Abstract
Subacute necrotizing sialadenitis (SANS) is an unusual inflammatory condition known to primarily affect the minor salivary glands of the palatal region. Patients usually present with a localized, often erythematous palatal swelling accompanied by an abrupt onset of pain. The disease usually resolves between 2 days and a week with few extrapalatal reports lasting longer than 1 week. We report a series of three cases of SANS involving the palate.
Keywords: Subacute necrotizing sialadenitis, Metaplasia, Palatal swelling
Introduction
Subacute necrotizing sialadenitis (SANS) is an unusual self-limiting, inflammatory condition known to primarily affect the minor salivary glands of the palatal region. SANS was first described by Werning et al. [1] as an erythematous, nonulcerated but painful firm swelling of the posterior hard palate. Lombardi et al. [2, 3] subsequently classified SANS to be a part of the spectrum of the more common, necrotizing sialometaplasia (NS) while others classified it as a separate or independent entity.
To the best of our knowledge, there have been 27 cases of SANS in the literature affecting minor palatal salivary glands and 6 cases affecting extrapalatal minor salivary glands [4–6]. The etiology is still unknown but infectious and allergic origins have been suggested, based on the simultaneous occurrence of close quarter communities and on the spontaneous healing [3]. Patients usually present with a localized, often erythematous palatal swelling accompanied by an abrupt onset of pain [2]. The disease usually resolves between 2 days and a week with few extrapalatal reports lasting longer than 1 week [4].
Upon an incisional biopsy, the lesion is characterized by a nonulcerated nodule of mucosa in which the underlying salivary glands show a subacute inflammation, represented by a mixed infiltrate of lymphocytes and neutrophils. Most of the ductal structures are lost or atrophic and the acinar cells are necrotic [2, 3].
Cases
We searched the oral and maxillofacial pathology archives at Columbia Presbyterian Hospital for cases of SANS over a period of 16 years (2000–2016). A total of 3 cases were reported during this time (Table 1). Age ranged from 26 to 66 years. All three cases were located in the hard palate. A history of palatal swelling was present in all three cases. Bilateral palatal swelling was seen in one case (Case 3, Fig. 1). The duration of the swelling was approximately 7 days. The extent of the swelling varied from unilateral involvement from canine to 2nd molar up the palatal midline to extensive bilateral involvement. Incisional biopsy was performed for all three cases and adequate recovery was seen within 3 weeks.
Table 1.
Clinical features and demographics of patients seen at Columbia Presbyterian Hospital (2000–2016)
| Serial no. | Year | Age (years) | Sex | Race | Presentation | Duration (days) | Location | Size (cm) |
|---|---|---|---|---|---|---|---|---|
| 1 | 2008 | 26 | F | N/A | Extensive unilateral swelling nonulcerated surface | >7 | L palate | 1.2 |
| 2 | 2012 | 66 | F | N/A | Unilateral round erythematous swelling | N/A | L palate | 0.8 |
| 3 | 2016 | 35 | F | N/A | Sudden increased pain and swelling | 7 | L and R palate | 1.5; 1.5 |
SANS subacute necrotizing sialadenitis, M male, F female, N/A not available
Fig. 1.

Bilateral palatal swelling in a 35-year-old patient. Biopsy of the lesion revealed findings consistent with SANS
Histology
The average size of the biopsy specimens was 1.25 cm in the largest dimension. Routine Hematoxylin and Eosin (H and E) stain was performed on representative sections. Microscopic examination revealed intact stratified squamous epithelium and extensive acinar necrosis (Figs. 2, 3) in the minor salivary gland lobules. Focal inflammatory infiltrate consisting of neutrophils, eosinophils, and mononuclear inflammatory cells was noted in the necrotic acini (Fig. 4). No ductal squamous metaplasia was seen.
Fig. 2.

Intact stratified squamous epithelium and extensive acinar necrosis of the palatal lesion (H&E, ×10 magnification)
Fig. 3.
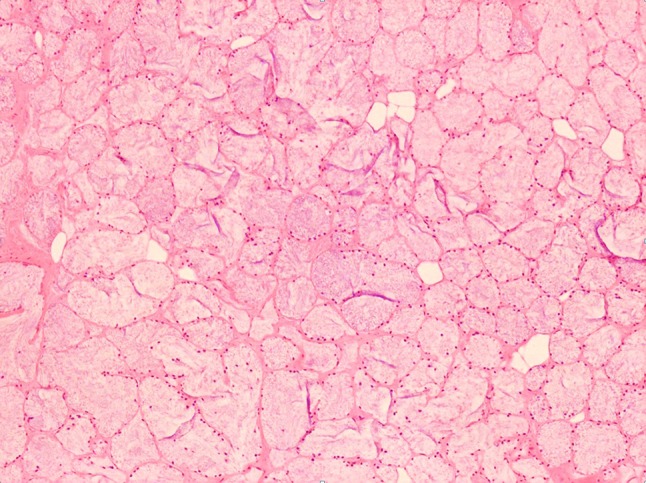
Extensive acinar necrosis in the minor salivary gland lobules (H&E, ×20 magnification)
Fig. 4.
