Abstract
Objectives
To examine trends and correlates of cannabis-involved emergency department (ED) visits in the United States from 2004 to 2011.
Methods
Data were obtained from the 2004-2011 Drug Abuse Warning Network. We analyzed trend in cannabis-involved ED visits for persons aged ≥12 years and stratified by type of cannabis involvement (cannabis-only, cannabis-polydrug). We used logistic regressions to determine correlates of cannabis-involved hospitalization versus cannabis-involved ED visits only.
Results
Between 2004 and 2011, the ED visit rate increased from 51 to 73 visits per 100,000 population aged ≥ 12 years for cannabis-only use (P-value for trend=0.004) and from 63 to 100 for cannabis-polydrug use (P-value for trend<0.001). Adolescents aged 12-17 years showed the largest increase in the cannabis-only-involved ED visit rate (Rate difference=80 per 100,000 adolescents). Across racial/ethnic groups, the most prevalent ED visits were noted among non-Hispanic blacks. Among cannabis-involved visits, the odds of hospitalization (versus ED visits only) increased with age strata compared with aged 12-17 years.
Conclusions
These findings suggest a notable increase in the ED visit numbers and rates for both the use of cannabis-only and cannabis-polydrug during the studied period, particularly among young people and non-Hispanic blacks.
Keywords: Cannabis, polydrug, emergency department, hospitalization
1. Introduction
The continued spread of decriminalization or medical cannabis use laws in many states as well as a rising cannabis use prevalence noted from the population-based surveys have drawn growing concerns about cannabis use’s potential adverse effects on health (e.g., addiction), which may trigger a wide range of unintended consequences (Substance Abuse and Mental Health Services Administration [SAMHSA], 2015a; Volkow et al., 2014). According to estimates from the 2014 National Survey on Drug Use and Health (NSDUH), 13.2% of persons aged ≥12 years (35 million) used cannabis in the past year, which increased by 2.6% (9.7 million) since 2004 (SAMHSA, 2015a). Nationally, an estimated 4 million of persons aged ≥12 years had a cannabis use disorder (CUD) in the past year (SAMHSA, 2015a). Among past-year cannabis users aged ≥12 years, 15% or more than 1 in 7 cannabis users were found to meet criteria for a CUD – an indicator of problem cannabis use or dependence that warrants intervention to reduce adverse effects (Wu et al., 2014). There has been an increased number of studies that examined cannabis use prevalence trends; however, the potential impact of cannabis use on healthcare utilization over time has not been adequately investigated (French et al., 2011; Hasin et al., 2015). This study used the national dataset to determine the national trend in cannabis-specific emergency department (ED) visits and hospitalization in order to better inform cannabis-involved healthcare utilization and to identify demographic groups disproportionally affected by cannabis-involved healthcare utilization.
Chronic or heavy cannabis use was associated with poor educational outcome and a wide range of health-related concerns, such as cognitive impairment, cannabis-impaired car accidents, addiction, symptoms of bronchitis, psychotic symptoms, depression, lung cancer, and reproductive health problems (Hall, 2015; Volkow et al., 2014). The latter may result in acute events or intensify existing medical conditions that are related to ED admissions. It was estimated that chronic drug use increased the probability of using ED for medical care by more than 30 percent (McGeary and French, 2000). Cannabis use may impair motor coordination and reaction times and interfere with driving performance (Volkow et al., 2014). A meta-analysis found that driving under the influence of cannabis use was associated with increased odds of motor vehicle collisions compared with unimpaired driving (Odds Ratio 1.92, 95% Confidence Interval (CI) 1.35-2.73) (Asbridge et al., 2012).
Despite continued concerns about cannabis use’s adverse effects on health and their related impact on healthcare utilization (Volkow et al., 2014), there is very limited information about cannabis-specific ED admission and subsequent hospitalization. Previously, Perron et al. (2011) found that 1.7% of lifetime adult cannabis users reported an ED visit. In a study of a national sample, Wu et al. (2012) estimated that 12.1% of adults nationally who sought medical care in ED used cannabis in the past year compared with 9.7% of adults who received care in ED. However, these self-report drug use and ED treatment data from surveys provide inadequate information to inform cannabis-involved treatment visits to determine the potential effects of cannabis use on ED admissions. Therefore, national-level datasets that include cannabis-involved ED admissions are needed. The Drug Abuse Warning Network (DAWN) specifically collected data on drug-involved ED visits (either a direct cause or contributor for the visits), hence the DAWN data can improve the study of associations between problem cannabis use and cannabis-involved ED and hospitalization (Center for Behavioral Health Statistics and Quality [CBHSQ], 2013).
Cannabis use was associated with sex, age, and race/ethnicity (Wu et al., 2012, 2014). Males in general were more likely than females to use cannabis and have a CUD (Wu et al., 2014). Adolescence is in the critical stage of brain development, and early and frequent cannabis use was associated with altered brain development (e.g., impairment in brain functional connectivity), which could increase adolescent users’ vulnerability to cannabis’s long-term effects on addiction, other psychiatric conditions, or cognitive impairment (Rubino et al., 2012; Volkow et al., 2014). Nationally, about 13% of adolescents used cannabis in the past year (Wu et al., 2014). Although past-year cannabis use was most common among adults aged 18-25 (29%), adolescent cannabis users were more likely than adult cannabis users to meet criteria for a CUD in the past year (Wu et al., 2014). Among U.S. high school seniors, the likelihood of unsafe driving was positively associated with substance use frequency, especially concurrent use of alcohol and cannabis (Terry-McElrath et al., 2014).
