Abstract
Objective
To document how long-acting reversible contraception (LARC) affects women’s sexual outcomes.
Methods
In this prospective, observational cohort study, we enrolled new-start intrauterine device (IUD) and contraceptive implant users attending four family planning clinics. Data collection occurred at baseline, one month, and three months. Primary outcomes were the Female Sexual Function Index, New Sexual Satisfaction Scale, and perceived sexual effects of method (positive, negative, or none). Secondary outcomes included other factors associated with LARC’s sexual acceptability, including the ability to “let go” in sex, sense of control over pregnancy, and bleeding changes. Chi-square and F-tests assessed differences between method groups at baseline, and mixed effects models, robust Wald chi-square tests, and conditional logistic regression documented differences from baseline and trends over time.
Results
In December 2014-April 2015, 200 patients consented and enrolled in the study. Among 159 women who completed three survey rounds, 20% selected copper IUDs, 46% levonorgestrel IUDs, and 34% implants. Sexual functioning and satisfaction scores did not change over time. However, across methods, participants were more likely to report improvements to their sexual lives compared to baseline (χ2 p<0.001). By 3 months, 40% (n=64) reported positive changes and 17% (n=27) negative changes. Positive sexual changes were associated with one’s sense of control over pregnancy and one’s ability to “let go” in sex. Negative sexual changes were largely attributable to increased vaginal bleeding.
Conclusion
Although new LARC users reported no measurable objective change in sexual function or satisfaction, a sizable minority reported perceived positive, method-related sexual changes.
Clinical Trial Registration
ClinicalTrials.gov, www.clinicaltrials.gov, NCT02734199.
Introduction
Contraceptive researchers and practitioners rarely assess sexual acceptability, or how contraception affects women’s sexual experiences.1–3 Research on male-based contraceptives4–6 demonstrates that sexual acceptability influences men’s uptake and use of these methods. Building evidence suggests sexual acceptability shapes women’s contraceptive practices as well.7–10 However, more studies are needed—especially for long-acting reversible contraception (LARC), the most effective contraceptive methods currently available.11, 12
Two major measurement gaps hinder the research to date. First, most studies are cross-sectional,13 preventing evaluation of sexual experiences over time.14 Second, most extant research takes a solely physiologic approach to sexual acceptability, primarily through sexual libido13, 14 or the Female Sexual Function Index.15 However, sexual acceptability includes other key domains, including psychological factors such as sexual disinhibition, sexual aspects of side effects such as bleeding and cramping, and women’s perceptions of whether their methods affect sexuality.7, 9, 16, 17
A 2014 review examined 11 LARC studies that included sexuality measures.18 Use of the intrauterine device (IUD) was more commonly associated with positive or neutral sexual effects than negative ones; however, the review identified mixed results, a lack of US studies, and potential methodological limitations. A 2016 US study found copper IUD users significantly less likely than Depot Medroxyprogesterone Acetate (DMPA) users to report lack of sexual desire in the last six months;13 however, it did not include baseline sexuality measures, which could have impacted study results. This prospective study addresses these gaps by documenting sexual acceptability using a variety of sexuality measures among women initiating a LARC method.
Materials and Methods
In this prospective, observational cohort study, participants were 18–44 year-old women seeking contraceptive services at one of four Planned Parenthood Association of Utah clinics from December 2014 to April 2015. The study was reviewed and approved by University of Utah’s Institutional Review Board. Per standard care protocols, patients received shared-decision-making counseling from a clinic staff member and then selected the contraceptive method of their choice. All patients who selected a currently-available LARC method (copper IUD, levonorgestrel IUD, or contraceptive implant) were informed by the counselor of the current study on sexuality and contraception. Study eligibility included a desire to prevent pregnancy for at least one year, fluency in English or Spanish, and a working phone number. Women who were sterilized, pregnant, or trying to get pregnant were ineligible. If eligible and willing to participate, patients provided informed consent and enrolled in the study during the same clinic visit. Participants received their devices free of charge, which they were informed about following contraceptive counseling and prior to completing the informed consent process.
Initial data collection took place prior to device insertion via use of the Research Electronic Data Capture (REDCap), a secure, web-based, research application. (Please see supplemental, online Appendix 1, available online at http://links.lww.com/xxx for the clinic intake form.) At one and three months, post-device-placement participants were prompted by their preferred method of communication (phone, text or email) to complete REDCap follow-up questionnaires. Surveys took approximately 15 minutes, and respondents received a small amount gift card credit for each completed round.
