Abstract
Quantitative assessments of the health status of a population are essential to make decisions and set priorities in the field of public health. Changing epidemiologic patterns increase the demand for comprehensive estimates of population health across the full health spectrum, including non-communicable diseases and injuries. Burden of disease (BoD) analysis has helped meet this need. With the success of the Global Burden of Disease (GBD) Study, the BoD technique has become predominantly associated with the GBD approach and its methodology using disability-adjusted life year (DALY) has been rapidly disseminated and generally accepted over the last several years. The first Korean BoD study using the DALY metric was presented in 2002. Various BoD studies have since been conducted, but the DALY concept has remained primarily academic and has not yet been actively utilized in the health policy arena. Here, we review the DALY metric and population-based Korean BoD studies using national health data, with the intent of increasing the understanding of their value and their potential role in strengthening future assessments of the Korean population’s health status.
Keywords: Burden of Disease, Disability-Adjusted Life Year, Population Health, Korea
Graphical Abstract
INTRODUCTION
Quantitative assessments of the health status of a population are important for decision-making and priority-setting processes in the field of public health (1). The health status and major health problems have traditionally been identified using metrics including cause-specific mortality rates, life expectancies, and incidence and prevalence rates (1). This approach is becoming unwieldy, however, when monitoring and comparing a number of problems over time, or assessing the impact of specific health interventions, as is done in cost-effectiveness analyses (2). Furthermore, recent changes in demographic and epidemiologic factors are having a major impact on the health status of many populations. For example, non-communicable diseases (NCDs) and their often non-fatal but long-term impact on health has become a major concern, leading researchers to question whether the observed gains in life expectancy have been accompanied by improvements in health status (1,3,4,5). Thus, methods to measure a population’s full health spectrum, including NCDs and injuries are required.
Burden of disease (BoD) analysis has helped meet this need (1). The Global Burden of Disease (GBD) study, launched by the World Bank and the World Health Organization (WHO) in 1991 (6-10), represents a major advance in the quantification of the impact of diseases, injuries, and risk factors and its results have increased our understanding of basic descriptive epidemiology of global population health (11). With the success of the GBD study, the BoD technique has become predominantly associated with the GBD approach and its methodology using disability-adjusted life year (DALY) is now widely accepted (1).
The first national BoD study in Korea using the DALY metric was presented in 2002 (12), and many diverse BoD studies have been conducted since (13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35). The DALY concept, however, is primarily used academically and has not yet been actually utilized in the health policy arena. Therefore, in this article, we review the DALY metric and population-based Korean BoD (KBD) studies, with the intent of increasing the understanding of their value and their potential role in strengthening future assessments of the Korean population’s health status.
DALY AS A SUMMARY MEASURE OF POPULATION HEALTH
Summary measures of population health (SMPH) combine information on mortality with that on the vast array of non-fatal health outcomes so as to represent a population’s health as a single numerical index (3,36). Such summary measures have a range of potential applications, such as comparing the health of one population with that of another, monitoring changes in the health of a given population over time, identifying and quantifying health inequalities within a population, providing appropriate and balanced attention to the effects of non-fatal health outcomes on overall population health, prioritizing health service delivery and planning, informing research and development efforts, and analyzing the benefits of health interventions to enable cost-effectiveness analyses (3,37).
The wide range of summary measures developed in the past fall into two broad categories: health expectancies and health gaps (2,3). Both classes use time as an appropriate metric for measuring the impact of both mortality and non-fatal health outcomes (3). Health expectancies estimate the average time that a person could expect to live in a defined state of health and are useful for summarizing the average health attainment of a population and for communication to a general audience (38). Health gaps extend the notion of mortality gaps to include time lived in states other than ideal health, and are used to measure the difference between the actual health of a population and a defined ideal (3,11). While health expectancy measures do not naturally lend themselves to disaggregation by categorically defined causes, health gap measures permit categorical attribution of the fatal and non-fatal BoDs and injuries to an exhaustive and mutually exclusive set of disease and injury causes (2,39). Because one of the fundamental goals in choosing an SMPH for quantifying the GBD is to enable identification of the relative magnitude of different health problems, including diseases, injuries, and risk factors, a health gap measure was chosen for the GBD project and a new SMPH, the DALY, was developed (2,39,40,41). Driven by the influential GBD projects (3,42,43,44,45,46,47,48,49,50), the DALY has attracted the most attention among composite health gap measures and become the dominant SMPH (1).
