Abstract
Global and national HIV/AIDS policies utilize the care cascade to emphasize the importance of continued engagement in HIV services from diagnosis to viral suppression. Several studies have documented barriers that men experience in accessing services at specific stages of care, but few have analyzed how these barriers operate along the care cascade. Brazil offers a unique setting for analyzing barriers to HIV care because it is a middle-income country with a large HIV epidemic and free, universal access to HIV/AIDS services. Semi-structured interviews were conducted in 2011 with HIV-infected men (n=25) receiving care at the only HIV/AIDS state reference center in Salvador, Brazil, the third largest city in the country. Interviews were transcribed and coded for analysis. Researchers identified barriers to services along the care cascade: health service-related obstacles (poor quality care, lengthy wait times, and drug supply problems); psychosocial and emotional challenges (fear of disclosure and difficulty accepting HIV diagnosis); indirect costs (transportation and absenteeism at work or school); low perceived risk of HIV; and toxicity and complexity of ARV regimens. The stages of the care cascade interrupted by each barrier were also identified. Most barriers affected multiple, and often all, stages of care, while toxicity and complexity of ARV regimens was only present at a single care stage. Efforts to eliminate more prevalent barriers have the potential to improve care continuity at multiple stages. Going forward, assessing the relative impact of barriers along one's entire care trajectory can help tailor improvements in service provision, facilitate achievement of viral suppression, and improve access to life-saving testing, treatment, and care.
Keywords: HIV/AIDS, care cascade, barriers, men, delay, Brazil
INTRODUCTION
Viral suppression minimizes HIV-related morbidity and mortality and reduces HIV transmission (Cohen et al., 2011; Gardner et al 2011). Antiretroviral drugs (ARVs) can effectively suppress viral loads, but late diagnosis, delayed linkage to care, and interruptions in adherence can compromise viral suppression, promote HIV progression, and facilitate ARV resistance (Anglaret et al., 2012; Harrigan et al., 2005; Hogan et al., 2012). As such, research has attempted to understand and improve linkages between stages of HIV care that collectively make up the HIV care cascade. The care cascade defined by the U.S. Centers for Disease Control and Prevention includes: HIV diagnosis, linkage to care, retention in care, ARV provision, and viral suppression (CDC, 2013).
Brazil, one of the first countries to guarantee free, universal ARV provision, has utilized the care cascade to assess national engagement in care. An estimated 80% of HIV-infected individuals know their HIV status, but only 33% maintain undetectable viral loads (Ministry of Health, 2013). Notably, in 2012, men comprised 65% of AIDS cases, and HIV-infected men experienced nearly double the mortality rate of women (Ministry of Health, 2013). While factors like male gender, older age, and substance use have been associated with delays at specific care stages (de Almeida et al., 2014; Grangeiro et al., 2012; Guimaraes et al., 2008; Souza et al., 2010), few studies have analyzed how barriers impede access to services along the entire care cascade, particularly in resource-limited settings (Mukolo et al., 2013). Therefore, to improve the quality of HIV services, we explored barriers affecting HIV infected-men at each stage of care in Salvador, Brazil.
METHODS
Semi-structured interviews were conducted with 25 HIV-infected men in Salvador, Brazil's third largest – and one of its lowest-income – cities. Through convenience sampling, members of the research team invited patients of a previous quantitative survey to participate in an interview at the time of a scheduled medical consultations or pharmacy visit at Salvador's only State Reference Center in 2011. For the quantitative survey, a list of scheduled patients at the State Reference Center had been provided to the study team, and staff members invited all patients to participate. To be included the study, participants must have been 18 or older and laboratory confirmed HIV diagnosis. Participants were excluded if they had received initial HIV/AIDS care at another health facility or were diagnosis with mental health disorders. Interview scripts were extensively field-tested and included open-ended questions about participants’ care trajectory, sexual behavior, and social experiences related to HIV. Interviews were conducted individually in private rooms after obtaining informed consent. No compensation was given for participation. All interviews were recorded, transcribed, and analyzed in Portuguese.