Baseline surveys collected information on variables that can influence both contraceptive choice and sexual outcomes and would later serve as control variables: sociodemographic information, obstetric history, relationship status and length, and health status (as captured by the WHO-5,19 a 5-item measure of functional health and well-being). Women were also asked, “How important are each of the following characteristics to you when you decide which birth control method to use?” Based on qualitative7, 17 and theoretical research,20 we included two sexual acceptability criteria (“it doesn’t reduce my libido” and “it doesn’t interrupt sex”) alongside the other more common criteria21 such as efficacy, hormonal content, and friend recommendation.
Our primary objective was to assess sexual outcomes among new LARC users over time while controlling for relevant baseline factors. Three measures contributing to the primary outcome were as follows: 1) the Female Sexual Function Index-6,22 a validated, 6-question measure including items on sexual desire/interest, arousal, lubrication, orgasm, pain, and satisfaction, 2) the New Sexual Satisfaction Scale23 a validated, 20-question measure with some functioning items but additional sexual domains such as partner-oriented items and the ability to “let go” during sex, and 3) a question devised and piloted by the research team about participants’ perceptions of their contraceptive method’s sexual effects, if any (“In the last 4 weeks, would you say your contraceptive method: made my sex life better, made it worse, or had no effect on my sex life?”).
Our secondary objective was to assess other sexual factors potentially involved in the sexual acceptability of these contraceptive methods, including the sexual-related selection criteria measures mentioned above. Other secondary sexual measures were based on recent qualitative research on the sexual acceptability of IUDs in the US.17 The potential sexual impacts of bleeding changes were captured with a question about vaginal bleeding in the last 4 weeks (no bleeding, less bleeding than before the device, no change, more bleeding). To capture the potential sexual impacts of sexual disinhibition by way of feeling extremely protected against pregnancy, we used two questions: 1) the “surrender” question of the New Sexual Satisfaction Scale, in which women ranked their satisfaction with their “ability to let go and ‘surrender’ to sexual pleasure during sex,” and 2) women’s responses (from strongly disagree to strongly agree) to an item phrased “I feel I have control over whether I get pregnant.”
All analyses were conducted with SAS software version 9.4.24 Descriptive statistics came from means (standard deviations) and percentages. F-tests (for continuous variables) and Pearson chi-square tests (for categorical variables) compared baseline characteristics across contraceptive groups. To assess trends in sexual outcomes over time, mixed-effects models were fit for continuous outcomes with time trend, random intercept, and random slope across time—separately for each contraceptive method and then with all the method groups combined. Interaction effects between contraceptive methods and time trend tested whether methods differed in their effect. Perceived impact of contraceptive method on sex life over time was compared across time points via robust Wald chi-square tests and conditional logistic regression. Models were fit both with and without adjustment for self-reported health, as a time-varying factor. Finally, we performed overall chi-square tests to document associations between perceived sexual changes (grouped as better, unchanged, and worse) and both vaginal bleeding and sexual disinhibition (i.e., the “surrender” question and the control-over-pregnancy question).
The primary aim of this study was to assess three sexual outcome measures in three groups of LARC users. However, given its prominence in the sexual acceptability literature, we based the sample size calculation on the Female Sexual Function Index (FSFI) and informed this with the method mix from historical data at the participating sites (12% implant, 60% levonorgestrel IUD, and 28% copper T IUD). Based on prior research, we assumed baseline average FSFI total scores of 31 (standard deviation = 5).25 We assumed the implant would lead to no change in FSFI and both IUDs would lead to a 5 unit improvement in FSFI total score over three months. With 125 subjects, we were powered at 90% at 5% significance to compare changes over time in total FSFI score between the three method groups—the equivalent of an effect size of 0.33. With an anticipated retention rate of 83%, we planned to recruit 150 subjects (18 implant, 90 levonorgestrel IUD, and 48 copper T IUD).”
