Abstract
Background: The Mediterranean diet has positively influenced various medical conditions, but only a paucity of studies has considered the relation between the Mediterranean diet and quality of life (QOL) among people living in North America.
Objective: We investigated whether a higher adherence to the Mediterranean diet (aMED) was associated with better QOL and decreased pain, stiffness, disability, and depression in a large cohort of North Americans from the Osteoarthritis Initiative.
Design: aMED was evaluated through a validated Mediterranean diet score categorized into quintiles. Outcomes of interest were QOL [assessed with the 12-Item Short-Form Health Outcome Survey (SF-12)]; disability, pain, and stiffness [assessed in both knees with the Western Ontario and McMaster Universities Arthritis Index (WOMAC)]; and depressive symptoms [assessed with the Center for Epidemiologic Studies Depression Scale (CES-D)].
Results: Of the 4470 participants (2605 women; mean age: 61.3 y), those with a higher aMED had significantly more favorable scores on all outcomes investigated (P < 0.0001 for all comparisons). After adjustment for potential confounders in linear regression analyses, a higher aMED was significantly associated with a higher SF-12 physical composite scale value (β: 0.10; 95% CI: 0.05, 0.15; P < 0.0001), lower WOMAC scores (except for stiffness), and lower CES-D scores (β: −0.05; 95% CI: −0.09, −0.01; P = 0.01). An adjusted logistic regression analysis, taking as reference those in the 2 highest quintiles of the aMED score, confirmed these findings.
Conclusion: Higher aMED is associated with better QOL and decreased pain, disability, and depressive symptoms. This trial was registered at clinicaltrials.gov as NCT00080171.
Keywords: depression, Mediterranean diet, quality of life osteoarthritis initiative, pain, disability
INTRODUCTION
The term Mediterranean diet is used to describe the traditional dietary habits of people in Greece, Spain, Italy, and other Mediterranean countries and is depicted as a food pyramid (1). The Mediterranean diet is an established healthy eating behavior that has consistently and positively influenced musculoskeletal, cardiovascular, metabolic, and cognitive health (2–5).
Interest in the importance of improving quality of life has been growing in recent years. Quality of life is an important patient-reported outcome and a measure of the impact an illness has on the functional health status as perceived by the patients themselves (6). In addition, quality of life is a relevant outcome among policymakers, researchers, and clinicians (7). Indeed, in response to the increasing age of the American population, several policies have been developed that specifically emphasize the importance of promoting quality of life in older age.
Surprisingly, there is a paucity of data that has considered the relation between the Mediterranean diet and quality of life, and most studies to date have been limited to European samples. Although limited to Mediterranean countries, 3 studies (8–10) have found that better quality of life was associated with a higher adherence to the Mediterranean diet (aMED).13 Another study found similar results in Australian individuals (11).
There is a notable lack of studies in North America that have assessed the impact of the Mediterranean diet on quality of life. To our knowledge, only 1 study in North America has assessed this impact (12). The authors of this study demonstrated that a higher aMED had a positive impact on quality of life and reduced the monetary burden associated with medical conditions. Another prospective study (13) reported that better adherence to a high-quality diet at midlife is linked to greater health and well-being later in life.
Given the potential benefits of the Mediterranean diet and limited data in North America, we investigated whether aMED is associated with better quality of life in a large cohort of North Americans. Moreover, we explored whether a higher adherence to this dietary pattern was associated with lower frequency of pain, stiffness, disability, and depression because each of these outcomes is closely related to quality of life.
METHODS
Data source and subjects
Data for this trial (NCT00080171) were obtained from the Osteoarthritis Initiative (OAI) database. We used variables acquired during baseline and screening evaluations (publicly available from November 2008). All participants were recruited as part of the ongoing publicly and privately funded multicenter and longitudinal OAI study (n = 4796). Patients with a high risk of knee osteoarthritis were recruited from 4 clinical sites in the United States (Baltimore, Maryland; Pittsburgh, Pennsylvania; Pawtucket, Rhode Island; and Columbus, Ohio) between February 2004 and May 2006 and were eligible if they 1) had knee osteoarthritis and reported knee pain in a 30-d period in the past 12 mo or 2) were at high risk of developing knee osteoarthritis (e.g., overweight or obese, knee injury or operation, parents or siblings with total knee replacement, frequent knee-bending activities that increase risk, and hand or hip osteoarthritis) (14).
All participants provided written informed consent. The OAI study protocol was approved by the institutional review board of the OAI Coordinating Center.
aMED (exposure)
Dietary pattern was analyzed with the use of a validated tool called the Block Brief 2000 food-frequency questionnaire (15). This food-frequency questionnaire contains a list of 70 items and is designed to assess usual food and beverage consumption over the past year. Frequency of consumption of the 70 foods was reported at 9 levels of intake from never to every day. In addition, there were 7 dietary behavior queries on food preparation methods and fat intake, 1 on fiber intake, and 13 on vitamin and mineral intakes.