Years of life lost (YLL), years lived with disability (YLD), and their sum, the DALY
The DALY, by aggregating information on mortality and morbidity into a single number in units of healthy life lost, provides a unique perspective that integrates fatal and non-fatal outcomes while still allowing each to be examined separately (51). One DALY is one lost year of healthy life (52). To allow aggregation and comparison of the burdens of different diseases and injuries, mortality is quantified as years of life lost (YLLs) by taking into account the age at which death occurs. YLL is computed by multiplying the number of deaths at each age by the standard life expectancy for that age (53). Morbidity is converted to years lived with disability (YLDs). YLD represents the lost years of full health. By means of disability weights, the degree of disability imposed by each condition on those who live with the disease is scaled from 0 (perfect health) to 1 (equivalent to death) (34,45,52,53,54,55). YLD is computed by multiplying the number of incident cases by their expected mean duration and the disability weight of the disease (53). These metrics, like all other SMPHs, explicitly or implicitly include a series of social value choices that must be decided in the planning process — namely, reference life expectancy, disability weights, time discounting, and age weights (3,56,57). Since the initial GBD study in 1990, these value choices have been extensively debated (3,42,43,44,45,46,47,48,49,50,57). In GBD 2010, a simpler version of DALYs was introduced (57,58) by the Institute for Health Metrics and Evaluation (IHME). That study used prevalence YLD rather than incidence YLD, and dropped time discounting and age weights, thereby resulting in a YLD computation procedure in which the prevalence of a sequela is multiplied by its associated disability weight (57). While the YLL calculation inherently takes an incidence-based perspective, non-fatal health outcomes can be quantified using either incidence- or prevalence-based measures (53,59,60,61). This issue is discussed further later in this article.
Ethics statement
The study protocol was approved by Korea University’s institutional review board (1040548-KU-IRB-13-164-A-1[E-A-1][E-A-1]).
MEASURING KOREAN POPULATION HEALTH USING THE DALY METRIC
The various KBD DALY measurement studies (13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35) can be narrowed down to two major works supported by the Ministry of Health and Welfare. The first, KBD 2002, was a 4-year research project and involved the collaboration of five institutions (Seoul National University, the Korea Institute for Health and Social Affairs, Kyung Hee University, Sungkyunkwan University, and Hanyang University). Using national population health data, this project demonstrated the applicability of DALYs for KBD analyses. The project provided a set of epidemiological estimates, YLLs, YLDs, and DALYs for 150 diseases and 3 risk factors for the reference year 2002. Key methodology and results were reported in 2007 (16). The second work, KBD 2012, is a recent 5-year project involving four collaborating institutions (Korea University, University of Ulsan, Ewha Womans University, and Kyung Hee University). Key findings from the first phase of the work have been published (29,30,31,32,33,34,35). The study covered 313 diseases and injuries for the reference year 2012, using improved methodology and an enhanced, higher-quality national database.
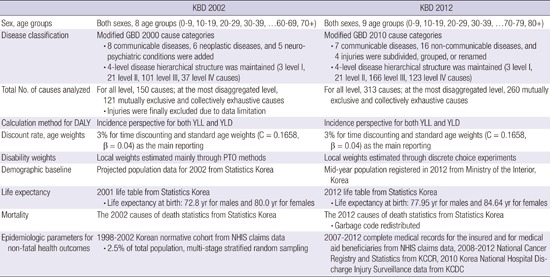
KBD 2002 vs. KBD 2012
While the basic concept and approach of the two major studies — KBD 2002 and KBD 2012 — were consistent with the original GBD study (3), some modifications were made to adapt them to the Korean population. Table 1 summarizes the methods and data sources of each study. In KBD 2002, a Korean normative cohort was constructed to estimate the epidemiologic data. The cohort was a representative sample of 1,209,693 participants randomly selected from National Health Insurance Service (NHIS) claims data from 1998 to 2002, which covers about 2.5% of the total eligible Korean population. Stratified random sampling was conducted with proportional allocation by age group, sex, area of residence, and type of insurance. To compensate for the limitations of the medical utilization database, morbidity estimates were determined by reviewing medical records. The severity of each non-fatal health outcome was quantified by medical professionals using measurement methods including person trade-off, time trade-off, visual analogue scale, and standard gamble. Cause-specific mortality was estimated from Statistics Korea 2002 data.