Barriers were defined as experiences reported by men that delayed or impeded access to HIV diagnosis, linkage to care, retention in care, ARV provision, or continued treatment to achieve viral suppression. Two authors (LV, ID) identified initial themes to code data through a literature review and deductively coded transcripts using NVivo software (QSR International) (Crabtree & Miller, 1999). Researchers (MH, SM, AB) identified barriers reported in transcripts and inductively coded themes emerging outside the literature (Boyatzis, 1998). During this process, common categories of barriers emerged. Outliers were explored by analyzing responses according to employment status, drug use, and sexual behavior to determine whether these socio-demographic characteristics were tied to any identified barriers.
RESULTS
Participant socio-demographic characteristics are summarized in Table 1. Men reported health service-related obstacles (perceived poor quality care, lengthy wait times, and drug supply problems); psychosocial and emotional challenges (fear of disclosure and difficulty accepting HIV diagnosis); indirect costs (transportation and absenteeism at work or school); low perce ived risk of HIV; and toxicity and complexity of ARV regimens. Most barriers interrupted multiple stages of the care cascade, while toxicity and complexity of ARV regimens was only present at a single stage.
Table 1.
Socio-demographic characteristics among men (n=25) receiving HIV/AIDS care at the Reference Center in Salvador, Brazil
| Variable | N |
|---|---|
| Age | |
| Less than 35 years | 7 |
| 35-44 | 8 |
| 45 and above | 10 |
| Color/ethnicitya | |
| Brown | 10 |
| Black | 11 |
| Other | 4 |
| Sexual behavior | |
| Men who have sex with only women | 9 |
| Men who have sex with men | 16 |
| Civil status | |
| With partner | 6 |
| Without partner | 19 |
| Employment | |
| Unemployed | 12 |
| Employed (formally or informally) | 13 |
| Residence | |
| Salvador | 21 |
| Outside Salvador | 4 |
| Length of time since diagnosis with HIV | |
| Less than 2 years | 6 |
| Between 2 and 5 years | 12 |
| 5 or more years | 7 |
| On treatment for HIV at the time of the interview | |
| Yes | 15 |
| No | 10 |
| Ever used drugs | |
| Yes | 8 |
| No | 17 |
| Current or previous known STD | |
| Yes | 14 |
| No | 11 |
Race in Brazil is commonly referred to as ‘cor’ or ‘color,’ referencing a person's phenotype (physical appearance) rather than one's ancestry (origin).
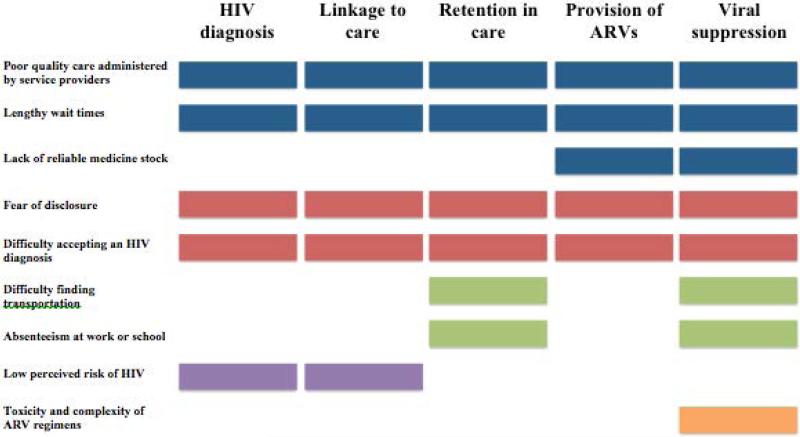
Among service-related obstacles, dissatisfaction with care from service providers and lengthy wait times negatively affected access to every care stage, while drug supply problems obstructed ARV provision and continued treatment. Emotional and psychosocial challenges impeded engagement at every stage. Indirect costs limited retention in care and continued treatment. Low perceived risk of HIV infection and disease progression delayed diagnosis and linkage to care.Toxicity and complexity of ARV regimens interrupted continued treatment. Notably, among socio-demographic characteristics explored, barriers differed only by sexual behavior: all men who have sex with men (MSM) feared disclosure and reported common experiences with HIV-related stigma, discrimination, violence, and homophobia. Nonetheless, about half of the study's men who had sex with only women (MSW) also reported fear of disclosure and often described experiences of HIV-related stigma and discrimination. In sum, HIV-infected men in Salvador, Brazil face many barriers that collectively impede access to care at every stage. Results are further detailed in Figure 1 and example quotes are found in Table 2.
