Abstract
Background
Defecatory disorders (DD) are defined by clinical and objective features of impaired rectal evacuation. The epidemiology of DD in the population is unknown, partly because many constipated patients do not undergo anorectal tests. Our objectives were to estimate the incidence rate and clinical features of DD in the community.
Methods
We reviewed the medical records of all patients older than 16 years in Olmsted County, MN, who had constipation and underwent anorectal manometry from 1999 through 2008. Criteria for diagnosing DD were constipation for 6 months or longer and one of the following: (i) abnormal rectal balloon expulsion test; (ii) reduced or increased perineal descent; or (iii) two or more abnormal features with defecography or surface electromyography.
Key Results
Of 11,112 constipated patients, 516 had undergone anal manometry; 245 of these (209 women, 36 men) had a DD. The mean (±SD) age at diagnosis was 44 years (±18) among women and 49 years (±19) among men. The overall age- and sex-adjusted incidence rate per 100,000 person-years was 19.3 (95% CI, 16.8–21.8). The age-adjusted incidence per 100,000 person-years was greater (P<.0001) in women (31.8 [95% CI, 27.4–36.1]) than in men (6.6 [95%, CI, 4.4–8.9]). Prior to the diagnosis of DD, nearly 30% of patients had irritable bowel syndrome (IBS), 48% had a psychiatric diagnosis, 18% had a history of abuse, and 21% reported urinary and/or fecal incontinence.
Conclusions & Inferences
Among constipated patients, DD are four-fold more common in women than men and often associated with IBS and psychiatric diagnoses.
Keywords: constipation, defecation, defecography, incidence
Chronic constipation is one of the most common digestive complaints. It affects 16% of Americans and accounts for more than $230 million annually in constipation-related U.S. health care costs (1). Studies from tertiary medical centers suggest that up to 50% of patients with chronic constipation have a defecatory disorder (DD) which results from inadequate propulsive rectal forces and/or increased resistance, functional not anatomical, to evacuation (2–5). It is important to diagnose DD because this condition is better managed with pelvic floor retraining (i.e., biofeedback therapy) than with laxatives (6–8).
A study from Olmsted County published in 1993 suggested that the age-adjusted prevalence of symptoms of functional constipation and DD in Olmsted County was 19 and 11 per 100 individuals, respectively (9). In that study, DD was diagnosed by symptoms only. However, while the history and a careful digital rectal examination may suggest a defecatory disorder, the diagnosis requires anorectal testing (10, 11). Since anorectal tests are not widely available in the community, it is conceivable that DD may not be diagnosed in constipated patients (12). Also, while there have been several trials of pelvic floor retraining with biofeedback therapy, few studies have described the clinical features of DD (13, 14). From a public health perspective, an estimate of the incidence of DD in the community may be useful for highlighting the role of anorectal testing and planning for future needs. Hence, the aims of this study were to estimate the incidence rate and clinical features of clinically diagnosed DD in a community.
METHODS
Setting
This study was approved by the Institutional Review Board at Mayo Clinic in Rochester, Minnesota.
Olmsted County is located in southeastern Minnesota, 90 miles from a major metropolitan center (Minneapolis/St. Paul). The 2010 census population was 144,248, with approximately 30% employed in the health care industry. The urban center of Rochester (2010 population, 106,769) is surrounded by rural countryside. The demographic characteristics closely resemble the US white population (15).
Residents of Olmsted County receive their medical care almost exclusively from two group practices - Mayo Clinic and Olmsted Medical Center. Mayo Clinic has maintained a common medical record system with its affiliated hospital (Mayo Clinic Hospital — Rochester) for over 100 years. All diagnoses and surgical procedures recorded during outpatient, inpatient, emergency room or nursing home visits, autopsy examinations, and death certificates are indexed, facilitating population-based studies. Annually, over 80% of the entire population is attended by one or both of these two practices, and 96% of local residents are seen at least once during any given four-year period (15). Because Mayo Clinic is the only institution in Olmsted County that offers the specialized testing required to diagnose DD, only Mayo Clinic patients who were Olmsted County residents were considered for review in this study.
Subjects and Review of Medical Records
All Olmsted County residents aged 16 years and older who were evaluated at Mayo Clinic between January 1, 1999 and December 31, 2008 and who received one of the following Hospital Adaptation of International Classification of Diseases (HICDA) codes, i.e., pelvic floor dysfunction (in men [07849250] and women [07859123]), functional constipation (05640112), anismus (05649314) or an ICD-9 code for irritable bowel syndrome (IBS) (564.1) were identified. Of the 11,112 patients residing in Olmsted County who had one or more of these diagnoses, 516 had undergone anal manometry. After excluding 4 patients who did not consent to review of their medical records for research, 512 patients (4.6%) were considered in this study. Additional anorectal tests in these 512 patients were as follows: barium (81 patients), magnetic resonance (25 patients), or scintigraphic defecography (55 patients), assessment of pelvic floor function with surface electromyography (EMG) (282 patients), and a balloon expulsion (BE) test (454 patients).
The medical records of all 245 subjects who satisfied the diagnostic criteria for a DD as discussed below were reviewed in detail. All information (i.e., demographic features, bowel symptoms, the results of diagnostic testing, medications, and any history of conditions that have been linked to DD) (14) was abstracted in a standardized manner and recorded on data collection forms. With one exception, only associated conditions that preceded the diagnosis of DD were considered in an attempt to identify conditions that were more likely causative for DD than consequences of the condition. Colonic and pelvic surgeries that were performed after the diagnosis of DD were also recorded. Height and weight were taken from the most recent data available adjacent to the date of diagnosis. The medical and surgical conditions documented in the medical records were diagnosed largely by specialists at Mayo Clinic. A gastroenterology trainee reviewed medical records to ensure that patients had symptoms of constipation, i.e., hard stools and/or infrequent evacuation for at least 6 months.
