Abstract
In recognition of Korea's rising burden of non-communicable diseases (NCDs), we investigated the nation's NCD status and extracted detailed information from the 2012 Korean Burden of Disease study. Consistent with that study, we used disability-adjusted life year (DALY) as a metric. Using national data sources and disability weights specific to the Korean population, we analyzed 116 disaggregated NCDs from the study's four-level disease and injury hierarchy for both sexes and nine age groups. Per 100,000 population, 21,019 DALYs were lost to 116 NCDs. Of those, 13.97% were due to premature death (death prior to the standard life expectancy for a subject's age) and 86.03% to non-fatal health outcomes. Based on traditional statistics, the main causes of health loss were mortality of neoplasms; cardiovascular and circulatory diseases; diabetes, urogenital, blood, and endocrine diseases; and chronic respiratory diseases. When combined with analyses of premature death and non-fatal outcomes, however, a substantially different view emerged: the main causes of health loss were diabetes mellitus, low back pain, chronic obstructive pulmonary disease, ischemic heart disease, ischemic stroke, cirrhosis of the liver, osteoarthritis, asthma, gastritis and duodenitis, and periodontal disease (in that order), collectively causing 49.20% of DALYs. Thus, burden of disease data using DALYs rather than traditional statistics brings a new perspective to characterization of the population's health that provides practical information useful for developing and targeting national NCD control programs to better meet national needs.
Keywords: Disability-adjusted Life Years, DALY, Burden of Disease, Non-communicable Diseases, Korea
Graphical Abstract
INTRODUCTION
In Korea, effective disease prevention, intervention, and treatment and advances in medical technology have dramatically increased the population's longevity (1). There remains a wide gap, however, between life expectancy per se and healthy, disability-free life expectancy (1,2,3). As of 2012, the mean life expectancy of the Korean population was 81.4 years while the healthy life expectancy was only 73.0 years (2), suggesting that Koreans experience approximately 8.4 years of disability or disease before their death, corresponding to about 10% of their life (1). The primary cause of these years of sickness is believed to be non-communicable diseases (NCDs). While both the standardized death rate and the avoidable death rate due to NCDs are steadily decreasing, the NCD burden is still high, accounting for 81% of total deaths and seven of the top 10 causes of death (1). Moreover, the need for effective management of lifestyle-related NCD risk factors is increasing (1). For adult men in Korea, the smoking rate is still over 40% and the high-risk drinking rate is about 12.5% (1). Physical activity is steadily decreasing in both sexes, while the intake of excessive calories and sodium is increasing (1). The treatment rate is currently only 58.6% for patients with hypertension and 40.6% for those with hypercholesterolemia, and the control rate is 41.8% for patients with diabetic complications such as fundus examination (1). Without substantial and realistic changes in risk factor management in the near future, NCDs will likely take a great toll, in the form of premature deaths and disabilities, and increase Korea's socioeconomic burden. Thus, it is crucial for the government to accurately understand the magnitude of current health issues, monitor their trends and provide appropriate and timely interventions, funds, and educational programs both to help those already suffering from NCDs and to prevent or postpone NCD development in healthy individuals. The indicators used most frequently in health reporting and policy development to identify the most important health problems are the mortality and causes of death statistics. While this approach is straightforward and easy to communicate, it highlights only one facet of population health, and has progressively become less informative when used exclusively to describe the overall health status of a population (4,5,6) now that we recognize non-fatal life-time impact from NCDs as a major concern. Given the importance of determining comprehensive estimates for all of these impacts on population health, the present study details the Korean population's NCD burden using disability-adjusted life years (DALYs), a metric that integrates disease-specific fatal and non-fatal outcomes into a single measure while still allowing the two classes of outcomes to be examined separately as well (7). We have also analyzed 2012 NCD death and incidence data to see how well the DALY metric captures the impact of both premature death and disability (8) and provides a unique and different perspective from traditional statistics. The overall goal of this study was to increase understanding of DALY analysis and help devise effective national NCD control strategies to better meet national health needs.
MATERIALS AND METHODS
Overview
We applied the methods of the original Global Burden of Disease (GBD) study (8,9), with some modifications to tailor the study to the Korean population. A detailed description is presented in (10).
Scope of analysis
The reference year used for this study is 2012, and subjects were divided by sex and into nine age groups (0–9, 10–19, …70–79, 80+). The 2012 Korean Burden of Disease (KBD) study's disease and injury categories were modified on the basis of the GBD 2010 study to capture the population's specific health issues while ensuring comparability with other disease burden studies (10). One of the three broad level I categories in this hierarchy was NCDs, and we included 116 NCDs at the most disaggregated level. The nine broad level II causes that encompass those 116 NCDs are neoplasms; cardiovascular and circulatory diseases; chronic respiratory diseases; cirrhosis of the liver; digestive diseases (except cirrhosis); neurological disorders; musculoskeletal disorders; other non-communicable diseases; and diabetes, urogenital, blood, and endocrine diseases. Mental and behavioral disorders have been addressed in a separate study (11) and therefore were excluded from this analysis.
Years of life lost due to premature mortality
Years of life lost (YLLs) were computed for each specific cause by multiplying the number of deaths at each age by the standard remaining life expectancy for that age (12). We used the 2012 edition of the annual life tables produced by Statistics Korea. There, the life expectancy at birth was 77.95 years for male Koreans and 84.64 years for female Koreans (13). Cause-specific mortality was estimated based on the Cause of Death Statistics Korea, 2012. When we could not determine cases' underlying causes of death because of the established problem of “garbage code” use (8), we adapted the GBD 2010 study's algorithms to redistribute those codes to probable causes of death (14). We computed two YLL data sets: one incorporating standard age-weights (C = 0.1658, β = 0.04) and a 3% time discount rate (9), and another with no age-weighting or time discounting.
