of physical frailty, few would argue that recovery in the psychological domain is critical to returning to preoperative levels of function.63,64
3.2 Cognitive Frailty
The impact of cardiac surgery on postoperative cognitive function has been debated for years.65,66 Challenged by measurement of cognition before and after cardiac surgery65,67, there are some fundamental vulnerabilities that may predispose patients to subsequent cognitive decline. It needs to be stated clearly that most patients who undergo cardiac surgery return to baseline.68,69 However, a small group of patients have a measureable cognitive decline after cardiac surgery.68-70
3.2.1 Preoperative Cognitive impairment
Patients with atherosclerosis have lower preoperative cognitive performance.69 There are many studies which identify a fundamental cognitive decline preoperatively in those patients undergoing cardiac surgery relative to age, gender, and education matched controls.69 If a cognitive insult is associated with cardiac surgery, those with pre-existing cognitive impairment are more likely to experience further decline.
3.2.2 Delirium
Delirium is an acute change in attention and cognition that occurs in up to 50% of cardiac surgery patients.71 Delirium is independently associated with functional decline after cardiac surgery.72 Recovery in surgical patients with delirium can be delayed, particularly in those patients with preoperative cognitive impairment.73 Patients who are preoperatively frail are more likely to develop delirium.74
3.2.3 Postoperative Cognitive Decline
While measurement of cognitive function is challenging in the preoperative and postoperative settings, there are several comprehensive reviews of cognitive decline following cardiac surgery.66,67 This postoperative cognitive decline has been found in both cardiac68-70 and non-cardiac surgery75,76 and can last for years. Postoperative cognitive decline appears to be more common among those with pre-existing cognitive impairments, however, suggesting that the decreased cognitive reserve is unable to respond to the stress of the surgical procedure (Figure 1).77
3.3 Mental Health
3.3.1 Depression
Cardiac surgery is associated with mental health stress when measured on standardized questionnaires. Rating questions regarding energy, mood, appetite, and thoughts about the future are contextually different as a patient is adapting to the impending cardiac surgery. A systematic review found that as patients entered the recovery period (2 weeks postoperatively), depressive symptoms measured on standard instruments and depression diagnosis was lower than preoperative levels.78 Importantly, those who were diagnosed with depression more than 1 week prior to cardiac surgery were less likely to experience depression remission postoperatively.78 This response to the mental health stress of cardiac surgery can provide valuable insight into cardiac surgery outcomes.
Despite the timing limitations, screening for preoperative depression has been found to be an important determinant of outcomes following cardiac surgery. Cardiac events included angina or heart failure that needed admission to hospital, myocardial infarction, cardiac arrest, percutaneous transluminal coronary angioplasty, repeat CABG, and cardiac mortality.79 There remains considerable debate as to whether depression in itself is a vascular phenomenon related to the atherosclerosis in these patients.62 The clinical take away highlights the importance of screening for depression in both pre- and postoperatively setting.63,64.
4. Social Frailty
4.1. Case Continued
Mr. P has lived in the same town for over 60 years and was once very connected in civic and religious organizations. He has seen his social network decline due to deaths and functional limitations of his friends. He feels less connected and does not regularly attend services. He has three children and four grandchildren. His daughter lives 45 minutes away, however tries to visit weekly. His other children and grandchildren live in distant states. He draws a small pension and has social security for income which allow him to pay the bills without savings. He recently asked his daughter to assist with paying the bills after a recent hospitalization.
There are social factors that predict recovery after cardiac surgery such as adaptive characteristics, social support, geographic distance, and socioeconomic status. There are also gender80 and racial disparities10in the availability of cardiac surgery care that influence outcomes. Additionally, sociodemographic influences can impair cardiac surgery outcomes. For example, <12 years of education increases risk of long-term mortality after cardiac surgery.81 These factors appear to be independent to the biological, physical, and cognitive stress of cardiac surgery.