Nationally, approximately 13% of blacks aged ≥ 12 years used cannabis in the past year compared with 11% of whites and 9% of Hispanics (Wu et al., 2014). Recent data estimated that black adolescents were about 68% more likely than white adolescents to have used cannabis and 34% more likely to have a CUD in the past year (Wu et al., 2015). These findings point towards the need to determine whether the number of cannabis-involved ED admissions was associated with sex, age, and race/ethnicity (i.e., increases among males, adolescents, or blacks). Besides demographic variables, polydrug use may intensify adverse effects of drug use and increase treatment admissions (Dean, 2006; CBHSQ, 2012). Based on prior DAWN data, 73% of ED visits involving cannabis also included other drug(s) in 2009 (CBHSQ, 2012). Because of the cost and challenges of conducting the study in ED settings to determine substance-specific ED admissions, this study capitalizes on existing datasets to examine cannabis-involved ED visits and hospitalization.
We compare use of cannabis only with use of cannabis and other drug(s) (cannabis-polydrug) to better understand the trend and patterns of cannabis-involved healthcare use (including subsequent hospitalization). We determine the national trends in cannabis-involved ED visits, stratified by cannabis and other drug use status (cannabis-only, cannabis-polydrug); quantify demographic patterns in cannabis-involved ED visits (age, sex, race/ethnicity); determine specific drugs commonly identified among cannabis-involved ED visits; and conduct adjusted analyses to identify correlates of cannabis-involved hospitalization versus cannabis-involved ED visit only. To our knowledge, this study is among the first to specifically examine the pattern of cannabis-involve ED visits and subsequent hospitalizations. Results will have timely clinical implications for informing demographic groups impacted by cannabis-involved hospitalizations.
2. Methods
2.1. Data source
Data were obtained from public-use datasets of the 2004-2011 Drug Abuse Warning Network (DAWN) (CBHSQ, 2013; SAMHSA, 2015c). DAWN is the only national representative surveillance system designed to monitor the trends in drug abuse and misuse involved hospital ED visits and subsequent hospitalizations (CBHSQ, 2013). The 2004-2011 DAWN used a stratified simple random sample of the non-Federal, short-stay, general surgical and medical hospitals with at least one 24-hour ED in the United States. DAWN provides a drug reference vocabulary (DRV), which can be used to identify specific illicit drug use and combinations among illicit drugs, non-medical prescription drugs, and alcohol. The most recent data of DAWN was from 2004 to 2011 due to the redesigned survey methodology in 2003, and it can be used to estimate the trends in the specific drug for the nation and selected metropolitan areas (CBHSQ, 2013).
The observation unit of DAWN data is an ED visit involving recent drug use (or alcohol only for patients younger than 21 years), and drug use can be a direct cause or contributor for the visits (CBHSQ, 2013). These substance-involved ED visits were identified and collected by trained DAWN reporters through reviewing the medical records of patients, and one visit may report multiple substance use (up to 16). This study focused on a subsample of cannabis-involved ED visits for admitted patients aged ≥12 years. In the final sample, the weighted number of ED visits were 2,823,321 from 2004 to 2011, and 41.1% (1,160,556) of them were related to cannabis-only and 58.9% (1,662,765) related to a combination of cannabis and other drug(s). The use of DAWN dataset was determined to be exempt from review by the institutional review board of Duke University Health System.
2.2. Study variables
A cannabis-involved ED visit was defined as any ED visit involving cannabis use for all-listed drug reported, and one patient may have several visits recorded by a number of visits. Based on the presence of cannabis and other drug(s), we categorized cannabis involvement into two categories: 1) cannabis-only (cannabis was the only drug identified); 2) cannabis-polydrug (cannabis plus one or more other illicit drugs or pharmaceuticals).
Other illicit drugs or pharmaceuticals included cocaine, heroin, stimulants (methamphetamine/amphetamine), hallucinogens (Ecstasy, phencyclidine, d-lysergic acid diethylamide, and miscellaneous hallucinogens), opiates/opioids, and sedatives/benzodiazepines.
Demographic characteristics of patients in the DAWN dataset included age (12-17, 18-20, 21-24, 25-29, 30-34, 35-44, 45-64, and 65 or older), sex (male and female), and race/ethnicity (Non-Hispanic white, Non-Hispanic black, Hispanic or Latino, and other races). Other races consisted of American Indian, Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, or mixed race/ethnicities (CBHSQ, 2013).
DAWN assigned a unique case type to each ED visit in order to analyze the similar admission reasons. The admission case types included seeking detoxification, suicide attempt, problem drug use (adverse reaction, overmedication, accidental ingestion and malicious poisoning) and other admission reasons.
2.3. Statistical analysis
We first described the trends in the annual number and rate of cannabis-involved ED visits, stratified by type of cannabis involvement (cannabis-only and cannabis-polydrug) and demographics. The ED visit rate for each type of cannabis involvement was computed by the number of relevant ED visits divided by the total number of resident population aged≥12 years from the US Census Bureau (CBHSQ, 2013). The ED visit rate for each demographic group was calculated by the number of relevant ED visits divided by the number of resident population for corresponding group. P-value for trend was estimated from univariate linear regression between the variable of interest and year. Finally, multiple logistic regression analyses were used to estimate associations between demographic factors and type of cannabis involvement, as well as to determine factors associated with hospitalization vs. ED only visits. All analyses took into account DAWN’s complex survey designs by using Stata 13.0 (StataCorp, 2013). All results are weighted figures.
