Abstract
Invasive candidiasis remains one of the most serious community and healthcare-acquired infections worldwide. Conventional Candida detection methods based on blood and plate culture are time-consuming and require at least 2–4 days to identify various Candida species. Despite considerable advances for candidiasis detection, the development of simple, compact and portable point-of-care diagnostics for rapid and precise testing that automatically performs cell lysis, nucleic acid extraction, purification and detection still remains a challenge. Here, we systematically review most prominent conventional and nonconventional techniques for the detection of various Candida species, including Candida staining, blood culture, serological testing and nucleic acid-based analysis. We also discuss the most advanced lab on a chip devices for candida detection.
Keywords: Blood culture, disease diagnostics, invasive Candidiasis, laboratory on a chip, loop-mediated isothermal amplification, microfluidics, nanotechnology
Introduction
The Fungal Kingdom consists of about one million species and it is estimated that only 400 of them can cause disease in humans.[1–3] Fungi reproduce mainly by the following two different ways: sexually by the fusion of haploid gametes/hyphae generated through meiosis or asexually by budding, fragmentation and spore formation. Fungi can also switch between these two forms.[4] Due to the highly dimorphic nature of fungi, its classification is difficult and continues to be revised. Fungi, including yeasts, molds and mushrooms, are involved in baking,[5] the production of alcoholic beverages, bio-remediation,[6] the production of antibiotics, vitamins, anticancer and cholesterol-lowering drugs,[7–9] and various types of chemical products.[10] Although fungi play a beneficial role in human life, some of them are hazardous to human health.[11] Yeast fungi, like Candida albicans, typically associate as a commensal symbiont with human hosts. Candida is also notoriously found as an opportunistic pathogen.[12]
The genus Candida contains about 150 species, but only few of them, such as C. albicans, C. tropicalis, C. glabrata, C. dubliniensis, C. krusei and C. parapsilosis, are implicated in human pathogenesis. Candida species live as commensals on skin, the gastrointestinal and genitourinary tracts. Repeated and lengthy episodes of neutropenia provide favorable conditions for Candida growth especially in critically ill patients facing AIDS,[13] blood cancer, bone marrow or solid organ transplants.[14–16] Preterm neonates,[17] intensive care and immunosuppressed patients [18] are considered more prone to Candida infections. Increased use of immunosuppressive agents, broad spectrum antibiotics, anti-cancer therapies, the use of indwelling catheters and long-term corticosteroid therapy [19] are all predisposing factors for acquiring Candida infections.[20] Superficial candidiasis, including chronic stomatitis, vulvovaginitis and mucocutaneous candidiasis, can be treated easily with hygiene measures and application of local ointments. Common clinical features associated with different Candida spp. are described in Table 1.
Table 1.
Candida infections in humans: Species related clinical features [162].
| Species | Related clinical features |
|---|---|
| C. albicans | Mucocutaneous infections: oropharyngeal, esophagitis, vaginitis; Deep-seated infections: pyelonephritis, peritonitis; Hematogenous infections: candidemia, meningitis, hepatosplenic |
| C. parapsilosis | Candidemia, deep infections associated with implanted devices, infections related to contaminated solutions responsible for most candidemia among neonates |
| C. tropicalis | Candidemia and systemic candidiasis in immunosuppressed patients Candidemia may be associated with severe myalgia and myositis |
| C. glabrata | Systemic candidiasis, candidemia, urinary tract infections |
| C. krusei | Candidemia, endophthalmitis, diarrhea in newborns |
Reproduced and modified with copyright permission from [162].
Epidemiological data of recent decades place Candida as the fourth major cause of nosocomial infections,[21] with about 50% of these cases attributed to C. albicans. Typically, disease progression by C. albicans is controlled by the innate immune system that recognizes a component in Candida’s cell wall through toll-like receptors (TLRs) and carbohydrate lectin receptors (CLRs).[22–24] Key factors involved in the pathogenicity of C. albicans include the potential of hyphal switch and the ability to form biofilms with which C. albicans can adhere to surfaces. Biofilm formation enhances C. albicans resistance to drugs and the immune system.[25,26]
Data from United States National Nosocomial Infection Surveillance (NNIS) system between 1990 and 1999 [27–30] showed that Candida was the fourth leading nosocomial pathogen.[31] Recent reports [32] identify Candida at the top of the pathogen list causing healthcare-associated bloodstream infections in the United States. These Candida-related bloodstream infections require prolonged hospitalization (additional 3–13 days, average hospital days for patients with similar illness =7.3) and significantly increase healthcare costs ($6000–$29,000 – more in comparison with normal hospitalization cost).[33,34] With mortality rates as high as 30%, nosocomial candidemia remains a major threat in hospitals, underscoring the need for rapid point-of-care (POC) detection to prevent wide-scale spread. Candida can also cause lethal infections leading to multiple organ failure and septic shock.[27,35–37] This situation could be exacerbated by drug resistance, which is relatively stable at 7% for fluconazole currently, is showing trends for multidrug resistance to other agents such as echinocandins. It is the emergence of multidrug resistance – a trend projected to worsen – that warrants developing a rapid and versatile POC detection platform that could be used for diagnosis and antimicrobial susceptibility screening. Sensitive and rapid detection of Candida can play a major role in the effective management of fungal infection and treatment monitoring.