Years lived with disability
We computed years lived with disability (YLDs) for each cause by multiplying the number of incident cases by the mean duration of each disease and its disability weight (12). As was done for YLLs, we developed two data sets, one incorporating standard age-weights and 3% time discounting and the other with no age-weighting or time discounting. To obtain the epidemiologic parameters required for YLD computation, we used the National Health Insurance Service (NHIS) claims data. To screen the subjects initially, we extracted the principal diagnosis after a sensitivity analysis with and without the first additional diagnosis. To determine the prevalence of each specific disease, we developed case definitions by considering the frequency of attendance at a healthcare facility and whether in-patient care was received during 2012. We extracted the incidence cases from the prevalence cases, defining incidence cases as those with no prior diagnosis in a time period of 1–5 years (from 2007 to 2011), depending on the disease characteristics. Finally, we calculated the prevalence and incidence for each cause based on the results of our sensitivity analyses, literature reviews, national health statistics reviews including Korea National Health and Nutrition Examination Survey, and professional consultations. For cancers, prevalence and incidence rates were extracted from the Korea Central Cancer Registry, according to ICD-10 codes from KBD 2012 study's cause categories. We used the DisMod II program (15) to estimate the duration and mean age at onset, then examined the outputs and adjusted the overestimated duration values. When the estimated disease duration exceeded the life expectancy at that age, we selected the life expectancy as the disease duration. We used the KBD 2012 estimates of the Korean version of disability weights, scaled from 0 (perfect health) to 1 (equivalent to death) (16), for each specific cause. For some NCDs that yielded a relatively high weight when outpatients accounted for >95% of cases, we estimated disease severity by evaluating outpatient and inpatient cases separately, applying the estimated disability weight to the inpatient cases, and applying the lowest disability weight value from the superordinate category to the outpatient cases.
Disability-adjusted life years
For each cause, DALYs were calculated as the sum of the YLLs and YLDs. Because our sensitivity analysis revealed no significant difference in the results between the data set with standard age-weighting and 3% time discounting and the set without age-weighting and time discounting (10), this report focuses on the set with standard age-weighting and time discounting.
Ethics statement
The study protocol was approved by Korea University's institutional review board (1040548-KU-IRB-13-164-A-1[E-A-1][E-A-1]). Informed consent was waived by the board.
RESULTS
Deaths in 2012
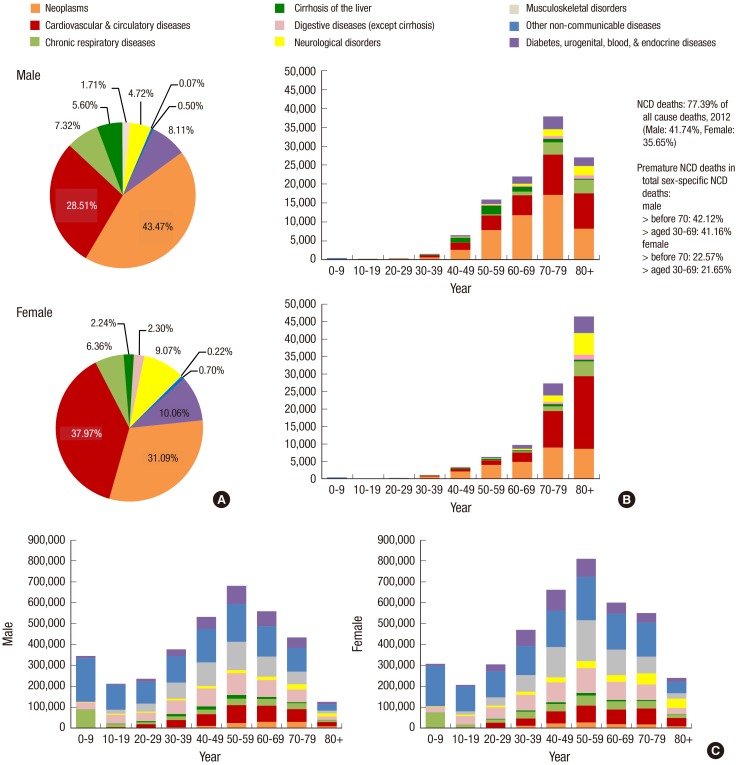
In 2012, the 116 NCDs accounted for 77.39% of all deaths in Korea. Fig. 1A shows the proportion and number of deaths caused by NCDs in 2012, and the distribution of each in males and in females in all age groups. Neoplasms; cardiovascular and circulatory diseases; and diabetes, urogenital, blood, and endocrine diseases collectively contributed about 80% of NCD mortality in both sexes (Fig. 1A). Beginning in the 40–49 age group, men showed a higher number of NCD-related deaths than women, and this difference increased steeply in the subsequent decades (Fig. 1B). As is expected due to their higher life expectancy, women had a higher number of deaths than men in their 80s. NCDs before 70 years of age accounted for 42.12% of premature deaths in men and 22.57% in women. Between 30–69 years of age, NCDs accounted for 41.16% of deaths in men and 21.65% in women.
Fig. 1.
Proportion (A) and number of deaths (B), and number of incidences (C) in non-communicable diseases (NCDs) for 9 broad cause groups by sex and age group, 2012.
Incidence in 2012
Fig. 1C shows the proportion, number, and age of people newly diagnosed with each NCD by sex in 2012. The patterns were similar for both sexes, although starting at 20 years of age, more overall cases occurred among women. Men and women aged 50–59 years showed the highest number of incidence cases.