3. Results
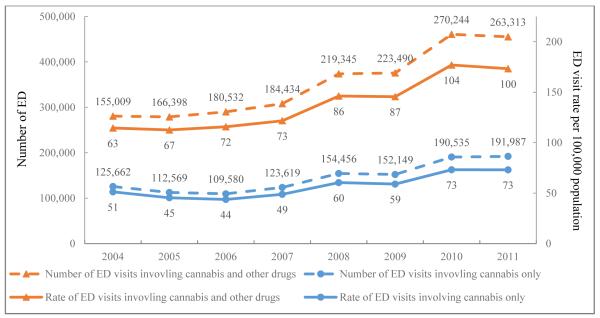
3.1. Trend in cannabis-involved ED visits (Figure 1)
Figure 1. The estimated number and rate per 100,000 population aged ≥12 years of cannabis-involved ED visits, 2004-2011 DAWN: cannabis-only vs. cannabis-polydrug admissions.
All numbers are weighted estimates, and the rate was defined as a weighted estimate of the ED visit number divided by 100,000 population aged ≥12 years.
Overall, both the annual number and rate of cannabis-involved ED visits showed a significantly increasing trend from 2004 to 2011. The rate of ED visits involving cannabis-only increased by 43% from 51 per 100,000 population aged ≥12 years in 2004 to 73 in 2011 (P-value for trend=0.004). The rate of ED visits involving cannabis-polydrug increased 59% from 63 per 100,000 population aged ≥12 years in 2004 to 100 per 100,000 population in 2011 (P-value for trend<0.001). Cannabis-polydrug had a higher number and rate of ED visits than cannabis-only each year. Among cannabis-involved ED visits, the presentation of alcohol has been stable over time (Table S1 in Supplemental Material).
3.2. Demographic trends in cannabis-involved ED visits (Table 1)
Table 1.
The estimated cannabis-involved ED visit ratea by demographic characteristics and type of cannabis involvement, 2004-2011 DAWN
| Cannabis-only admissions | Cannabis-polydrug admissions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| 2004 | 2011 | Average rate (04-11) |
Rate Difference (11 vs. 04) |
P-value for trend |
2004 | 2011 | Average rate (04-11) |
Rate Difference (11 vs. 04) |
P-value for trend |
|
| ED visits | 51 | 73 | 57 | 22 | 0.004 | 63 | 100 | 81 | 37 | <0.001 |
| Age in years | ||||||||||
| 12-17 | 79 | 159 | 111 | 80 | 0.004 | 75 | 81 | 75 | 6 | 0.109 |
| 18-20 | 164 | 226 | 190 | 63 | 0.009 | 130 | 218 | 205 | 87 | 0.007 |
| 21-24 | 123 | 172 | 135 | 49 | 0.009 | 134 | 275 | 196 | 141 | <0.001 |
| 25-29 | 92 | 114 | 99 | 21 | 0.009 | 126 | 206 | 158 | 80 | <0.001 |
| 30-34 | 75 | 95 | 68 | 20 | 0.111 | 107 | 160 | 130 | 53 | 0.011 |
| 35-44 | 43 | 55 | 44 | 12 | 0.079 | 77 | 111 | 94 | 35 | <0.001 |
| 45-64 | 17 | 29 | 20 | 12 | 0.008 | 24 | 51 | 38 | 27 | <0.001 |
| 65+ | 1 | 3 | 2 | 2 | 0.038 | - | - | - | - | - |
| Sex | ||||||||||
| Male | 79 | 96 | 81 | 17 | 0.024 | 82 | 136 | 107 | 54 | <0.001 |
| Female | 25 | 51 | 34 | 26 | <0.001 | 45 | 66 | 57 | 21 | <0.001 |
| Race/ethnicity | ||||||||||
| White, non-Hispanic | 30 | 51 | 41 | 22 | 0.001 | 51 | 93 | 72 | 43 | <0.001 |
| Black, non-Hispanic | 120 | 185 | 132 | 65 | 0.013 | 114 | 200 | 161 | 87 | 0.004 |
| Hispanic or Latino | 80 | 67 | 53 | −13 | 0.786 | 43 | 57 | 50 | 13 | 0.019 |
| Other races | 15 | 23 | 12 | 8 | 0.133 | - | 16 | 11 | - | - |
The rate was the number of ED visits per 100,000 subgroup population, and it was calculated by a weighted estimate of the ED visit number divided by the number of the population in the corresponding group.
Results are weighted estimates.
A dash (-) indicated an estimated with a relative standard error (RSE) greater than 50% or an estimated based on fewer than 30 visits.
Between 2004 and 2011, the cannabis-only ED visit rate for adolescents increased from 79 to 159 per 100,000 aged 12-17 years (Rate difference=80; P-value for trend=0.004), and the cannabis-polydrug ED visit rate for young adults aged 21-24 years increased from 134 to 275 per 100,000 aged 21-24 years (Rate difference=141; P-value for trend<0.001). Both showed an increase among all age groups. Non-Hispanic blacks had the highest increase in the ED visit rate, an increase by 65 ED visits per 100,000 blacks for cannabis-only from 2004 to 2011 (P-value for trend=0.013) and 87 for cannabis-polydrug (P-value for trend=0.004), and the increases over doubled those of non-Hispanic whites.
3.3. Characteristics of cannabis-involved ED visits (Table 2)
Table 2.