The Mediterranean diet score proposed by Panagiotakos et al. (16) was used to evaluate aMED. However, the aMED score was slightly modified to better capture the dietary habits of North Americans. aMED takes into consideration several foods commonly used by Mediterranean populations. Each food has a score from 0 (less adherent) to 5 (better adherence); the total score ranges from 0 to 55, with higher scores indicating a higher aMED. Cereals (e.g., bread, pasta, rice), potatoes, fruits, vegetables, legumes, and fish were categorized (in servings per month) as 0 = never, 1 = 1–4, 2 = 5–8, 3 = 9–12, 4 = 13–18, and 5 = >18. Because no information about the consumption of whole cereals compared with refined cereals was collected, all types of grains were considered in our analyses under the same heading. Red meat, poultry, and full-fat dairy product (e.g., milk, cheese, yogurt) consumption was categorized (in servings per month) as 0 = ≥18, 1 = 13–17, 2 = 9–12, 3 = 5–8, 4 = 1–4, and 5 = never. The use of olive oil was categorized (in times per week) as 0 = never, 1 = rarely, 2 = ≤1, 3 = 2, 4 = 3–6, and 5 = daily. Finally, alcoholic beverages were categorized (in milliliters per day) as 0 = ≥700 or 0, 1 = 600–699, 2 = 500–599, 3 = 400–499, 4 = 300–399, and 5 = <300.
Outcomes
Quality of life was considered as the primary outcome and investigated through the 12-Item Short-Form Health Outcome Survey (SF-12) (17). This score is compiled from 12 questions that were summarized by the physical composite scale (PCS) score and mental composite scale (MCS) (17). The range of possible final SF-12 scores is 0–100, with higher scores indicating better health status and quality of life (17).
As for secondary outcomes, we included the Western Ontario and McMaster Universities Arthritis Index (WOMAC) (18). The WOMAC is a validated scale for assessing the presence of pain, stiffness, and physical functioning (or disability) caused by osteoarthritis. Both knees were considered in the OAI. The responses for each subscale (pain, stiffness, disability) were categorized on a 5-point Likert scale ranging from none (0 points) to extreme (4 points) (18). The maximum possible score was 68, and the final score was normalized to 100 (range: 0–100), with higher scores reflecting greater activity limitations (18). The presence of any depressive symptoms was derived from the 20-item Center for Epidemiologic Studies Depression Scale (CES-D) instrument (19). The range of possible scores was 0–60, with higher scores indicating more depressive symptoms (19).
Covariates
We selected potential self-reported confounders in the OAI that might influence the relation between aMED and outcome variables of interest (SF-12, WOMAC, and CES-D). Physical activity was evaluated with the use of the validated Physical Activity Scale for the Elderly (20). This scale covers 12 different activities (e.g., walking, sports, housework), is scored from 0 without a maximum score, and includes the following covariates: race, smoking status, educational status, and annual income.
Validated general health measures of self-reported comorbidities were assessed by calculating a modified Charlson comorbidity score, with higher scores indicating an increased severity of conditions (21). Of the several medical conditions assessed through the Charlson comorbidity score, we reported descriptively the prevalence of fractures, heart failure, stroke, chronic obstructive pulmonary disease, diabetes, and cancer.
Statistical analyses
For continuous variables, normal distributions were tested with the use of the Kolmogorov-Smirnov test. The data are shown as means ± SDs for quantitative measures and frequency and percentages for all discrete variables. P values were calculated as follows. For continuous variables, differences between the means of the covariates by aMED quintiles were calculated with the use of ANOVA, and a chi-square test was applied for discrete variables. Levene’s test was used to test the homoscedasticity of variances, and if its assumption was violated, Welch’s ANOVA was used. Post hoc analyses and Bonferroni adjustment were applied to compare data. Corrected P values (P < 0.0005) from a Student’s t test were reported when the P value from the ANOVA was significant.
Multivariate linear regression models were calculated with the use of aMED as the exposure and the following as outcomes: SF-12 MCS, SF-12 PCS, WOMAC (and its subscales, i.e., pain, stiffness, disability) for the right and left knees, and CES-D. Factors significantly different across aMED quintiles (taking P < 0.10) or significantly associated with ≥1 outcome during the univariate analysis (P < 0.05) were included. Multicollinearity among covariates was assessed through a variance inflation factor, with a score of 2 resulting in the exclusion of a variable. The Physical Activity Scale for the Elderly showed a variance inflation factor >2 in analyses regarding SF-12 and was consequently excluded from all analyses. The basic model was not adjusted for any confounders. The fully adjusted model included age, sex, race, BMI, educational status, smoking status, annual income, Charlson comorbidity index, use of analgesic drugs, and total energy intake. Linear regression data are reported as βs (95% CIs).