Assessment of Anorectal Function
Anorectal testing was conducted using established diagnostic techniques described previously. Anal resting and squeeze pressures were measured with water-perfused manometry in 47 patients (16) and high resolution anorectal manometry (ARM) in 465 patients, before and after December 2007, respectively (17). The external traction necessary to facilitate rectal expulsion of a 50 mL balloon filled with water, which is significantly correlated with the time required for BE in the seated position, was assessed (16, 18, 19). Impaired rectal evacuation was diagnosed by the need for ≥200 grams of external traction to facilitate rectal BE.
Additional tests (i.e., defecography and/or anal surface EMG) were generally performed when the anal manometry and rectal BE tests were inconclusive or incomplete (e.g, when latex allergy precluded assessment of rectal BE). Anal surface EMG activity at rest and during simulated evacuation was assessed with a Thought Technology Ltd (TTL) Rectal Sensor placed in the anal canal or a TTL Extension Surface Cable attached to the perianal surface via disposable electrodes (Thought Technology Ltd, Montreal, Quebec, Canada). These sensors were connected via cables to a U-Control sEMG 60Hz amplifier (Thought Technology Ltd, Montreal, Quebec, Canada). Paradoxical contraction was defined by an increase in EMG activity greater than 20% above the baseline value (11). Anorectal images were acquired at rest, during voluntary contraction, and evacuation of rectal contents with barium radiography, magnetic resonance, or scintigraphic defecography. During scintigraphic defecography, less than 72% rectal evacuation in 4 minutes was considered abnormal (20). For all techniques, perineal descent (PD) during simulated defecation of less than 1 cm or greater than 5 cm was considered abnormal.
Diagnosis of Defecatory Disorders
The diagnosis of DD was based on the clinical features and anorectal testing (5, 21). All patients had a history of constipation for >6 months, a documented clinical impression consistent with DD, and least one of the following three criteria:
An abnormal rectal BE test, which is very sensitive and specific for diagnosing DD (10, 11, 22).
Two or more of the following features: high anal resting pressure by manometry, i.e., greater than the 90th percentile value for healthy subjects (16, 17), paradoxical contraction on surface EMG during simulated defecation, or incomplete rectal evacuation during proctography. Because dyssynergia is frequently observed in healthy people, this was not used for diagnosing DD (23).
Reduced (<1 cm) or increased (>5 cm) perineal descent measured with proctography.
Statistical Analysis