DALYs in 2012
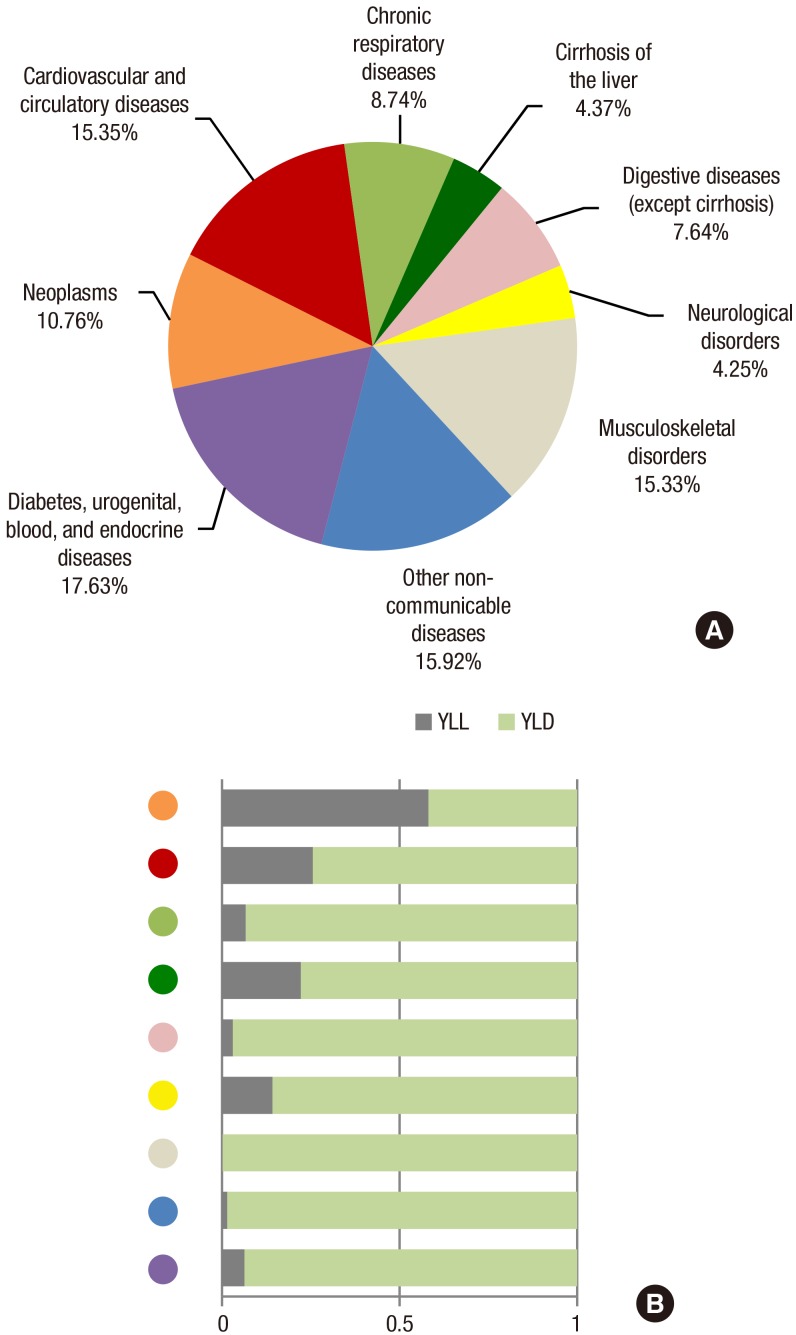
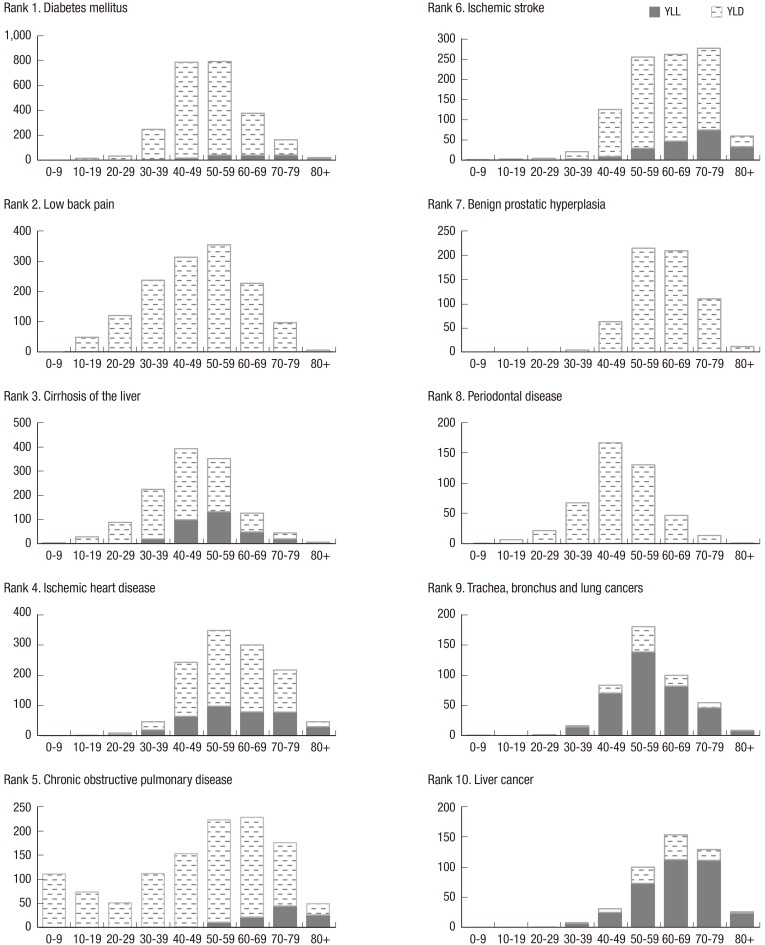
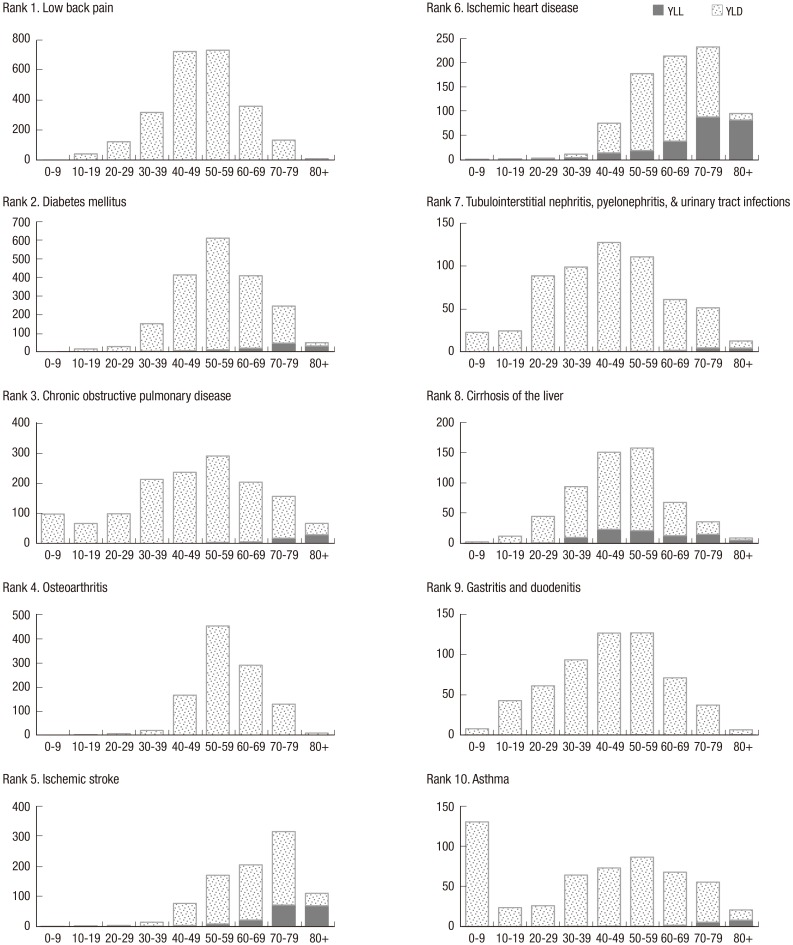
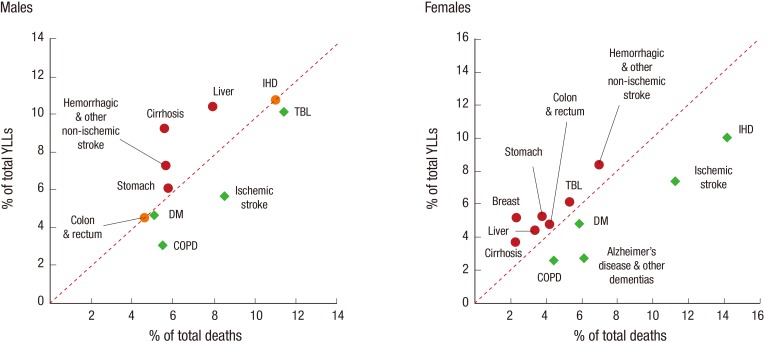
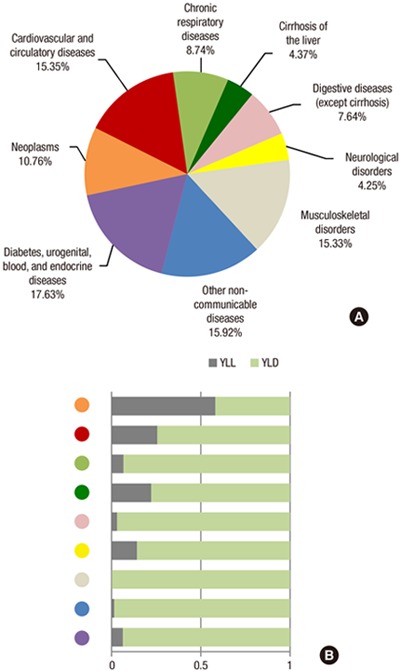
Per 100,000 population, 21,019 DALYs were lost to 116 NCDs in 2012, of which 13.97% were due to premature death and 86.03% to non-fatal health outcomes. YLDs made a larger contribution than YLLs to the NCD burden in all broad cause groups except neoplasms (Fig. 2). Fig. 2 shows the percent of DALYs lost to each of the nine broad groups of NCDs, as well as their YLL and YLD components. Table 1 lists the major specific causes accounting for more than 1% of total NCD DALYs in each of the nine broad categories. Table 2A and 2B present the leading 10 causes of YLLs, YLDs, and DALYs by sex. The leading 10 causes accounted for about half of the total NCD DALYs – 51.76% in men and 49.77% in women. The life cycle burden caused by each of the 10 sex-specific leading causes of DALYs is shown in Fig. 3 for males and in Fig. 4 for females. Premature death, represented by YLLs, was more frequent in men and was mainly caused by cirrhosis of the liver; ischemic heart disease (IHD); chronic obstructive pulmonary disease (COPD); ischemic stroke; trachea, bronchus and lung cancers (TBL); and liver cancer. Even males as young as 10–29 years old experienced low back pain and cirrhosis of the liver. The overall YLD share was larger in women. Burden from musculoskeletal conditions (MSK) such as low back