Table 1. Summary of methods and data sources for KBD 2002 and KBD 2012.
| KBD 2002 | KBD 2012 | |
|---|---|---|
| Sex, age groups | Both sexes, 8 age groups (0–9, 10–19, 20–29, 30–39, …60–69, 70+) | Both sexes, 9 age groups (0–9, 10–19, 20–29, 30–39, …70–79, 80+) |
| Disease classification | Modified GBD 2000 cause categories | Modified GBD 2010 cause categories |
| · 8 communicable diseases, 6 neoplastic diseases, and 5 neuro-psychiatric conditions were added | · 7 communicable diseases, 16 non-communicable diseases, and 4 injuries were subdivided, grouped, or renamed | |
| · 4-level disease hierarchical structure was maintained (3 level I, 21 level II, 101 level III, 37 level IV causes) | · 4-level disease hierarchical structure was maintained (3 level I, 21 level II, 166 level III, 123 level IV causes) | |
| Total No. of causes analyzed | For all level, 150 causes; at the most disaggregated level, 121 mutually exclusive and collectively exhaustive causes | For all level, 313 causes; at the most disaggregated level, 260 mutually exclusive and collectively exhaustive causes |
| · Injuries were finally excluded due to data limitation | ||
| Calculation method for DALY | Incidence perspective for both YLL and YLD | Incidence perspective for both YLL and YLD |
| Discount rate, age weights | 3% for time discounting and standard age weights (C = 0.1658, β = 0.04) as the main reporting | 3% for time discounting and standard age weights (C = 0.1658, β = 0.04) as the main reporting |
| Disability weights | Local weights estimated mainly through PTO methods | Local weights estimated through discrete choice experiments |
| Demographic baseline | Projected population data for 2002 from Statistics Korea | Mid-year population registered in 2012 from Ministry of the Interior, Korea |
| Life expectancy | 2001 life table from Statistics Korea | 2012 life table from Statistics Korea |
| · Life expectancy at birth: 72.8 yr for males and 80.0 yr for females | · Life expectancy at birth: 77.95 yr for males and 84.64 yr for females | |
| Mortality | The 2002 causes of death statistics from Statistics Korea | The 2012 causes of death statistics from Statistics Korea |
| · Garbage code redistributed | ||
| Epidemiologic parameters for non-fatal health outcomes | 1998–2002 Korean normative cohort from NHIS claims data | 2007–2012 complete medical records for the insured and for medical aid beneficiaries from NHIS claims data, 2008–2012 National Cancer Registry and Statistics from KCCR, 2010 Korea National Hospital Discharge Injury Surveillance data from KCDC |
| · 2.5% of total population, multi-stage stratified random sampling |
KBD = Korean Burden of Disease, GBD = Global Burden of Disease, DALY = disability-adjusted life year, YLL = years of life lost due to premature mortality, YLD = years lived with disability, PTO = Person Trade-off, NHIS = National Health Insurance Service, KCCR = Korea Central Cancer Registry, KCDC = Korea Centers for Disease Control and Prevention.
In KBD 2012, considerable effort was made to address the limitations of KBD 2002: the cause list was expanded to encompass 313 causes, the complete medical records for 2007–2012 were used instead of sample cohort data, and data from the Korea Central Cancer Registry and the Korea Centers for Disease Control and Prevention were added to improve the precision of cancer and injury estimates. Disability weights were estimated through discrete choice experiments. For cause-specific mortality, “garbage code” redistribution algorithms were used to improve accuracy of the problematic underlying causes of death in the data. Although we are fairly confident in the values estimated from these refined data and enhanced methodologies, there remain opportunities to enhance the precision of the underlying epidemiological data. One option is to combine treatment or prescription information with the main diagnostic codes in NHIS claims data analyses. An uncertainty level could also be provided based on sensitivity analysis of different extraction criteria. Additionally, consistent longitudinal epidemiologic studies and population-based surveys would support these results, providing supplementary information that could validate the epidemiological indicators or indicate how the NHIS claims data could be adjusted to reflect population estimates more precisely.
While these single-year works provide valuable comprehensive health status assessments and indicate the important contributors to a population’s BoD at a given time(Tables 2 and 3), they do not allow the study of changing epidemiologic patterns over time. To continue providing evidence to guide policy and practice priorities (62), such information should be produced and updated on a regular basis using consistent data and metrics. This would strengthen health assessments using the DALY metric in Korea and enhance their value for policy and program development (63).
Table 2. Top 10 specific causes of disability-adjusted life years (DALYs) in KBD 2002.
| Rank | Specific cause | ICD-10 codes | DW | YLLs | YLDs | DALYs |
|---|---|---|---|---|---|---|
| 1 | Diabetes mellitus | E10–E14 | 0.39 | 199 | 770 | 970 |
| 2 | Cerebrovascular disease | I60–I69 | 0.80 | 533 | 404 | 937 |
| 3 | Asthma | J45–J46 | 0.50 | 50 | 659 | 709 |
| 4 | Peptic ulcer disease | K25–K27 | 0.15 | 9 | 667 | 676 |
| 5 | Ischemic heart disease | I20–I25 | 0.73 | 199 | 324 | 523 |
| 6 | Cirrhosis of the liver | K70, K74 | 0.79 | 278 | 129 | 407 |
| 7 | Rheumatoid arthritis | M05–M06 | 0.50 | 4 | 355 | 359 |
| 8 | Unipolar major depression | F32 | 0.66 | 1 | 330 | 331 |
| 9 | Liver cancer | C22 | 0.87 | 262 | 37 | 299 |
| 10 | Stomach cancer | C16 | 0.85 | 230 | 61 | 291 |
YLLs, YLDs, and DALYs per 100,000 population. Sums may not add up to exact total due to rounding.