Characteristics of cannabis-involved ED visits by type of cannabis involvement, 2004-2011 DAWN
| Characteristics | Cannabis-only admission (N=1,160,556)a |
Cannabis-polydrug admissions (N=1,662,765)a |
AOR of Cannabis- polydrug vs. cannabis- only admissions |
|---|---|---|---|
|
|
|||
| Column % | Column % | AOR (95%CI)b | |
| Age in years | |||
| 12-17 | 19.63 | 9.22 | Ref. |
| 18-20 | 17.26 | 13.02 | 1.56 (1.33-1.83) |
| 21-24 | 15.82 | 16.05 | 2.12 (1.75-2.58) |
| 25-29 | 13.96 | 15.69 | 2.26 (1.85-2.76) |
| 30-34 | 9.29 | 12.40 | 2.76 (2.25-3.38) |
| 35-44 | 12.93 | 19.01 | 3.02 (2.39-3.81) |
| 45-64 | 10.56 | 14.36 | 2.89 (2.48-3.36) |
| 65+ | 0.55 | 0.25 | 0.99 (0.60-1.65) |
| Sex | |||
| Male | 69.51 | 64.04 | Ref. |
| Female | 30.49 | 35.96 | 1.23 (1.11-1.36) |
| Race/ethnicity | |||
| White, non-Hispanic | 53.22 | 64.01 | Ref. |
| Black, non-Hispanic | 30.55 | 25.60 | 0.66 (0.59-0.74) |
| Hispanic or Latino | 14.61 | 9.39 | 0.65 (0.55-0.77) |
| Other races | 1.63 | 0.99 | 0.56 (0.44-0.71) |
| Case type | |||
| Seeking detox | 3.28 | 12.52 | Ref. |
| Suicide attempt | 1.16 | 6.14 | 1.41 (1.08-1.83) |
| Problem drug use | 0.41 | 0.46 | 0.34 (0.21-0.56) |
| Other cases | 95.16 | 80.88 | 0.26 (0.21-0.31) |
| Disposition | |||
| Treated and released | 68.12 | 56.05 | Ref. |
| Admitted to same hospital | 19.02 | 26.22 | 1.32 (1.15-1.51) |
| Other dispositions | 12.86 | 17.74 | 1.41 (1.24-1.60) |
| Alcohol | |||
| Alcohol involvement | 36.76 | 34.18 | Ref. |
| Non-alcohol | 63.24 | 65.82 | 0.80 (0.71-0.89) |
AOR: adjusted odds ratio; CI: confidence interval; Ref.: reference group.
Boldface: the estimate in a group differed from the estimate in the reference group, P<0.05.
Results are weighted estimates.
Logistic regressions were adjusted for complex survey design and the admission year.
Among age groups, 19.63% of cannabis-only-involved ED visits were adolescents aged 12-17 years, which were higher than other age groups. Compared with adolescent admissions, those aged 35-44 years were most likely to use cannabis and other drug(s) (AOR=3.02, 95% CI=2.39-3.81). Black admissions were less likely to involve cannabis-polydrug than white admissions (AOR=0.66, 95% CI=0.59-0.74). Over 26% of ED visits involving cannabis-polydrug and 19% of ED visits involving cannabis-only were admitted to inpatient care.
3.4. Patterns of polydrug use by demographics (Table 3)
Table 3.
Patterns of other substance use among cannabis-polydrug ED visits: 2004-2011 DAWN
| Cannabis-involved admissions |
Other substances identified |
Cocaine | Heroin | Stimulantsa | Hallucinogensb | Inhalants | Opiates/ Opioidsc |
Sedatives /Benzodiazepinesd |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N | Row %e | Row % e | Row % e | Row % e | Row % e | Row % e | Row % e | |
| ED visits | 1,662,765 | 44.1 | 7.9 | 15.4 | 9.9 | 0.5 | 26.9 | 29.1 |
| Age in years | ||||||||
| 12-17 | 153,313 | 22.4 | 3.6 | 14.6 | 14.7 | 1.7 | 21.4 | 27.2 |
| 18-20 | 216,432 | 28.8 | 7.9 | 14.1 | 16.7 | 1.0 | 28.2 | 28.6 |
| 21-24 | 266,909 | 34.6 | 10.2 | 15.8 | 12.1 | 0.4 | 32.1 | 31.9 |
| 25-29 | 260,922 | 41.3 | 9.1 | 15.8 | 10.8 | 0.3 | 30.6 | 32.1 |
| 30-34 | 206,232 | 47.7 | 7.6 | 16.3 | 10.1 | 0.2 | 28.8 | 32.9 |
| 35-44 | 316,012 | 61.4 | 8.6 | 12.0 | 5.5 | 0.2 | 23.4 | 26.4 |
| 45-64 | 238,742 | 59.8 | 6.6 | 9.3 | 2.9 | 0.2 | 22.9 | 24.7 |
| 65+ | 4,203 | 47.1 | 2.7 | 4.5 | - | - | 20.5 | 23.2 |
| Sex | ||||||||
| Male | 1,064,700 | 45.3 | 8.7 | 12.9 | 10.7 | 0.6 | 26.1 | 26.8 |
| Female | 597,730 | 42.2 | 6.6 | 15.5 | 8.5 | 0.3 | 28.4 | 33.2 |
| Race/ethnicity | ||||||||
| White, non-Hispanic | 982,772 | 33.2 | 8.6 | 15.8 | 6.9 | 0.5 | 36.8 | 38.3 |
| Black, non-Hispanic | 393,061 | 67.2 | 5.4 | 4.0 | 16.8 | 0.4 | 12.7 | 14.1 |
| Hispanic or Latino | 144,201 | 54.8 | 9.4 | 19.4 | 10.1 | 0.8 | 9.6 | 15.0 |
| Other races | 15,210 | 42.2 | 6.1 | 24.5 | 13.2 | 0.3 | 12.0 | 18.2 |
A dash (-) indicated an estimated with a relative standard error (RSE) greater than 50% or an estimated based on fewer than 30 visits.
