Abstract
Objectives
To assess the influence of cone beam CT (CBCT) on treatment plan before surgical intervention of mandibular third molars and to identify radiographic factors with an impact on deciding on coronectomy.
Methods
186 mandibular third molars with an indication for surgical intervention underwent a radiographic examination with two methods: (1) panoramic imaging in combination with stereo-scanography and (2) CBCT. After the radiographic examination a treatment plan (TP) was established: either surgical removal (Sr) or coronectomy (Co). The first TP was based on the panoramic image and stereo-scanogram, while the second TP was established after CBCT was available. Logistic regression analyses were used to identify factors predisposing for Co after CBCT.
Results
Treatment was performed according to the second TP. Agreement between the first and second TP was seen in 164 cases (88%), while the TP changed for 22 teeth (12%) after CBCT. Direct contact between the third molar and the mandibular canal had the highest impact on deciding on Co [odds ratio (OR) = 101.8, p < 0.001]. Direct contact was not a sufficient factor, however; thus, lumen narrowing of the canal (OR = 38.9–147.2, p < 0.001) and canal positioned in a bending or a groove in the root complex (OR = 32.8, p = 0.016) were additional canal-related factors for deciding on Co.
Conclusion
CBCT influenced the treatment plan for 12%. Direct contact in combination with narrowing of the canal lumen and canal positioned in a bending or a groove in the root complex observed in CBCT images were significant factors for deciding on coronectomy.
Keywords: radiography, coronectomy, third molar
Surgical intervention of semi-impacted mandibular third molars traditionally involves removal of the entire tooth. Recently, coronectomy (i.e. removal of the tooth crown leaving the root complex) has, however, become common in cases where direct contact between the tooth and the mandibular canal is observed in radiographs to avoid injury to the inferior alveolar nerve (IAN).1-5 An altered neurosensory function of the IAN is most often temporary, but if the condition becomes permanent it is a significant surgical complication.6
Several radiographic methods are available for treatment planning before removal of mandibular third molars. The traditional method and state-of-the art is panoramic imaging,7 in some cases combined with intraoral images or other image modalities providing different projection angles.8 If the roots of the third molar over-project the mandibular canal in the panoramic image further examination may be necessary. An option for further assessment is stereo-scanography, which has been known since the 1990s.8-10 In stereo-scanograms the relation between the roots of the third molar and the mandibular canal can be determined by viewing with stereopsis or using the tube shift technique.9,11
Cone beam CT (CBCT) has recently been introduced as a valuable diagnostic method in dentistry;12,13 however, the present knowledge of the impact of CBCT on diagnosis and treatment decision as well as treatment outcome is limited. One study examined root resorption of the lateral incisor caused by an ectopically positioned canine and found that orthodontists' management decisions were not much influenced by CBCT compared with a panoramic image alone or intraoral images.14 CBCT has also been suggested for the radiographic examination of mandibular third molars where an intimate relationship to the mandibular canal is suspected, because it adds detailed information on the bucco-oral aspect of the roots and jaw, including the position and course of the mandibular canal.15-19 It was recently reported in a pilot study that the surgical technique was changed (removal of bone, elevator placement, tooth sectioning) when CBCT was available compared with only panoramic images before surgical removal of mandibular third molars.20 No studies, however, have examined the impact of CBCT on treatment planning before surgical intervention of mandibular third molars.
The aims of this study were to assess the influence of CBCT on treatment plan before surgical intervention of mandibular third molars and to identify radiographic factors with an impact on deciding on coronectomy vs surgical removal.
Material and methods
Patients
The study was approved by the local Committee of Ethics, Aarhus, Denmark. A total of 294 patients (with 565 mandibular third molars) underwent a clinical examination and were screened for participation in this study. The patients were recruited from the section of Oral and Maxillofacial Surgery and Oral Pathology, Department of Dentistry, Aarhus University, Denmark, to have one or two mandibular third molars surgically removed. A panoramic radiograph was at disposal for the clinical examination. The panoramic radiograph was either included in the referral records of the patient from the general practitioner or a panoramic examination was performed at the section of Oral Radiology, Department of Dentistry, Aarhus University, Denmark, using either a Cranex Tome unit (Soredex, Helsinki, Finland) with a phosphor image plate receptor (Digora image plate and PCT scanner; Soredex, Helsinki, Finland) or a ProMax unit (Planmeca, Helsinki, Finland) with a charge-coupled device (CCD)-based image receptor. After the clinical examination it was decided whether surgical intervention was indicated. Indications were (1) recurring episodes of pericoronitis (≥ 2 episodes); (2) caries or resorption of the second molar (distal surface); (3) unrestorable caries of the third molar; (4) progressive marginal bone loss of the second molar (distal surface) or third molar; or (5) other pathological conditions related to the third molar. Only third molars scheduled for removal demonstrating over-projection of the roots/parts of the tooth and the mandibular canal in the panoramic image were included in this study. The study eventually included 186 mandibular third molars (89 left-side and 97 right-side molars) in 135 patients (68 males and 67 females; mean age: 25.5 years, range: 18.2–68.3 years). These patients were referred to the department of oral radiology for additional radiographic examinations.