KBD = Korean Burden of Disease, ICD-10 = International Classification of Diseases 10th revision, DW = disability weight, YLL = years of life lost due to premature mortality, YLD = years lived with disability.
Table 3. Top 10 specific causes of disability-adjusted life years (DALYs) in KBD 2012.
| Rank | Specific cause | ICD-10 codes | DW | YLLs | YLDs | DALYs |
|---|---|---|---|---|---|---|
| 1 | Diabetes mellitus | E100, E101, E103–E111, E113–E121, E123–E131, E133–E139 | 0.59 | 138 | 2,042 | 2,181 |
| 2 | Low back pain | M469, M47, M480, M481, M482, M488, M489, M51, M52, M530, M533, M538, M539, M54 | 0.31 | 0 | 1,915 | 1,915 |
| 3 | Chronic obstructive pulmonary disease | J40–J44, J47 | 0.69 | 84 | 1,221 | 1,305 |
| 4 | Ischemic heart disease | I20–I25 | 0.79 | 308 | 703 | 1,011 |
| 5 | Ischemic stroke | I63, I65, I66, I670, I671, I672, I673, I675, I676, I677, I678, I679, I693 | 0.81 | 186 | 767 | 954 |
| 6 | Cirrhosis of the liver | B18, I85, K70, K717, K72, K73, K74, K752, K753, K754, K758, K759, K766, K767, K769 | 0.69 | 204 | 715 | 919 |
| 7 | Falls | W00–W19 | 0.61 | 71 | 684 | 755 |
| 8 | Osteoarthritis | M15–M19 | 0.37 | 0 | 701 | 701 |
| 9 | Motorized vehicle with three or more wheels | V30–V79, V872–V873 | 0.59 | 109 | 588 | 697 |
| 10 | Self-harm | X60–X67, X68, X69, X70, X71, X72–X74, X75, X76–X77, X78–X83 | 0.61 | 573 | 27 | 600 |
YLLs, YLDs, and DALYs per 100,000 population. Sums may not add up to exact total due to rounding.
KBD = Korean Burden of Disease, ICD-10 = International Classification of Diseases 10th revision, DW = disability weight, YLL = years of life lost due to premature mortality, YLD = years lived with disability.
KBD vs. GBD
While the GBD study provided an overall picture of global health, it depended on sparse and often inconsistent data (54), and it used the same disability weights for everyone in a given health state and the same ideal life expectancy for all regions of the world. Thus, the data are not likely to be equally descriptive for all nations. We conducted the KBD, on the other hand, as a national study. We adopted the GBD concepts but used Korean data sources that reflect the Korean health status and disease states. The current KBD methodology is described elsewhere (29,30,31,32,33,34,35). We used life expectancy tables produced by Statistics Korea, derived local disability weights, and applied time discounting and standard age weights to incidence-based YLLs and YLDs. We extracted basic epidemiologic parameters mainly from the claims data of NHIS, the national insurer that covers about 97% of the population and is presumed to have complete medical records for both the insured and medical aid beneficiaries (64). Even with its limitations, NHIS represents the overall population trends in health care needs. Because the data and methods used by the KBD and GBD differed, their results are not directly comparable.
Incidence-based DALYs vs. Prevalence-based DALYs
In the GBD 1990 and subsequent WHO updates, DALYs were computed from incidence-based YLDs to ensure consistency with the inherently incidence-based YLL calculations (57,59). Therefore, the sum of the two components (i.e., DALYs) estimates the future stream of healthy years that will be lost as a result of the current-year incidences of specific conditions (11). If both fatal and non-fatal outcomes are analyzed using prevalence, a health gap could be measured based on the prevalence of non-fatal health outcomes and of deceased individuals who would have lost years of life in the reference time period (3). However, the self-described prevalence-based studies actually compute incidence-based YLLs and prevalence-based YLDs and then simply combine the two components. This inconsistency calls into question the utility of the resulting DALYs, which could best be described as the years of future life lost to premature deaths in the reference year plus the amount of disability experienced in the reference year (61). This was considered an acceptable method in IHME’s GBD 2010 (57,61), and the methods and estimates from that study contributed to the recent updates of the WHO’s Global Health Estimates for mortality, causes of death, and disease burden (5,59). In terms of YLDs, incidence-based estimates describe health loss resulting from newly diagnosed cases in the reference year, and thus reflect more recent epidemiological trends. Prevalence-based estimates, on the other hand, describe current health losses arising from incident or prevalent cases in the reference time period. Taking advantages of both methods as appropriate, the ongoing KBD project has decided to calculate both incidence- and prevalence-based YLDs and will perform comparative analyses in the 2017 follow-up study.