4.2. Coping
While cardiac surgical care and outcomes continue to improve10, cardiac surgery brings a substantial “unknown”, particularly for the under-informed patient. For example, a cardiac surgery patient is subjected to perioperative protocols for pain, ambulation, and nutrition. These protocols are appropriate for care, but can be different from the patient routine. While most patients will adapt to the short-term change in routine, frail patients have been described to have a maladaptive response to such stressors.82 Similarly, increased anxiety measured preoperatively has been associated with negative outcomes postoperatively.81
Coping with these risks and deviations from routine, draw on the patient's psychological and social functioning. For example, older hospitalized, patients who have low psychosocial resources had increased hospital mortality, longer LOS, discharge to a higher level of care, and increased readmission.52 Additionally, short-term depression and anxiety among older adults following cardiac surgery are partially alleviated when patients employ prayer and are hopeful as part of their coping strategy, but may not impact long-term outcomes.83
4.3 Social Support
Postoperative recovery following cardiac surgery draws on the patient's social structure.84 For example, having home support for daily activities, such as driving to follow up appointments, allows a patient to focus on recovery. A recent report found that married patients had improved mortality or functional recovery relative to separated or widowed patients.85 Social support might allow home-based cardiac rehabilitation which was associated with improved health related quality of life86 relative to usual care. Another study found that patients who lived near the hospital where surgery was performed had lower mortality, presumable due to the ability of social support during and after the surgery.87
4.4 Addiction
In addition, preoperative addiction can be a risk factor for negative surgical outcomes. Pain perception is different in patients with nicotine and opioid addiction. Preoperative alcohol intake is associated with increased complications.88 Smokers were noted to have higher amount of pain medication after CABG compared to non-smokers.89 Routine use of nicotine replacement therapy is not recommended as a randomized study found increased mortality after CABG90 and a meta-analysis of ICU patients was not conclusive.91 Patients with opium dependence have a high threshold for pain medication and a recent study showed that spinal anesthesia may reduce the incidence of postoperative delirium.92
5. Overlap of Biopsychosocial Frailty Domains
5.1 Case Continued
Mr P. and his surgeon have a discussion about cardiac surgery including the perioperative course, the need for follow-up and cardiac risk modification, the potential benefits to his function, and the potential operative, functional, and cognitive risks. In evaluating the patient, the surgeon collects information on the patient's baseline physiologic function, his limited physical performance, his cognitive decline, and his social isolation. The patient wants to discuss the surgery with his daughter before deciding to undergo surgery, as the decision would affect her as well.
5.2 Overlap
In the context of the cardiac surgery stressor, there are vulnerabilities within the biological, psychological, and social singular domains alone that influence poor recovery. Pragmatically, these vulnerabilities do not occur within the isolation of a single domain – there is overlap. For example, increasing age is associated with comorbidity, physical frailty, cognitive impairment, depression, social isolation, socioeconomic status. All of these factors are independently associated with outcomes after cardiac surgery. Logically, we assume that the accumulation of deficits in a cognitively impaired, highly-comorbid, and isolated patient is going to present a less optimal candidate for surgery. However, the intersection of these domains with cardiac surgery outcomes needs exploration to make this definitive statement.
6. Conclusion
With the acceptance that cardiac surgery is a stressor event for the older adult patient, the recovery response following surgery can be utilized to gain an understanding of a population who might not be able to recover from that stress – a frail population. Frailty is a geriatric syndrome14,93 with a constellation of symptoms and many contributing factors. While literature has primarily focused on physical frailty, vulnerability in the psychological or social domain contributes to the vulnerability to the surgical stressor. Deficits in multiple domains likely increase the risk of negative postoperative outcomes. Lastly, despite choosing a focus on cardiac surgery, the literature on the impact of perioperative frailty remains sufficiently heterogeneous. As such this review serves to highlight the need for standardized definitions and measurement tools in older adult undergoing surgery. Preoperative screening is helpful at identifying vulnerabilities, but the clinically applicable tools for this screening need additional prospective clinical investigation.
Supplementary Material
Figure 2. Biopsychosocial Model for Frailty.
As a vulnerability to stress, frailty can occur in the biological, psychological, or social domains. Importantly, there is overlap among the domains, resulting in vulnerability outside of the narrowly defined physical frailty criteria.
Clinical Vignette.
Mr. P is 86 year old man develops typical crushing chest pain with exertion that does not respond to medical therapy. On non-invasive testing he is found to have ischemia with mild activity and a large reversible defect. Catheterization demonstrates three-vessel coronary disease and he is scheduled for cardiac surgery.