Results are weighted estimates.
Stimulants: methamphetamine and amphetamine.
Hallucinogens: MDMA (Ecstasy), phencyclidine (PCP), d-lysergic acid diethylamide (LSD), miscellaneous hallucinogens.
Opiates/opioids: narcotic pain relievers (buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, morphine, oxycodone, proxyphene products and methadone, and unspecified opiates/opioids.
Sedatives/benzodiazepines: barbiturates, benzodiazepines (alprazolam, clonazepam, diazepam, lorazepam), diphenhydramine, hydroxyzine and zolpidem.
Row % was calculated by the number of other specific substance combined with cannabis divided number of any other substance identified for each demographic groups.
There were 1,662,765 ED visits involved cannabis and at least one other drug. Cocaine (44.1%), opiates/opioids (26.9%) and sedatives/benzodiazepines (29.1%) were the drug classes commonly identified among cannabis-polydrug admissions. Among cannabis-polydrug ED admissions, 67% of blacks and 55% of Hispanics used cocaine together with cannabis, while opiates/opioids (36.8%) and sedatives/benzodiazepines (38.3%) were the most common drugs among whites.
3.5. Factors associated with hospitalization relative to ED visits only (Table 4)
Table 4.
Adjusted logistic regression analysis of factors associated with hospitalizations (relative to treated and released from ED), stratified by type of cannabis involvement, 2004-2011 DAWN
| Model 1: Any cannabis-involved admissions |
Model 2: Cannabis-only admission |
Model 3: Cannabis-polydrug admissions |
|
|---|---|---|---|
|
|
|||
| AOR (95%CI) | AOR (95%CI) | AOR (95%CI) | |
| Categories of cannabis use (vs. cannabis-only) |
|||
| Cannabis-polydrug | 1.31 (1.15-1.50) | ||
| Age in years (vs. 12-17) | |||
| 18-20 | 1.65 (1.34-2.04) | 1.80 (1.40-2.32) | 1.44 (1.00-2.08) |
| 21-24 | 1.86 (1.54-2.24) | 2.11 (1.62-2.75) | 1.57 (1.09-2.27) |
| 25-29 | 2.36 (1.83-3.06) | 2.64 (1.99-3.49) | 2.04 (1.37-3.03) |
| 30-34 | 2.94 (2.25-3.84) | 3.46 (2.55-4.68) | 2.45 (1.63-3.67) |
| 35-44 | 3.19 (2.48-4.10) | 3.35 (2.47-4.54) | 2.84 (1.96-4.12) |
| 45-64 | 3.80 (3.01-4.80) | 3.94 (2.92-5.30) | 3.44 (2.47-4.79) |
| 65+ | 7.73 (4.59-13.01) | 7.77 (4.10-14.73) | 7.95 (3.11-20.30) |
| Sex (vs. male) | |||
| Female | 1.01 (0.91-1.12) | 0.86 (0.73-1.02) | 1.10 (0.96-1.26) |
| Race/ethnicity (vs. while, non-Hispanic) |
|||
| Black , non-Hispanic | 0.95 (0.81-1.11) | 1.01 (0.81-1.27) | 0.91 (0.77-1.07) |
| Hispanic or Latino | 1.07 (0.78-1.46) | 1.24 (0.93-1.67) | 0.93 (0.68-1.25) |
| Other races | 1.29 (0.86-1.94) | 1.35 (0.93-1.97) | 1.29 (0.65-2.54) |
| Alcohol use (vs. non-alcohol) | |||
| Alcohol | 0.94 (0.85-1.04) | 0.98 (0.81-1.19) | 0.91 (0.79-1.04) |
| Case type (vs. seeking detox) | |||
| Suicide attempt | 2.54 (1.72-3.76) | 1.78 (0.88-3.62) | 2.64 (1.76-3.96) |
| Problem drug use | 0.11 (0.05-0.23) | 0.02 (0.01-0.05) | 0.16 (0.07-0.36) |
| Others | 0.53 (0.42-0.68) | 0.52 (0.35-0.78) | 0.53 (0.41-0.69) |
AOR: adjusted odds ratio; CI: confidence interval.
Bold faced: P<0.05.
Logistic regressions were adjusted for complex survey design and the admission year.
In Model 1, use of cannabis and other drug(s) (vs. cannabis-only) increased the likelihood of hospitalization relative to ED visit only (AOR=1.31, 95% CI=1.15-1.50). In all models, young adult admissions (21-24 years) had higher odds of cannabis-involved hospitalization than adolescent admissions (12-17 years), and the odds increased with age strata.
4. Discussion
This study used a national sample of drug-involved ED visits to inform the trends in cannabis-involved ED visits. Our results reveal an increased trend in ED utilization involving cannabis use from 2004 to 2011, and suggest cannabis use might potentially add burden to the healthcare system. We found that, between 2004 and 2011, adolescents aged 12-17 years and non-Hispanic blacks showed the fastest increase in the cannabis-only-involved ED visit rate, and that young adults aged 21-24 years and non-Hispanic blacks had the highest increase in cannabis-polydrug-involved ED visit rate. The drug classes commonly identified among cannabis-polydrug ED visits were cocaine, opiates/opioids, and sedatives/benzodiazepines. Relative to ED visits only, the odds of hospitalization increased with older age strata compared with adolescent admissions, suggesting a heavier burden in cannabis-involved ED visits and hospitalization among older cannabis users.