Incidence rates (per 100,000 person-years) were calculated assuming the total Olmsted County population was at risk. Age-adjusted, sex-specific, and age- and sex-adjusted incidence rates were computed by direct adjustment to U.S. census data (U.S. White 2010), and 95% confidence intervals (CI) computed assuming a Poisson distribution. Poisson regression models were used to assess the association of incidence rates with age and sex. A potential calendar period effect was also examined in additional models based on age- and sex-specific crude rates for three separate time periods (1999–2002, 2003–2005, and 2006–2008) within the study interval. Fischer’s exact test was used to evaluate the association between sex and relevant clinical variables. All results are expressed as Mean±SD.
RESULTS
Diagnosis of defecatory disorders
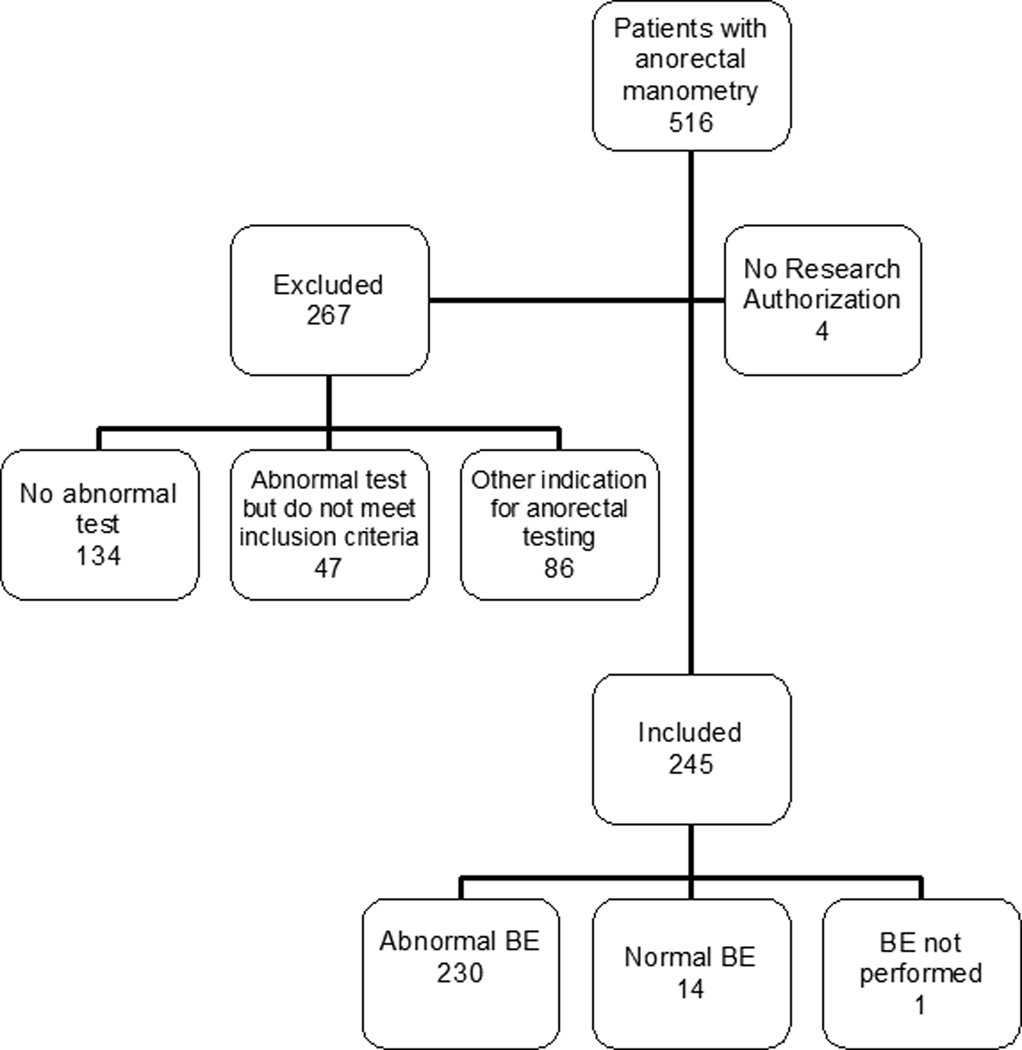
Between 1999 and 2008, 512 of 11,112 (4.6%) Olmsted County residents (446 women, 66 men) with constipation and who had undergone anorectal manometry were identified. This proportion increased from 3.6% between 1999 and 2002 to 5.4% between 2003 and 2005, but plateaued thereafter (i.e., 5.1% between 2006 and 2008). Of these 512 patients, 267 patients were excluded from further analysis because the anorectal manometry was indicated for a condition other than constipation (86 patients), because the anorectal tests were normal (134 patients), or because the tests were abnormal but did not satisfy the diagnostic criteria for DD (47 patients) (Figure 1). The remaining 245 patients (209 women, 36 men) had constipation and anorectal tests consistent with a defecatory disorder. The diagnosis was based on an abnormal BE test (230 patients), defecography alone (3 patients), defecography and anorectal manometry (6 patients), and defecography and surface EMG (5 patients). The mean (±SD) age at diagnosis was not significantly different between women (44±18 years) and men (49±19 years). Sixty-three of 245 patients (26%) had a body mass index (BMI) ≥30 kg/m2, and 25 patients (10%) had a BMI ≥35 kg/m2.
Figure 1. Study flow and results of diagnostic tests.
BE - balloon expulsion
Temporal trends in the incidence of defecatory disorders and the relationship to age and gender
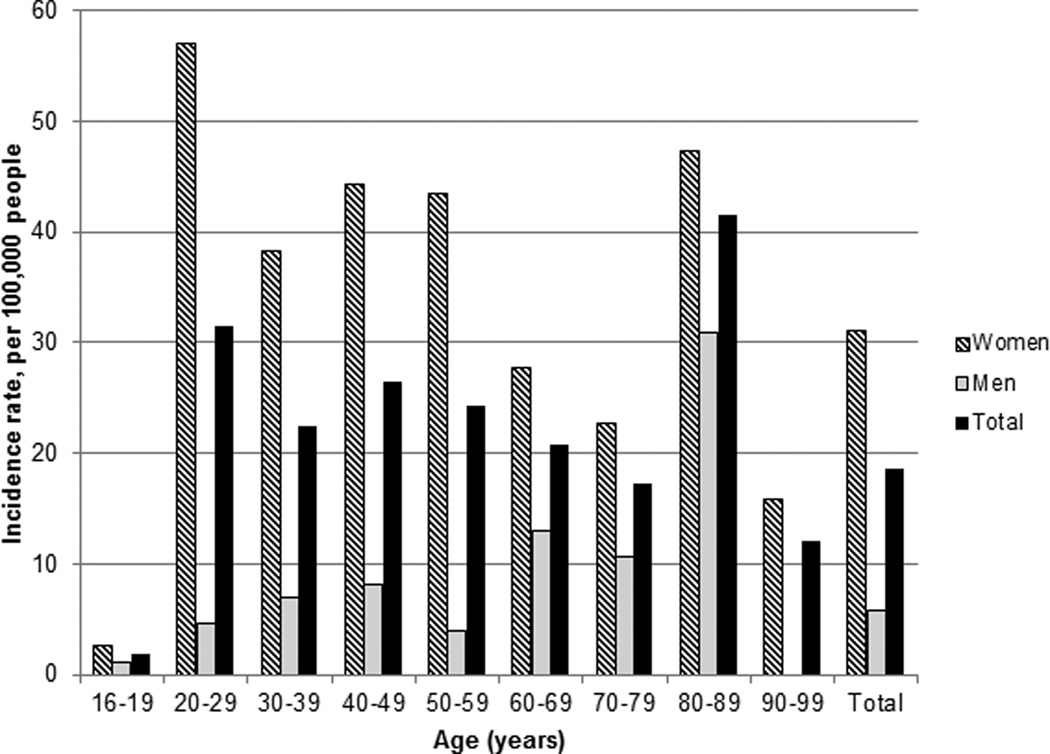
The overall age- and sex-adjusted (to the US white population in the year 2010) incidence rate per 100,000 person-years was 19.3 (95% CI, 16.8–21.8). The age-adjusted incidence per 100,000 person-years was greater (P<.0001) in women (31.8 [95% CI, 27.4–36.1]) than in men (6.6 [95% CI 4.4–8.9]). The incidence was associated with age in men (P=.002) and women (P=.0001). In women, the incidence was greatest (57 per 100,000) between the age of 20–29 years, then declined with a second peak between the age of 80–89 years (Figure 2). In men, the incidence was less than or around 10 per 100,000 person-years until the age of 80–89 years, where it increased to 30 per 100,000 person-years.
Figure 2. Distribution of the incidence rate of defecatory disorders by age and sex.
The age-adjusted incidence was greater (P<.0001) in women than men. The incidence was associated with age in men (P=.002) and women (P=.0001).