Radiographic examination
The additional radiographic examinations consisted of stereo-scanography and a three-dimensional (3D) CBCT examination. A Scanora unit (Soredex, Helsinki, Finland) was used for the scanography, and the image receptor was a Digora phosphor plate. The stereo-scanograms consisted of a series of four images (stereo-scopic multiview), which displayed the third molar in one orthogonal and one disto-eccentric projection and two projections cranial to these.9 In both directions the tube shift angle was 4°. This technique allows for viewing with stereopsis, but also the tube-shift rule can be used.9-11
Two CBCT units were used for the CBCT examinations, either the NewTom 3G (QR SRL, Verona, Italy; 83 third molars) or the Scanora 3D (103 third molars). In the NewTom scanner, the patients were examined with a 6-inch field of view (FOV) and in the Scanora 3D with a 6 × 6 cm FOV. The FOV was centred at the mandibular third molar region. Unfortunately, the NewTom 3G was not available in the last part of the study period for patient inclusion; therefore, more third molars were examined with the Scanora 3D.
The stereo-scanograms and panoramic images were exported from their dedicated software and viewed in general software (DigiView PACS) with possibilities to use zoom function and image enhancement such as brightness, contrast and gamma curve functions. The CBCT scans were reconstructed in the three planes, axial, sagittal and coronal, and viewed in their dedicated software (NNT for NewTom 3G; OnDemand® for Scanora 3D). All images were assessed on flat panel 19- or 20-inch quality monitors: SyncMaster 203B (Samsung, Cheonan City, Korea), Olorin VistaLine (Olorin AB, Kungsbacka, Sweden) or Philips 190S (Philips, Eindhoven, The Netherlands)).
Radiographic assessment
One of three trained observers (two oral radiologists and one under specialist training) recorded the following tooth-related variables for the third molar in question in stereo-scanograms and CBCT scans: (1) state of impaction (impacted/semi-impacted); (2) angulation (horizontal/disto-angulated/mesio-angulated/vertical); (3) number of roots (1, 2 or > 2); (4) root morphology of the distal and mesial root (assessed separately; straight/buccal-/oral-/distal-/mesial bending); and (5) relation to the mandibular canal (direct contact/no direct contact).
The relationship between the roots of the third molar and the mandibular canal was assessed according to the radiographic method used. Thus, in the scanograms, direct contact was recorded, if the third molar and the mandibular canal were at the same level in the bucco-oral plane as viewed with stereopsis and/or the tube-shift rule. In the CBCT, direct contact was recorded, if there was no bony separation between the third molar and the mandibular canal in at least one of the three section planes. In these cases the following canal-related variables were recorded: (1) the diameter of the canal lumen in its course over the tooth/roots (constant lumen diameter, more than half of the lumen diameter or half or less of the lumen diameter); (2) canal positioned in a bending or a groove in the root complex (yes/no); 3) extent of the contact area between the root complex and the canal (less than half of the root length or half or more of the root length).
The observers stated their findings from the scanograms and CBCT images in two separate reports. In the majority of the cases, the scanogram and the CBCT examination of the same tooth was assessed by two different observers. In the few cases where both radiographic examinations of the same tooth were assessed by the same observer, a longer time period was intercalated between the assessments to minimize registration bias. The radiographic reports were available to the surgeons together with the actual images during the treatment planning.
Surgical treatment plan
One of the radiologists, together with two surgeons (an oral and maxillofacial surgeon—the same for all cases—and the operating surgeon) went through each imaging method while at the same time having access to the radiologist's report. On the basis of the clinical examination, panoramic image, stereo-scanograms and the radiographic report of the scanograms, the surgeons then established in consensus the first treatment plan. There were two options: (1) surgical removal of the entire tooth, or (2) removal of the tooth crown leaving the root complex (coronectomy). Afterwards, a second treatment plan with the same options was established on basis of the CBCT scan and the radiographic report of this examination.