Our study extends epidemiological data on cannabis use trends and cannabis-related health conditions. The possible effects of cannabis use on health over time not only depend on the prevalence of cannabis use, but also on the cannabis potency and dose, administration mode, and individual experiences with cannabis and other drugs (Hall, 2015). It is worrisome that cannabis potency in samples of seized cannabis had steadily increased from 5.3% in 2000 to 12.2% in 2014 (ONDCP, 2015), and that use of high-potency cannabis may enhance addiction or treatment demand (Freeman and Winstock, 2015). Our results of the increase in cannabis-involved ED visits are in line with other reports. In the Treatment Episode Data Set, the proportion of cannabis-involved admissions to addiction-related treatment facilities among persons aged ≥12 years increased from 15.8% in 2004 to 18.3% in 2011 (SAMHSA, 2015b). Colorado legalized medical cannabis in 2000 and recreational cannabis in 2014. A recent study of statewide ED visit data (2011-2014) on ICD-codes found an increasing trend in ED visits that were potentially related to CUD in Colorado (Kim et al., 2016). Given the continued wave of cannabis legalization and reports of increased availability of higher-potency cannabis, our findings reinforce the need for research to identify subgroups at risk for CUD and related healthcare utilization.
4.1. Increase in ED use among adolescents
We found that the cannabis-only-involved ED visit rate in adolescents aged 12-17 years grew faster than that of other age groups between 2004 and 2011. This finding implies that the prevalence of problem cannabis use among adolescents may have risen. On the other hand, because the DAWN data represent treatment admissions, the admission rate may also be influenced by a subset of severe adolescents who had frequent cannabis-involved admissions. National surveys found that the overall prevalence of any current cannabis use among adolescents remained stable between 2004 and 2011 (Johnson et al., 2015; SAMHSA, 2015a). However, it is imperative to conduct in-depth analysis of problem cannabis use to better inform targeted intervention for adolescents who need timely help, as a crude indicator of any cannabis use may overlook high-risk groups of cannabis users. For example, the prevalence of past-year CUD was lower among adolescents aged 12-17 (3.4%) than young adults aged 18-25 (5.7%); but adjusted analysis controlling for demographics and other substance use found that young adults were about 20% less likely than adolescents to have a CUD (Wu et al., 2014). Among adolescent past-year cannabis users, as many as 25.6% met criteria for a CUD compared with 19.4% of adult past-year cannabis users aged 18-25 (Wu et al., 2014). Adolescents are vulnerable to cannabis exposure. Short-term consequences of cannabis use may include impaired short-term memory, decreased concentration or problem solving, and altered judgment; which could interfere with learning or increase unprotected sexual behaviors and medical conditions (Dougherty et al., 2013; Volkow et al., 2014). Adolescent-onset and long-term cannabis use increase the risk for altered brain development, declined IQ, and psychiatric disorder (Lubman et al., 2015; Meier et al., 2012; Volkow et al., 2014).
4.2. Increase in ED use among blacks
We found that non-Hispanic blacks had the highest increase in the cannabis-involved ED visit rate across racial/ethnic groups from 2004 to 2011. This finding and other reports suggest the need to monitor cannabis-related health events and develop intervention for black cannabis users. Hasin et al. (2015) found that past-year cannabis use (4.7% vs. 12.7%) and CUD (1.8% vs. 4.6%) among black adults increased between 2001-2002 and 2012-2013. Blow et al. (2011) used latent class analyses to study drug-related ED admissions and found that blacks were most likely to be in the primary cannabis use group. In a sample of adults with alcohol/drug use disorders, Pacek et al. (2012) found that a greater proportion of blacks (22%) had a CUD than whites (11%) or Hispanics (10%). Several factors may be related to the elevated rate of cannabis-involved ED admissions among blacks. First, perceived regular cannabis use as great risk among blacks has significantly declined by 10% between 2004 and 2012, which may be related to cannabis legalization (Pack et al., 2015). Second, blunt use was found to be comparatively prevalent among blacks that may be related to the elevated prevalence of cannabis use problems (Golub et al., 2006; Timberlake, 2013). For example, Montgomery (2015) found that blunt use among blacks was related to a pattern of an earlier age of onset of cigarette, cigar and cannabis use than no use of blunt (tobacco use only). Recent studies showed that blunt use was associated with increased odds of cannabis use disorder among blacks (Cohn et al., 2016; Fairman, 2015). Lastly, blacks have faced more barriers to mental health care than white, and a delay to access timely healthcare may be related to excess use of ED care (Cook et al., 2010). The DAWN data are based on encounters. Future research is needed to clarify further the severity of cannabis use and healthcare use patterns, including moderating effects (e.g., access to addiction care), for blacks and young adults.
4.3. Increase in ED and hospitalization use among cannabis-polydrug users
This study also identified important finding regarding elevated odds of cannabis-involved ED admission plus subsequent hospitalizations among adult cannabis-polydrug users aged ≥30 years. This finding is consistent with epidemiologic data, showing that active older drug users tend to have to a pervasive pattern of medical comorbidities and an elevated rate of treatment admissions, especially among persons aged 50-64 years (Wu and Blazer, 2011). The long-term effect of cannabis use among middle-aged or elder adults may be related to manifestations of multiple health conditions, such as addiction, memory impairment, or cardiovascular disease that require more treatment (Auer et al., 2016; Hall, 2015; Thomas et al., 2014).