The detection of Candida has become very important due to an increased incidence of Candida infection, especially in immunocompromised patients. Current laboratory settings and Candida detection methods are very time-consuming and require at least 2–4 days to identify Candida spp.[40] As Candida infects mostly the patients who are in intensive care units (ICUs) and require urgent treatment, the fast detection of Candida has become extremely important for these immunocompromised subjects and preterm neonates. There is an increasing need to identify other Candida spp. along with C. albicans because of differences in fluconazole susceptibility.[41] Although C. albicans shows low resistance to triazoles, other species such as C. glabrata and C. krusei are resistive to usual doses of triazoles.[42–46] These species are 32 times less susceptible to fluconazole than C. albicans. It has also been observed that more than one Candida spp. can be found in clinical samples, especially from neonates.[47] Rapid identification of C. albicans along with other species has led to the development of new commercial products and techniques. Previous reviews published on Candida detection are focused mainly on conventional techniques.[38,39] Here, we review conventional and nonconventional diagnostic assays in the market and in the development pipeline for Candida detection. We have discussed diagnostic assays for Candida detection at the POC. We also review the technological advancements and potential challenges faced by researchers, which has been schematized in Figure 1.
Figure 1.
Schematic of conventional and nonconventional methods for Candida detection.
Detection of Candida
Methods available for the detection of Candida can be broadly classified into microscopic examination, conventional detection methods and nonconventional techniques. The microscopic examination consists of nonspecific staining with calcofluor white (CFW) and specific staining of Candida with fluorescent in situ hybridization (FISH)/antibodies. Conventional methods include carbohydrate assimilation and fermentation reactions, culture-based Candida detection, blood culture and nucleic acid detection techniques, while the nonconventional methods covered various lab chip (LOC) devices developed for Candida detection.
Microscopic examination
Nonspecific staining with calcofluor white (CFW)
The microscopic detection of Candida in clinical specimens can guide the laboratory selection of appropriate media and culture techniques to confirm the presence of Candida. The clinician and laboratory staff usually determine the detection technique based on the origin and form of the sample. For specimens, such as nail clippings, skin scrapings, tissues, aspirates and respiratory specimens, microscopic observation and detection can be used, whereas for fluidic samples such as blood and urine, culture methods are preferred.[48,49] Calcofluor white (CFW) staining may be used for direct examination of most samples using fluorescent microscopy. CFW has been extensively used in textile and paper industry as “fluorescent brightner” as it prevents the yellowing of fabric or paper. It binds to β 1–3 and β 1–4 polysaccharides of the chitin ring found in the fungus cell wall.[50,51] It gives bright green to bluish color when excited by ultraviolet (UV) radiation with an absorbance peak maximum at 347 nm. The addition of potassium hydroxide (KOH) with CFW can enhance the visualization of fungal elements in specimens. Chitin, found in fungi cell wall, is resistant to KOH digestion as reported earlier.[52,53] KOH dissolves other cells faster than fungi because of chitinous cell walls of fungi.[54] CFW at 0.0025% concentration mixed into peptone and glucose medium can also be used to differentiate various Candida species.[55] C. krusei (elongated cells) and C. torulopsis glabrata (oval cells) gave only slight fluorescence at the end of the cells, whereas C. albicans showed characteristic pseudohyphae. Although the cell shape and size of C. parapsilosis were similar to those of C. krusei, the former showed fluorescence over the entire cell surface. C. tropicalis was also differentiated based on CFW fluorescence patterns as shown in Figure 2. A substantial amount of CFW nonspecific binding with human cellular material especially lung tissue, blood vessels and skin sections is expected, but microorganisms can be distinguished by experienced laboratory staff based on their characteristic morphology.[54] CFW staining of certain fungi, such as Pneumocystis carinii and Coccidioides immitis, have been reported to be problematic and fluorescence results have been found to be dependent on a CFW supplier.[56,57] Although CFW staining can serve as rapid fungi detection tool, due to the reported variability of results and nonspecific binding of CFW, the need for validating the results with other culture-based methods is always recommended. Additionally, CFW staining kills the organism, hence drug resistance testing becomes impossible.