Box 1.
Stressors of Cardiac Surgery
| Biological |
| Inflammation |
| Anaesthesia |
| Fluid Shifts |
| Cardiopulmonary Bypass |
| Pain |
| Immobilization |
| Sleep Deprivation |
| Psychological |
| Cognition |
| Depression |
| Anxiety |
| Delirium |
| Self-perception |
| Social |
| Physical limitations |
| Care demands on family |
| Financial resources |
| Access to necessities |
| Community isolation |
| Threats to independence |
Highlights.
Cardiac surgery is a stressful event in the life of an older patient
Recovery from cardiac surgery is dependent on the vulnerabilities of the patient
Vulnerabilities to the surgery occur in biological, psychological and social domains
Overlap of vulnerability domains likely increases the risk of negative outcomes
Acknowledgements
Dr. Rudolph is supported by the VA Health Services Research and Development Center of Innovation in Long Term Services and Supports (CIN 13-419) and the VA QUERI- Geriatrics and Extended Care Partnered Evaluation Center for Community Nursing Homes (PEC 15-465). Dr. Arora is supported by a grant from the Canadian Institute for Health Research and has received an unrestricted educational grant from Pfizer Canada Inc. We are thankful to Ms. Debra D'Allesandro for her insights on this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors declare no conflicts of interest.
References
- 1.Fried LP, Hadley EC, Walston JD, et al. From bedside to bench: research agenda for frailty. Sci Aging Knowledge Environ. 2005;2005(31):pe24. doi: 10.1126/sageke.2005.31.pe24. [DOI] [PubMed] [Google Scholar]
- 2.Quinlan N, Marcantonio ER, Inouye SK, Gill TM, Kamholz B, Rudolph JL. Vulnerability: the crossroads of frailty and delirium. Journal of the American Geriatrics Society. 2011;59(Suppl 2):S262–268. doi: 10.1111/j.1532-5415.2011.03674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Afilalo J, Mottillo S, Eisenberg MJ, et al. Addition of frailty and disability to cardiac surgery risk scores identifies elderly patients at high risk of mortality or major morbidity. Circ Cardiovasc Qual Outcomes. 2012;5(2):222–228. doi: 10.1161/CIRCOUTCOMES.111.963157. [DOI] [PubMed] [Google Scholar]
- 4.Beggs T, Sepehri A, Szwajcer A, Tangri N, Arora RC. Frailty and perioperative outcomes: a narrative review. Can J Anaesth. 2015;62(2):143–157. doi: 10.1007/s12630-014-0273-z. [DOI] [PubMed] [Google Scholar]
- 5.Green P, Woglom AE, Genereux P, et al. The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: a single- center experience. JACC Cardiovasc Interv. 2012;5(9):974–981. doi: 10.1016/j.jcin.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sepehri A, Beggs T, Hassan A, et al. The impact of frailty on outcomes after cardiac surgery: a systematic review. J Thorac Cardiovasc Surg. 2014;148(6):3110–3117. doi: 10.1016/j.jtcvs.2014.07.087. [DOI] [PubMed] [Google Scholar]
- 7.Sundermann S, Dademasch A, Rastan A, et al. One-year follow-up of patients undergoing elective cardiac surgery assessed with the Comprehensive Assessment of Frailty test and its simplified form. Interact Cardiovasc Thorac Surg. 2011;13(2):119–123. doi: 10.1510/icvts.2010.251884. discussion 123. [DOI] [PubMed] [Google Scholar]
- 8.Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54(6):991–1001. doi: 10.1111/j.1532-5415.2006.00745.x. [DOI] [PubMed] [Google Scholar]
- 9.Fedarko NS. The biology of aging and frailty. Clin Geriatr Med. 2011;27(1):27–37. doi: 10.1016/j.cger.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics—2015 Update. Circulation. 2015;131:434–441. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 11.Seco M, Edelman JJ, Forrest P, et al. Geriatric cardiac surgery: chronology vs. biology. Heart Lung Circ. 2014;23(9):794–801. doi: 10.1016/j.hlc.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Altarabsheh SE, Deo SV, Rababa'h AM, et al. Off-pump coronary artery bypass reduces early stroke in octogenarians: a meta-analysis of 18,000 patients. Ann Thorac Surg. 2015;99(5):1568–1575. doi: 10.1016/j.athoracsur.2014.12.057. [DOI] [PubMed] [Google Scholar]