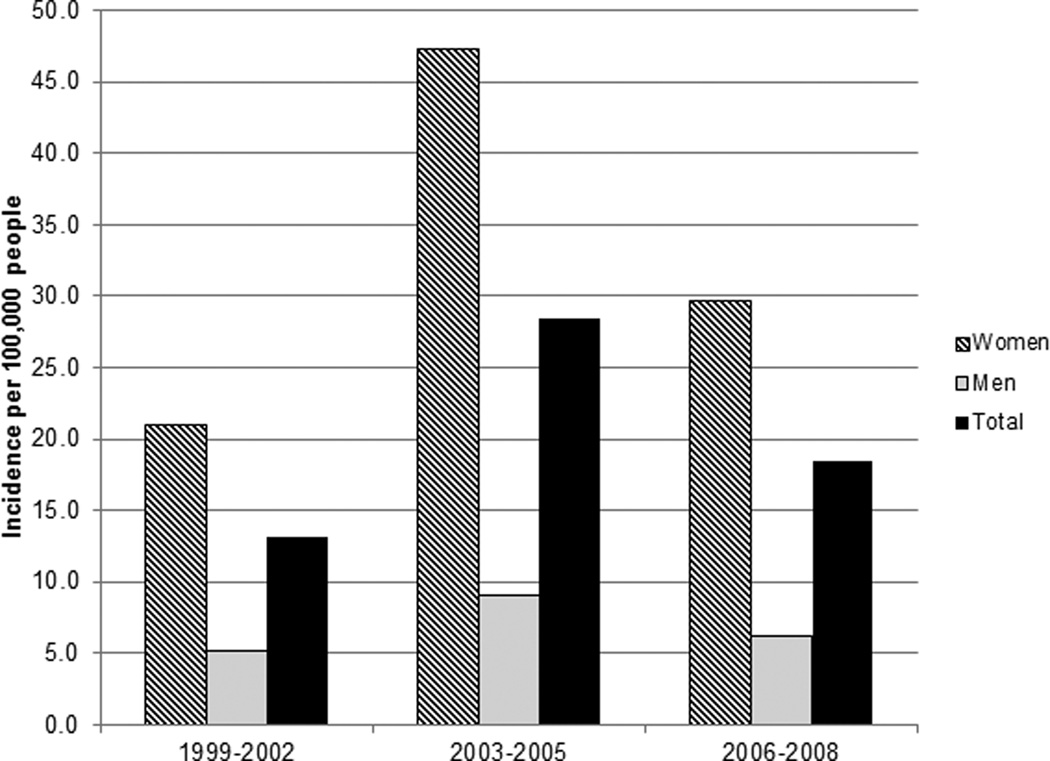
The incidence was also associated with calendar period in women (P<.0001) but not in men (P=.28) (Figure 3). In women, the overall incidence per 100,000 person-years increased from 21.0 between 1999 and 2002 to 47.4 between 2003 and 2005, but declined to 29.7 between 2006 and 2008.
Figure 3. Temporal trends in the incidence rate of defecatory disorders.
The incidence was associated with calendar period in women (P<.0001) but not in men (P=.28).
Associated medical conditions
Nearly 30% of patients had IBS, 48% had a prior psychiatric diagnosis, and 18% had shared with a physician that they had a history of abuse (Table 1). Neurological diseases were uncommon. Of the conditions, only a rectocoele was associated (P=.02) with sex, being more common in women (13%) than in men (0%). While depression and a history of abuse were more common in women, differences were not statistically significant.
Table 1.
Comparison of Clinical Features, Psychiatric Diseases, and Pelvic Surgeries in Olmsted County in Men and Women with Clinically Diagnosed Defecatory Disordersa, b
| Female (209) | Male (36) | Total (245) | P-value | |
|---|---|---|---|---|
| Age | 44 ± 18 | 49 ± 19 | 44 ± 18 | 0.078 |
| BMI | 26.7±6.0 | 28.8±6.0 | 27.0±6.0 | 0.060 |
|
Other gastroenterological and pelvic floor disorders |
||||
| Irritable bowel syndrome | 62 (30%) | 9 (25%) | 71 (29%) | 0.69 |
| Inflammatory bowel disease | 1 (0.5%) | 1 (3%) | 2 (0.8%) | 0.27 |
| Fecal incontinence | 21 (10%) | 4 (11%) | 25 (10%) | 0.77 |
| Rectocoele | 28 (13%) | 0 (0%) | 28 (11%) | 0.019 |
| Rectal prolapse | 5 (2%) | 0 (0%) | 5 (2%) | 1 |
| Enterocele | 5 (2%) | 0 (0%) | 5 (2%) | 1 |
| Cystocele | 18 (9%) | 0 (0%) | 18 (7%) | 0.084 |
| Urinary incontinence | 32 (15%) | 1 (3%) | 33 (13%) | 0.060 |
| Endometriosis | 13 (6%) | NA | ||
| Polycystic ovarian disease | 4 (2%) | NA | ||
| Neurological diseases | ||||
| Parkinson’s disease | 0 (0%) | 2 (6%) | 2 (0.8%) | 0.021 |
| Multiple sclerosis | 2 (1%) | 0 (0%) | 2 (0.8%) | 1 |
| Diabetes mellitus | 7 (3%) | 4 (11%) | 11 (4%) | 0.061 |
| Diabetic neuropathy | 2 (1%) | 2 (6%) | 4 (2%) | 0.104 |
| Psychiatric conditions | ||||
| Depression | 97 (46%) | 10 (28%) | 107 (44%) | 0.045 |
| Anxiety disorder | 36 (17%) | 6 (17%) | 42 (17%) | 1 |
| PTSD | 7 (3%) | 0 (0%) | 7 (3%) | 0.60 |
| Eating disorder | 15 (7%) | 0 (0%) | 15 (6%) | 0.14 |
| Any psychiatric diagnosis | 103 (49%) | 15 (42%) | 118 (48%) | 0.47 |
| Emotional abuse | 4 (2%) | 0 (0%) | 4 (2%) | 1 |
| Physical abuse | 7 (3%) | 2 (6%) | 9 (4%) | 0.62 |
| Sexual abuse | 8 (4%) | 1 (3%) | 9 (4%) | 1 |
| More than 1 type of abuse | 20 (10%) | 1 (3%) | 21 (8%) | 0.33 |
| Any abuse | 41 (20%) | 4 (11%) | 45 (18%) | 0.35 |
|
Gastrointestinal or pelvic surgeries |
||||
| Cholecystectomy | 20 (10%) | 3 (8%) | 23 (9%) | 1 |
| Appendectomy | 35 (17%) | 4 (11%) | 39 (16%) | 0.47 |
| Abdominal wall hernia repair | 9 (4%) | 1 (3%) | 10 (4%) | 1 |
| Surgery for pelvic organ prolapse |
29 (14%) | 1 (3%) | 30 (12%) | 0.093 |
| Partial colectomy | 5 (2%) | 3 (8%) | 8 (3%) | 0.097 |
| Total colectomy | 0 (0%) | 1 (3%) | 1 (0.4%) | 0.15 |
| Hysterectomy | 62 (30%) | NA | ||
| Abdominal | 42 (20%) | NA | ||
| Vaginal | 20 (10%) | NA | ||
Abbreviations: Body Mass Index (BMI); Post-Traumatic Stress Disorder (PTSD).