In a similar way, a logistic regression analysis was calculated. aMED was categorized as higher (fourth and fifth quintiles) compared with lower adherence (first, second, and third quintiles). In addition, except for CES-D, for which a cutoff of 16 indicates the presence of depressive symptoms (19), the outcomes were divided by the median value of the sample included in this research. Similarly, we ran the same analyses taking the single components of the Mediterranean diet as the outcome and dividing the adherence in low (0 to 3 over 5 points) and high (4 or 5). Adjusted ORs and 95% CIs were finally calculated to estimate the strength of the associations between aMED and the outcomes.
All analyses were performed with the use of SPSS version 21.0 (IBM). All statistical tests were 2-tailed, and P < 0.05 was assumed to be statistically significant.
RESULTS
Sample selection
All participants in this study were recruited as part of the ongoing multicenter and longitudinal OAI study initially including 4796 American participants, of which 243 were excluded because of missing aMED data or unreliable caloric intake (<500 or >5000 kcal/d; cutoffs suggested in the OAI as unreliable caloric intake). A further 83 participants were excluded because of missing data on the outcomes of interest. The final sample size was 4470 participants (1865 men and 2605 women) (Supplemental Figure 1).
Descriptive characteristics
The mean ± SD age of the participants was 61.3 ± 9.2 y (range: 45–79 y). The mean ± SD aMED score was 28.1 ± 5.1 (range: 5–44).
Table 1 shows the baseline characteristics by aMED quintiles. Those in the highest quintile (reflecting higher aMED) were older and more likely to be women, white, and have a higher educational status and income than those within the other quintiles, whereas no differences emerged for self-reported physical activity. Those in the highest quintile of aMED were leaner (as shown by lower BMI values) and less frequently had fractures and diabetes, but a higher presence of cancer was seen in this quintile than in the other quintiles (Table 1).
TABLE 1.
Descriptive findings of the participants by aMED1
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | P value | |
| n | 1076 | 888 | 1008 | 870 | 628 | |
| aMED score | 21.4 ± 2.62 | 26.1 ± 0.8 | 29.0 ± 0.8 | 32.0 ± 0.8 | 35.8 ± 2.0 | <0.0001 |
| Energy intake, kcal/d | 1407 ± 609 | 1388 ± 552 | 1432 ± 586 | 1423 ± 544 | 1416 ± 515 | 0.53 |
| Age, y | 59.0 ± 8.8 | 61.2 ± 9.0a,b | 61.6 ± 9.3a,c | 62.7 ± 9.0b,c,d | 63.2 ± 9.2d | <0.0001 |
| PASE, points | 158.9 ± 83.8 | 160.7 ± 79.8 | 166.4 ± 82.6 | 157.3 ± 79.1 | 158.6 ± 81.8 | 0.11 |
| Women | 555 (51.6)3 | 525 (59.1) | 607 (60.2) | 520 (59.8) | 398 (63.4) | <0.0001 |
| Whites | 754 (70.1) | 698 (78.6) | 824 (81.7) | 761 (87.5) | 547 (87.1) | <0.0001 |
| Smoking, previous or current | 485 (45.4) | 407 (46.1) | 459 (45.9) | 429 (49.5) | 305 (49.0) | 0.57 |
| Degree | 244 (22.7) | 263 (29.7) | 295 (29.3) | 321 (36.9) | 234 (37.3) | <0.0001 |
| Yearly income <$50,000 | 563 (54.7) | 524 (60.6) | 596 (61.0) | 549 (65.2) | 406 (67.6) | <0.0001 |
| Medical conditions | ||||||
| BMI, kg/m2 | 29.8 ± 4.9 | 29.2 ± 4.8 | 28.4 ± 4.7a | 28.0 ± 4.7a,b | 27.3 ± 4.5b | <0.0001 |