FUTURE DIRECTIONS
Our recent finding that non-fatal outcomes play a more important role than deaths in the nation’s disease burden (29,30) highlights the usefulness of DALYs for describing the overall health status of a population (1,3,4,5). Furthermore, NCD prevalence is expected to increase over the next decades (65) and concurrently, effective interventions and advances in medical technology are expected to allow those with NCDs to live longer in relatively good health. Thus, assessing the magnitude of a nation’s disease burden, rather than calculating the number of deaths, prevalence, or incidence cases, would be a more helpful approach when devising strategies to control population health. Our suggested priorities for future BoD studies in Korea are the following.
Extending the range of DALY analysis
In BoD studies, the burden can be readily disaggregated by cause at the level of diseases and risk factors, and it can be estimated for any population subgroup (66). Linking the burden with risk factors can yield insight into how best to investigate avoidable disease. Several factor- or cause-specific analyses have been conducted, but population-level, comprehensive, and comparative assessments of the disease burden attributable to specific risk factors have not been performed in Korea. The KBD project expects to assess 29 common Korean risk factors in public health. Identifying risk factors and the contribution of those factors to the burden is important, but methods to reduce risk factors at the individual- and population-levels should be studied simultaneously (67). Our KBD project team is also developing a cost-effectiveness analysis model using the CHOosing Interventions that are Cost-Effective (WHO-CHOICE) method (68). Information on intervention effectiveness is expected to provide a useful evidence base for setting priorities to maximize population health with limited resources (68). In addition, regional and socioeconomic analyses can lead to targeted health planning and allow monitoring of inequalities in the distribution of health care services. More broadly, the usefulness of DALYs should be evaluated further as we develop more practical health statistics to meet the nation’s specific health planning needs.
Improving estimate precision
The accuracy of DALYs depends primarily on the accuracy of the underlying epidemiologic data (52,69,70). The KBD project is working to address the study’s limitations and methodological problems to improve this accuracy (29). We hope to refine the methods and improve the validity of the DALY estimates so we can more precisely measure Korean population health (66).
Producing comparative and consistent evidence
While GBD paints the big picture and compares diseases, injuries, and risk factors in different world populations (57), KBD quantifies the national burden of disease in Korea. The KBD study would be more meaningful if it could track changes that occur over time so that patterns, progress, and new challenges could be identified. Estimates for a wide range of health problems should be produced and updated regularly and consistently (29,54,57). This broad body of evidence will strengthen the KBD analysis, which will help guide future health policy, interventions, and research.
Footnotes
Funding: This study was supported by a grant from the Korean Health Technology R & D Project, Ministry of Health and Welfare, Republic of Korea (Study No. HI13C0729).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study supervision: Yoon SJ. Study conception and design: Yoon J. Writing manuscript: Yoon J. Critical revision: Yoon SJ. Approval of the final manuscript: all authors.
References
- 1.Pinheiro P, Plaß D, Krämer A. The burden of disease approach for measuring population health. In: Krämer A, Khan MM, Kraas F, editors. Health in Megacities and Urban Areas. Heidelberg: Physica-Verlag; 2011. pp. 21–38. [Google Scholar]
- 2.Mathers CD, Lopez AD, Murray CJ. The burden of disease and mortality by condition: data, methods, and results for 2001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ, editors. Global Burden of Disease and Risk Factors. Washington, D.C.: World Bank; 2006. pp. 45–240. [PubMed] [Google Scholar]
- 3.Murray CJ, Salomon JA, Mathers CD, Lopez AD. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva: World Health Organization; 2002. [Google Scholar]
- 4.van der Maas PJ. Applications of summary measures of population health. In: Murray CJ, Salomon JA, Mathers CD, Lopez AD, editors. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva: World Health Organization; 2002. pp. 53–60. [Google Scholar]