- 13.Singh AK, Maslow AD, Machan JT, et al. Long-term survival after use of internal thoracic artery in octogenarians is gender related. J Thorac Cardiovasc Surg. 2015;150(4):891–899. doi: 10.1016/j.jtcvs.2015.07.052. [DOI] [PubMed] [Google Scholar]
- 14.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. Journal of the American Geriatrics Society. 2007;55(5):780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27(1):17–26. doi: 10.1016/j.cger.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 16.Moore M, Williams B, Ragsdale S, et al. Translating a multifactorial fall prevention intervention into practice: a controlled evaluation of a fall prevention clinic. J Am Geriatr Soc. 2010;58(2):357–363. doi: 10.1111/j.1532-5415.2009.02683.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mariotto A, De Leo D, Buono MD, Favaretti C, Austin P, Naylor CD. Will elderly patients stand aside for younger patients in the queue for cardiac services? Lancet. 1999;354(9177):467–470. doi: 10.1016/S0140-6736(98)12192-X. [DOI] [PubMed] [Google Scholar]
- 18.Bouma BJ, van den Brink RB, Zwinderman K, et al. Which elderly patients with severe aortic stenosis benefit from surgical treatment? An aid to clinical decision making. The Journal of heart valve disease. 2004;13(3):374–381. [PubMed] [Google Scholar]
- 19.Miller DC, Blackstone EH, Mack MJ, et al. Transcatheter (TAVR) versus surgical (AVR) aortic valve replacement: occurrence, hazard, risk factors, and consequences of neurologic events in the PARTNER trial. J Thorac Cardiovasc Surg. 2012;143(4):832–843. e813. doi: 10.1016/j.jtcvs.2012.01.055. [DOI] [PubMed] [Google Scholar]
- 20.Schoenenberger AW, Stortecky S, Neumann S, et al. Predictors of functional decline in elderly patients undergoing transcatheter aortic valve implantation (TAVI). Eur Heart J. 2013;34(9):684–692. doi: 10.1093/eurheartj/ehs304. [DOI] [PubMed] [Google Scholar]
- 21.Webb JG, Wood DA, Ye J, et al. Transcatheter valve-in-valve implantation for failed bioprosthetic heart valves. Circulation. 2010;121(16):1848–1857. doi: 10.1161/CIRCULATIONAHA.109.924613. [DOI] [PubMed] [Google Scholar]
- 22.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 23.Rockwood K. Frailty and its definition: a worthy challenge. J Am Geriatr Soc. 2005;53(6):1069–1070. doi: 10.1111/j.1532-5415.2005.53312.x. [DOI] [PubMed] [Google Scholar]
- 24.Alexander KP, Anstrom KJ, Muhlbaier LH, et al. Outcomes of cardiac surgery in patients > or = 80 years: results from the National Cardiovascular Network. J Am Coll Cardiol. 2000;35(3):731–738. doi: 10.1016/s0735-1097(99)00606-3. [DOI] [PubMed] [Google Scholar]
- 25.Srinivasan AK, Oo AY, Grayson AD, et al. Mid-term survival after cardiac surgery in elderly patients: analysis of predictors for increased mortality. Interact Cardiovasc Thorac Surg. 2004;3(2):289–293. doi: 10.1016/j.icvts.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–744. doi: 10.1093/ejcts/ezs043. discussion 744-735. [DOI] [PubMed] [Google Scholar]
- 27.Anderson RP. First publications from the Society of Thoracic Surgeons National Database. Ann Thorac Surg. 1994;57(1):6–7. doi: 10.1016/0003-4975(94)90355-7. [DOI] [PubMed] [Google Scholar]
- 28.Head SJ, Osnabrugge RL, Howell NJ, et al. A systematic review of risk prediction in adult cardiac surgery: considerations for future model development. Eur J Cardiothorac Surg. 2013;43(5):e121–129. doi: 10.1093/ejcts/ezt044. [DOI] [PubMed] [Google Scholar]