Variables expressed as percentages (numbers), or means ± standard deviations.
Only conditions that preceded the diagnosis of DD were considered here.
Obstetric history and other pelvic floor disorders
Prior to the diagnosis of a DD, 51 (21%) of 245 patients reported urinary incontinence (32 women and 1 man), and/or fecal incontinence (21 women and 4 men). Physical examination and/or imaging studies revealed pelvic organ prolapse (i.e., rectocele, rectal prolapse, enterocele, or cystocele) in 39 of 245 patients (16%), which affected one (25 [10%]) or more compartments (14 [6%]). Sixty-two (25%) had a hysterectomy, and 20 (12%) had undergone colonic or pelvic surgery for urinary incontinence, a cystocele, rectocele, or a colectomy. Only 2 patients had pelvic surgery after the diagnosis of DD.
One hundred thirty-one women (63%) had one or more children; 108 women (52%) had 2 or more children. The median number of children was 2 (0–8). Overall, 36% of females were nulliparous. All 5 females aged 16–19 years and 40 (78%) females aged 20–29 years were nulliparous.
Medications
At diagnosis, 168 patients (69%) were taking one or more medications that have been associated with constipation. Of these, 84 patients (34%) were taking a medication (i.e., calcium channel or adrenergic α2 blockers, calcium supplement, tricyclic antidepressants, or opioids) that is strongly implicated to cause constipation (Table 2). Of note, only 7% were taking opioids. One hundred and one patients (41%) were taking one or more medications for managing constipation, most frequently a fiber supplement, a stool softener, or an osmotic laxative (Table 2). There were no significant differences between the proportions of men and women who were taking medications.
Table 2.
Distribution of Medications in in Men and Women in Olmsted County with Clinically Diagnosed Defecatory Disorders
| Female (201) | Male (34) | Total (235) | P-value | |
|---|---|---|---|---|
| Thyroid hormone supplement | 24 (11%) | 2 (6%) | 26 (11%) | 0.39 |
| Antihypertensive (diuretics, ACE, adrenergic alpha or beta blockers, angiotensin receptor blockade) |
29 (14%) | 10 (28%) | 39 (16%) | 0.047 |
| Calcium channel blockers | 11 (5%) | 3 (8%) | 14 (6%) | 0.44 |
| Lipid lowering agents | 24 (11%) | 8 (22%) | 32 (13%) | 0.10 |
| Antihistamine | 34 (16%) | 7 (19%) | 41 (17%) | 0.63 |
| Calcium | 48 (23%) | 2 (6%) | 50 (20%) | 0.014 |
| Antidepressants | 107 (51%) | 17 (47%) | 124 (51%) | 0.72 |
| Tricyclic | 16 (8%) | 3 (8%) | 19 (8%) | 0.75 |
| Multiple or other | 16 (8%) | 2 (6%) | 18 (7%) | 1 |
| SSRI or SNRI | 87 (42%) | 14 (39%) | 101 (41%) | 0.86 |
| Antipsychotic | 12 (6%) | 4 (11%) | 16 (6%) | 0.27 |
| Non narcotic pain medications | 92 (44%) | 19 (53%) | 111 (45%) | 0.37 |
| Opioids | 15 (7%) | 3 (8%) | 18 (7%) | 0.73 |
| Medications for constipation | ||||
| Fiber supplement | 43 (21%) | 5 (14%) | 48 (20%) | 0.50 |
| Osmotic laxative (sorbitol, lactulose, PEG, MOM) |
30 (14%) | 4 (11%) | 34 (14%) | 0.80 |
| Stimulant laxative (1=Senna/sennosides) |
18 (9%) | 1 (3%) | 19 (8%) | 0.32 |
| Lubricant laxative (mineral oil) | 2 (1%) | 0 (0%) | 2 (0.8%) | 1 |
| Enema (1=fleet, 2=water) | 3 (1%) | 2 (6%) | 5 (2%) | 0.16 |
| Suppository (1=glycerin, 2=dulcolax, 3=NOS) |
9 (4%) | 2 (6%) | 11 (4%) | 0.67 |
| Stool softener (1=colace) | 34 (16%) | 2 (6%) | 36 (15%) | 0.125 |
| Lubiprostone | 1 (0.5%) | 0 (0%) | 1 (0.4%) | 1 |
| Tegaserod | 6 (3%) | 0 (0%) | 6 (2%) | 0.60 |
Abbreviations: ACE, angiotensin-converting enzyme; MOM, Milk of Magnesia; NOS, not otherwise specified; PEG, polyethylene glycol; SNRI, serotonin and norepinephrine reuptake inhibitors; SSRI, selective serotonin reuptake inhibitors;
DISCUSSION
In this study, the age- and sex-adjusted incidence rate per 100,000 person-years for clinically diagnosed DD among adults in Olmsted County was 19.3, which is greater than the corresponding incidence rate of Crohn’s disease (i.e., 5.8 between 1940 and 1993) but less than the incidence of clinically diagnosed IBS (i.e., 196 between 1991 and 1993) (24, 25). In the latter study, which was conducted during a different time period, constipation was the presenting symptom in approximately 16% of patients, which approximates to an incidence rate of 31 per 100,000 person-years. Allowing for differences in the time period and methods between the prior study in IBS and the present study, a crude comparison suggests that a substantial proportion of patients with constipation have a DD. Because the medical records of only fraction of 11,112 patients were reviewed, we cannot assess what proportion had symptom criteria for constipation. Nonetheless, only approximately 5% of patients had undergone anorectal manometry, which suggests that the observed incidence of DD in this study may be conservative.