| Knee osteoarthritis | 264 (25.9) | 203 (24.3) | 230 (24.0) | 219 (26.3) | 119 (19.7) | 0.16 |
| Hip osteoarthritis | 61 (5.9) | 70 (8.2) | 78 (8.0) | 75 (8.9) | 35 (5.8) | 0.16 |
| Hand osteoarthritis | 155 (14.9) | 135 (15.8) | 181 (18.6) | 171 (20.2) | 105 (17.3) | 0.08 |
| Fractures | 93 (8.3) | 47 (5.4) | 61 (6.2) | 41 (4.8) | 29 (4.7) | 0.004 |
| Heart attack | 29 (2.8) | 18 (2.1)) | 14 (1.4) | 8 (0.9) | 20 (3.2) | 0.08 |
| Heart failure | 27 (2.5) | 23 (2.6) | 15 (1.5) | 13 (1.5) | 11 (1.8) | 0.88 |
| Stroke | 32 (3.0) | 35 (4.0) | 22 (2.2) | 21 (2.4) | 23 (3.7) | 0.52 |
| COPD | 28 (2.7) | 20 (2.3) | 22 (2.2) | 15 (1.8) | 12 (1.9) | 1.00 |
| Diabetes | 102 (9.8) | 82 (9.4) | 73 (7.3) | 52 (6.1) | 27 (4.4) | <0.0001 |
| Cancer | 22 (2.1) | 33 (3.8) | 43 (4.3) | 36 (4.2) | 32 (5.1) | 0.04 |
| Charlson comorbidity score | 0.4 ± 0.9a,b,c,d | 0.5 ± 0.9a,e,f | 0.4 ± 0.8b,e,g,h | 0.3 ± 0.8c,g,i | 0.4 ± 0.8d,f,h,i | 0.03 |
| Use of analgesic drugs | 452 (42.2) | 362 (40.9) | 415 (41.3) | 343 (39.6) | 236 (37.8) | 1.00 |
P values were calculated with the use of ANOVA and the chi-square test for continuous and categorical variables, respectively. When the P value from the ANOVA was significant, means not sharing a common superscript letter are significantly different at P < 0.0005 based on a Bonferroni-corrected P value from a Student’s t test. aMED, adherence to Mediterranean diet; COPD, chronic obstructive pulmonary disease; PASE, Physical Activity Scale for the Elderly.
Mean ± SD (all such values).
n (%) (all such values).
Quality of life parameters and aMED
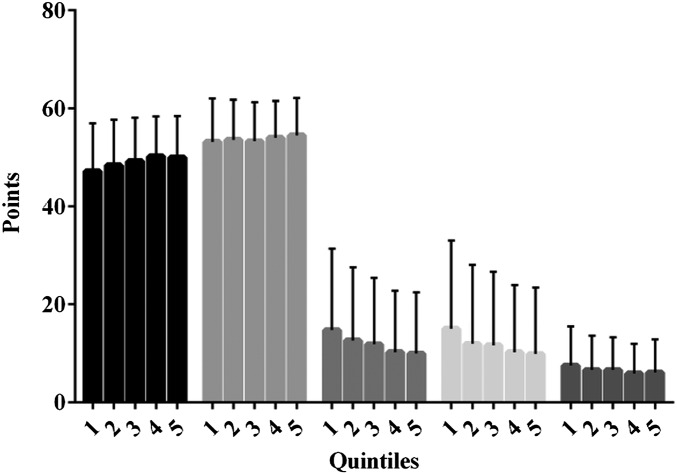
As shown in Figure 1, those with a higher aMED showed significantly higher SF-12 PCS (quintile 5: 50.0 ± 8.5 compared with quintile 1: 47.2 ± 9.8; P < 0.0001) and SF-12 MCS scores (quintile 5: 54.5 ± 7.6 compared with quintile 1: 53.2 ± 8.8; P < 0.0001). The participants with a higher aMED showed significantly lower WOMAC scores (right knee—quintile 5: 9.9 ± 12.5 compared with quintile 1: 14.7 ± 16.6 points; P < 0.0001; left knee—quintile 5: 9.8 ± 13.6 compared with quintile 1: 15.0 ± 18.0; P < 0.0001)—i.e., less pain and disability—and CES-D scores (quintile 5: 6.1 ± 6.7 compared with quintile 1: 7.5 ± 8.0; P < 0.0001)—i.e., fewer depressive symptoms (Figure 1).
FIGURE 1.
Mean ± SD scores of SF-12, WOMAC (total scores), and CES-D by quintiles of aMED. P values were calculated with the use of ANOVA for all comparisons. All P values were <0.0001 after applying Bonferroni’s correction. The outcomes compared (from left to right) were the SF-12 physical composite scale, the SF-12 mental health composite scale, WOMAC (left and right knees), and the CES-D. aMED, adherence to Mediterranean diet; CES-D, Center for Epidemiologic Studies Depression Scale; SF-12, 12-Item Short-Form Health Survey; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Table 2 shows linear regression analyses with aMED as the exposure variable and the SF-12 items, WOMAC scores, and CES-D scores as the outcomes. After adjusting for potential confounders, higher aMED scores were significantly associated with higher SF-12 PCS (β: 0.10; 95% CI: 0.05, 0.15; P < 0.0001), lower WOMAC total scores (except for stiffness), and lower CES-D scores (β: −0.05; 95% CI: −0.09, −0.01; P = 0.01).