Surgical treatment
The patients were given ibuprofen (600 mg) and performed mouth-rinsing for 1 min with a 0.12% chlorhexidine solution pre-operatively. A standard flap approach was used for all surgical procedures. After raising a full-thickness mucoperiostal flap, buccal/distal bone was removed with a burr under sterile saline irrigation. When surgical removal was performed, the tooth was removed in one piece or several pieces after sectioning with a burr also under sterile saline irrigation. Coronectomy was performed by horizontally splitting the crown of the third molar at the level of the cemento-enamel junction without mobilizing the root complex. The root complex was lowered approximately 2–3 mm under the level of the adjacent bone and left in situ. When surgical removal was performed, the socket was inspected to identify whether the IAN was visible. Inflammatory tissue and sharp bone edges were removed before meticulous irrigation of the extraction socket and the operation field. Finally, the flap was repositioned and sutured using two or three resorbable sutures (Vicryl 4-0, Ethicon, Germany).
The patient was given standard post-operative information and a prescription for 600 mg of ibuprofen to be taken up to three times daily as needed. In addition, the patients were instructed to perform mouth-rinsing with 0.12% chlorhexidine solution twice daily for 1 week. The patients underwent a control examination and had the sutures removed 1 week post-operatively.
Data treatment
Based on the second treatment plan, initial logistic regression analyses with coronectomy as the outcome variable were performed for all tooth-related variables (state of impaction, angulation, number of roots, root morphology and relation to the mandibular canal) to identify factors observed in CBCT predisposing for deciding on coronectomy. Root morphology was recoded for the mesial and distal root components separately in three ways: (1) bending/no bending; (2) buccal or oral bending/no buccal or oral bending, and (3) mesial or distal bending/no mesial or distal bending. These recoded categories were all tested separately. Only variables that showed a statistically significant impact on deciding on coronectomy in the initial analyses were entered into the final multivariate logistic regression analysis together with patient-related variables (gender and age). Age was entered ascending as a continuous-scale variable.
Since the most significant factor for deciding on coronectomy was direct contact between the root complex and the mandibular canal, additional initial logistic regression analyses with coronectomy as the outcome variable were performed selecting only molars with direct contact between the tooth and the mandibular canal, and the following canal-related variables were entered: (1) diameter of the canal lumen, (2) canal positioned in a bending or a groove in the root complex, and (3) extent of the contact area between the root complex and the canal. Only variables that showed a statistically significant impact on deciding on coronectomy in the initial analyses were entered into the final multivariate logistic regression analysis together with gender and age.
The data were analysed using SPSS v. 13.0 and a 5% level of significance was applied.
Results
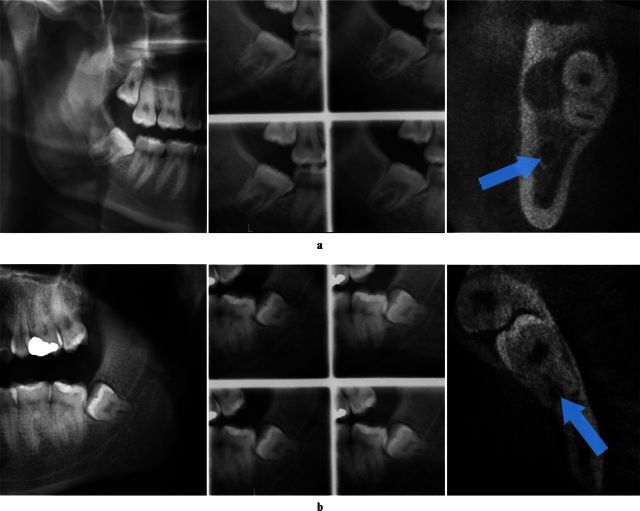
Table 1 shows the treatment plans based on the panoramic image and scanograms combined and on the CBCT images. Agreement between surgical removal/coronectomy in the first and second treatment plan was seen in 164 (88.2%) cases (surgical removal, 139; coronectomy, 25). Figure 1a shows an example of a right third molar where surgical removal was decided in both treatment plans. The treatment plan changed for 22 (11.8%) of the 186 teeth. For seven molars, the treatment plan was changed from coronectomy to surgical removal. They were all assessed to have direct contact between the roots of the molar and the mandibular canal on scanograms, but CBCT showed bony separation between these structures. 15 molars changed treatment plan from surgical removal to coronectomy; an example is shown in Figure 1b. All except one (which was assessed to have no direct contact between the tooth and the mandibular canal, but the canal was positioned in a bending of the root complex) were assessed with direct contact between the roots of the molar and the mandibular canal on CBCT, but not on scanograms.