pain and osteoarthritis was apparently higher in women. Fig. 5 presents the shifts in relative importance of the top ten causes of YLL or death for each sex that occur upon considering the age at death for each cause. The top three causes with a high frequency of death in men – TBL cancers (11.45% of total deaths), IHD (11.04%), and ischemic stroke (8.53%) – became less important when the age at death was taken into account, demonstrated by their contribution of 10.13%, 10.78%, and 5.63% of total YLLs, respectively. Four other causes became more important, including, from largest to smallest shift in importance, cirrhosis of the liver (5.60% of total deaths), liver cancer (7.92%), hemorrhagic and other non-ischemic stroke (5.63%), and stomach cancer (5.73%), which accounted for 9.22%, 10.44%, 7.29%, and 6.11% of total YLLs, respectively. Three of the top four causes of death in women likewise decreased in importance when considering age at death, including IHD (14.14% of total deaths), ischemic stroke (11.24%), and Alzheimer's disease and other dementias (6.08%), which were responsible, respectively, for 10.02%, 7.38%, and 2.73% of YLLs for women. Seven causes became more important: breast cancer (2.29% of total deaths), stomach cancer (3.76%), hemorrhagic and other non-ischemic stroke (6.96%), cirrhosis of the liver (2.24%), liver cancer (3.35%), TBL cancers (5.33%), and colon and rectum cancers (4.15%), contributing 5.20%, 5.23%, 8.42%, 3.65%, 4.42%, 6.18%, and 4.80% of total YLLs, respectively.