Results
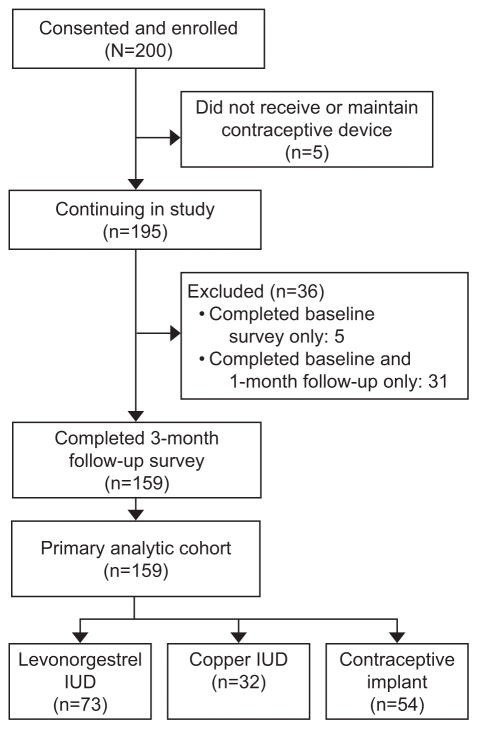
A total of 195 women consented to participate in the study and had successful insertions. Out of 195 enrollees, 159 original study participants (32 copper IUD users, 73 levonorgestrel users, and 54 contraceptive implant users) completed the three-month follow-up, indicating a retention rate of 82% (Figure 1). In the month prior to study enrollment, participants had used the following methods, either by themselves or in conjunction with other methods (not shown): 45% condoms (n=86 for male condoms, n=1 for female condom), 28% withdrawal (n=54), 19% oral contraceptives (n=36), 12% no method, 10% 3-month injection (n=20), 7% emergency contraception (n=14), 4% vaginal ring (n=8), 2% contraceptive patch (n=4), 3% fertility awareness methods (n=5), 1% spermicide (n=2), and 1% copper IUD.
Figure 1.
Participant Flow Diagram
Table 1 displays baseline characteristics of participants, by method selected. Participants had a mean age of 27 years, the majority were unmarried (80%, n=120) and had at least some college or vocational training (64%, n=97), and one-third were women of color (23% [n=35] Hispanic non-white and 10% [n=15] non-Hispanic other). There were few significant socio-demographic differences between method groups save for age, with contraceptive implant users were slightly younger in years.
Table 1.
Participant Characteristics and Criteria for Choosing a New Contraceptive Method Selected by New–Start Contraceptive Users at Baseline, by Method
| Characteristics/Criteria | Total n(%)* | Copper IUD n(%) | LNG IUD n(%) | Implant n(%) | P-value† |
|---|---|---|---|---|---|
| Method chosen at baseline | 159(100) | 32(20.1) | 73(45.9) | 54(34.0) | |
| Age in years, mean ± SD | 26.9 ± 6.1 | 27.0 ± 6.03 | 28.1 ± 6.09 | 25.1 ± 5.82 | 0.021 |
| Highest level of education completed | 0.428 | ||||
| 11th grade or less | 5(3.3) | 6(3.3) | 1(1.5) | 3(5.8) | |
| 12th grade (completed high school or GED) | 49(32.5) | 9(30.0) | 20(29.0) | 20(38.5) | |
| Vocational/technical training | 17 (11.3) | 3(10.0) | 11(15.9) | 3(5.8) | |
| Associate degree or some college | 55(36.4) | 11(36.7) | 23(33.3) | 21(40.4) | |
| College graduate or higher | 25(16.6) | 6(20.0) | 14(20.3) | 5(9.6) | |
| Race/ethnicity | 0.078 | ||||
| Non-Hispanic white | 102(67.1) | 17(56).7 | 54(78.3) | 31(58.5) | |
| Hispanic non-white | 35(23.0) | 10(33.3) | 11(15.9) | 14(26.4) | |
| Non-Hispanic other | 15(9.9) | 3(10.0) | 4(5.8) | 8(15.1) | |
| Current employment/student status | 0.717 | ||||
| Unemployed | 33(20.8) | 6(18.8) | 14(19.2) | 13(24.1) | |
| Working full time | 80(50.3) | 17(53.1) | 36(49.3) | 27(50.0) | |
| Working part time | 30(18.9) | 4(12.5) | 15(20.6) | 11(20.4) | |
| Disabled or sick leave | 13(8.2) | 3(9.4) | 7(9.6) | 3(5.6) | |
| Retired | 3(1.9) | 2(6.3) | 1(1.4) | 0(0.0) | |
| Annual household income | 0.090 | ||||
| <$10,000 | 30(19.7) | 5(16.7) | 13(18.8) | 12(22.6) | |
| $10,000–$29,999 | 76(50.0) | 14(46.7) | 42(60.9) | 20(37.7) | |
| ≥$30,000 | 46(30.3) | 11(36.7) | 14(20.3) | 21(39.6) | |
| Relationship characteristics | |||||
| Less than 3 months | 29(21.6) | 6(21.4) | 14(22.6) | 9(20.5) | 0.319 |
| 3 months to 1 year | 40(29.9) | 12(42.9) | 14(22.6) | 14(31.8) | |
| 1–3 years | 31(23.1) | 5(17.9) | 13(21.0) | 13(29.6) | |
| More than 3 years | 34(25.4) | 5(17.9) | 21(33.9) | 8(18.2) | |
| Marital status | 0.721 | ||||
| Never married, not living with partner | 79(52.3) | 12(41.4) | 35(50.7) | 32(60.4) | |
| Cohabiting | 20(13.3) | 4(13.8) | 10 (14.5) | 6(11.3) | |
| Married | 31(20.5) | 7(24.1) | 14(20.3) | 10((18.9) | |