TABLE 2.
Association between aMED and SF-12, WOMAC, and CES-D scores1
| Unadjusted linear regression |
Fully adjusted linear regression |
|||
| β (95% CI) | P value | β (95% CI) | P value | |
| SF-12 | ||||
| MCS | 0.08 (0.04, 0.13) | 0.001 | 0.02 (−0.03, 0.07) | 0.37 |
| PCS | 0.22 (0.17, 0.27) | <0.0001 | 0.10 (0.05, 0.15) | <0.0001 |
| WOMAC | ||||
| Right knee pain | −0.07 (−0.09, −0.06) | <0.0001 | −0.02 (−0.04, −0.01) | 0.008 |
| Right knee stiffness | −0.02 (−0.03, −0.01) | <0.0001 | 0.03 (−0.02, 0.08) | 0.20 |
| Right knee disability | −0.24 (−0.30, −0.18) | <0.0001 | −0.08 (−0.14, −0.03) | 0.004 |
| Right knee total | −0.33 (−0.42, −0.25) | <0.0001 | −0.11 (−0.19, −0.04) | 0.004 |
| Left knee pain | −0.07 (−0.09, −0.05) | <0.0001 | −0.02 (−0.04, −0.003) | 0.02 |
| Left knee stiffness | −0.03 (−0.04, −0.02) | <0.0001 | −0.008 (−0.02, 0.002) | 0.11 |
| Left knee disability | −0.24 (−0.30, −0.17) | <0.0001 | −0.07 (−0.14, −0.01) | 0.02 |
| Left knee total | −0.33 (−0.43, −0.24) | <0.0001 | −0.11 (−0.19, −0.02) | 0.02 |
| CES-D | −0.11 (−0.16, −0.07) | <0.0001 | −0.05 (−0.09, −0.01) | 0.01 |
Data were obtained through a linear regression analysis. The fully adjusted model included the following as covariates: age, sex, race, BMI (in kg/m2), education, smoking status, annual income, Charlson comorbidity index, use of analgesic drugs, and total energy intake. P < 0.05 was considered significant after adjusting for all covariates in the fully adjusted model. aMED, adherence to Mediterranean diet; CES-D, Center for Epidemiologic Studies Depression Scale; MCS, mental health composite scale; PCS, physical composite scale; SF-12, 12-Item Short-Form Health Survey; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Table 3 shows a logistic regression analysis taking the 2 quintiles with higher aMEDs as the comparison. After adjusting for potential confounders, lower aMED was significantly associated with lower quality of life (OR: 1.20; 95% CI: 1.05, 1.38; P = 0.01 for SF-12 MCS and OR: 1.19; 95% CI: 1.01, 1.39; P = 0.03 for SF-12 PCS). Conversely, no significant association emerged between aMED and WOMAC or CES-D except for WOMAC right knee total score (OR: 1.17; 95% CI: 1.02, 1.33; P = 0.03).
TABLE 3.
Association between low aMED and poor SF-12, WOMAC, and CES-D scores1
| Unadjusted OR (95% CI) | P value | Fully adjusted OR (95% CI) | P value | |
| SF-12 | ||||
| MCS | 1.35 (1.17, 1.57) | <0.0001 | 1.20 (1.05, 1.38) | 0.01 |
| PCS | 1.39 (1.22, 1.57) | <0.0001 | 1.19 (1.01, 1.39) | 0.03 |
| WOMAC | ||||
| Right knee pain | 1.29 (1.14, 1.47) | <0.0001 | 1.11 (0.98, 1.28) | 0.11 |
| Right knee stiffness | 1.14 (1.00, 1.30) | 0.05 | 1.02 (0.89, 1.17) | 0.78 |
| Right knee disability | 1.33 (1.17, 1.50) | <0.0001 | 1.14 (0.99, 1.30) | 0.07 |
| Right knee total | 1.37 (1.21, 1.55) | <0.0001 | 1.17 (1.02, 1.33) | 0.03 |
| Left knee pain | 0.78 (0.69, 0.89) | <0.0001 | 0.91 (0.80, 1.04) | 0.19 |
| Left knee stiffness | 1.19 (1.05, 1.35) | 0.006 | 1.07 (0.94, 1.22) | 0.32 |
| Left knee disability | 1.20 (1.06, 1.34) | 0.006 | 1.02 (0.89, 1.16) | 0.80 |
| Left knee total | 1.22 (1.08, 1.38) | 0.002 | 1.04 (0.91, 1.19) | 0.60 |
| CES-D | 1.57 (1.25, 1.96) | <0.0001 | 1.22 (0.96, 1.55) | 0.10 |
Data were obtained through a logistic regression analysis. aMED was categorized with the use of the fourth and fifth quintiles (higher adherence = reference) compared with the other 3 quintiles. Median values for all scores were considered for the logistic regression analysis except for CES-D, for which 16 was considered to be the cutoff of clinical depression. The fully adjusted model included the following as covariates: age, sex, race, BMI (in kg/m2), education, smoking status, annual income, Charlson comorbidity index, use of analgesic drugs, and total energy intake. P < 0.05 was considered significant after adjusting for all covariates in the fully adjusted model. aMED, adherence to Mediterranean diet; CES-D, Center for Epidemiologic Studies Depression Scale; MCS, mental health composite scale; PCS, physical composite scale; SF-12, 12-Item Short-Form Health Survey; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Supplemental Table 1 shows the adjusted logistic regression analyses of singular components of the Mediterranean diet and the outcomes of interest in our research. Taking those with a higher adherence as the reference group (scoring 4 or 5 on each component), participants with a lower adherence to vegetables had increased odds of having low SF-12 PCS (OR: 1.52; 95% CI: 1.10, 2.13; P = 0.01) and depression (OR: 1.72, 95% CI: 1.14, 2.63; P = 0.01). In addition, people with a lower consumption of fish were at higher odds of reporting right knee pain (OR: 1.27; 95% CI: 1.00, 1.61; P = 0.048). Participants with a higher consumption of poultry were more likely to report depression (OR: 1.34, 95% CI: 1.07, 1.67; P = 0.01) (Supplemental Table 1).