- 5.Department of Health Statistics and Information Systems, World Health Organization. WHO Methods and Data Sources for Country-level Causes of Death 2000??012. Global Health Estimates Technical Paper WHO/HIS/HSI/GHE/2014.7. Geneva: World Health Organization; 2014. [Google Scholar]
- 6.World Bank. World Development Report 1993: Investing in Health. New York, NY: Oxford University Press; 1993. [Google Scholar]
- 7.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: global burden of disease study. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 8.Murray CJ, Lopez AD. Regional patterns of disability-free life expectancy and disability-adjusted life expectancy: global burden of disease study. Lancet. 1997;349:1347–1352. doi: 10.1016/S0140-6736(96)07494-6. [DOI] [PubMed] [Google Scholar]
- 9.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 10.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: global burden of disease study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 11.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ, editors. Global Burden of Disease and Risk Factors. Washington, D.C.: World Bank; 2006. [PubMed] [Google Scholar]
- 12.Yoon SJ, Lee H, Shin Y, Kim YI, Kim CY, Chang H. Estimation of the burden of major cancers in Korea. J Korean Med Sci. 2002;17:604–610. doi: 10.3346/jkms.2002.17.5.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee H, Yoon SJ, Ahn HS. Measuring the burden of major cancers due to smoking in Korea. Cancer Sci. 2006;97:530–534. doi: 10.1111/j.1349-7006.2006.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park JH, Yoon SJ, Lee HY, Cho HS, Lee JY, Eun SJ, Park JH, Kim Y, Kim YI, Shin YS. Estimating the burden of psychiatric disorder in Korea. J Prev Med Public Health. 2006;39:39–45. [PubMed] [Google Scholar]
- 15.Lee H, Yoon SJ, Ahn HS, Moon OR. Estimation of potential health gains from reducing multiple risk factors of stroke in Korea. Public Health. 2007;121:774–780. doi: 10.1016/j.puhe.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Yoon SJ, Bae SC, Lee SI, Chang H, Jo HS, Sung JH, Park JH, Lee JY, Shin Y. Measuring the burden of disease in Korea. J Korean Med Sci. 2007;22:518–523. doi: 10.3346/jkms.2007.22.3.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hong KS. Disability-adjusted life years analysis: implications for stroke research. J Clin Neurol. 2011;7:109–114. doi: 10.3988/jcn.2011.7.3.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong KS, Ali LK, Selco SL, Fonarow GC, Saver JL. Weighting components of composite end points in clinical trials: an approach using disability-adjusted life-years. Stroke. 2011;42:1722–1729. doi: 10.1161/STROKEAHA.110.600106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong KS, Kim J, Cho YJ, Seo SY, Hwang SI, Kim SC, Kim JE, Kim A, Cho JY, Park HK, et al. Burden of ischemic stroke in Korea: analysis of disability-adjusted life years lost. J Clin Neurol. 2011;7:77–84. doi: 10.3988/jcn.2011.7.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim YM, Kim JW, Lee HJ. Burden of disease attributable to air pollutants from municipal solid waste incinerators in Seoul, Korea: a source-specific approach for environmental burden of disease. Sci Total Environ. 2011;409:2019–2028. doi: 10.1016/j.scitotenv.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 21.Chung SE, Cheong HK, Park JH, Kim HJ. Burden of disease of multiple sclerosis in Korea. Epidemiol Health. 2012;34:e2012008. doi: 10.4178/epih/e2012008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oh IH, Yoon SJ, Yoon TY, Choi JM, Choe BK, Kim EJ, Kim YA, Seo HY, Park YH. Health and economic burden of major cancers due to smoking in Korea. Asian Pac J Cancer Prev. 2012;13:1525–1531. doi: 10.7314/apjcp.2012.13.4.1525. [DOI] [PubMed] [Google Scholar]
- 23.Kim EJ, Yoon SJ, Jo MW, Kim HJ. Measuring the burden of chronic diseases in Korea in 2007. Public Health. 2013;127:806–813. doi: 10.1016/j.puhe.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 24.Kim YM, Park JH, Choi K, Noh SR, Choi YH, Cheong HK. Burden of disease attributable to the Hebei Spirit oil spill in Taean, Korea. BMJ Open. 2013;3:e003334. doi: 10.1136/bmjopen-2013-003334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park JH, Eum JH, Bold B, Cheong HK. Burden of disease due to dementia in the elderly population of Korea: present and future. BMC Public Health. 2013;13:293. doi: 10.1186/1471-2458-13-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park JH, Lee KS, Choi KS. Burden of cancer in Korea during 2000-2020. Cancer Epidemiol. 2013;37:353–359. doi: 10.1016/j.canep.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 27.Lee KS, Park JH. Burden of disease in Korea during 2000-10. J Public Health (Oxf) 2014;36:225–234. doi: 10.1093/pubmed/fdt056. [DOI] [PubMed] [Google Scholar]