| Separated, divorced, or widowed | 21(13.9) | 6(20.7) | 10 (14.5) | 5(9.4) | |
| Reasons for choosing a new birth control method | |||||
| It's the most effective method | 0.712 | ||||
| Not at all important | 4(2.7) | 1(3.5) | 1(1.5) | 2(3.9) | |
| Slightly or quite important | 31(21.1) | 4(13.8) | 15(22.4) | 12(23.5) | |
| Extremely important | 112(76.2) | 24(82.8) | 51(76.1) | 37(72.6) | |
| It doesn't reduce my libido | |||||
| Not at all important | 9(6.4) | 0(0.0) | 4(6.1) | 5(10.4) | 0.554 |
| Slightly or quite important | 23(16.3) | 5(18.5) | 10(15.2) | 8(16.7) | |
| Extremely important | 109(77.3) | 22(81.5) | 52(78.8) | 35(72.9) | |
| It doesn't interrupt sex | 0.730 | ||||
| Not at all important | 6(4.0) | 0(0.0) | 4(5.9) | 2(3.9) | |
| Slightly or quite important | 34(22.8) | 7(24.1) | 17(25.0) | 10(19.2) | |
| Extremely important | 109(73.2) | 22(75.9) | 47(69.1) | 40(76.9) | |
| It is acceptable to my partner | 0.264 | ||||
| Not at all important | 36(24.3) | 6(21.4) | 14(20.6) | 16(30.8) | |
| Slightly or quite important | 55(37.2) | 7(25.0) | 28(41.2) | 20(38.5) | |
| Extremely important | 57(38.5) | 15(53.6) | 26(38.2) | 16(30.8) | |
| It doesn't contain hormones | 0.000 | ||||
| Not at all important | 39(29.1) | 2(6.9) | 20(32.3) | 17(39.5) | |
| Slightly or quite important | 60(44.8) | 6(20.7) | 32(51.6) | 22(51.2) | |
| Extremely important | 35(26.1) | 21(72.4) | 10(16.1) | 4(9.3) | |
| It's recommended by my friends | 0.251 | ||||
| Not at all important | 62(41.9) | 9(30.0) | 29(43.3) | 24(47.1) | |
| Slightly or quite important | 75(50.7) | 16(53.3) | 34(50.8) | 25(49.0) | |
| Extremely important | 11(7.4) | 5(16.7) | 4(6.0) | 2(3.9) | |
| It's in line with my religious beliefs | 0.022 | ||||
| Not at all important | 115(82.7) | 22(84.6) | 53(84.1) | 40(80.0) | |
| Slightly or quite important | 17(12.2) | 0(0.0) | 8(12.7) | 9(18.0) | |
| Extremely important | 7(5.0) | 4(15.4) | 2(3.2) | 1(2.0) |
Totals vary between 134 and 159 due to missing data items
P–values are for null hypothesis of no difference in percentage distribution (tested via Fisher’s exact test) or means (tested via F–test) between contraceptive methods groups
Table 1 also features information on method selection criteria. Over three-quarters (76%, n=112) of women said method effectiveness is extremely important to them in choosing a method; just as many said it was extremely important that a method doesn’t reduce libido (77%, n=109) and doesn’t interrupt sex (73%, n=109). There were no significant differences across method groups. There were few differences in selection criteria by method group—although, as expected, women who selected the copper IUD were significantly more likely than the other two groups to say that “lack of hormones” was extremely important.
Table 2 shows the three primary sexuality measures by both method type and time period. Neither overall Female Sexual Function Index scores nor New Sexual Satisfaction Scale scores differed significantly between each of the three LARC groups at any time or between time periods. However, participants were significantly more likely to report perceived improvements to their sexual lives as a result of their contraceptive method (χ2 p<0.000). For example, at one month, 38% of women (n=60) indicated their new method had improved their sex life in the last four weeks, compared to 15% (n=24) reporting their method had made their sex life worse. By three months, 40% (n=64) of women reported positive changes and 17% (n=27) reported negative changes. Sexual outcomes showed few differences across the method groups.
Table 2.