Table 1. Treatment plans based on panoramic image and scanograms or cone beam CT (number of teeth; percentage in parentheses).
| CBCT | Panoramic image and scanograms |
||
| Surgical removal | Coronectomy | Total | |
| Surgical removal | 139 (74.7) | 7 (3.8) | 146 |
| Coronectomy | 15 (8.1) | 25 (13.4) | 40 |
| Total | 154 | 32 | 186 |
CBCT, cone beam CT.
Figure 1.
Two representative cases. From left to right: panoramic image, stereo-scanogram and cone beam CT (CBCT). Arrows indicate the mandibular canal. (a) No change in treatment plan. Surgical removal was decided on the basis of panoramic image and stereo-scanogram as well as CBCT. (b) Change in treatment plan. Surgical removal was decided on the basis of panoramic image and stereo-scanogram, while coronectomy was decided after CBCT
As a result, coronectomy was eventually planned for 40 (25 and 15) molars after CBCT. Since the surgeons were most confident with the treatment plan after CBCT, this plan was the basis for the final treatment decision, and all third molars were intended to be operated according to that. However, the root complex of one molar, scheduled for coronectomy, mobilized during the operation; consequently, the tooth was removed and included in the surgical removal group (surgical removal, n = 147, coronectomy, n = 39).
Table 2 shows the tooth-related variables as recorded in CBCT in relation to the surgical treatment. When tested in the logistic regression analysis with coronectomy as the outcome, Table 3 shows that direct contact between the roots of the molar and the mandibular canal highly predisposed for deciding on coronectomy, and the probability for coronectomy was over 100 times higher if there was direct contact [odds ratio (OR) = 102; p < 0.001]. The only other significant tooth-related factor was a bending of the distal root in the bucco-oral plane (OR = 23, p = 0.002), and finally increased age was associated with a slightly higher probability of coronectomy (OR = 1.1, p = 0.04).
Table 2. Distribution of tooth-related variables as observed in cone beam CT in relation to surgical intervention.
| Parameter | Surgical removal (n = 147) | Coronectomy (n = 39) |
| State of impaction | ||
| impacted | 9 | 3 |
| semi-impacted | 138 | 36 |
| Angulation | ||
| horizontal | 30 | 6 |
| distal | 20 | 2 |
| mesial | 53 | 16 |
| vertical | 44 | 15 |
| Number of roots | ||
| 1 | 16 | 2 |
| 2 | 109 | 30 |
| > 2 | 22 | 7 |
| Distal root, any bending | ||
| yes | 51 | 10 |
| no | 96 | 29 |
| Distal root, buccal or oral bending | ||
| yes | 10 | 7 |
| no | 137 | 32 |
| Distal root, mesial or distal bending | ||
| yes | 59 | 16 |
| no | 88 | 23 |
| Mesial root, any bending | ||
| yes | 103 | 29 |
| no | 44 | 10 |
| Mesial root, buccal or oral bending | ||
| yes | 15 | 3 |
| no | 132 | 36 |
| Mesial root, mesial or distal bending | ||
| yes | 112 | 31 |
| no | 35 | 8 |
| Direct contact with the canal | ||
| yes | 54 | 37 |
| no | 93 | 2 |
Table 3. Multivariate logistic regression analysis for tooth-related factors as well as gender and age, predisposing for coronectomy as the surgical intervention (total, n = 186; the reference category in parentheses).
| Parameter | Coronectomy (n = 39) |
||
| Odds ratio | p-value | 95% CI | |
| Relation to the canal (not direct) | |||
| direct | 101.8 | < 0.001 | 14.782–700.364 |
| Gender (male) | |||
| female | 1.0 | 0.938 | 0.409–2.633 |
| Age (ascending) | 1.1 | 0.040 | 1.004–1.109 |
| Distal root, buccal/oral bending (no bending) | |||
| bending | 23.3 | 0.002 | 3.202–169.775 |
CI, confidence interval.