Similar to a prior cohort (14), the incidence of DD was much more common, indeed 4-fold higher, in women than in men (32 versus 7 per 100,000). By contrast, between 1988 and 2003 the incidence of symptoms of functional constipation was only two-fold greater in women than in men in Olmsted County (26). Hence, the greater incidence in women cannot be entirely explained by a higher incidence of symptoms of functional constipation in women than in men. Why DD are more common in women than in men is unclear. In this study, the peak incidence of diagnosis of DD was in women aged 20–29 years; 78% of these women and 36% of the overall cohort were nulliparous, which does not support a predominant role for obstetric pelvic floor injury in DD. Likewise, a case-control study observed that obstetric risk factors were not associated with DD, and that hysterectomy was associated with a borderline increased risk (odds ratio 3.9, 95% CI, 1.0–15.6) (27). At the other extreme, a DD was diagnosed in the 7th decade and thereafter in many men and women. Indeed in men, the peak incidence of diagnosis of DD was in the 9th decade. Another possible explanation is that DD result from excessive straining in children with constipation. In this study, the age of onset of constipation could not be reliably obtained from the records. In the largest cohort of patients with DD, 37% of patients reported that their symptoms dated back to childhood (14). A long-term longitudinal assessment reported that 30% of 418 children with constipation who sought medical attention had symptoms beyond the age of 16 years (28). However, by contrast to our cohort, 67% of constipated children in the latter study were boys. Thus, a population-based, case-control study with a careful review of obstetric and surgical records is necessary to determine the contribution of these risk factors to DD (29).
Temporal trends in the incidence of diagnosis of DD were statistically significant in women but not in men. Among women, the incidence of DD increased substantially in 2003–2005 compared to 1999–2002, but declined thereafter. Conceivably, this increase during 2003–2005 is at least partly explained by increased recognition of the condition and utilization of anorectal testing. Indeed, the proportion of constipated patients who underwent anorectal manometry increased from 3.8% between 1999 and 2002 to 5.8% between 2003 and 2005, but plateaued thereafter (i.e., 5.3% between 2006 and 2008).
Nearly 50% of patients had a psychiatric diagnosis, over 40% of patients had depression, and 51% were taking an antidepressant. The proportion of patients with a psychiatric diagnosis is lower than the prevalence in our tertiary practice (65%) (13) but similar to or lower than the prevalence of depression in functional constipation in other studies (30, 31). Also, 18% of patients reported a history of abuse, as documented in the clinical records, which is lower than the prevalence (i.e., 31% for physical abuse and 22% for sexual abuse) ascertained with a questionnaire in a cohort of patients with DD (14). Nearly one quarter of patients also had fecal and/or urinary incontinence, and 12% had pelvic floor surgery before the diagnosis of DD. The overlap between DD and fecal incontinence (32–34) and separately with pelvic floor pelvic organ prolapse has been described (16). The prevalence of obesity (26%) in this cohort is comparable to that in this community (personal communication, Dr. Kent Bailey, Mayo Clinic).
From a public health perspective, these findings have two major implications. First, because DD are better managed with pelvic floor biofeedback therapy rather than laxatives, they reinforce the need for anorectal testing, as emphasized in recent guidelines (35, 36). While high resolution anorectal manometry requires considerable expertise, a portable manometry device and the rectal balloon expulsion test may facilitate access to anorectal testing in the community (11, 37). Second, the high prevalence of psychological disturbances reinforces the need for managing the condition with multi-disciplinary approaches rather than with biofeedback therapy alone.
To our knowledge this is the first study to estimate the incidence rate and clinical features of clinically diagnosed DD in the community. Mayo Clinic is the primary care provider for a majority of residents in Olmsted County, reducing the potential for referral bias. The diagnosis of DD was based on rigorous criteria and a review of the complete medical records. However, there are several limitations, in addition to those discussed above. The findings are representative of a white population but may be generalizable to other populations. Symptom assessment was based on a review of medical records rather than a systematic questionnaire. However, a priori, it seems likely that patients referred for anorectal testing had clinically significant constipation. Because only a small proportion of constipated patients in Olmsted County had anorectal testing, these findings may be conservative and underestimate the actual incidence of DD in the community. The prevalence of associated conditions, particularly obstetric pelvic floor injury and sensitive issues (e.g., abuse), may also be underestimated because detailed obstetric records were not available and a questionnaire was not administered. The association between joint hypermobility and DD was not evaluated (38).