- 29.Park JH, Watt DG, Roxburgh CS, Horgan PG, McMillan DC. Colorectal Cancer, Systemic Inflammation, and Outcome: Staging the Tumor and Staging the Host. Ann Surg. 2016;263(2):326–336. doi: 10.1097/SLA.0000000000001122. [DOI] [PubMed] [Google Scholar]
- 30.Amar D, Zhang H, Park B, Heerdt PM, Fleisher M, Thaler HT. Inflammation and outcome after general thoracic surgery. Eur J Cardiothorac Surg. 2007;32(3):431–434. doi: 10.1016/j.ejcts.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 31.Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Interv Aging. 2014;9:433–441. doi: 10.2147/CIA.S45300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hemmann K, Sirotina M, De Rosa S, et al. The STS score is the strongest predictor of long-term survival following transcatheter aortic valve implantation, whereas access route (transapical versus transfemoral) has no predictive value beyond the periprocedural phase. Interact Cardiovasc Thorac Surg. 2013;17(2):359–364. doi: 10.1093/icvts/ivt132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Afilalo J, Alexander KP, Mack MJ, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol. 2014;63(8):747–762. doi: 10.1016/j.jacc.2013.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 35.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 36.Nobili A, Franchi C, Pasina L, et al. Drug utilization and polypharmacy in an Italian elderly population: the EPIFARM-elderly project. Pharmacoepidemiol Drug Saf. 2011;20(5):488–496. doi: 10.1002/pds.2108. [DOI] [PubMed] [Google Scholar]
- 37.Kennedy JM, van Rij AM, Spears GF, Pettigrew RA, Tucker IG. Polypharmacy in a general surgical unit and consequences of drug withdrawal. Br J Clin Pharmacol. 2000;49(4):353–362. doi: 10.1046/1365-2125.2000.00145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Slotman GJ. Prospectively validated predictions of shock and organ failure in individual septic surgical patients: the Systemic Mediator Associated Response Test. Crit Care. 2000;4(5):319–326. doi: 10.1186/cc715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perl M, Gebhard F, Knoferl MW, et al. The pattern of preformed cytokines in tissues frequently affected by blunt trauma. Shock. 2003;19(4):299–304. doi: 10.1097/00024382-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Holmes JHt, Connolly NC, Paull DL, et al. Magnitude of the inflammatory response to cardiopulmonary bypass and its relation to adverse clinical outcomes. Inflamm Res. 2002;51(12):579–586. doi: 10.1007/pl00012432. [DOI] [PubMed] [Google Scholar]
- 41.Pedersen BK, Bruunsgaard H, Ostrowski K, et al. Cytokines in aging and exercise. Int J Sports Med. 2000;21(Suppl 1):S4–9. doi: 10.1055/s-2000-1444. [DOI] [PubMed] [Google Scholar]
- 42.Cohen HJ. In search of the underlying mechanisms of frailty. J Gerontol A Biol Sci Med Sci. 2000;55(12):M706–708. doi: 10.1093/gerona/55.12.m706. [DOI] [PubMed] [Google Scholar]
- 43.Pawelec G. Immunosenescence and vaccination. Immunity & ageing : I & A. 2005;2:16. doi: 10.1186/1742-4933-2-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Biglioli P, Cannata A, Alamanni F, et al. Biological effects of off-pump vs. on-pump coronary artery surgery: focus on inflammation, hemostasis and oxidative stress. Eur J Cardiothorac Surg. 2003;24(2):260–269. doi: 10.1016/s1010-7940(03)00295-1. [DOI] [PubMed] [Google Scholar]
- 45.Pai JK, Pischon T, Ma J, et al. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004;351(25):2599–2610. doi: 10.1056/NEJMoa040967. [DOI] [PubMed] [Google Scholar]
- 46.Magovern JA, Singh D, Teekell-Taylor L, Scalise D, McGregor W. Preoperative clinical factors are important determinants of the inflammatory state before and after heart surgery. ASAIO J. 2007;53(3):316–319. doi: 10.1097/MAT.0b013e31804b19f7. [DOI] [PubMed] [Google Scholar]