4.4. Implications
Infrequent screening of problem drug use and under-treatment of drug use disorders at general healthcare settings may contribute to ED admissions (Rockett et al., 2003; Tai et al., 2012). Cannabis-related health risks may be overlooked by adolescents and their parents, or healthcare providers (Chung et al., 2003). During ED visits, toxicology questions or testing as a screening method may improve the identification of problem cannabis use, in particular for adolescents (Bernstein et al., 2009). These data also show the importance of taking into account racial/ethnic variations (cannabis and cocaine use among blacks; cannabis and sedative/opiate use among whites) in the screening, assessment and intervention for cannabis-related drug use problems and other healthcare needs. Cannabis-related intervention research should be expanded to target adolescents and blacks (Pitts and Shrier, 2014; Woolard et al., 2013). There is a need for research to develop risk-stratified screening and targeted interventions for high-risk groups (e.g., adolescents, blacks, middle-aged active drug users), especially at ED settings where drug-involved events may be more common than other settings.
4.5. Limitation
The results should be interpreted within the following limitations. First, although cannabis-involved ED visit reflected recent or active cannabis use and it was considered either a direct cause or a contributor to the visits (CBHSQ, 2013), the causality between cannabis use and ED visits cannot be determined. Regarding the reason for ED admission, most of the reasons were coded as unknown, which constrain our analysis for this variable. Second, the DAWN data do not include the information about the frequency and dose of cannabis use. Third, about 8% of ED visits did not document the race/ethnicity in DAWN between 2004 and 2011 (SAMHSA, 2015a), and the missing data may result in the underestimates. Finally, when polydrug use was reported by DAWN, the principle cause of the ED visits cannot be definitely determined.
4.6. Conclusion
This study provides the national-level findings specifically for cannabis-involved healthcare utilization. By using the only national-level drug-related ED admission dataset available, we were able to examine the national trends in the ED visits for cannabis-only and cannabis-polydrug. These findings indicated a notable increase in cannabis-involved utilization of ED during the studied period. There is a continuous need to monitor cannabis-related healthcare utilization, especially among young people and blacks as well as states permitting recreational cannabis use. Research is needed to identify and develop feasible screening and intervention approaches in general medical settings to prevent or reduce problem cannabis use and related health concerns.
Supplementary Material
Acknowledgments
Role of the funding source: This work was made possible by research support from the U.S. National Institutes of Health (UG1DA040317, R01MD007658, R01DA019623, R01DA019901; PI, Li-Tzy Wu). The sponsoring agency had no further role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Footnotes
Conflicts of Interest: None.
References
- Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auer R, Vittinghoff E, Yaffe K, et al. Association between lifetime marijuana use and cognitive function in middle age: the coronary artery risk development in young adults (CARDIA) Study. JAMA Intern Med. 2016;176(3):352–361. doi: 10.1001/jamainternmed.2015.7841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Acad Emerg Med. 2009;16(11):1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Barry KL, et al. Alcohol and drug use among patients presenting to an inner-city emergency department: a latent class analysis. Addict Behav. 2011;36(8):793–800. doi: 10.1016/j.addbeh.2010.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality . Outcomes of drug-related emergency department visits associated with polydrug use. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; Rockville, MD: 2012. [Google Scholar]
- Center for Behavioral Health Statistics and Quality . Drug Abuse Warning Network methodology report, 2011 update. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; Rockville, MD: 2013. [Google Scholar]
- Chung T, Colby SM, O'Leary TA, Barnett NP, Monti PM. Screening for cannabis use disorders in an adolescent emergency department sample. Drug Alcohol Depend. 2003;70(2):177–186. doi: 10.1016/s0376-8716(02)00346-0. [DOI] [PubMed] [Google Scholar]
- Cohn A, Johnson A, Ehlke S, Villanti AC. Characterizing substance use and mental health profiles of cigar, blunt, and non-blunt marijuana users from the National Survey of Drug Use and Health. Drug Alcohol Depend. 2016;160:105–111. doi: 10.1016/j.drugalcdep.2015.12.017. [DOI] [PubMed] [Google Scholar]
- Cook BL, McGuire TG, Lock K, Zaslavsky AM. Comparing methods of racial and ethnic disparities measurement across different settings of mental health care. Health Serv Res. 2010;45(3):825–847. doi: 10.1111/j.1475-6773.2010.01100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean A. Illicit drugs and drug interactions. Australian Pharmacist. 2006;25:684. [Google Scholar]
- Dougherty DM, Mathias CW, Dawes MA, et al. Impulsivity, attention, memory, and decision-making among adolescent marijuana users. Psychopharmacology. 2013;226(2):307–319. doi: 10.1007/s00213-012-2908-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairman BJ. Cannabis problem experiences among users of the tobacco–cannabis combination known as blunts. Drug Alcohol Depend. 2015;150:77–84. doi: 10.1016/j.drugalcdep.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman T, Winstock A. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med. 2015;45(15):3181–3189. doi: 10.1017/S0033291715001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French MT, Fang H, Balsa AI. Longitudinal analysis of changes in illicit drug use and health services utilization. Health Serv Res. 2011;46:877–899. doi: 10.1111/j.1475-6773.2010.01218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub A, Johnson BD, Dunlap E. The growth in marijuana use among American youths during the 1990s and the extent of blunt smoking. J Ethn Subst Abuse. 2006;4(3-4):1–21. doi: 10.1300/J233v04n03_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19–35. doi: 10.1111/add.12703. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RM, Fairman B, Gilreath T, Xuan Z, Rothman EF, Parnham T, Furr-Holden CD. Past 15-year trends in adolescent marijuana use: differences by race/ethnicity and sex. Drug Alcohol Depend. 2015;155:8–15. doi: 10.1016/j.drugalcdep.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HS, Hall KE, Genco EK, Van Dyke M, Barker E, Monte AA. Marijuana tourism and emergency department visits in Colorado. N Engl J Med. 2016;374(8):797–798. doi: 10.1056/NEJMc1515009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubman DI, Cheetham A, Yücel M. Cannabis and adolescent brain development. Pharmacol Therapeut. 2015;148:1–16. doi: 10.1016/j.pharmthera.2014.11.009. [DOI] [PubMed] [Google Scholar]
- McGeary KA, French MT. Illicit drug use and emergency room utilization. Health Serv Res. 2000;35:153–169. [PMC free article] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109(40):E2657–E2664. doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery L. Marijuana and tobacco use and co-use among African Americans: Results from the 2013, National Survey On Drug Use and Health. Addict Behav. 2015;51:18–23. doi: 10.1016/j.addbeh.2015.06.046. [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control Policy (ONDCP) [Accessed June 3, 2016];National Drug Control Strategy Data Supplement 2015 [The White House web site] 2015 Available at: https://www.whitehouse.gov//sites/default/files/ondcp/policy-and-research/2015_data_supplement_final.pdf.