Fig. 2.
Proportions of disability-adjusted life years (DALYs) (A) with the YLL and YLD as a proportion of total DALYs (B) according to broad 9 cause groups in 2012.
YLL, years of life lost due to premature mortality; YLD, years lived with a disability.
Table 1. Disability-adjusted life years (DALYs) ranked by 9 broad cause groups, 2012.
| Rank | Broad cause group | DALYs | % of Total NCD DALYs |
|---|---|---|---|
| Specific cause in the group | |||
| 1 | Diabetes, urogenital, blood, & endocrine diseases | 3,706 | 17.63 |
| Diabetes mellitus | 2,181 | 10.37 | |
| Tubulointerstitial nephritis, pyelonephritis, & urinary tract infections | 402 | 1.91 | |
| Benign prostatic hyperplasia | 308 | 1.47 | |
| 2 | Other non-communicable diseases | 3,346 | 15.92 |
| Periodontal disease | 425 | 2.02 | |
| Refraction & accommodation disorders | 353 | 1.68 | |
| Vision loss | 290 | 1.38 | |
| Glaucoma | 276 | 1.31 | |
| Eczema | 250 | 1.19 | |
| Dental caries | 242 | 1.15 | |
| Abscess, impetigo, and other bacterial skin diseases | 238 | 1.13 | |
| Cataracts | 234 | 1.11 | |
| Cellulitis | 216 | 1.03 | |
| 3 | Cardiovascular & circulatory diseases | 3,226 | 15.35 |
| Ischemic heart disease | 1,011 | 4.81 | |
| Ischemic stroke | 954 | 4.54 | |
| Hemorrhagic & other non-ischemic stroke | 366 | 1.74 | |
| Hypertensive heart disease | 361 | 1.72 | |
| 4 | Musculoskeletal disorders | 3,223 | 15.33 |
| Low back pain | 1,915 | 9.11 | |
| Osteoarthritis | 701 | 3.34 | |
| Neck pain | 283 | 1.34 | |
| 5 | Neoplasms | 2,261 | 10.76 |
| Trachea, bronchus & lung cancers | 318 | 1.51 | |
| Stomach cancer | 306 | 1.46 | |
| Liver cancer | 288 | 1.37 | |
| Colon & rectum cancers | 273 | 1.30 | |
| 6 | Chronic respiratory diseases | 1,838 | 8.74 |
| Chronic obstructive pulmonary disease | 1,305 | 6.21 | |
| Asthma | 491 | 2.34 | |
| 7 | Digestive diseases (except cirrhosis) | 1,607 | 7.64 |
| Gastritis & duodenitis | 441 | 2.10 | |
| Gastroesophageal reflux disease | 413 | 1.96 | |
| 8 | Cirrhosis of the liver | 919 | 4.37 |
| 9 | Neurological disorders | 894 | 4.25 |
| Alzheimer's disease & other dementias | 383 | 1.82 | |
| Epilepsy | 214 | 1.02 |
DALYs per 100,000 population. Specific causes accounting for more than 1% of total DALYs are included and ranked within each group.
Table 2A. Top 10 specific causes of years of life lost (YLLs) due to premature mortality, years lived with a disability (YLDs), and disability-adjusted life years (DALYs) in 2012 by sex: male cases.
| Specific causes | DALYs | YLLs | YLDs | |||
|---|---|---|---|---|---|---|
| rank | No. (%) | rank | No. (%) | rank | No. (%) | |
| Diabetes mellitus | 1 | 2,439 (12.06) | 8 | 161 (4.65) | 1 | 2,278 (13.60) |
| Low back pain | 2 | 1,402 (6.93) | 80 | 0.09 (0.003) | 2 | 1,401 (8.37) |
| Cirrhosis of the liver | 3 | 1,262 (6.24) | 4 | 320 (9.22) | 4 | 942 (5.63) |
| Ischemic heart disease | 4 | 1,214 (6.01) | 1 | 374 (10.78) | 5 | 841 (5.02) |
| Chronic obstructive pulmonary disease | 5 | 1,175 (5.81) | 10 | 106 (3.06) | 3 | 1,069 (6.38) |
| Ischemic stroke | 6 | 1,009 (4.99) | 7 | 195 (5.63) | 6 | 814 (4.86) |
| Benign prostatic hyperplasia | 7 | 616 (3.05) | 81 | 0 (0) | 7 | 616 (3.68) |
| Periodontal disease | 8 | 453 (2.24) | 81 | 0 (0) | 8 | 453 (2.70) |
| Trachea, bronchus and lung cancers | 9 | 447 (2.21) | 3 | 351 (10.13) | 39 | 96 (0.57) |
| Liver cancer | 10 | 447 (2.21) | 2 | 362 (10.44) | 40 | 85 (0.50) |
| Asthma | 11 | 436 (2.15) | 30 | 16 (0.45) | 9 | 420 (2.51) |
| Hemorrhagic & other non-ischemic stroke | 12 | 402 (1.99) | 5 | 253 (7.29) | 32 | 149 (0.89) |
| Stomach cancer | 13 | 399 (1.97) | 6 | 212 (6.11) | 27 | 187 (1.12) |
| Gastroesophageal reflux disease | 14 | 334 (1.65) | 78 | 0.25 (0.01) | 10 | 334 (1.99) |
| Colon and rectum cancers | 15 | 326 (1.61) | 9 | 158 (4.55) | 29 | 168 (1.00) |
YLLs, YLDs, DALYs per 100,000 males. Sums may not add up to exact total due to rounding.