- 47.Ishii Y, Schuessler RB, Gaynor SL, et al. Inflammation of atrium after cardiac surgery is associated with inhomogeneity of atrial conduction and atrial fibrillation. Circulation. 2005;111(22):2881–2888. doi: 10.1161/CIRCULATIONAHA.104.475194. [DOI] [PubMed] [Google Scholar]
- 48.Rudolph JL, Ramlawi B, Kuchel GA, et al. Chemokines are associated with delirium after cardiac surgery. J Gerontol A Biol Sci Med Sci. 2008;63(2):184–189. doi: 10.1093/gerona/63.2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Toth MJ, Poehlman ET. Energetic adaptation to chronic disease in the elderly. Nutrition reviews. 2000;58(3 Pt 1):61–66. doi: 10.1111/j.1753-4887.2000.tb01840.x. [DOI] [PubMed] [Google Scholar]
- 50.Judge JO, Schechtman K, Cress E. The relationship between physical performance measures and independence in instrumental activities of daily living. The FICSIT Group. Frailty and Injury: Cooperative Studies of Intervention Trials. J Am Geriatr Soc. 1996;44(11):1332–1341. doi: 10.1111/j.1532-5415.1996.tb01404.x. [DOI] [PubMed] [Google Scholar]
- 51.Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56(20):1668–1676. doi: 10.1016/j.jacc.2010.06.039. [DOI] [PubMed] [Google Scholar]
- 52.Hoogerduijn JG, de Rooij SE, Grobbee DE, Schuurmans MJ. Predicting functional decline in older patients undergoing cardiac surgery. Age and ageing. 2014;43(2):218–221. doi: 10.1093/ageing/aft165. [DOI] [PubMed] [Google Scholar]
- 53.Visser M, van Venrooij LM, Vulperhorst L, et al. Sarcopenic obesity is associated with adverse clinical outcome after cardiac surgery. Nutrition, metabolism, and cardiovascular diseases : NMCD. 2013;23(6):511–518. doi: 10.1016/j.numecd.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 54.Skelton DA, Greig CA, Davies JM, Young A. Strength, power and related functional ability of healthy people aged 65-89 years. Age and ageing. 1994;23(5):371–377. doi: 10.1093/ageing/23.5.371. [DOI] [PubMed] [Google Scholar]
- 55.Morley JE. Anorexia, sarcopenia, and aging. Nutrition. 2001;17(7-8):660–663. doi: 10.1016/s0899-9007(01)00574-3. [DOI] [PubMed] [Google Scholar]
- 56.Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg. 1999;134(1):36–42. doi: 10.1001/archsurg.134.1.36. [DOI] [PubMed] [Google Scholar]
- 57.Umezawa-Makikado LD, Flordelís-Lasierra JL, Pérez-Vela JL, Montejo-González JC. Early Enteral Nutrition in Postoperative Cardiac Surgery Patients with Severe Hemodynamic Failure and Venoarterial (VA) Extracorporeal Membrane Oxygenation (ECMO). In: Rajendram R, Preedy VR, Patel VB, editors. Diet and Nutrition in Critical Care. Springer; New York: 2014. pp. 1–14. [Google Scholar]
- 58.Hogue CW, Jr., Lappas GD, Creswell LL, et al. Swallowing dysfunction after cardiac operations. Associated adverse outcomes and risk factors including intraoperative transesophageal echocardiography. J Thorac Cardiovasc Surg. 1995;110(2):517–522. doi: 10.1016/S0022-5223(95)70249-0. [DOI] [PubMed] [Google Scholar]
- 59.van Venrooij LM, de Vos R, Borgmeijer-Hoelen MM, Haaring C, de Mol BA. Preoperative unintended weight loss and low body mass index in relation to complications and length of stay after cardiac surgery. Am J Clin Nutr. 2008;87(6):1656–1661. doi: 10.1093/ajcn/87.6.1656. [DOI] [PubMed] [Google Scholar]
- 60.Rockwood K, Davis H, MacKnight C, et al. The Consortium to Investigate Vascular Impairment of Cognition: methods and first findings. Can J Neurol Sci. 2003;30(3):237–243. doi: 10.1017/s0317167100002663. [DOI] [PubMed] [Google Scholar]
- 61.Selnes OA, Vinters HV. Vascular cognitive impairment. Nat Clin Pract Neurol. 2006;2(10):538–547. doi: 10.1038/ncpneuro0294. [DOI] [PubMed] [Google Scholar]