- Pacek LR, Malcolm RJ, Martins SS. Race/ethnicity differences between alcohol, marijuana, and co-occurring alcohol and marijuana use disorders and their association with public health and social problems using a national sample. Am J Addict. 2012;21(5):435–444. doi: 10.1111/j.1521-0391.2012.00249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 2015;149:232–244. doi: 10.1016/j.drugalcdep.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perron BE, Bohnert AS, Monsell SE, Vaughn MG, Epperson M, Howard MO. Patterns and correlates of drug-related ED visits: results from a national survey. Am J Emerg Med. 2011;29(7):704–710. doi: 10.1016/j.ajem.2010.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitts S, Shrier LA. Substance abuse screening and brief intervention for adolescents in primary care. Pediatr Ann. 2014;43(10):412. doi: 10.3928/00904481-20140924-09. [DOI] [PubMed] [Google Scholar]
- Rockett IR, Putnam SL, Jia H, Smith GS. Assessing substance abuse treatment need: a statewide hospital emergency department study. Am J Emerg Med. 2003;41:802–813. doi: 10.1067/mem.2003.189. [DOI] [PubMed] [Google Scholar]
- Rubino T, Zamberletti E, Parolaro D. Adolescent exposure to cannabis as a risk factor for psychiatric disorders. J Psychopharmacol. 2012;26(1):177–88. doi: 10.1177/0269881111405362. [DOI] [PubMed] [Google Scholar]
- Stata [computer program] StataCorp LP; College Station: 2013. Release 13. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2014 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; Rockville, MD: 2015a. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Treatment Episode Data Set (TEDS): 2003-2013. National Admissions to Substance Abuse Treatment Services; Substance Abuse and Mental Health Services Administration; Rockville, MD: 2015b. (BHSIS Series S-75). HHS Publication No. (SMA) 15-4934. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Drug Abuse Warning Network (DAWN), 2004-2011. Inter-university Consortium for Political and Social Research [distributor]; Ann Arbor, MI: 2015c. [Google Scholar]
- Tai B, Wu LT, Clark HW. Electronic health records: essential tools in integrating substance abuse treatment with primary care. Subst Abuse Rehabil. 2012;3:1–8. doi: 10.2147/SAR.S22575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath YM, O'Malley PM, Johnston LD. Alcohol and marijuana use patterns associated with unsafe driving among U.S. high school seniors: high use frequency, concurrent use, and simultaneous use. J Stud Alcohol Drugs. 2014;75(3):378–389. doi: 10.15288/jsad.2014.75.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas G, Kloner RA, Rezkalla S. Adverse cardiovascular, cerebrovascular, and peripheral vascular effects of marijuana inhalation: what cardiologists need to know. Am J Cardiol. 2014;113(1):187–190. doi: 10.1016/j.amjcard.2013.09.042. [DOI] [PubMed] [Google Scholar]
- Timberlake DS. The changing demographic of blunt smokers across birth cohorts. Drug Alcohol Depend. 2013;130(1):129–134. doi: 10.1016/j.drugalcdep.2012.10.022. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219–2227. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolard R, Baird J, Longabaugh R, Nirenberg T, Lee CS, Mello MJ, Becker B. Project reduce: reducing alcohol and marijuana misuse: effects of a brief intervention in the emergency department. Addict Behav. 2013;38(3):1732–1739. doi: 10.1016/j.addbeh.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG. Illicit and nonmedical drug use among older adults: a review. J Aging Health. 2011;23(3):481–504. doi: 10.1177/0898264310386224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Swartz MS, Wu Z, Mannelli P, Yang C, Blazer DG. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann Emerg Med. 2012;60(2):172–180. doi: 10.1016/j.annemergmed.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Brady KT, Mannelli P, Killeen TK, Workgroup NA. Cannabis use disorders are comparatively prevalent among nonwhite racial/ethnic groups and adolescents: a national study. J Psychiatr Res. 2014;50:26–35. doi: 10.1016/j.jpsychires.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Swartz MS, Brady KT, Hoyle RH, Workgroup NA. Perceived cannabis use norms and cannabis use among adolescents in the United States. J Psychiatr Res. 2015;64:79–87. doi: 10.1016/j.jpsychires.2015.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.