Sexual Outcomes by Method Group, Across Time
| BASELINE | ONE MONTH | THREE MONTHS | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sexual Outcome | copper IUD | LNG IUD | implant | all | copper IUD | LNG IUD | implant | all | copper IUD | LNG IUD | implant | all | P |
| Female Sexual Function Index (FSFI– 6) score [mean ± standard deviation] | 23.6±6.74 | 22.5±6.22 | 21.8 ± 8.31 | 22.5±7.09 | 21.5±6.33 | 22.8±7.46 | 21.4 ± 8.74 | 22.1±7.70 | 22.1±6.99 | 22.5±7.61 | 21.0±8.98 | 21.9±7.97 | 0.39* |
| New Sexual Satisfaction Scale (NSSS) score [mean ± standard deviation] | 34.1±10.7 | 32.4±11.6 | 31.8±12.2 | 32.5±11.6 | 32.9±10.1 | 32.5±12.7 | 31.0±11.5 | 32.1±11.8 | 33.0±11.5 | 32.2±12.7 | 31.7±12.0 | 32.2±12.2 | 0.51* |
| Subjective item: In the past 4 weeks, would you say your contraceptive method has… [n(%)] | 0.000† | ||||||||||||
| worsened my sex life | 13(43.3) | 20(29.0) | 9(17.0) | 42(27.6) | 7(21.9) | 11(15.1) | 6(11.10) | 24(15.1) | 7(21.9) | 11(15.1) | 9(16.70) | 27(17.0) | |
| had no effect on my sex life | 12(40.0) | 37(53.6) | 37(69.8) | 86(56.6) | 12(37.5) | 32(43.8) | 31(57.4) | 75(47.2) | 9(28.1) | 33(45.2) | 26(48.2) | 68(42.8) | |
| improved my sex life | 5(16.7) | 12(17.4) | 7(13.2) | 24(15.8) | 13(40.6) | 30(41.1) | 17(31.5) | 60(37.7) | 16(50.0) | 29(39.7) | 19(35.2) | 64(40.3) | |
P–value for time trend (regression slope) in overall percentages across time points tested by F–test in mixed effects model for continuous outcomes, and by robust Wald chi–square test from generalized estimating equation for ordinal outcome. This time trend across accounts for within–individual correlation across time.
P–value for robust Wald chi–square (χ2) test for time trend (cumulative logit regression slope).
The significance of women’s perceived sexual improvements due to contraceptive method remained even after adjusting for all differences between individuals via conditional logistic regression (not shown in tables). This method compares individuals with themselves at different time points with respect to perceived impact of contraceptive method on sex life. Women remained significantly more likely to report positive changes at both one and three months, with odds ratios of 4.64 [95%CI: 2.38–9.92] and 5.61 [95%CI: 2.83–10.0] respectively.
To help explain reports of positive versus negative method-related sexual changes, we performed chi-square tests between the measure of perceived sexual changes and the three secondary sexual outcomes: reports of vaginal bleeding changes, the surrender question of the New Sexual Satisfaction Scale, and the control-over-pregnancy variable (Table 3). Since there were few significant differences in sexuality outcomes by method, and to simplify data presentation, we combined the three contraceptive method groups into one for these analyses. All three variables were significantly associated with women’s perceived sexual changes. For example, at one month, among those women who reported their method had made their sex life worse, the overwhelming majority (88%, n=21) reported increased vaginal bleeding, compared to only 38% (n=23) of women reporting sexual improvements. In terms of sexual surrender, women reporting negative sexual changes due to their method in the last month were significantly less likely to be satisfied with their ability to “let go” during sex. Finally, among women reporting positive sexual changes, a greater proportion reported the highest levels of perceived control over pregnancy.
Table 3.