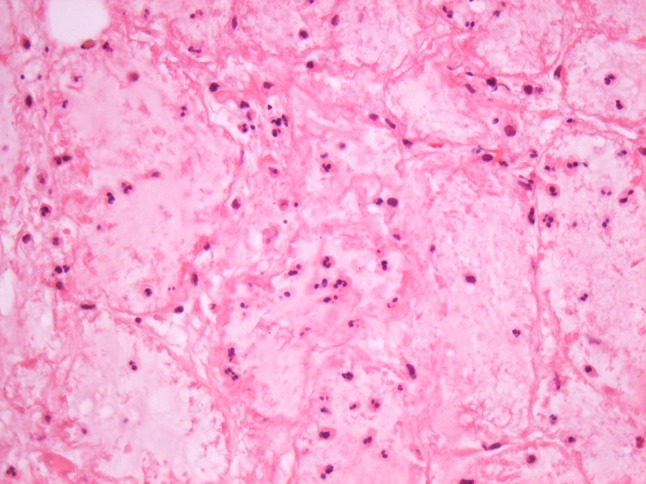
Inflammatory infiltrate consisting of neutrophils and eosinophils noted in the necrotic acini (H&E, ×40 magnification)
Discussion
SANS is generally considered as a rare inflammatory condition involving the minor salivary glands [1–3]. SANS is most commonly seen in teenagers and young adults, and the most frequently described locations are hard or soft palate [1–3]. Many authors see SANS as an unusual subtype or early stage of NS, based on the clinical and histopathologic features [3]. However, others see SANS as a distinct and uncommon condition with only 33 cases reported to this date [4–6]. In our view, SANS is a separate clinical entity that has unique clinical and pathological features. SANS occurs more commonly in younger adults and often present as a painful hard or soft palate nodule with intact mucosa. Unlike NS, SANS does not ulcerate and heals between 2 days and 1 week. NS, on the other hand, often presents in middle-aged adults and surface ulceration is a prominent feature. Average healing time for NS is between 5 and 6 weeks.
We have reviewed a number of reported SANS cases in the literature from 1990 to 2015 and have identified 27 cases in the literature affecting minor palatal salivary glands and 6 cases affecting extrapalatal minor salivary glands [4–6]. In Table 2 we summarize these findings.
Table 2.
Literature review of all reported cases of SANS
| References | No. of cases | Age (years) | Sex | Race | Presentation | Location | Size (cm) |
|---|---|---|---|---|---|---|---|
| Werning et al. [1] | 12 | Range 18–29 (mean 20) | M | 10 W 2 N/A |
Firm painful nodules with erythematous and nonulcerated surface | 8 hard palate 3 soft palate 1 anterior tonsillar pillar |
0.3–1.0 |
| Van der Wal et al. [8] | 3 | 17 | M | N/A | Painful swelling | Hard palate, bilateral | 0.8 |
| 20 | F | N/A | No painful swelling | R hard palate | N/A | ||
| 15 | M | N/A | Painful swelling some of the days’ duration | R hard palate, some days | N/A | ||
| Fowler and Brannon [2] | 7 | 24 | F | W | Nodule with recent pain | R hard palate | 0.5 |
| 15 | F | W | Mildly tender nodule | L, P, hard palate | 1.2 | ||
| 26 | F | W | Swelling | L, P, hard palate | 0.8 | ||
| 45 | M | W | Nodule | R hard palate | N/A | ||
| 37 | F | W | Firm tender mass | R soft palate | 1.5 | ||
| 19 | M | A | Slightly painful | L hard palate | 2.0 | ||
| 24 | M | W | Acutely painful mass | R hard palate | 0.5 | ||
| Castro et al. [7] | 1 | 30 | F | N/A | Painful submucosal nodule of 1 mo duration | L buccal mucosa | N/A |
| Lombardi et al. [3] | 3 | 23 | F | N/A | Slightly painful nodule, bilateral | P hard palate | L 1 |
| 22 | M | N/A | Asymptomatic | P hard palate | R < 1 | ||
| 40 | M | N/A | Unknown | P hard palate | 0.8 | ||
| Suresh et al. [4] | 5 | 51 | M | W | Painful hard mobile lump with rapid increase in size | R buccal mucosa | 1.5 |
| 30 | M | W | Painful swelling with rapid increase in size | Ventral tongue | 1 | ||
| 33 | F | W | Painful swelling with sudden increase in size | R upper lip | 1 | ||
| 70 | F | W | Painful swelling with rapid increase in size | R buccal mucosa | 1 | ||
| 37 | F | W | Painless swelling with gradual increase in size | ventral tongue | 1.5 | ||
| Maloth et al. [5] | 1 | 24 | M | N/A | Painful unilateral round erythematous swelling | R, M palate | 0.7 |
| Eyibilen et al. [9] | 1 | 36 | M | N/A | Fragile tender hemorrhagic mass | L, M palate | 5 × 7 |
SANS subacute necrotizing sialadenitis, M male, F female, N/A not available, W white, A African American, R right, L left, P posterior
Most patients with SANS present to the medical and dental clinic with painful swelling in the minor salivary gland. The mean age of presentation is 27 years (range 15–70). The swelling usually involved the hard or soft palate but buccal mucosa, upper lip, and ventral tongue are also possible locations. The swelling increases in size in days to weeks but can be gradual in onset. Multifocal presentation is rare.