DISCUSSION
We have demonstrated in this large cross-sectional study that North Americans who are more adherent to the Mediterranean diet also reported a substantially better quality of life and decreased pain, disability, and depressive symptoms.
The traditional Mediterranean diet is characterized by a high intake of olive oil, fruits, nuts, vegetables, and cereals; moderate intake of fish and poultry; low intake of dairy products, red meat, processed meats, and sweets; and moderate intake of wine (ideally red). As recently shown by the Prevention with Mediterranean Diet trial (22), this dietary pattern is efficacious in reducing cardiovascular events in people at a higher risk of cardiovascular conditions. However, data regarding the impact of Mediterranean diet on quality of life are still missing from the literature.
As expected, those with a higher aMED had a significantly lower BMI and proportion of diabetes but significantly higher education than other participants. However, those who demonstrated a higher aMED were significantly older, which is in agreement with previous research (23). Altogether, these findings suggest that participants with a higher aMED have a better overall health profile, which likely influences our findings of a relation between the Mediterranean diet and quality of life. Nonetheless, we adjusted for the prevalence of many physical health comorbidities in our data, and the results seemed to be robust. However, we did find some evidence that suggests that there was a small difference in the self-reported prevalence of cancer according to aMED quintile. This potential finding could be attributed to chance (P = 0.04) or to the fact that participants in this group were older and had a higher educational status (P < 0.0001) and annual income (P < 0.0001) and thus probably better access to health care; therefore, cancer may have been detected earlier.
Of particular relevance is the finding of a higher aMED with a lower prevalence of fractures. Specifically, participants in quintile 5 had almost half the prevalence of fractures than those in quintile 1, and it is largely known that bone fractures are associated with worse quality of life. Our findings seem to support a recent study (2) that showed that the Mediterranean diet is associated with a reduced risk in hip fracture in postmenopausal women. Thus, the protective effect of the Mediterranean diet may have contributed to our finding that a higher aMED is associated with better quality of life.
After adjusting for potential confounders (including severity of comorbidity and social and economic factors), our data showed that the association between aMED and SF-12, WOMAC, and CES-D was only partially attenuated. These results suggest that the Mediterranean diet could be associated with better quality of life, which may be related through mechanisms leading to a decrease of cardiovascular and metabolic diseases (22, 24). A first hypothesis is linked to the fact that a higher aMED is associated with a decrease in inflammation (25) because inflammation is linked to worse quality of life (26). Another potential mechanism is the impact of the Mediterranean diet on oxidative stress markers (27), which is another pathway associated with poor quality of life. Moreover, the Mediterranean diet seems to increase adiponectin (28), a hormone secreted by adipose tissue, with relevant insulin-sensitizing, antidiabetogenic, and anti-inflammatory effects. Our data seem to indirectly support this hypothesis because people with a higher aMED had lower BMI values even if they reported similar daily calorie intake. Finally, the Mediterranean diet also has important antiatherosclerotic effects (29), even if other factors play a role. Because atherosclerosis is associated with worse quality of life (30), this might explain the association between higher aMED and quality of life.