Figure 1.
Barriers along the care cascade among men (n=25) receiving HIV/AIDS care at the Reference Center in Salvador, Brazil
Table 2.
Quotes illustrating summary examples of barriers identified from qualitative interviews
| Barriers | Quote illustrating summary examples of barriers |
|---|---|
| Poor quality care administered by service providers (n=11) | [The pharmacist made a] bad joke ... People working in healthcare need to be prepared to work with patients who face this type of problem [HIV]. |
| Lengthy wait times (n=18) | We call in advance and can't contact anyone. There is no communication... When we come, they don't want to give us the medication. They want to reschedule again. I already went a week without taking my medication because of this. |
| Reliable medicine stock (n=6) | It's scary...One time the girl told me ‘there's no medicine.’ I thought, ‘If I don't take my medicine, my viral load will rise ...and what will I do?’ That is my biggest worry: not having the ability to continue my treatment, the disease progresses, and I don't survive. |
| Fear of disclosure (n=21) | I saw someone I knew, and I left. I didn't want to pick up the [test] result. |
| Difficulty accepting an HIV diagnosis n=19) | Why didn't I seek treatment? Because I was denying that I had this disease.... |
| Difficulty finding transportation (n=15) | It's difficult for me because I have to leave my city to come here. Sometimes I don't have enough money to pay for the trip. |
| Absenteeism at work or school (n=6) | I [asked the receptionist], ‘Can you look for another date that's better?’ because of work, so as to not interrupt my schedule. |
| Low perceived risk (n=4) | [Interviewer]: Why didn't you pick up the test result? ... [Participant]: I honestly thought that it was impossible for me to get that... [Interviewer]: You learned the result and disappeared for a year... [Participant]: I thought ‘Oh, because [my other STI] was cured, I wouldn't have to deal with that anymore’. Without thinking that I really had this disease... |
| Toxicity and complexity of ARV regimens (n=22) | I take [the medication] and I don't, ...I've had negative reactions to the majority of the drugs.... I'm still trying to find a better combination |
DISCUSSION
With respect to health service provision, poor quality care and lengthy wait times were common reasons for disengagement in all stages of HIV care. Prior studies in Brazil and other high- and low-income settings found that similar service-related obstacles discouraged HIV testing, exacerbated loss to follow-up, and increased likelihood of non-adherence (Bezabhe et al., 2014; Bonolo et al., 2005; de Almeida et al., 2014; Lorenc et al., 2011; Meyerson et al., 2014; Schuster et al., 2005). Measures to improve patient satisfaction and diminish wait times are necessary steps to enhancing care continuity. Potential strategies include training health care workers to address specific complaints that emerged from the interviews including confidentiality and provider-patient interactions; adequately matching demand for care with provider availability; and improving organizational procedures to expedite care.
While participant descriptions of poor quality care and wait times are consistent with current literature, the availability of ARVs in Brazil is disputed. Reports of a limited drug supply are concerning given Brazil's guarantee of ARVs and adoption of a test-and-treat strategy (Ministry of Health, 2013). While some studies have reported drug shortages (Melchior et al., 2006; Ribeiro et al., 2012), a national survey of providers described sufficient ARV stock (Nemes et al., 2013). Given these discrepancies, future research should investigate HIV drug supply in Brazil and its impact on patient care.