Table 2B. Top 10 specific causes of years of life lost (YLLs) due to premature mortality, years lived with a disability (YLDs), and disability-adjusted life years (DALYs) in 2012 by sex: female cases.
| Specific causes | DALYs | YLLs | YLDs | |||
|---|---|---|---|---|---|---|
| rank | No. (%) | rank | No. (%) | rank | No. (%) | |
| Low back pain | 1 | 2,429 (11.13) | 79 | 0.13 (0.01) | 1 | 2,429 (12.51) |
| Diabetes mellitus | 2 | 1,921 (8.80) | 7 | 116 (4.81) | 2 | 1,806 (9.30) |
| Chronic obstructive pulmonary disease | 3 | 1,436 (6.58) | 13 | 62 (2.59) | 3 | 1,373 (7.07) |
| Osteoarthritis | 4 | 1,081 (4.95) | 82 | 0 (0) | 4 | 1,081 (5.57) |
| Ischemic stroke | 5 | 898 (4.12) | 3 | 177 (7.38) | 5 | 721 (3.71) |
| Ischemic heart disease | 6 | 806 (3.70) | 1 | 241 (10.02) | 8 | 566 (2.91) |
| Tubulointerstitial nephritis, pyelonephritis, & urinary tract infections | 7 | 597 (2.74) | 30 | 13 (0.54) | 6 | 584 (3.01) |
| Cirrhosis of the liver | 8 | 574 (2.63) | 10 | 88 (3.65) | 11 | 486 (2.50) |
| Gastritis and duodenitis | 9 | 573 (2.62) | 71 | 1 (0.04) | 7 | 572 (2.94) |
| Asthma | 10 | 546 (2.50) | 26 | 17 (0.72) | 9 | 529 (2.72) |
| ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ |
| Gastroesophageal reflux disease | 12 | 492 (2.25) | 77 | 0.26 (0.01) | 10 | 491 (2.53) |
| ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ |
| Hemorrhagic & other non-ischemic stroke | 17 | 330 (1.51) | 2 | 202 (8.42) | 39 | 128 (0.66) |
| Breast cancer | 18 | 325 (1.49) | 6 | 125 (5.20) | 27 | 200 (1.03) |
| ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ |
| Colon and rectum cancers | 28 | 220 (1.01) | 8 | 115 (4.80) | 40 | 105 (0.54) |
| Stomach cancer | 29 | 214 (0.98) | 5 | 126 (5.23) | 44 | 88 (0.45) |
| ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ |
| Trachea, bronchus and lung cancers | 31 | 188 (0.86) | 4 | 149 (6.18) | 60 | 40 (0.21) |
| ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ |
| Liver cancer | 45 | 129(0.59) | 9 | 106(4.42) | 70 | 23 (0.12) |
YLLs, YLDs, DALYs per 100,000 females. Sums may not add up to exact total due to rounding.
Fig. 3.
Top 10 causes of disability-adjusted life years (DALYs) with the YLL and YLD shares in males by age-group. X-axis: age group, Y-axis: DALYs per 100,000 males. The maximum value of the Y-axis was tailored to the distribution.
YLL, years of life lost due to premature mortality; YLD, years lived with a disability.
Fig. 4.
Top 10 causes of disability-adjusted life years (DALYs) with the YLL and YLD shares in females by age-group. X-axis: age group, Y-axis: DALYs per 100,000 females. The maximum value of the Y-axis was tailored to the distribution.
YLL, years of life lost due to premature mortality; YLD, years lived with a disability.
Fig. 5.
Comparison of the proportional distribution of death and years of life lost (YLL) by leading cause of death, 2012.
Cirrhosis, cirrhosis of the liver; liver, liver cancer; IHD, ischemic heart disease; TBL, trachea, bronchus and lung cancers; stomach, stomach cancer; colon & rectum, colon and rectum cancers; DM, diabetes mellitus; COPD, chronic obstructive pulmonary disease; breast, breast cancer.
DISCUSSION
Disease mortality, incidence, and prevalence data are traditional measures of a population's burden of disease, and premature mortality can be used to assess the impact of NCDs (17). A health problem or disease can have a relatively low incidence but cause serious disability or death, resulting in a high disease burden. Conversely, some common illnesses may cause a much smaller burden (18). Using DALYs, we were able to assess the impact of both fatal and non-fatal outcomes by considering the age and life expectancy at the time of each cause-specific death as well as the relative severity of various disabilities. Converting those data to years of health loss, we were able to provide a different view compared to a simple rank order of deaths or incidences; specifically, a view that allows comparisons among the burdens of a broad range of NCDs by sex and by age.
The top 5 broad groups that caused a large number of DALYs were diabetes, urogenital, blood, and endocrine diseases; other non-communicable diseases; cardiovascular and circulatory diseases; MSK; and neoplasms. The top 10 specific causes of DALYs in both sexes included, in order of importance, diabetes mellitus (DM), low back pain, COPD, IHD, ischemic stroke, cirrhosis of the liver, osteoarthritis, asthma, gastritis and duodenitis, and periodontal disease. Our results show that non-fatal outcomes contribute more significantly than premature death to the nation's disease burden, which is consistent with the statement from Murray et al. that “what ails most persons is not necessarily what kills them” (19). Some of the top 10 causes of YLLs were also among the top 10 causes of DALYs, including cirrhosis of the liver, IHD, COPD, ischemic stroke and two types of cancer (TBL and liver cancers) in men and DM, ischemic stroke, IHD, and cirrhosis of the liver in women. Although these were all main causes of premature death, the fraction of DALYs from YLLs was relatively low for these causes, ranging from 6.02% to 30.8%, except the two cancers in men (78.6% for TBL cancers and 81.1% for liver cancer).