Associations between Perceived Sexual Changes Due to Method (Better, Unchanged, Worse) and Vaginal Bleeding, Sexual Surrender/Disinhibition, and Control over Pregnancy, by Time*
| ONE MONTH | THREE MONTHS | |||||||
|---|---|---|---|---|---|---|---|---|
| Covariates | sexual improvements | no sexual change | sexual detractions | p value† | sexual improvements | no sexual change | sexual detractions | p– value† |
| N‡ | 60 | 75 | 24 | 64 | 68 | 27 | ||
| Vaginal bleeding in the last 4 weeks (n(%)) | 0.004† | 0.000† | ||||||
| no vaginal bleeding | 11(18.3) | 13(17.3) | 0(0.0) | 0.000§ | 18(28.1) | 18(26.5) | 3(11.1) | 0.000§ |
| less bleeding than before device | 20(33.3) | 16(21.3) | 2(8.3) | 24(37.5) | 18(26.5) | 1(3.7) | ||
| no change in bleeding | 6(10.0) | 5(6.7) | 1(4.2) | 5(7.8) | 3(4.4) | 3(11.1) | ||
| more bleeding than before device | 23(38.3) | 41(54.7) | 21(87.5) | 17(26.6) | 29(42.7) | 20(74.1) | ||
| Satisfaction with your ability to "let go" and surrender to sexual pleasure in the last 4 weeks (n(%)) | ||||||||
| 0.014† | 0.000† | |||||||
| very/extremely satisfied | 44(73.3) | 33(47.1) | 10(41.7) | 0.002§ | 46(71.9) | 34(53.2) | 7(28.0) | 0.000§ |
| moderately satisfied | 9(15.0) | 18(25.7) | 6(25.0) | 12(18.8) | 13(20.3) | 7(28.0) | ||
| not at all/a little satisfied | 7(11.7) | 19(27.1) | 8(33.3) | 6(9.4) | 17(26.6) | 11(44.0) | ||
| "I feel like I have control over when I get pregnant"‡ (n(%)) | ||||||||
| 0.131† | 0.079†§ | |||||||
| strongly agree | 50(83.3) | 49(65.3) | 15(62.5) | 0.040§ | 50(78.1) | 50(73.5) | 16(59.3) | 0.014§ |
| somewhat agree | 6(10.0) | 16(21.3) | 6(25.0) | 12(18.8) | 13(19.1) | 5(18.5) | ||
| neither agree nor disagree, | 4(6.7) | 10(13.3) | 3(12.5) | 2(3.1) | 5(7.4) | 6(22.2) | ||
| somewhat disagree, and strongly disagree (combined) | ||||||||
Here, all method groups (copper IUDs, levonorgestrel IUDs, implants) are combined. Results represent cross–sectional associations between perceived sexual changes and other sexual covariates between at one time period (1 month, 3 months).
P values are from Fisher’s exact test of null hypothesis that percentage distributions are equal in all sexual change groups.
Sample sizes in cross–tabulations vary between 153 and 159 due to missing data items.
P values are from Mantel–Haenszel chi–square test of correlation between sexual change and ratings on the three variables.
Discussion
This study assessed 159 US women’s sexual experiences with IUDs and contraceptive implants while controlling for baseline sexuality factors. The overwhelming majority reported either no sexual changes or positive sexual changes after using a LARC method for three months. These findings align with European and Middle Eastern research showing sexual improvements in some women using IUDs.18, 26–29 Although participants in the current study did not report significant changes in sexual functioning or satisfaction, over half reported perceived sexual changes due to their method. Those few women who reported negative sexual changes were significantly more likely to have experienced increased vaginal bleeding.
Findings from this study expand how we define and measure the concept of contraception’s sexual acceptability.20 The few contraceptive studies that have included any sexual measures tend to either use the Female Sexual Function Index15 or a single sexual functioning measure such as lack of interest in sex.13 However, such functioning measures were not designed for young, healthy, contraception-seeking women. They may also miss sexual domains such as psychological factors, subjective perceptions, or sexual aspects of bleeding and cramping.17, 20 In our study, sexual functioning and satisfaction did not change significantly with LARC use, while women’s perceptions of their method’s sexual effects did. Such perceptions are likely to influence contraceptive continuation. Moreover, we documented correlates of these perceived sexual improvements. For example, sexual improvements were strongly associated with the ability to “let go” in sex and one’s sense of control over pregnancy prevention, suggesting that many women may be able to enjoy sexual activity more when the threat of pregnancy is reduced—a finding that corroborates qualitative research on the sexual acceptability of IUDs in the US.17
A final important finding is that sexual-related criteria may influence women’s selection of new contraceptive methods more than previously examined. Proportionally as many participants in this study valued efficacy as they did methods that neither reduce libido nor interrupt sex. These findings align with recent research by Gomez and Clark,21 who found that the most frequently selected contraceptive feature by potential IUD users was “does not interfere with the pleasure of sex”–thereby trumping features such as effectiveness. Sexual criteria should be better integrated into contraceptive counseling protocols and decision support tools.
Findings should be interpreted in light of study limitations. First and foremost, our study included LARC methods only and no control group. We therefore cannot determine if LARC users are sexually or psychologically different compared to women who select hormonal methods or barrier methods, nor if LARC users have better sexual outcomes. Future studies should include a broader array of contraceptive methods, including condom-only users or another type of non-hormonal comparison group.