Emotional and psychosocial challenges, including fear of disclosure and difficulty accepting an HIV diagnosis, limited access to all care stages. These results are consistent with prior research (Kerr et al., 2013; Melchior et al., 2007; Nakigozi et al., 2013; Nelson et al., 2010; Solorio et al. 2013; Souza et al., 2010). Improved availability and quality of counseling services may help HIV-infected men accept HIV diagnosis and negotiate disclosure. Notably, services must consider privacy, as many participants emphasized concerns about confidentiality at the Reference Center. While several studies have highlighted positive effects of counseling services on continuity of care (Gruber et al., 2011; Leider et al., 2011), these services must be tailored to needs of their community. Notably, all MSM feared disclosure and reported common experiences with HIV-related stigma, discrimination, violence, and homophobia. While Brazil responded progressively to diverse sexualities early in the epidemic, social conservatism has presented new challenges to the country's stance on homosexuality (Corrêa, 2013). Given that MSW also reported fear of disclosure, in addition to MSM's disproportionate representation in Brazil's epidemic (Kerr et al., 2013; Malta et al., 2010), efforts to eliminate HIV-related stigma, discrimination, violence, and homophobia should be redoubled.
Indirect costs associated with transportation and absenteeism at work or school impeded access to retention in care and continued treatment, and these are well-known predictors of poor health outcomes across stages of care in Salvador and elsewhere (Eberhart et al., 2013; Ferreira et al., 2012; Lankowski et al., 2014; Oliveira, 2009; Saha et al., 2014; Trepka et al., 2014). Even in settings where ARVs are free, indirect costs must be addressed to increase care continuity. Transportation vouchers and expanded consultation and pharmacy hours could mitigate these challenges.
Low perceived risk of HIV was a barrier to both HIV diagnosis and linkage to care. While prior studies indicate that men frequently do not perceive themselves at risk for HIV (Filipe et al., 2005; Kerr et al., 2013; Souza et al, 2010), our study connects low perceived risk with later HIV diagnosis and disrupted care. Increased routine testing can facilitate earlier diagnosis by informing individuals of their status regardless of risk perception. Service providers must also ensure newly diagnosed individuals understand consequences of disease progression and interrupted care. Continued research is needed to identify and address factors that delay HIV diagnosis, as many participants underwent testing only upon diagnosis of another medical problem.
Prior research in Brazil and elsewhere links ARV toxicity and complexity with interrupted treatment (Bezabhe et al., 2014; Guimaraes et al., 2008; Melchior et al., 2007; Saha et al., 2014). While HIV is increasingly understood as a chronic disease, continued support for the emotional and physical impact of taking ARVs is needed. Increased access to simplified regimens and combination drugs throughout Brazil may improve adherence and facilitate viral suppression.
This study's primary limitation is that all participants were connected to care, excluding those most disenfranchised. Further, this analysis did not assess clinical status, and the small sample size limited generalizability of findings. Additionally, models of the care cascade are not well defined in national or global guidelines, so assigning barriers to stages is not always straightforward. Nonetheless, this study uniquely assesses barriers to HIV care by contextualizing them along the entire care cascade.
CONCLUSION
This analysis demonstrates that efforts to eliminate more prevalent barriers along the care cascade may improve continued engagement in services by operating at multiple care stages. Research should further explore the relative impact of barriers along one's entire care trajectory, including those limiting HIV diagnosis and affecting vulnerable populations. Diminishing barriers along the care cascade can reduce HIV-related morbidity and mortality in Brazil, and globally, by improving access to life-saving testing, treatment, and care.
ACKNOWLEDGEMENTS
There are no acknowledgements to report.
FUNDING
This work was supported by the Brazilian National Department of STD/AIDS and Viral Hepatitis in the Ministry of Health; the Foundation for Research Support in the State of Bahia; the HIV/AIDS Reference Center of the Bahia Department of Health (CEDAP); the Pathfinder Foundation; the National Institutes of Health under [grants T32 DA12911-12; 1T37MD008655]; the Lifespan/Tufts/Brown Center for AIDS Research [grant P30 AI042853]; the National Institute of Allergy and Infectious Diseases; and the Brazil Community Health Fellows Program of Brown University.