It is seen from Table 2 that direct contact between the tooth and the canal was observed in 37 of the 39 teeth that received coronectomy (for 2 teeth within the coronectomy group bony separation was recorded, 1 with the canal placed in a bending of the root complex and the other with high risk for compromising the IAN during the removal due to a buccal bending of the root complex). However, direct contact was also seen in 36.7% of the teeth that were surgically removed. This means that direct contact to the canal was a necessary (all but two) but not sufficient sign in CBCT to decide on coronectomy. Therefore, additional analyses were performed to identify other canal-related factors that predisposed for coronectomy by selecting only third molars with direct contact to the canal (n = 91). Table 4 shows the logistic regression analysis with coronectomy as the outcome in the group of teeth with direct contact to the canal. All canal-related variables except “contact area” were highly significant factors for deciding on coronectomy. The probability of choosing coronectomy was extremely high if the lumen of the canal was narrowed, approximately 40 times higher if there was a buccal or oral bending on the distal root, and almost 33 times higher if the canal was positioned in bending or a groove in the root complex. The distribution of the canal-related variables between the coronectomy and the surgical removal group in cases with direct contact to the canal is shown in Table 5.
Table 4. Multivariate logistic regression analysis for additional canal-related factors predisposing for a coronectomy as the surgical treatment within the group of molars with direct contact to the mandibular canal (total with direct contact, n = 91; the reference category in parentheses).
| Parameter | Coronectomy (n = 37) |
||
| Odds ratio | p-value | 95% CI | |
| Gender (male) | |||
| female | 0.6 | 0.520 | 0.15–2.61 |
| Age (ascending) | 1.1 | 0.153 | 0.96–1.33 |
| Distal root, buccal or oral bending (no) | |||
| yes | 41.7 | 0.004 | 3.38–513.73 |
| Diameter of the canal lumen (constant) | |||
| > ½ the diameter | 147.2 | < 0.001 | 14.50–1493.43 |
| ≤ ½ the diameter | 38.9 | < 0.001 | 6.92–218.92 |
| Canal in root bending (no) | |||
| yes | 32.8 | 0.016 | 1.90–566.97 |
| Contact area between root and canal (< ½ of the root length) | |||
| ≥ ½ of the root length | 1.1 | 0.911 | 0.20–6.21 |
CI, confidence interval.
Table 5. Distribution of additional canal-related variables in cases observed with direct contact to the canal in CBCT in relation to surgical treatment.
| Parameter | Direct contact to canal in CBCT (n = 91) |
||
| Surgical removal (n = 54) | Coronectomy (n = 37) |
||
| Changed (n = 14) | Remained (n = 23) | ||
| Diameter of the canal lumen | |||
| constant | 27 (50%) | 2 (14%) | 1 (4%) |
| > ½ of the size | 22 (41%) | 3 (21%) | 6 (26%) |
| ≤ ½ of the size | 5 (9%) | 9 (64%) | 16 (70%) |
| Canal in a root bending | |||
| no | 53 (98%) | 10 (71%) | 21 (91%) |
| yes | 1 (2%) | 4 (29%) | 2 (9%) |
| Contact area between root and canal | |||
| < ½ of the root length | 49 (91%) | 13 (93%) | 11 (48%) |
| ≥ ½ of the root length | 5 (9%) | 1 (7%) | 12 (52%) |
CBCT, cone beam CT.
Table 5 also shows the additional canal-related variables in the coronectomy group distributed between those teeth where treatment plan was changed to coronectomy and those that remained in the coronectomy group after CBCT. The major reason for the change seems to be narrowing of the canal lumen, which was seen in 12 out of the 14 that changed, while the other factors (canal positioned in a root bending and large contact area between root and canal) explained the remaining.
At the 1 week follow-up two patients complained about paraesthesia of the lower lip (the inferior alveolar nerve), but after 1 month they both had normal sensation. The two third molars in question were surgically removed; one was scheduled for surgical removal in both treatment plans, and one had changed from coronectomy to surgical removal after CBCT.
Discussion
It is generally accepted that a panoramic image is the method of first choice for assessment of mandibular third molars before surgery (Radiation protection. European guidelines on radiation protection in dental radiology. The safe use of radiographs in dental practice. European Committee Issue N° 136 2004), and many previous studies have focused on the validity of the panoramic image.16,21-28 Traditionally, seven signs that indicate direct contact between the roots of the third molar and the mandibular canal have been used in panoramic images,29 but they are not equally reliable. In a recent review it was concluded that three of the signs (interruption of the white line of the canal, diversion of the canal and darkening of the roots) were more valid than the remaining four,30,31 but it was also concluded that absence of these signs could not ensure that direct contact does not exist. If the roots of the mandibular third molar over-project the mandibular canal in the initial image, projections from different angles or planes are therefore usually needed. The traditional method is intraoral radiography with eccentric projections, which, however, may be quite uncomfortable for the patient and result in many retakes.32 Another frequently used method in our department is stereo-scanography, with four differently angulated projections, which has been shown to be a valid method, and even more valid than intraoral eccentric radiography for assessment of mandibular third molars.8,10,33 If this modality is not available, an alternative may be a posteroanterior open mouth projection, which is frequently used in other departments.18
Even with the use of stereopsis it may not always be easy to determine the relation between the molar and the mandibular canal in stereo-scanograms. CBCT imaging is a relatively new modality that has the advantage of displaying the bucco-oral aspect of the relation between the molar and the canal, and several studies have assessed the use of CBCT before surgical removal of mandibular third molars and found CBCT to be superior to panoramic images to display the relation between the molar and the mandibular canal.15-19,25,34 However, no previous study has examined whether the treatment plan will change when CBCT is available compared with merely a panoramic image and scanograms, or which factors that have an impact on deciding on coronectomy vs surgical removal of the entire tooth.