The finding that low back pain was the most frequent cause of outpatient cases and the second greatest burden, with 99.81% of its DALYs resulting from YLDs in both sexes, is in line with the worldwide trend of high prevalence and high burden of MSK conditions (20,21,22,23,24). Because of their long-term pain and physical disability, MSK conditions are costly for individuals and for society. Even though the burden of these conditions is projected to increase as the population ages and becomes more obese (25), a population-based understanding of the magnitude of the problem is lacking. Research to assess the most effective and affordable strategies for MSK prevention and management is urgently needed, as is targeted and practical planning to deal with the increased healthcare burden caused by these conditions. Diabetes mellitus has continuously been within the top 3 causes of disease burden in both sexes since this population-level study began in 2002 (26,27), and high-risk populations are increasing; as of 2013, one in four adults had impaired fasting glucose (28). Alarmingly, the number of childhood and adolescent patients with type 2 diabetes has also been increasing steadily since 2006 (28). If this trend continues, the diabetic population is likely to double by 2050, reaching 6 million (29).
NCD patients often fail to recognize the progression of their disease and present at hospitals only when their disease has become acute or they have developed long-term complications (17). This approach often leads to considerable health and socioeconomic costs. Strategies targeting young and middle-aged people, whose diseases may still be in the “invisible” stage, are urgently needed to curb development of NCDs and to detect them in time for early intervention. These strategies include improving awareness of the long-term consequences of unhealthy lifestyle habits and educating the population on NCD prevention and management strategies, in ways that maximize and integrate local primary health care services. This is ideally started in childhood, when many health behaviors are shaped, but it is never too late to start. Although cerebrovascular disease deaths dramatically decreased over the past several years, resulting in increased YLDs from this cause, the number of deaths caused by its after-effects has actually increased (1). To prevent these premature deaths, patients and health professionals should be involved in follow-up management. The large gaps between the rankings of causes of death and the rankings YLLs are noteworthy because they suggest that people die at younger ages from those causes. All of these various metrics and analyses should be applied when setting priorities or targeted intervention.
This study highlighted the magnitude of Korea's NCD burden using the best national data sources, but it had several limitations. Methodological issues are in line with those described in KBD 2012 (10). First, we extracted prevalence and incidence data from claim-based administrative sources that do not include people with unmet medical needs, so the burden might be underestimated. Also, more precise extraction criteria could enhance the accuracy of the underlying epidemiologic data. To this end, one possible approach would be analyses incorporating treatment or prescription information with the main diagnosis codes. Second, we did not consider multiple pathologies or comorbidities for disability weighting and YLD computations, nor did we consider severity levels for disability weights. Even though we carefully examined the estimated values and tried to adjust for causes having more than 95% outpatient cases but relatively high estimated weights by separating outpatient and inpatient cases, the final YLD values might be more valid if all diseases were analyzed at multiple severity levels specific to each disease. Finally, our results cannot be directly compared to previous Korean disease burden studies mainly due to differences in disease categories and our newly estimated disability weights. Government-led regular updates using the same methodology and data sources should be implemented to compile a broad body of evidence that allows meaningful and accurate assessment of trends over time and relative magnitudes of the nation's disease burdens.
The global disease management paradigm is shifting from treatment-oriented to prevention-orientated management in an effort to reduce the avoidable burden of NCDs (30). Numerous possible interventions for preventing and managing NCDs are already well established (17,31,32,33,34,35). More importantly, in order to properly prioritize and adapt those interventions to our targeted population, we must be able to determine both individual- and population-level feasibility and preventability, and to predict the scope of the effects (36). A broad spectrum of evidence is needed to guide large-scale prevention and control programs that can effectively reverse the rise of premature death and disability caused by NCDs in Korea. Population-level burden of disease data using DALYs, as presented in this study, can capture aspects of our population's health in a perspective that differs substantially from that provided by traditional indicators. The results of this study, particularly when combined with the upcoming results of our study identifying risk factors and analyzing cost effectiveness of interventions, will provide a more specific and detailed guide for developing and targeting national NCD control programs to meet the nation's urgent needs.
Footnotes
Funding: This study was supported by a grant from the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (Study No. HI13C0729).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study supervision: Yoon SJ. Study conception and design: Yoon J, Yoon SJ. Analysis and interpretation of data: Yoon J, Seo H, Oh IH, Yoon SJ. Acquisition of data: Yoon J, Seo H. Preparation of the first draft: Yoon J. Finalization of the manuscript: Yoon J, Yoon SJ. Approval of the final version of the manuscript: all authors.
References
- 1.Korea Centers for Disease Control and Prevention. Factbook: Non-communicable Diseases 2015. Cheongju: Korea Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 2.Statistics Korea. Trends in life expectancy and healthy life expectancy [Internet] [accessed on 3 January 2015]. Available at http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=2758.