REFERENCES
- Anglaret X, Minga A, Gabillard D, Ouassa T, Messou E, Morris B, Seyler C. AIDS and non-AIDS morbidity and mortality across the spectrum of CD4 cell counts in HIV-infected adults before starting antiretroviral therapy in Cote d'Ivoire. Clinical Infectious Diseases. 2012;54(5):714–723. doi: 10.1093/cid/cir898. doi: 10.1093/cid/cir898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM, Bimirew MA, Kassie DM. Barriers and Facilitators of Adherence to Antiretroviral Drug Therapy and Retention in Care among Adult HIV-Positive Patients: A Qualitative Study from Ethiopia. PLoS One. 2014;9(5):e97353. doi: 10.1371/journal.pone.0097353. doi: 10.1371/journal.pone.0097353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boletim Epidemiológico: HIV/AIDS. Ministry of Health; Brasília, Brazil: 2013. [Google Scholar]
- Bonolo F, Cesar CC, Acurcio FA, Ceccato M, de Padua CA, Alvares J, Guimaraes MD. Non-adherence among patients initiating antiretroviral therapy: a challenge for health professionals in Brazil. AIDS. 2005;19(Suppl 4):S5–13. doi: 10.1097/01.aids.0000191484.84661.2b. [DOI] [PubMed] [Google Scholar]
- Boyatzis R. Transforming qualitative information: Thematic analysis and code development. Sage; Thousand Oaks, CA: 1998. [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Team HS. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrêa S. Francis the First and the politics of sexuality in Latin America. Sexuality Policy Watch. 2013 [Google Scholar]
- Crabtree B, Miller W. A template approach to text analysis: Developing and using codebooks. In: Crabtree B, Miller W, editors. In Doing qualitative research. Sage; Newbury Park, CA: 1999. pp. 163–177. [Google Scholar]
- de Almeida MC, de Jesus Pedroso N, do Socorro L, van Keulen M, Jacome GP, Fernandes GC, Yokoo EM, Tuboi SH. Loss to Follow-Up in a Cohort of HIV-Infected Patients in a Regional Referral Outpatient Clinic in Brazil. AIDS and Behavior. 2014;18(12):2387–96. doi: 10.1007/s10461-014-0812-1. doi: 10.1007/s10461-014-0812-1. [DOI] [PubMed] [Google Scholar]
- Eberhart MG, Yehia BR, Hillier A, Voytek CD, Blank MB, Frank I, Brady KA. Behind the cascade: analyzing spatial patterns along the HIV care continuum. Journal of Acquired Immune Deficiency Syndrome. 2013;64(Suppl 1):S42–51. doi: 10.1097/QAI.0b013e3182a90112. doi: 10.1097/QAI.0b013e3182a90112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira DC, da Silva GA. [Routes to care--the itineraries of people living with HIV]. Ciência & Saúde Coletiva. 2012;17(11):3087–3098. doi: 10.1590/s1413-81232012001100025. [DOI] [PubMed] [Google Scholar]
- Filipe EM, Batistella E, Pine A, Santos NJ, Paiva V, Segurado A, Hearst N. Sexual orientation, use of drugs and risk perception among HIV-positive men in Sao Paulo, Brazil. International Journal of STDs and AIDS. 2005;16(1):56–60. doi: 10.1258/0956462052932764. [DOI] [PubMed] [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical Infectious Diseases. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grangeiro A, Escuder MM, Pereira JC. Late entry into HIV care: lessons from Brazil, 2003 to 2006. BMC Infectious Diseases. 2012;12:99. doi: 10.1186/1471-2334-12-99. doi: 10.1186/1471-2334-12-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber D, Campos P, Dutcher M, Safford L, Phillips K, Craw J, Gardner L. Linking recently diagnosed HIV-positive persons to medical care: perspectives of referring providers. AIDS Care. 2011;23(1):16–24. doi: 10.1080/09540121.2010.498865. doi: 10.1080/09540121.2010.498865. [DOI] [PubMed] [Google Scholar]