The surgeons in the present study established the treatment plan on the basis of the CBCT findings, and the second treatment plan was therefore the final treatment plan. It may be acknowledged though that the two treatment plans were identical for 88% of the cases and for 63% of those that eventually received coronectomy. Thus, 12% of the third molars changed treatment plan after CBCT. It is not possible to speculate on the number of post-operative complications that might have occurred if the treatment had been performed according to the first treatment plan, which was based on panoramic images and scanograms, a method that is less dose- and work-demanding than CBCT. Only randomized clinical trials can determine whether fewer complications will occur if the treatment is based on CBCT compared with other less resource-requiring modalities. A review on CBCT has argued that CBCT should not be seen as a reference standard since, being a diagnostic method, it is in itself apt to both false-positive (direct contact is seen, which in reality does not exist) and false-negative registrations (direct contact is not seen, but exists in reality).35 Whether false-negative registrations were made in CBCT images or other factors were decisive for the two cases with sensory disturbances cannot be determined from the present study.
A recently published study found that direct contact between the roots of the third molar and the mandibular canal and lumen narrowing observed in CBCT images were risk factors for higher IAN impairment after surgery.34 Another study used absence of bony separation between the roots and the canal on CBCT as an eligible reason for deciding on coronectomy instead of surgical removal. It was suggested that coronectomy should be the treatment of choice when there was a high risk for IAN injury. In that study, two patients in the surgical removal group (n = 87) had paraesthesia of the lower lip and chin and none in the coronectomy group (n = 88).3 Sensory changes after surgical removal of mandibular third molars due to injury of the IAN has been stated to range between 0.3% and 8.4% in a recent review.6 In our study, no permanent sensory disturbances were reported, but temporary sensory disturbances were reported in two cases, which is 1.2% of the total number of surgically removed teeth. In one of these cases, surgical removal was decided both when the treatment plan was based on stereograms and CBCT, and in the other case the treatment plan had changed from coronectomy to surgical removal after CBCT.
Semi-impacted mandibular third molars are traditionally treated by removal of the entire tooth. In recent years, it has been suggested that molars with an intimate relation to the mandibular canal as observed in radiographs may be treated by coronectomy to minimize the risk of injury to the IAN.1-5 When surgical intervention of the third molar was indicated, the treatment plan involved surgical removal or coronectomy. As may be expected, the observation with the highest impact on deciding on coronectomy was direct contact to the mandibular canal. The probability of coronectomy was over 100 times higher if there was no bony separation between the third molar and the mandibular canal than if bone was separating these structures in the CBCT sections. Thus, the relation to the canal was an important factor when establishing the treatment plan, which can also be seen from the seven cases in which the treatment plan changed from coronectomy to surgical removal. In these cases, CBCT revealed bony separation between the roots of the third molar and the mandibular canal, although the relation was registered as direct in the stereo-scanograms. However, direct contact to the canal observed in CBCT images was a “necessary but not sufficient” sign for determining coronectomy, since not all 91 cases where this sign was present were treated by coronectomy. Further analyses thus showed that the probability for coronectomy was extremely high, if the diameter of the canal lumen narrowed in its course over the tooth/roots, and this factor, in addition with no bony separation between the structures, explained most of the changes occurring from surgical removal to coronectomy. There were two molars assigned to coronectomy, which in the radiographic report did not have direct contact to the canal. In one of these cases the canal was positioned in a bending of the root complex, and in the other case the risk for compromising the IAN during removal was very high due to a buccal bending of the root.