- 3.Ko SJ, Jung YH. Health-adjusted life expectancy in Korea. Issue Focus. 2014;247:1–8. [Google Scholar]
- 4.Murray CJ, Salomon JA, Mathers CD, Lopez AD. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva: World Health Organization; 2002. [Google Scholar]
- 5.Van der Maas PJ. Applications of summary measures of population health. In: Murray CJ, Salomon JA, Mathers CD, Lopez AD, editors. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva: World Health Organization; 2002. pp. 53–60. [Google Scholar]
- 6.Pinheiro P, Plaß D, Krämer A. The burden of disease approach for measuring population health. In: Krämer A, Khan MH, Kraas F, editors. Health in Megacities and Urban Areas. Heidelberg: Springer; 2011. pp. 21–38. [Google Scholar]
- 7.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Measuring the global burden of disease and risk factors, 1990??001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ, editors. Global Burden of Diseases and Risk Factors. Washington, D.C.: The World Bank; 2006. pp. 1–14. [Google Scholar]
- 8.Murray CJ, Lopez AD. The Global Burden of Disease: a Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Boston, MA: Harvard University Press; 1996. [Google Scholar]
- 9.Mathers CD, Vos T, Lopez A, Salomon J, Ezzati M. National Burden of Disease Studies: a Practical Guide. Geneva: World Health Organization; 2001. [Google Scholar]
- 10.Yoon J, Oh IH, Seo H, Kim EJ, Gong YH, Ock M, Lim D, Lee WK, Lee YR, Kim D, et al. Disability-adjusted Life Years for 313 Diseases and Injuries: the 2012 Korean Burden of Disease Study. J Korean Med Sci. 2016;31(Suppl 2):S146–S157. doi: 10.3346/jkms.2016.31.S2.S146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim D, Lee WK, Park H. Disability-adjusted Life Years (DALYs) for Mental and Substance Use Disorders in the Korean Burden of Disease Study 2012. J Korean Med Sci. 2016;31(Suppl 2):S191–S199. doi: 10.3346/jkms.2016.31.S2.S191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Metrics: disability-adjusted life year (DALY) [Internet] [accessed on 30 November 2015]. Available at http://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/
- 13.Korean Statistical Information Service. Life table [Internet] [accessed on 17 November 2015]. Available at http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE&parentId=A#SubCont.
- 14.Lee YR, Kim YA, Park SY, Oh CM, Kim YE, Oh IH. Application of a Modified Garbage Code Algorithm to Estimate Cause-Specific Mortality and Years of Life Lost in Korea. J Korean Med Sci. 2016;31(Suppl 2):S121–S128. doi: 10.3346/jkms.2016.31.S2.S121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barendregt JJ, Van Oortmarssen GJ, Vos T, Murray CJ. A generic model for the assessment of disease epidemiology: the computational basis of DisMod II. Popul Health Metr. 2003;1:4. doi: 10.1186/1478-7954-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ock M, Lee JY, Oh IH, Park H, Yoon SJ, Jo MW. Disability Weights Measurement for 228 Causes of Disease in the Korean Burden of Disease Study 2012. J Korean Med Sci. 2016;31(Suppl 2):S129–S138. doi: 10.3346/jkms.2016.31.S2.S129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alwan A. Global Status Report: on Noncommunicable Diseases 2010. Geneva: World Health Organization; 2011. [Google Scholar]
- 18.Mathers C, Boerma T, Fat DM. The Global Burden of Disease: 2004 Update. Geneva: World Health Organization; 2008. [Google Scholar]
- 19.Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369:448–457. doi: 10.1056/NEJMra1201534. [DOI] [PubMed] [Google Scholar]
- 20.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 21.Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, et al. The global burden of low back pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:968–974. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 22.Hoy DG, Smith E, Cross M, Sanchez-Riera L, Buchbinder R, Blyth FM, Brooks P, Woolf AD, Osborne RH, Fransen M, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014;73:982–989. doi: 10.1136/annrheumdis-2013-204344. [DOI] [PubMed] [Google Scholar]
- 23.March L, Smith EU, Hoy DG, Cross MJ, Sanchez-Riera L, Blyth F, Buchbinder R, Vos T, Woolf AD. Burden of disability due to musculoskeletal (MSK) disorders. Best Pract Res Clin Rheumatol. 2014;28:353–366. doi: 10.1016/j.berh.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 24.Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, Charlson F, Davis A, Degenhardt L, Dicker D. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoy D, Geere JA, Davatchi F, Meggitt B, Barrero LH. A time for action: opportunities for preventing the growing burden and disability from musculoskeletal conditions in low- and middle-income countries. Best Pract Res Clin Rheumatol. 2014;28:377–393. doi: 10.1016/j.berh.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Yoon SJ, Bae SC, Lee SI, Chang H, Jo HS, Sung JH, Park JH, Lee JY, Shin Y. Measuring the burden of disease in Korea. J Korean Med Sci. 2007;22:518–523. doi: 10.3346/jkms.2007.22.3.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim EJ, Yoon SJ, Jo MW, Kim HJ. Measuring the burden of chronic diseases in Korea in 2007. Public Health. 2013;127:806–813. doi: 10.1016/j.puhe.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 28.Korean Diabetes Association; National Heatlh Insurance Service (KR) Korean Diabetes Fact Sheet: 2015. Seoul: Korean Diabetes Association; 2015. [Google Scholar]
- 29.Kwon HS, Kim WH, Lee DY, Park SI. Current status and need for a Korean diabetes prevention study. Public Health Wkly Rep. 1995;8:746–753. [Google Scholar]
- 30.World Health Organization. Noncommunicable Diseases Progress Monitor 2015. Geneva: World Health Organization; 2015. [Google Scholar]
- 31.World Health Organization. Preventing Chronic Diseases: a Vital Investment. Geneva: World Health Organization; 2005. [Google Scholar]
- 32.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 33.Alleyne G, Binagwaho A, Haines A, Jahan S, Nugent R, Rojhani A, Stuckler D, Lancet NCD Action Group Embedding non-communicable diseases in the post-2015 development agenda. Lancet. 2013;381:566–574. doi: 10.1016/S0140-6736(12)61806-6. [DOI] [PubMed] [Google Scholar]
- 34.Bonita R, Magnusson R, Bovet P, Zhao D, Malta DC, Geneau R, Suh I, Thankappan KR, McKee M, Hospedales J, et al. Country actions to meet UN commitments on non-communicable diseases: a stepwise approach. Lancet. 2013;381:575–584. doi: 10.1016/S0140-6736(12)61993-X. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization. Global Action Plan: for the Prevention and Control of Noncommunicable Diseases 2013-2020. Geneva: World Health Organization; 2013. [Google Scholar]
- 36.Ezzati M, Riboli E. Can noncommunicable diseases be prevented? Lessons from studies of populations and individuals. Science. 2012;337:1482–1487. doi: 10.1126/science.1227001. [DOI] [PubMed] [Google Scholar]