- 62.Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Silbersweig D, Charlson M. Clinically defined vascular depression. Am J Psychiatry. 1997;154(4):562–565. doi: 10.1176/ajp.154.4.562. [DOI] [PubMed] [Google Scholar]
- 63.Horne D, Kehler DS, Kaoukis G, et al. Impact of physical activity on depression after cardiac surgery. Can J Cardiol. 2013;29(12):1649–1656. doi: 10.1016/j.cjca.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 64.Horne D, Kehler S, Kaoukis G, et al. Depression before and after cardiac surgery: do all patients respond the same? J Thorac Cardiovasc Surg. 2013;145(5):1400–1406. doi: 10.1016/j.jtcvs.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 65.Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59(5):1289–1295. doi: 10.1016/0003-4975(95)00106-u. [DOI] [PubMed] [Google Scholar]
- 66.Newman S, Stygall J, Hirani S, Shaefi S, Maze M. Postoperative cognitive dysfunction after noncardiac surgery: a systematic review. Anesthesiology. 2007;106(3):572–590. doi: 10.1097/00000542-200703000-00023. [DOI] [PubMed] [Google Scholar]
- 67.Rudolph JL, Schreiber KA, Culley DJ, et al. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand. 2010;54(6):663–677. doi: 10.1111/j.1399-6576.2010.02236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.van Dijk D, Spoor M, Hijman R, et al. Cognitive and cardiac outcomes 5 years after off-pump vs on-pump coronary artery bypass graft surgery. JAMA. 2007;297(7):701–708. doi: 10.1001/jama.297.7.701. [DOI] [PubMed] [Google Scholar]
- 69.Selnes OA, Grega MA, Bailey MM, et al. Cognition 6 years after surgical or medical therapy for coronary artery disease. Ann Neurol. 2008;63(5):581–590. doi: 10.1002/ana.21382. [DOI] [PubMed] [Google Scholar]
- 70.Newman MF, Kirchner JL, Phillips-Bute B, et al. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344(6):395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 71.Rudolph JL, Jones RN, Levkoff SE, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119(2):229–236. doi: 10.1161/CIRCULATIONAHA.108.795260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rudolph JL, Inouye SK, Jones RN, et al. Delirium: an independent predictor of functional decline after cardiac surgery. Journal of the American Geriatrics Society. 2010;58(4):643–649. doi: 10.1111/j.1532-5415.2010.02762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gleason LJ, Schmitt EM, Kosar CM, et al. Effect of Delirium and Other Major Complications on Outcomes After Elective Surgery in Older Adults. JAMA Surg. 2015;150(12):1134–1140. doi: 10.1001/jamasurg.2015.2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jung P, Pereira MA, Hiebert B, et al. The impact of frailty on postoperative delirium in cardiac surgery patients. J Thorac Cardiovasc Surg. 2015;149(3):869–875. e861–862. doi: 10.1016/j.jtcvs.2014.10.118. [DOI] [PubMed] [Google Scholar]
- 75.Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet. 1998;351(9106):857–861. doi: 10.1016/s0140-6736(97)07382-0. [DOI] [PubMed] [Google Scholar]
- 76.Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108(1):18–30. doi: 10.1097/01.anes.0000296071.19434.1e. [DOI] [PubMed] [Google Scholar]
- 77.Nadelson MR, Sanders RD, Avidan MS. Perioperative cognitive trajectory in adults. Br J Anaesth. 2014;112(3):440–451. doi: 10.1093/bja/aet420. [DOI] [PubMed] [Google Scholar]
- 78.Ravven S, Bader C, Azar AR, Rudolph JL. Depressive Symptoms after CABG Surgery: a meta- analysis. Harvard Rev Psychiatry. 2013;21(2):59–69. doi: 10.1097/HRP.0b013e31828a3612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Connerney I, Shapiro PA, McLaughlin JS, Bagiella E, Sloan RP. Relation between depression after coronary artery bypass surgery and 12-month outcome: a prospective study. Lancet. 2001;358(9295):1766–1771. doi: 10.1016/S0140-6736(01)06803-9. [DOI] [PubMed] [Google Scholar]