In conclusion, the treatment plan based on a panoramic image and stereo-scanogram combined and on CBCT was identical in 88% of the cases. The treatment plan changed in 12% of the cases, and the majority of these changes were from surgical removal to coronectomy. Of the 20% (39 of 186 third molars) of the examined teeth within the coronectomy group, the highest impact factor for this decision was direct contact (no bony separation) between the third molar and the mandibular canal. Direct contact was, however, not a sufficient factor for deciding on coronectomy (37 coronectomies out of 91 teeth with direct contact), but in combination with lumen narrowing and the canal positioned in a bending or a groove of the root complex it was favoured at the expense of removal of the entire tooth. The present strategy resulted in two cases with temporary sensory disturbances (1.08%), and none were permanent.
Acknowledgments
Bjarne Simonsen, Jens Hartlev and Birgit Kenrad are thanked for contributing their knowledge and time.
Footnotes
The authors would like to thank “Calcinfonden” for financial support to carry out the study.
References
- 1.Renton T, Hankins M, Sproate C, McGurk M. A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg 2005;43:7–12. [DOI] [PubMed] [Google Scholar]
- 2.Leung YY, Cheung LK. Can coronectomy of wisdom teeth reduce the incidence of inferior dental nerve injury? Ann R Australas Coll Dent Surg 2008;19:50–51. [PubMed] [Google Scholar]
- 3.Cilasun U, Yildirim T, Guzeldemir E, Pektas ZO. Coronectomy in patients with high risk of inferior alveolar nerve injury diagnosed by computed tomography. J Oral Maxillofac Surg 2011;69:1557–1561. [DOI] [PubMed] [Google Scholar]
- 4.Leung YY, Cheung LK. Safety of coronectomy versus excision of wisdom teeth: a randomized controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:821–827. [DOI] [PubMed] [Google Scholar]
- 5.Dolanmaz D, Yildirim G, Isik K, Kucuk K, Ozturk A. A preferable technique for protecting the inferior alveolar nerve: coronectomy. J Oral Maxillofac Surg 2009;67:1234–1238. [DOI] [PubMed] [Google Scholar]
- 6.Leung YY, Cheung LK. Risk factors of neurosensory deficits in lower third molar surgery: an literature review of prospective studies. Int J Oral Maxillofac Surg 2011;40:1–10. [DOI] [PubMed] [Google Scholar]
- 7.Radiation Protection136:Europeanguidelinesonradiationprotectionindentalradiology the safeuseofradiographsindentalpractice Luxembourg: Office for Official Publications of the European Communities; 2004. Available from: ec.europa.eu/energy/nuclear/radioprotection/publication/doc/136_en.pdf [Google Scholar]
- 8.Wenzel A, Aagaard E, Sindet-Pedersen S. Evaluation of a new radiographic technique: outcome following removal of mandibular third molars. Dentomaxillofac Radiol 1998;27:264–269. [DOI] [PubMed] [Google Scholar]
- 9.Tammisalo T, Happonen RP, Tammisalo EH. Stereographic assessment of mandibular canal in relation to the roots of impacted lower third molar using multiprojection narrow beam radiography. Int J Oral Maxillofac Surg 1992;21:85–89. [DOI] [PubMed] [Google Scholar]
- 10.Wenzel A, Aagaard E, Sindet-Pedersen S. Evaluation of a new radiographic technique: diagnostic accuracy for mandibular third molars. Dentomaxillofac Radiol 1998;27:255–263. [DOI] [PubMed] [Google Scholar]
- 11.Wenzel A. Dental students' ability for three-dimensional perception of two-dimensional images using natural stereopsis: its impact on radiographic localization. Dentomaxillofac Radiol 1999;28:98–104. [DOI] [PubMed] [Google Scholar]
- 12.Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E. Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 2009;38:187–195. [DOI] [PubMed] [Google Scholar]
- 13.Carter L, Farman AG, Geist J, Scarfe WC, Angelopoulos C, Nair MK, et al. American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:561–562. [DOI] [PubMed] [Google Scholar]
- 14.Bjerklin K, Bondemark L. Ectopic maxillary canines and root resorption of adjacent incisors. Does computed tomography (CT) influence decision-making by orthodontists? Swed Dent J 2008;32:179–185. [PubMed] [Google Scholar]
- 15.Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N, et al. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:253–259. [DOI] [PubMed] [Google Scholar]
- 16.Suomalainen A, Venta I, Mattila M, Turtola L, Vehmas T, Peltola JS. Reliability of CBCT and other radiographic methods in preoperative evaluation of lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:276–284. [DOI] [PubMed] [Google Scholar]