In conclusion, the age- and sex-adjusted incidence rate of clinically diagnosed DD in a community was 19.3 per 100,000 person-years, which is approximately 3-fold greater than the prevalence of Crohn’s disease in the same community. The incidence of DD was 5-fold higher in women than in men. Nearly 50% of patients had a psychiatric diagnosis, and over 40% of patients had depression. Among women, the incidence of DD increased substantially in 2003–2005 compared to 1999–2002, but declined thereafter. Taken together, these findings reinforce the recommendation to consider anorectal testing in patients with chronic constipation refractory to simple laxatives (1, 35).
KEY POINTS.
This study evaluated the epidemiology of defecatory disorders (DD) in the population, which is currently unknown.
The overall age and sex adjusted incidence rate of defecatory disorders (DD) in Olmsted County between 1999 and 2008 was 19.3 per 100,000 person-years (95% CI, 16.8–21.8).
DD are relatively common in the community; the incidence of diagnosis of DD is greater than Crohn’s disease. DD are more common in women, and are frequently associated with psychiatric conditions and IBS.
Acknowledgments
The authors would like to thank Barbara Abbott and Pauline Funk for excellent assistance with data retrieval and Ms. Kristi Simmons for superb editorial support.
Funding: This study was supported by USPHS NIH Grant R01 DK078924, and also by Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Disclosures
Competing Interests: The authors have no competing interests.
Contributions
Jessica Noelting. Chart review, writing and editing of the manuscript
John Eaton. Study design, chart review, writing and editing of the manuscript.
Rok Seon Choung. Study design and editing manuscript.
Alan Zinsmeister. Statistical analysis and editing the manuscript.
G Richard Locke III. Study design, writing and editing of the manuscript.
Adil Bharucha. Study design, case adjudication, writing and editing of the manuscript.
REFERENCES
- 1.Bharucha AE, Pemberton JH, Locke GR., 3rd American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144:218–238. doi: 10.1053/j.gastro.2012.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Surrenti E, Rath DM, Pemberton JH, Camilleri M. Audit of constipation in a tertiary referral gastroenterology practice. Am J Gastroenterol. 1995;90:1471–1475. [PubMed] [Google Scholar]
- 3.Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology. 2006;130:1510–1518. doi: 10.1053/j.gastro.2005.11.064. [DOI] [PubMed] [Google Scholar]
- 4.Iantorno G, Cinquetti M, Mazzocchi A, Morelli A, Bassotti G. Audit of constipation in a gastroenterology referral center. Dig Dis Sci. 2007;52:317–320. doi: 10.1007/s10620-006-9486-5. [DOI] [PubMed] [Google Scholar]
- 5.Rao SS. Advances in diagnostic assessment of fecal incontinence and dyssynergic defecation. Clin Gastroenterol Hepatol. 2010;8:910–919. doi: 10.1016/j.cgh.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130:657–664. doi: 10.1053/j.gastro.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 7.Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized Controlled Trial Shows Biofeedback to be Superior to Pelvic Floor Exercises for Fecal Incontinence. Dis Colon Rectum. 2009;52:1730–1737. doi: 10.1007/DCR.0b013e3181b55455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rao SS, Valestin J, Brown CK, Zimmerman B, Schulze K. Long-term efficacy of biofeedback therapy for dyssynergic defecation: randomized controlled trial. Am J Gastroenterol. 2010;105:890–896. doi: 10.1038/ajg.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talley NJ, Weaver AL, Zinsmeister AR, Melton LJ., 3rd Functional constipation and outlet delay: a population-based study. Gastroenterology. 1993;105:781–790. doi: 10.1016/0016-5085(93)90896-k. [DOI] [PubMed] [Google Scholar]
- 10.Ratuapli SK, Bharucha AE, Noelting J, Harvey DM, Zinsmeister AR. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology. 2013;144:314–322. e312. doi: 10.1053/j.gastro.2012.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiarioni G, Kim SM, Vantini I, Whitehead WE. Validation of the balloon evacuation test: reproducibility and agreement with findings from anorectal manometry and electromyography. Clin Gastroenterol Hepatol. 2014;12:2049–2054. doi: 10.1016/j.cgh.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Bharucha AE, Rao SSC. An update on anorectal disorders for gastroenterologists. Gastroenterology. 2014;146:37–45. e32. doi: 10.1053/j.gastro.2013.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nehra V, Bruce BK, Rath-Harvey DM, Pemberton JH, Camilleri M. Psychological disorders in patients with evacuation disorders and constipation in a tertiary practice. Am J Gastroenterol. 2000;95:1755–1758. doi: 10.1111/j.1572-0241.2000.02184.x. [DOI] [PubMed] [Google Scholar]
- 14.Rao SS, Tuteja AK, Vellema T, Kempf J, Stessman M. Dyssynergic defecation: demographics, symptoms, stool patterns, and quality of life. J Clin Gastroenterol. 2004;38:680–685. doi: 10.1097/01.mcg.0000135929.78074.8c. [DOI] [PubMed] [Google Scholar]