- 28.Lee S, Shin H. Municipal disease burden attributable to heat wave. J Korean Soc Health Educ Promot. 2014;31:51–62. [Google Scholar]
- 29.Yoon J, Oh IH, Seo H, Kim EJ, Gong YH, Ock M, Lim D, Lee WK, Lee YR, Kim D, et al. Disability-adjusted Life Years for 313 Diseases and Injuries: the 2012 Korean Burden of Disease Study. J Korean Med Sci. 2016;31(Suppl 2):S146–S157. doi: 10.3346/jkms.2016.31.S2.S146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoon J, Seo H, Oh IH, Yoon SJ. The Non-Communicable Disease Burden in Korea: Findings from the 2012 Korean Burden of Disease Study. J Korean Med Sci. 2016;31(Suppl 2):S158–S167. doi: 10.3346/jkms.2016.31.S2.S158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee WK, Lim D, Park H. Disability-Adjusted Life Years (DALYs) for Injuries Using Death Certificates and Hospital Discharge Survey by the Korean Burden of Disease Study 2012. J Korean Med Sci. 2016;31(Suppl 2):S200–S207. doi: 10.3346/jkms.2016.31.S2.S200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee YR, Kim YA, Park SY, Oh CM, Kim YE, Oh IH. Application of a Modified Garbage Code Algorithm to Estimate Cause-Specific Mortality and Years of Life Lost in Korea. J Korean Med Sci. 2016;31(Suppl 2):S121–S128. doi: 10.3346/jkms.2016.31.S2.S121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lim D, Lee WK, Park H. Disability-adjusted Life Years (DALYs) for Mental and Substance Use Disorders in the Korean Burden of Disease Study 2012. J Korean Med Sci. 2016;31(Suppl 2):S191–S199. doi: 10.3346/jkms.2016.31.S2.S191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ock M, Lee JY, Oh IH, Park H, Yoon SJ, Jo MW. Disability Weights Measurement for 228 Causes of Disease in the Korean Burden of Disease Study 2012. J Korean Med Sci. 2016;31(Suppl 2):S129–S138. doi: 10.3346/jkms.2016.31.S2.S129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim SH, Lee HJ, Ock M, Go DS, Kim HJ, Lee JY, Jo MW. Disability-Adjusted Life Years for Maternal, Neonatal, and Nutritional Disorders in Korea. J Korean Med Sci. 2016;31(Suppl 2):S184–S190. doi: 10.3346/jkms.2016.31.S2.S184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Field MJ, Gold MR Institute of Medicine (US) Committee on Summary Measures of Population Health. Summarizing Population Health: Directions for the Development and Application of Population Metrics. Washington, D.C.: National Academies Press; 1998. [PubMed] [Google Scholar]
- 37.Mathers CD, Sadana R, Salomon JA, Murray CJ, Lopez AD. Estimates of DALE for 191 Countries: Methods and Results. Global Programme on Evidence for Health Policy Working Paper No. 16. Geneva: World Health Organization; 2000. [Google Scholar]
- 38.Mahapatra P. Priority-setting in the health sector and summary measures of population health. In: Murray CJ, Salomon JA, Mathers CD, Lopez AD, editors. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva: World Health Organization; 2002. pp. 83–90. [Google Scholar]
- 39.Mathers CD, Ezzati M, Lopez AD, Murray CJ, Rodgers A. Causal decomposition of summary measures of population health. In: Murray CJ, Salomon JA, Mathers CD, Lopez AD, editors. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva: World Health Organization; 2002. pp. 273–290. [Google Scholar]
- 40.Murray CJ, Salomon JA, Mathers C. A critical examination of summary measures of population health. Bull World Health Organ. 2000;78:981–994. [PMC free article] [PubMed] [Google Scholar]
- 41.Murray CJ, Acharya AK. Understanding DALYs (disability-adjusted life years) J Health Econ. 1997;16:703–730. doi: 10.1016/s0167-6296(97)00004-0. [DOI] [PubMed] [Google Scholar]
- 42.Airoldi M, Morton A. Adjusting life for quality or disability: stylistic difference or substantial dispute? Health Econ. 2009;18:1237–1247. doi: 10.1002/hec.1424. [DOI] [PubMed] [Google Scholar]
- 43.Arnesen T, Kapiriri L. Can the value choices in DALYs influence global priority-setting? Health Policy. 2004;70:137–149. doi: 10.1016/j.healthpol.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 44.Lyttkens CH. Time to disable DALYs? On the use of disability-adjusted life-years in health policy. Eur J Health Econ. 2003;4:195–202. doi: 10.1007/s10198-003-0169-2. [DOI] [PubMed] [Google Scholar]
- 45.Nygaard E. Is it feasible or desirable to measure burdens of disease as a single number? Reprod Health Matters. 2000;8:117–125. doi: 10.1016/s0968-8080(00)90013-2. [DOI] [PubMed] [Google Scholar]
- 46.AbouZahr C, Vaughan JP. Assessing the burden of sexual and reproductive ill-health: questions regarding the use of disability-adjusted life years. Bull World Health Organ. 2000;78:655–666. [PMC free article] [PubMed] [Google Scholar]