- 17.Neugebauer J, Shirani R, Mischkowski RA, Ritter L, Scheer M, Keeve E, et al. Comparison of cone-beam volumetric imaging and combined plain radiographs for localization of the mandibular canal before removal of impacted lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:633–42; discussion 643. [DOI] [PubMed] [Google Scholar]
- 18.Flygare L, Ohman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig 2008;12:291–302. [DOI] [PubMed] [Google Scholar]
- 19.Susarla SM, Sidhu HK, Avery LL, Dodson TB. Does computed tomographic assessment of inferior alveolar canal cortical integrity predict nerve exposure during third molar surgery? J Oral Maxillofac Surg 2010;68:1296–1303. [DOI] [PubMed] [Google Scholar]
- 20.Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Vlijmen OJ, et al. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int J Oral Maxillofac Surg 2011;40:834–839. [DOI] [PubMed] [Google Scholar]
- 21.Bell GW. Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve. Radiological and surgical findings, and clinical outcome. Br J Oral Maxillofac Surg 2004;42:21–27. [DOI] [PubMed] [Google Scholar]
- 22.Benediktsdottir IS, Wenzel A. Accuracy of digital panoramic images displayed on monitor, glossy paper, and film for assessment of mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:217–222. [DOI] [PubMed] [Google Scholar]
- 23.Bundy MJ, Cavola CF, Dodson TB. Panoramic radiographic findings as predictors of mandibular nerve exposure following third molar extraction: digital versus conventional radiographic techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:e36–40. [DOI] [PubMed] [Google Scholar]
- 24.Ferrus-Torres E, Gargallo-Albiol J, Berini-Aytes L, Gay-Escoda C. Diagnostic predictability of digital versus conventional panoramic radiographs in the presurgical evaluation of impacted mandibular third molars. Int J Oral Maxillofac Surg 2009;38:1184–1187. [DOI] [PubMed] [Google Scholar]
- 25.Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Berge SJ. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg 2009;38:964–971. [DOI] [PubMed] [Google Scholar]
- 26.Monaco G, Montevecchi M, Bonetti GA, Gatto MR, Checchi L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc 2004;135:312–318. [DOI] [PubMed] [Google Scholar]
- 27.Nakamori K, Fujiwara K, Miyazaki A, Tomihara K, Tsuji M, Nakai M, et al. Clinical assessment of the relationship between the third molar and the inferior alveolar canal using panoramic images and computed tomography. J Oral Maxillofac Surg 2008;66:2308–2313. [DOI] [PubMed] [Google Scholar]
- 28.Szalma J, Lempel E, Csuta T, Bartfai D, Jeges S, Olasz L. The role of panoramic radiography in assessing the risk of injury to the inferior alveolar nerve before the extraction of mandibular wisdom teeth. The effect of the extent of root curvature and inferior alveolar canal-root tip overlap on the risk assessment. Fogorv Sz 2010;103:43–48. [PubMed] [Google Scholar]
- 29.Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 1990;28:20–25. [DOI] [PubMed] [Google Scholar]
- 30.Atieh MA. Diagnostic accuracy of panoramic radiography in determining relationship between inferior alveolar nerve and mandibular third molar. J Oral Maxillofac Surg 2010;68:74–82. [DOI] [PubMed] [Google Scholar]
- 31.Wenzel A. It is not clear whether commonly used radiographic markers in panoramic images possess predictive ability for determining the relationship between the inferior alveolar nerve and the mandibular third molar. J Evid Based Dent Pract 2010;10:232–234. [DOI] [PubMed] [Google Scholar]
- 32.Matzen LH, Christensen J, Wenzel A. Patient discomfort and retakes in periapical examination of mandibular third molars using digital receptors and film. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:566–572. [DOI] [PubMed] [Google Scholar]
- 33.Matzen LH, Christensen J, Wenzel A. Accuracy of scanography using storage phosphor plate systems and film for assessment of mandibular third molars. Dentomaxillofac Radiol 2011;40:306–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eyrich G, Seifert B, Matthews F, Matthiessen U, Heusser CK, Kruse AL, et al. 3-dimensional imaging for lower third molars: is there an implication for surgical removal? J Oral Maxillofac Surg 2011;69:1867–1872. [DOI] [PubMed] [Google Scholar]
- 35.Guerrero ME, Shahbazian M, Elsiena Bekkering G, Nackaerts O, Jacobs R, Horner K. The diagnostic efficacy of cone beam CT for impacted teeth and associated features: a systematic review. J Oral Rehabil 2011;38:208–216. [DOI] [PubMed] [Google Scholar]