Secondary limitation are as follows. Our sexual measure regarding perceived sexual changes due to method only had three possible response categories (no change, better, or worse); a greater number of responses or a continuous scale may have picked up more nuance. Participants may have been using contraceptive method(s) in the month before the study that could have affected their sexual measures at baseline and over the course of the study. However, we used the study methodology described here due to its practicality and feasibility; moreover, a group of participants who have used no contraceptive method(s) in the month before the study would be sexually select compared to a more average contraceptive-seeking population. In addition, the clinical setting of this study offered a realistic versus a laboratory environment, but one cost of this setting was the inability to collect data on all eligible participants who declined enrollment. Finally, since clinical assistants highlighted the sexual aspects of the study when enrolling potential participants, our sample may be select–that is, they may represent patients who care more about sexuality than the average contraceptive user. On the other hand, we argue that sexuality is of interest to most if not all women seeking contraception–a finding upheld in other studies.21
Study findings suggest at least two clinical implications. First, practitioners may wish to reassure patients that they are unlikely to experience declines in sexual function or satisfaction as a result of their LARC method. Moreover, they may wish to inform contraceptive users about the potentially sexual-enhancing aspects of LARC methods–that is, that a greater proportion of LARC users will perceive positive versus negative sexual effects due to their method, and the overwhelming majority will experience either no sexual change or a positive sexual change. This information may improve LARC method uptake and satisfaction with potential positive public health benefits. Second, patients deserve upfront education and reassurances about the management of increased bleeding and cramping. The few women in this study reporting negative sexual changes were also likely to report increased vaginal bleeding—an effect that will typically improve for levonorgestrel IUD users and may be ameliorated for copper IUD users and contraceptive implant users.30
Supplementary Material
Acknowledgments
The authors thank the clinic staff at the four recruiting family planning clinics for their critical work in making the study a success, and Renee Kramer for her editorial assistance.
Supported by a grant from the Society of Family Planning (SFPRF7-21). Jenny A. Higgins also acknowledges support from an NIH K12 award (K12 HD055894) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and a NICHD Population Research Infrastructure grant (P2C HD047873). Study data were collected and managed using REDCap (Research Electronic Data Capture) hosted at the University of Utah; this service is supported by Center for Clinical and Translational Sciences grant 8UL1TR000105 (formerly UL1RR025764, NCATS/NIH).
Footnotes
Presented at the Society of Family Planning’s annual North American Forum on Family Planning, November 11-16, 2015, Chicago, Illinois.
Financial Disclosure:
David K. Turok receives speaking honoraria from Allergan and Medicines360; is a consultant for Bioceptive; and serves on advisory boards for Actavis, Bayer, Pharmanest and Teva. The Department of Obstetrics and Gynecology, University of Utah, receives research funding from Bayer, Bioceptive, Contramed, Medicines360, Merck, and Teva. The other authors did not report any potential conflicts of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations.
Contributor Information
Jenny A. Higgins, University of Wisconsin, Madison, Wisconsin.
Jessica N. Sanders, University of Utah, Salt Lake City, Utah.
Mari Palta, University of Wisconsin, Madison Wisconsin.
David K. Turok, University of Utah, Salt Lake City, Utah.
References
- 1.Philpott A, Knerr W, Maher D. Promoting protection and pleasure: amplifying the effectiveness of barriers against sexually transmitted infections and pregnancy. Lancet. 2006;368:2028–31. doi: 10.1016/S0140-6736(06)69810-3. [DOI] [PubMed] [Google Scholar]
- 2.Higgins JA, Hirsch JS. The pleasure deficit: revisiting the "sexuality connection" in reproductive health. Perspectives on sexual and reproductive health. 2007;39:240–7. doi: 10.1363/3924007. [DOI] [PubMed] [Google Scholar]
- 3.Severy LJ, Newcomer S. Critical issues in contraceptive and STI acceptability research. Journal of Social Issues. 2005;61:45–65. [Google Scholar]
- 4.Hensel DJ, Stupiansky NW, Herbenick D, Dodge B, Reece M. Sexual pleasure during condom-protected vaginal sex among heterosexual men. The journal of sexual medicine. 2012;9:1272–6. doi: 10.1111/j.1743-6109.2012.02700.x. [DOI] [PubMed] [Google Scholar]
- 5.Randolph ME, Pinkerton SD, Bogart LM, Cecil H, Abramson PR. Sexual pleasure and condom use. Archives of sexual behavior. 2007;36:844–8. doi: 10.1007/S10508-007-9213-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. Hormonal contraception for men: acceptability and effects on sexuality. World Health Organization Task Force on Psychosocial Research in Family Planning, Special Programme of Research, Development and Research Training in Human Reproduction Studies in family planning. 1982;13:328–42. [PubMed] [Google Scholar]