- 80.Ried M, Lunz D, Kobuch R, et al. Gender's impact on outcome in coronary surgery with minimized extracorporeal circulation. Clinical research in cardiology : official journal of the German Cardiac Society. 2012;101(6):437–444. doi: 10.1007/s00392-011-0410-4. [DOI] [PubMed] [Google Scholar]
- 81.Cserep Z, Losoncz E, Balog P, et al. The impact of preoperative anxiety and education level on long-term mortality after cardiac surgery. J Cardiothorac Surg. 2012;7:86. doi: 10.1186/1749-8090-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Andrew MK, Fisk JD, Rockwood K. Psychological well-being in relation to frailty: a frailty identity crisis? Int Psychogeriatr. 2012;24(8):1347–1353. doi: 10.1017/S1041610212000269. [DOI] [PubMed] [Google Scholar]
- 83.Ai AL, Ladd KL, Peterson C, Cook CA, Shearer M, Koenig HG. Long-term Adjustment After Surviving Open Heart Surgery: The Effect of Using Prayer for Coping Replicated in a Prospective Design. Gerontologist. 2010;50(6):798–809. doi: 10.1093/geront/gnq046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hoogendijk EO, van Hout HP, van der Horst HE, et al. Do psychosocial resources modify the effects of frailty on functional decline and mortality? J Psychosom Res. 2014;77(6):547–551. doi: 10.1016/j.jpsychores.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 85.Neuman MD, Werner RM. Marital Status and Postoperative Functional Recovery. JAMA Surg. 2015 doi: 10.1001/jamasurg.2015.3240. online:E1-E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Salavati M, Fallahinia G, Vardanjani AE, Rafiei H, Mousavi S, Torkamani M. Comparison Between Effects of Home Based Cardiac Rehabilitation Programs Versus Usual Care on the Patients' Health Related Quality of Life After Coronary Artery Bypass Graft. Glob J Health Sci. 2015;8(4):49795. doi: 10.5539/gjhs.v8n4p196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chou S, Deily ME, Li S. Travel distance and health outcomes for scheduled surgery. Medical care. 2014;52(3):250–257. doi: 10.1097/MLR.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 88.Bradley KA, Rubinsky AD, Sun H, et al. Alcohol screening and risk of postoperative complications in male VA patients undergoing major non-cardiac surgery. J Gen Intern Med. 2011;26(2):162–169. doi: 10.1007/s11606-010-1475-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Creekmore FM, Lugo RA, Weiland KJ. Postoperative opiate analgesia requirements of smokers and nonsmokers. The Annals of pharmacotherapy. 2004;38(6):949–953. doi: 10.1345/aph.1D580. [DOI] [PubMed] [Google Scholar]
- 90.Paciullo CA, Short MR, Steinke DT, Jennings HR. Impact of nicotine replacement therapy on postoperative mortality following coronary artery bypass graft surgery. The Annals of pharmacotherapy. 2009;43(7):1197–1202. doi: 10.1345/aph.1L423. [DOI] [PubMed] [Google Scholar]
- 91.Wilby KJ, Harder CK. Nicotine replacement therapy in the intensive care unit: a systematic review. J Intensive Care Med. 2014;29(1):22–30. doi: 10.1177/0885066612442053. [DOI] [PubMed] [Google Scholar]
- 92.Tabatabaie O, Matin N, Heidari A, et al. Spinal anesthesia reduces postoperative delirium in opium dependent patients undergoing coronary artery bypass grafting. Acta anaesthesiologica Belgica. 2015;66(2):49–54. [PubMed] [Google Scholar]
- 93.Boyd CM, Xue QL, Simpson CF, Guralnik JM, Fried LP. Frailty, hospitalization, and progression of disability in a cohort of disabled older women. Am J Med. 2005;118(11):1225–1231. doi: 10.1016/j.amjmed.2005.01.062. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.