- 47.Williams A. Calculating the global burden of disease: time for a strategic reappraisal? Health Econ. 1999;8:1–8. doi: 10.1002/(sici)1099-1050(199902)8:1<1::aid-hec399>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 48.Sundby J. Are women disfavoured in the estimation of disability adjusted life years and the global burden of disease? Scand J Public Health. 1999;27:279–285. [PubMed] [Google Scholar]
- 49.Arnesen T, Nord E. The value of DALY life: problems with ethics and validity of disability adjusted life years. BMJ. 1999;319:1423–1425. doi: 10.1136/bmj.319.7222.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Anand S, Hanson K. Disability-adjusted life years: a critical review. J Health Econ. 1997;16:685–702. doi: 10.1016/s0167-6296(97)00005-2. [DOI] [PubMed] [Google Scholar]
- 51.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Measuring the global burden of disease and risk factors, 1990??001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ, editors. Global Burden of Disease and Risk Factors. Washington, D.C.: World Bank; 2006. pp. 1–14. [Google Scholar]
- 52.Murray CJ, Lopez AD. The Global Burden of Disease: a Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press; 1996. [Google Scholar]
- 53.World Health Organization. Metrics: disability-adjusted life year (DALY) [Internet] [accessed on 30 Novermber 2015]. Available at http://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/
- 54.Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369:448–457. doi: 10.1056/NEJMra1201534. [DOI] [PubMed] [Google Scholar]
- 55.Mathers C, Fat DM, Boerma JT. The Global Burden of Disease: 2004 Update. Geneva: World Health Organization; 2008. [Google Scholar]
- 56.Mathers CD, Vos T, Lopez AD, Salomon J, Ezzati M. National Burden of Disease Studies: a Practical Guide. Edition 2.0. Global Program on Evidence for Health Policy. Geneva: World Health Organization; 2001. [Google Scholar]
- 57.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, Naghavi M, Salomon JA, Shibuya K, Vos T, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 58.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 59.Department of Health Statistics and Information Systems, World Health Organization. WHO Methods and Data Sources for Global Burden of Disease Estimates 2000-2011. Global Health Estimates Technical Paper WHO/HIS/HSI/GHE/2013.4. Geneva: World Health Organization; 2013. [Google Scholar]
- 60.Murray CJ. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull World Health Organ. 1994;72:429–445. [PMC free article] [PubMed] [Google Scholar]
- 61.Schroeder SA. Incidence, prevalence, and hybrid approaches to calculating disability-adjusted life years. Popul Health Metr. 2012;10:19. doi: 10.1186/1478-7954-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, Charlson F, Davis A, Degenhardt L, Dicker D, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Begg SJ, Vos T, Barker B, Stanley L, Lopez AD. Burden of disease and injury in Australia in the new millennium: measuring health loss from diseases, injuries and risk factors. Med J Aust. 2008;188:36–40. doi: 10.5694/j.1326-5377.2008.tb01503.x. [DOI] [PubMed] [Google Scholar]
- 64.National Health Insurance Service (KR) Major statistics on National Health Insurance Services, 2012 [Internet] [accessed on 11 November 2015]. Available at http://www.nhis.or.kr.
- 65.Alwan A. Global Status Report: on Noncommunicable Diseases 2010. Geneva: World Health Organization; 2011. [Google Scholar]
- 66.Mathers C, Vos T, Stevenson C. The Burden of Disease and Injury in Australia. Canberra: Australian Institute of Health and Welfare; 1999. [Google Scholar]
- 67.Ezzati M, Riboli E. Can noncommunicable diseases be prevented? Lessons from studies of populations and individuals. Science. 2012;337:1482–1487. doi: 10.1126/science.1227001. [DOI] [PubMed] [Google Scholar]
- 68.World Health Organization. Cost effectiveness and strategic planning (WHO-CHOICE) [Internet] [accessed on 11 April 2016]. Available at http://www.who.int/choice/cost-effectiveness/en/
- 69.Lapostolle A, Lefranc A, Gremy I, Spira A. Sensitivity analysis in summary measure of population health in France. Eur J Public Health. 2008;18:195–200. doi: 10.1093/eurpub/ckm109. [DOI] [PubMed] [Google Scholar]
- 70.Melse JM, Essink-Bot ML, Kramers PG, Hoeymans N, Dutch Burden of Disease Group A national burden of disease calculation: Dutch disability-adjusted life-years. Am J Public Health. 2000;90:1241–1247. doi: 10.2105/ajph.90.8.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]