Clinical and microscopic features have pointed towards a traumatic, an infectious, or an allergic etiology [5, 7]. Clinical features that support an infectious origin for SANS include the prevalence of the disease among young adults living in close quarters as well as the immediate onset, localization, and spontaneous resolution of symptoms [1, 2]. In addition, the cases reported from Werning et al. and Fowler suggest an association with upper respiratory tract infection with a peak incidence in the fall and winter seasons. A traumatic etiology is possible but difficult to prove without patient recollection of trauma or evidence of injury. Viral transmission is likely ruled out as there have not been any viral particles found in samples of the affected glands [3]. The presence of few eosinophils and spontaneous healing have suggested that SANS is not of allergic origin [2]. Furthermore, all lesions occurred as solitary lesions with no tendency for multifocality and resolved without the need for topical or systemic medication within 3 weeks’ duration [4].
The differential diagnosis of SANS includes NS and chronic sialadenitis (CS). NS presents a striking analogy with SANS. Both NS and SANS share a similar patient profile, with involvement at a rather younger age in SANS. They share the same site of distribution on the posterior lateral hard palate, with the exception that NS can also affect major salivary glands, nasal cavity, maxillary sinus, and larynx. Lastly, they have similar necrosis of mucous acini of minor salivary glands and both exhibit spontaneous healing [3].
Clinical differences between NS and SANS are the duration and type of symptoms, the clinical appearance, and the length of the healing time. From the reported cases, the average delay preceding diagnosis is shorter for SANS (~1 week) than for NS (~3 weeks) [2]. NS usually presents as a large ulcer of variable pain where SANS is smaller, erythematous swelling, and almost always associated with pain [2]. SANS has not been reported as an ulcer. Histologically, the main difference between NS and SANS is the prominent squamous metaplasia in the regenerating necrotic acini and ducts seen in NS. In SANS, microscopy shows ductal loss and atrophy but squamous metaplasia is normally mild or absent [4].
In conclusion, clinicians should be aware of this unique entity and include it as a diagnostic possibility for patients presenting with nonulcerated painful palatal swellings.
References
- 1.Werning JT, Waterhouse JP, Mooney JW. Subacute necrotizing sialadenitis. Oral Surg Oral Med Oral Pathol. 1990;70:756–759. doi: 10.1016/0030-4220(90)90015-K. [DOI] [PubMed] [Google Scholar]
- 2.Fowler CB, Brannon RB. Subacute necrotizing sialadenitis: report of 7 cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2000;89:600–609. doi: 10.1067/moe.2000.105943. [DOI] [PubMed] [Google Scholar]
- 3.Lombardi T, Samson J, Kuffer R. Subacute necrotizing sialadenitis: a form of necrotizing sialometaplasia? Arch Otolaryngol Head Neck Surg. 2003;129:972–975. doi: 10.1001/archotol.129.9.972. [DOI] [PubMed] [Google Scholar]
- 4.Suresh L, Aguirre A. Subacute necrotizing sialadenitis: a clinicopathological study. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2007;104:385–390. doi: 10.1016/j.tripleo.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 5.Maloth SGK, Latha S, Pai A, Komali B. Subacute necrotizing sialadenitis—a case report. J Indian Acad Oral Med Radiol. 2007;19:345. [Google Scholar]
- 6.Eyibilen AON, Aladağ I, Ozkan F, Kaya Z, Köseoğlu D. An unusual giant subacute necrotizing sialadenitis as an emergency case of otolaryngology. J Ear Nose Throat. 2008;19:216–219. [PubMed] [Google Scholar]
- 7.Castro WH, Drummond SN, Gomez RS. Subacute necrotizing sialadenitis in the buccal mucosa. J Oral Maxillofac Surg. 2002;60:1494–1496. doi: 10.1053/joms.2002.36134. [DOI] [PubMed] [Google Scholar]
- 8.van der Wal JE, Kraaijenhagen HA, van der Waal I. Subacute necrotising sialadenitis: a new entity? Br J Oral Maxillofac Surg. 1995;33(5):302–303. doi: 10.1016/0266-4356(95)90042-X. [DOI] [PubMed] [Google Scholar]
- 9.Eyibilen A, Ozkan NC, Aladağ I, Ozkan F, Kaya Z, Köseoğlu D. An unusual giant subacute necrotizing sialadenitis as an emergency case of otolaryngology. Kulak Burun Bogaz Ihtis Derg. 2009;19(4):216–219. [PubMed] [Google Scholar]