Regarding the other outcomes, our data also suggest that a higher aMED is associated with less pain, disability, and depressive symptoms. Our findings about pain are in agreement with the current literature that attributes the Mediterranean diet as having anti-inflammatory and analgesic effects (31). The potential influence of the Mediterranean diet on disability is less established. However, a recent study (6) showed that a higher aMED was associated with a longer life without disability. Our data also suggest that a higher aMED is associated with less depressive symptoms (32). This relation might be related to prior research suggest that a higher aMED is associated with better cognitive performance, which may also influence the significant association with depression (33).
Finally, we also found that the Mediterranean diet had a more favorable effect on each of these outcomes when considered collectively rather than when considered as singular dimensions of the diet. Our findings regarding the adherence to singular components are sparse because only those participants with a lower consumption of vegetables and fish had worse quality of life. Therefore, our data suggest that people seeking to acquire the health benefits described herein should follow this dietetic regimen as a whole rather than as singular components.
The findings of our research should be considered within their limitations. The main limitation is the cross-sectional nature of our research. Thus, residual confounding (e.g., socioeconomic status) is very likely. It is also possible that a reverse causation may be evident; i.e., participants with better quality of life eat better. Clearly, future longitudinal research is required to disentangle the directionality of these variables. Second, we were not able to consider the influence of biohumoral markers in the association between Mediterranean diet and outcomes. Nonetheless, these markers could be of importance. A third limitation is that the medical conditions are self-reported, which could have introduced bias. In addition, we used a slightly modified version of a previous Mediterranean diet adherence (16), thus possibly introducing another bias.
Our study also has several strengths, including the large sample size and the fact that only North Americans were included. Because of unhealthy dietary habits in Westernized countries, including the United States, these findings emphasize that the Mediterranean diet may be one way to improve quality of life.
In conclusion, our data suggest that a higher aMED is associated with better quality of life and decreased pain, disability, and depressive symptoms. Our findings suggest that this dietary pattern may have a beneficial effect on several aspects linked to disability and thus may lead to healthier aging.
Acknowledgments
The authors’ responsibilities were as follows—NV and MN: analyzed the data; BS, MS, and CL: wrote the manuscript; SM: had primary responsibility for the final content; and all authors: read and approved the final manuscript. None of the authors reported a conflict of interest related to the study.
Footnotes
Abbreviations used: aMED, adherence to the Mediterranean diet; CES-D, Center for Epidemiologic Studies Depression Scale; MCS, mental composite scale; OAI, Osteoarthritis Initiative; PCS, physical composite scale; SF-12, 12-Item Short-Form Health Outcome Survey; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
REFERENCES
- 1.Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, Trichopoulos D. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 1995;61:1402S–6S. [DOI] [PubMed] [Google Scholar]
- 2.Haring B, Crandall CJ, Wu C, LeBlanc ES, Shikany JM, Carbone L, Orchard T, Thomas F, Wactawaski-Wende J, Li W, et al. . Dietary patterns and fractures in postmenopausal women. JAMA Intern Med 2016;176:645–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nissensohn M, Román-Viñas B, Sánchez-Villegas A, Piscopo S, Serra-Majem L. The effect of the Mediterranean diet on hypertension: a systematic review and meta-analysis. J Nutr Educ Behav 2016;48:42–53.e1. [DOI] [PubMed] [Google Scholar]
- 4.Schwingshackl L, Missbach B, König J, Hoffmann G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr 2015;18:1292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cao L, Tan L, Wang H-F, Jiang T, Zhu X-C, Lu H, Tan M-S, Yu J-T. Dietary patterns and risk of dementia: a systematic review and meta-analysis of cohort studies. Mol Neurobiol 2015. Nov 9 (Epub ahead of print; DOI: 10.1007/s12035-015-9516-4). [DOI] [PubMed] [Google Scholar]
- 6.May AM, Struijk EA, Fransen HP, Onland-Moret NC, de Wit GA, Boer JMA, van der Schouw YT, Hoekstra J, Bueno-de-Mesquita HB, Peeters PHM, et al. . The impact of a healthy lifestyle on disability-adjusted life years: a prospective cohort study. BMC Med 2015;13:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pérez-Tasigchana RF, León-Muñoz LM, López-García E, Banegas JR, Rodríguez-Artalejo F, Guallar-Castillón P. Mediterranean diet and health-related quality of life in two cohorts of community-dwelling older adults. PLoS One 2016;11:e0151596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muñoz M-A, Fíto M, Marrugat J, Covas M-I, Schröder H. Adherence to the Mediterranean diet is associated with better mental and physical health. Br J Nutr 2009;101:1821–7. [DOI] [PubMed] [Google Scholar]