- Guimaraes MD, Rocha GM, Campos LN, de Freitas FM, Gualberto FA, Teixeira R, de Castilho FM. Difficulties reported by HIV-infected patients using antiretroviral therapy in Brazil. Clinicas (Sao Paulo) 2008;63(2):165–172. doi: 10.1590/s1807-59322008000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrigan PR, Hogg RS, Dong WW, Yip B, Wynhoven B, Woodward J, Montaner JS. Predictors of HIV drug-resistance mutations in a large antiretroviral-naive cohort initiating triple antiretroviral therapy. Journal of Infectious Diseases. 2005;191(3):339–347. doi: 10.1086/427192. doi: 10.1086/427192. [DOI] [PubMed] [Google Scholar]
- HIV/AIDS Care Continuum 2013 Retrieved from http://aids.gov/federal-resources/policies/care-continuum/
- Hogan CM, Degruttola V, Sun X, Fiscus SA, Del Rio C, Hare CB, Little S. The setpoint study (ACTG A5217): effect of immediate versus deferred antiretroviral therapy on virologic set point in recently HIV-1-infected individuals. Journal of Infectious Diseases. 2012;205(1):87–96. doi: 10.1093/infdis/jir699. doi: 10.1093/infdis/jir699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBGE . Estimativas populacionais para os municípios brasileiros. Brazilian Institute of Geography and Statistics; 2013. Retrieved from http://www.ibge.gov.br/home/estatistica/populacao/estimativa2013/estimativa_dou.shtm. [Google Scholar]
- Kerr LR, Mota RS, Kendall C, Pinho Ade A, Mello MB, Guimaraes MD, Rutherford G. HIV among MSM in a large middle-income country. AIDS. 2013;27(3):427–435. doi: 10.1097/QAD.0b013e32835ad504. doi: 10.1097/QAD.0b013e32835ad504. [DOI] [PubMed] [Google Scholar]
- Lankowski AJ, Siedner MJ, Bangsberg DR, Tsai AC. Impact of Geographic and Transportati.on-Related Barriers on HIV Outcomes in Sub-Saharan Africa: A Systematic Review. AIDS and Behavior. 2014;18(7):1199–223. doi: 10.1007/s10461-014-0729-8. doi: 10.1007/s10461-014-0729-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leider J, Fettig J, Calderon Y. Engaging HIV-positive individuals in specialized care from an urban emergency department. AIDS Patient Care and STDS. 2011;25:89–93. doi: 10.1089/apc.2010.0205. doi: 10.1089/apc.2010.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenc T, Marrero-Guillamon I, Llewellyn A, Aggleton P, Cooper C, Lehmann A, Lindsay C. HIV testing among men who have sex with men (MSM): systematic review of qualitative evidence. Health Education Research. 2011;26(5):834–846. doi: 10.1093/her/cyr064. doi: 10.1093/her/cyr064. [DOI] [PubMed] [Google Scholar]
- Malta M, Magnanini MM, Mello MB, Pascom AR, Linhares Y, Bastos FI. HIV prevalence among female sex workers, drug users and men who have sex with men in Brazil: a systematic review and meta-analysis. BMC Public Health. 2010;10:317. doi: 10.1186/1471-2458-10-317. doi: 10.1186/1471-2458-10-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior R, Nemes MI, Alencar TM, Buchalla CM. [Challenges of treatment adherence by people living with HIV/AIDS in Brazil]. Revista de Saúde Pública. 2007;41(Suppl 2):87–93. doi: 10.1590/s0034-89102007000900014. [DOI] [PubMed] [Google Scholar]
- Melchior R, Nemes MI, Basso CR, Castanheira ER, Alves MT, Buchalla CM, Donini AA. [Evaluation of the organizational structure of HIV/AIDS outpatient care in Brazil]. Revista de Saúde Pública. 2006;40(1):143–151. doi: 10.1590/s0034-89102006000100022. [DOI] [PubMed] [Google Scholar]
- Meyerson B, Barnes P, Emetu R, Bailey M, Ohmit A, Gillespie A. Institutional and structural barriers to HIV testing: elements for a theoretical framework. AIDS Patient Care and STDS. 2014;28(1):22–27. doi: 10.1089/apc.2013.0238. doi: 10.1089/apc.2013.0238. [DOI] [PubMed] [Google Scholar]