- 15.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 16.Bharucha AE, Fletcher JG, Seide B, Riederer SJ, Zinsmeister AR. Phenotypic variation in functional disorders of defecation. Gastroenterology. 2005;128:1199–1210. doi: 10.1053/j.gastro.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 17.Noelting J, Ratuapli SK, Bharucha AE, Harvey DM, Ravi K, Zinsmeister AR. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol. 2012;107:1530–1536. doi: 10.1038/ajg.2012.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bharucha AE, Seide B, Fox JC, Zinsmeister AR. Day-to-day reproducibility of anorectal sensorimotor assessments in healthy subjects. Neurogastroenterol Motil. 2004;16:241–250. doi: 10.1111/j.1365-2982.2004.00499.x. [DOI] [PubMed] [Google Scholar]
- 19.Ratuapli S, Bharucha AE, Harvey D, Zinsmeister AR. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterol Motil. 2013;25:e813–e820. doi: 10.1111/nmo.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pezim ME, Pemberton JH, Levin KE, Litchy WJ, Phillips SF. Parameters of anorectal and colonic motility in health and in severe constipation. Dis Colon Rectum. 1993;36:484–491. doi: 10.1007/BF02050015. [DOI] [PubMed] [Google Scholar]
- 21.Bharucha AE. Difficult defecation: difficult problem assessment and management; what really helps? Gastroenterol Clin North Am. 2011;40:837–844. doi: 10.1016/j.gtc.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Minguez M, Herreros B, Sanchiz V, et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology. 2004;126:57–62. doi: 10.1053/j.gastro.2003.10.044. [DOI] [PubMed] [Google Scholar]
- 23.Grossi U, Carrington EV, Bharucha AE, Horrocks EJ, Scott SM, Knowles CH. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut. 2015 doi: 10.1136/gutjnl-2014-308835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loftus EV, Jr, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Crohn's disease in Olmsted County, Minnesota, 1940–1993: incidence, prevalence, and survival. Gastroenterology. 1998;114:1161–1168. doi: 10.1016/s0016-5085(98)70421-4. [DOI] [PubMed] [Google Scholar]
- 25.Locke GR, 3rd, Yawn BP, Wollan PC, Melton LJ, 3rd, Lydick E, Talley NJ. Incidence of a clinical diagnosis of the irritable bowel syndrome in a United States population. Aliment Pharmacol Ther. 2004;19:1025–1031. doi: 10.1111/j.1365-2036.2004.01938.x. [DOI] [PubMed] [Google Scholar]
- 26.Choung RS, Locke GR, 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Cumulative incidence of chronic constipation: a population-based study 1988–2003. Aliment Pharmacol Ther. 2007;26:1521–1528. doi: 10.1111/j.1365-2036.2007.03540.x. [DOI] [PubMed] [Google Scholar]
- 27.Klingele CJ, Bharucha AE, Fletcher JG, Gebhart JB, Riederer SG, Zinsmeister AR. Pelvic organ prolapse in defecatory disorders. Obstet Gynecol. 2005;106:315–320. doi: 10.1097/01.AOG.0000171104.72972.34. [DOI] [PubMed] [Google Scholar]
- 28.van Ginkel R, Reitsma JB, Buller HA, van Wijk MP, Taminiau JA, Benninga MA. Childhood constipation: longitudinal follow-up beyond puberty. Gastroenterology. 2003;125:357–363. doi: 10.1016/s0016-5085(03)00888-6. [DOI] [PubMed] [Google Scholar]
- 29.Bharucha AE, Zinsmeister AR, Schleck CD, Melton LJ., 3rd Bowel disturbances are the most important risk factors for late onset fecal incontinence: a population-based case-control study in women. Gastroenterology. 2010;139:1559–1566. doi: 10.1053/j.gastro.2010.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Whitehead WE, Palsson OS, Levy RR, Feld AD, Turner M, Von Korff M. Comorbidity in irritable bowel syndrome. Am J Gastroenterol. 2007;102:2767–2776. doi: 10.1111/j.1572-0241.2007.01540.x. [DOI] [PubMed] [Google Scholar]
- 31.Bouchoucha M, Hejnar M, Devroede G, Boubaya M, Bon C, Benamouzig R. Patients with irritable bowel syndrome and constipation are more depressed than patients with functional constipation. Dig Liver Dis. 2014;46:213–218. doi: 10.1016/j.dld.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 32.Rao SS, Ozturk R, Stessman M. Investigation of the pathophysiology of fecal seepage. Am J Gastroenterol. 2004;99:2204–2209. doi: 10.1111/j.1572-0241.2004.40387.x. [DOI] [PubMed] [Google Scholar]
- 33.Bharucha AE, Fletcher JG, Harper CM, et al. Relationship between symptoms and disordered continence mechanisms in women with idiopathic fecal incontinence. Gut. 2005;54:546–555. doi: 10.1136/gut.2004.047696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burgell RE, Bhan C, Lunniss PJ, Scott SM. Fecal incontinence in men: coexistent constipation and impact of rectal hyposensitivity. Dis Colon Rectum. 2012;55:18–25. doi: 10.1097/DCR.0b013e318237f37d. [DOI] [PubMed] [Google Scholar]
- 35.Bharucha AE, Locke GR, Pemberton JH. AGA Practice Guideline on Constipation: Technical Review. Gastroenterology. 2013;144:218–238. doi: 10.1053/j.gastro.2012.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Gastroenterological A. Bharucha AE, Dorn SD, Lembo A, Pressman A. American gastroenterological association medical position statement on constipation. Gastroenterology. 2013;144:211–217. doi: 10.1053/j.gastro.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 37.Bharucha AE, Stroetz R, Feuerhak K, Szarka LA, Zinsmeister AR. A novel technique for bedside anorectal manometry in humans. Neurogastroenterol Motil. 2015;27:1504–1508. doi: 10.1111/nmo.12636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mohammed SD, Lunniss PJ, Zarate N, et al. Joint hypermobility and rectal evacuatory dysfunction: an etiological link in abnormal connective tissue? Neurogastroenterol Motil. 2010;22:e1085–e1283. doi: 10.1111/j.1365-2982.2010.01562.x. [DOI] [PubMed] [Google Scholar]