- 7.Higgins JA, Hirsch JS. Pleasure and power: Incorporating sexuality and inequality into research on contraceptive use and unintended pregnancy. Am J Public Health. 2008;98:1803–13. doi: 10.2105/AJPH.2007.115790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith NK, Jozkowski KN, Sanders SA. Hormonal contraception and female pain, orgasm and sexual pleasure. Journal of sexual medicine. 2013;11:462–70. doi: 10.1111/jsm.12409. [DOI] [PubMed] [Google Scholar]
- 9.Higgins JA, Davis AR. Contraceptive sex acceptability: a commentary, synopsis and agenda for future research. Contraception. 2014;90:4–10. doi: 10.1016/j.contraception.2014.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanders SA, Graham CA, Bass JL, Bancroft J. A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception. 2001;64:51–8. doi: 10.1016/s0010-7824(01)00218-9. [DOI] [PubMed] [Google Scholar]
- 11.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniels K, Daugherty J, Jones J. Current contraceptive status among women aged 15–44: United States, 2011–2013. Hyattsville, MD: National Council for Health Statistics; 2014. Dec, [Google Scholar]
- 13.Boozalis A, Tutlam NT, Chrisman Robbins C, Peipert JF. Sexual Desire and Hormonal Contraception. Obstetrics and gynecology. 2016;127:563–72. doi: 10.1097/AOG.0000000000001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis AR, Castano PM. Oral contraceptives and libido in women. Annual review of sex research. 2004;15:297–320. [PubMed] [Google Scholar]
- 15.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of sex and marital therapy. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JA, Hoffman S, Graham CA, Sanders SA. Relationships between condoms, hormonal methods, and sexual pleasure and satisfaction: an exploratory analysis from the Women's Well-Being and Sexuality Study. Sexual health. 2008;5:321–30. doi: 10.1071/sh08021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JA, Ryder K, Skarda G, Koepsel E, Bennett EA. The sexual acceptability of intrauterine contraception: a qualitative study of young adult women. Perspectives on sexual and reproductive health. 2015;47:115–22. doi: 10.1363/47e4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanders JN, Smith NK, Higgins JA. The intimate link: a systematic review of highly effective reversible contraception and women's sexual experience. Clinical obstetrics and gynecology. 2014;57:777–89. doi: 10.1097/GRF.0000000000000058. [DOI] [PubMed] [Google Scholar]
- 19.Primack BA. The WHO-5 Wellbeing Index performed the best in screening for depression in primary care. ACP journal club. 2003;139:48. [PubMed] [Google Scholar]
- 20.Higgins JA, Smith NK. The Sexual Acceptability of Contraception: Reviewing the Literature and Building a New Concept. Journal of sex research. 2016:1–40. doi: 10.1080/00224499.2015.1134425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gomez AM, Clark JB. The relationship between contraceptive features preferred by young women and interest in IUDs: an exploratory analysis. Perspectives on sexual and reproductive health. 2014;46:157–63. doi: 10.1363/46e2014. [DOI] [PubMed] [Google Scholar]
- 22.Isidori AM, Pozza C, Esposito K, Giugliano D, Morano S, Vignozzi L, et al. Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. The journal of sexual medicine. 2010;7:1139–46. doi: 10.1111/j.1743-6109.2009.01635.x. [DOI] [PubMed] [Google Scholar]
- 23.Stulhofer A, Busko V, Brouillard P. Development and bicultural validation of the new sexual satisfaction scale. Journal of sex research. 2010;47:257–68. doi: 10.1080/00224490903100561. [DOI] [PubMed] [Google Scholar]
- 24.SAS software. Base SASR 9.4 Procedures Guide. Cary, NC: SAS Institute, Inc; 2015. [Google Scholar]
- 25.Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. Journal of sex & marital therapy. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 26.Oddens BJ. Women's satisfaction with birth control: a population survey of physical and psychological effects of oral contraceptives, intrauterine devices, condoms, natural family planning, and sterilization among 1466 women. Contraception. 1999;59:277–86. doi: 10.1016/s0010-7824(99)00034-7. [DOI] [PubMed] [Google Scholar]
- 27.Skrzypulec V, Drosdzol A. Evaluation of quality of life and sexual functioning of women using levonorgestrel-releasing intrauterine contraceptive system--Mirena. Collegium antropologicum. 2008;32:1059–68. [PubMed] [Google Scholar]
- 28.Gorgen H, Api M, Akca A, Cetin A. Use of the Levonorgestrel-IUS in the treatment of menorrhagia: assessment of quality of life in Turkish users. Arch Gynecol Obstet. 2009;279:835–40. doi: 10.1007/s00404-008-0834-x. [DOI] [PubMed] [Google Scholar]
- 29.Enzlin P, Weyers S, Janssens D, Poppe W, Eelen C, Pazmany E, et al. Sexual functioning in women using levonorgestrel-releasing intrauterine systems as compared to copper intrauterine devices. The journal of sexual medicine. 2012;9:1065–73. doi: 10.1111/j.1743-6109.2011.02266.x. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. MMWR. 5. Vol. 62. Atlanta: CDC; 2013. US Selected Practice Recommendations for Contraceptive Use, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.