- Mukolo A, Villegas R, Aliyu M, Wallston KA. Predictors of late presentation for HIV diagnosis: a literature review and suggested way forward. AIDS and Behavior. 2013;17(1):5–30. doi: 10.1007/s10461-011-0097-6. doi: 10.1007/s10461-011-0097-6. [DOI] [PubMed] [Google Scholar]
- Nakigozi G, Atuyambe L, Kamya M, Makumbi FE, Chang LW, Nakyanjo N, Gray R. A qualitative study of barriers to enrollment into free HIV care: perspectives of never-in-care HIV-positive patients and providers in Rakai, Uganda. BioMed Research International. 2013;2013:470245. doi: 10.1155/2013/470245. doi: 10.1155/2013/470245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson KM, Thiede H, Hawes SE, Golden MR, Hutcheson R, Carey JW, Jenkins RA. Why the wait? Delayed HIV diagnosis among men who have sex with men. Journal of Urban Health. 2010;87(4):642–655. doi: 10.1007/s11524-010-9434-8. doi: 10.1007/s11524-010-9434-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemes MI, Alencar TM, Basso CR, Castanheira ER, Melchior R, Alves MT, Santos MA. Assessment of outpatient services for AIDS patients, Brazil: comparative study 2001/2007. Revista de Saúde Pública. 2013;47(1):137–146. doi: 10.1590/s0034-89102013000100018. [DOI] [PubMed] [Google Scholar]
- Oliveira IB. [Universal access? Obstacles to access, continuity of treatment, and gender issues at a specialized HIV/AIDS clinic in Salvador, Bahia State, Brazil]. Cadernos de Saúde Pública. 2009;25(Suppl 2):S259–268. doi: 10.1590/s0102-311x2009001400008. [DOI] [PubMed] [Google Scholar]
- Protocolo Clínico e Diretrizes Terapêuticas para Manejo da Infecção pelo HIV em Adultos. Ministry of Health; Brasília, Brazil: p. 2013. [Google Scholar]
- Ribeiro FA, Tupinambas U, Fonseca MO, Greco DB. Durability of the first combined antiretroviral regimen in patients with AIDS at a reference center in Belo Horizonte, Brazil, from 1996 to 2005. Brazilian Journal of Infectious Diseases. 2012;16(1):27–33. [PubMed] [Google Scholar]
- Saha R, Saha I, Sarkar AP, Das DK, Misra R, Bhattacharya K, Bhattacharya A. Adherence to highly active antiretroviral therapy in a tertiary care hospital in West Bengal, India. Singapore Medical Journal. 2014;55(2):92–98. doi: 10.11622/smedj.2014021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster MA, Collins R, Cunningham WE, Morton SC, Zierler S, Wong M, Kanouse DE. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. Journal of General Internal Medicine. 2005;20(9):807–813. doi: 10.1111/j.1525-1497.2005.05049.x. doi: 10.1111/j.1525-1497.2005.05049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solorio R, Forehand M, Simoni J. Attitudes towards and Beliefs about HIV Testing among Latino Immigrant MSM: A Comparison of Testers and Nontesters. AIDS Research and Treatment. 2013;2013:563537. doi: 10.1155/2013/563537. doi: 10.1155/2013/563537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza Junior PR, Szwarcwald CL, Castilho EA. Self-rated health by HIV-infected individuals undergoing antiretroviral therapy in Brazil. Cadernos de Saúde Pública. 2011;27(Suppl 1):S56–66. doi: 10.1590/s0102-311x2011001300007. [DOI] [PubMed] [Google Scholar]
- Souza Vde S, Czeresnia D. Demands and expectations of users of HIV testing and counseling centers. Revista de Saúde Pública. 2010;44(3):441–447. doi: 10.1590/s0034-89102010005000010. [DOI] [PubMed] [Google Scholar]
- Trepka MJ, Fennie KP, Sheehan DM, Lutfi K, Maddox L, Lieb S. Late HIV diagnosis: Differences by rural/urban residence, Florida, 2007-2011. AIDS Patient Care and STDS. 2014;28(4):188–197. doi: 10.1089/apc.2013.0362. doi: 10.1089/apc.2013.0362. [DOI] [PMC free article] [PubMed] [Google Scholar]