- 9.Henríquez Sánchez P, Ruano C, de Irala J, Ruiz-Canela M, Martínez-González MA, Sánchez-Villegas A. Adherence to the Mediterranean diet and quality of life in the SUN Project. Eur J Clin Nutr 2012;66:360–8. [DOI] [PubMed] [Google Scholar]
- 10.Bonaccio M, Di Castelnuovo A, Bonanni A, Costanzo S, De Lucia F, Pounis G, Zito F, Donati MB, de Gaetano G, Iacoviello L. Adherence to a Mediterranean diet is associated with a better health-related quality of life: a possible role of high dietary antioxidant content. BMJ Open 2013;3:e003003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Milte CM, Thorpe MG, Crawford D, Ball K, McNaughton SA. Associations of diet quality with health-related quality of life in older Australian men and women. Exp Gerontol 2015;64:8–16. [DOI] [PubMed] [Google Scholar]
- 12.Abdullah MMH, Jones JPH, Jones PJH. Economic benefits of the Mediterranean-style diet consumption in Canada and the United States. Food Nutr Res 2015;59:27541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Samieri C, Sun Q, Townsend MK, Chiuve SE, Okereke OI, Willett WC, Stampfer M, Grodstein F. The association between dietary patterns at midlife and health in aging: an observational study. Ann Intern Med 2013;159:584–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Felson DT, Nevitt MC. Epidemiologic studies for osteoarthritis: new versus conventional study design approaches. Rheum Dis Clin North Am 2004;30:783–97. [DOI] [PubMed] [Google Scholar]
- 15.Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: development and validation. Epidemiology 1990;1:58–64. [DOI] [PubMed] [Google Scholar]
- 16.Panagiotakos DB, Pitsavos C, Stefanadis C. Dietary patterns: a Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiovasc Dis 2006;16:559–68. [DOI] [PubMed] [Google Scholar]
- 17.Ware J, Kosinski M, Keller SDA. 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–33. [DOI] [PubMed] [Google Scholar]
- 18.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–40. [PubMed] [Google Scholar]
- 19.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 20.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 1999;52:643–51. [DOI] [PubMed] [Google Scholar]
- 21.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care 1996;34:73–84. [DOI] [PubMed] [Google Scholar]
- 22.Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, et al. . Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–90. [DOI] [PubMed] [Google Scholar]
- 23.Inelmen EM, Toffanello ED, Enzi G, Sergi G, Coin A, Busetto L, Manzato E. Differences in dietary patterns between older and younger obese and overweight outpatients. J Nutr Health Aging 2008;12:3–8. [DOI] [PubMed] [Google Scholar]
- 24.Salas-Salvadó J, Bulló M. Reduction in the incidence of type 2 diabetes with the Mediterranean diet. Diabetes Care 2011;34:14–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: the ATTICA study. J Am Coll Cardiol 2004;44:152–8. [DOI] [PubMed] [Google Scholar]
- 26.Nowakowski ACH. Chronic inflammation and quality of life in older adults: a cross-sectional study using biomarkers to predict emotional and relational outcomes. Health Qual Life Outcomes 2014;12:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chatzianagnostou K, Del Turco S, Pingitore A, Sabatino L, Vassalle C. The Mediterranean lifestyle as a non-pharmacological and natural antioxidant for healthy aging. Antioxidants (Basel) 2015;4:719–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fragopoulou E, Panagiotakos DB, Pitsavos C, Tampourlou M, Chrysohoou C, Nomikos T, Antonopoulou S, Stefanadis C. The association between adherence to the Mediterranean diet and adiponectin levels among healthy adults: the ATTICA study. J Nutr Biochem 2010;21:285–9. [DOI] [PubMed] [Google Scholar]
- 29.Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, Willett WC, Rimm EB, Hu FB. Changes in diet quality scores and risk of cardiovascular disease among us men and women. Circulation 2015;131:2212–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dickens C, Cherrington A, McGowan L. Depression and health-related quality of life in people with coronary heart disease: a systematic review. Eur J Cardiovasc Nurs 2012;11:265–75. [DOI] [PubMed] [Google Scholar]
- 31.Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D’Armiento M, D’Andrea F, Giugliano D. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 2004;292:1440–6. (A). [DOI] [PubMed] [Google Scholar]
- 32.Rahe C, Unrath M, Berger K. Dietary patterns and the risk of depression in adults: a systematic review of observational studies. Eur J Nutr 2014;53:997–1013. [DOI] [PubMed] [Google Scholar]
- 33.Knight A, Bryan J, Murphy K. Is the Mediterranean diet a feasible approach to preserving cognitive function and reducing risk of dementia for older adults in Western countries? New insights and future directions. Ageing Res Rev 2016;25:85–101. [DOI] [PubMed] [Google Scholar]