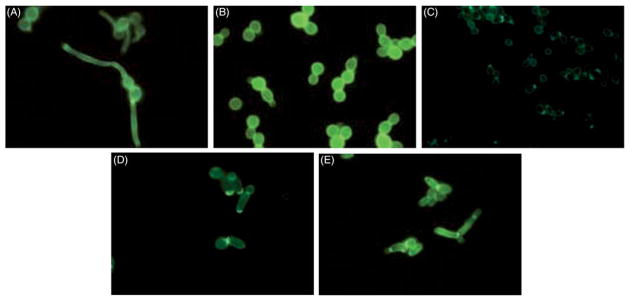
Figure 2.
CFW staining of Candida spp. (A) Fluorescent image of C. albicans after germ tube production. The long tubes are pseudohyphae, the characteristic morphology of C. albicans. (B) UV fluorescent image of C. tropicalis having oval shape and bright CFW staining over whole cell. (C) Fluorescent image of C. torulopsis glabrata, very slight CFW staining at the ends of oval cells. (D) Fluorescent image of C. krusei, slight CFW staining at the end of elongated cells. (E) Fluorescent image of C. parapsilosis, dull fluorescence over whole elongated cells. Reproduced with the permission from.[54]
Specific staining of Candida with FISH/antibodies
Specific fluorescent staining of tissue specimens based on immunochemistry and genetic markers is considered one of the most reliable methods for the diagnosis of Candida infection. FISH is a technique that uses fluorescent oligonucleotide probes that specifically bind to genes present in the cell’s genome. FISH technique was employed to differentiate C. parapsilosis from C. albicans using probes targeting 18S rRNA region of Candida.[58] C. albicans was successfully detected in tissue specimens of brain, kidney and spleen of infected mice. It was reported that FISH methods were prone to lengthy and dim fluorescent signals if DNA-based probes were used for Candida detection.[59] Efforts have also been made to overcome these challenges by using different DNA-based probes along with unlabeled helper probes. The helper probes significantly increased the fluorescent intensity of C. albicans when used with different FISH DNA-based probes (Calb-1249 or CalB-2208).[59] For enhanced FISH staining, peptide nucleic acid (PNA)-based probes targeting 26S rRNA region were also employed. PNA-based FISH-labeling technique improved signal intensity in shorter amounts of time.[60] In another report, C. albicans was identified after isolation from media using PNA FISHFlow (AdvanDX, MA).[61] The PNA FISHFlow Kit was also tested to analyze its efficiency to identify Candida from 150 clinical isolates collected from various sources. Isolates were hybridized with PNA-based probes after 24-h culture on agar plates.[61] It successfully identified different Candida spp. including C. glabrata, C. albicans, C. tropicalis, C. krusei, C. parapsilosis, C. dubliniensis, C. kefyr and others. The specificity and sensitivity of PNA FISHFlow probes for Candida identification were 100% (49 of 49) and 100% (101 of 101) respectively and the whole staining process completed in 1 h.[61] Gherna et al. also used the PNA FISH detection kit from AdvanDX and identified C. albicans and C. glabrata from 40 positive blood culture bottles in 1.25 h.[62] In another report, FISH oligonucleotide probes, labeled with fluorescein isothiocyanate (FITC; green signal) and fluorochrome CY3 (red signal), were synthesized by Microsynth (Switzerland, Table 2).[63,64] Candida was detected in 98% of positive blood samples (49 of 50) with PF2 all yeast probe. Different Candida spp. were also accurately identified with specific FISH probes. For example, in one specimen, FISH method detected C. parapsilosis, whereas the conventional method misidentified it as C. glabrata.[63,64] It was later confirmed with repeated culture methods that detected Candida spp. was C. parapsilosis as correctly identified by FISH method.[63,64] Overall, FISH detection methods offer a rapid platform for specific identification of Candida spp. from blood culture. Although it gives high sensitivity and specificity, FISH cannot be employed directly with patient blood samples without culture. Blood culture can take up to two weeks before giving positive results. There is a need to optimize FISH testing protocols for application in patient blood samples directly that may be achieved by incorporating efficient cell separation and centrifugation processes.
Table 2.
| FISH probe name | Oligonucleotide sequence (5′-3′) | Specificity | rRNA positiona |
|---|---|---|---|
| PF2 | CTC TGG CTT CAC CCT ATT C | All yeast | 18/618 |
| Caal | GCC AAG GCT TAT ACT CGC T | C. albicans | 18/1249 |
| Cagl | CCG CCA AGC CAC AAG GAC T | C. glabrata | 18/651 |
| Cpara | CCT GGT TCG CCA AAA AGG C | C. parapsilosis | 18/651 |
| Ckrus | GAT TCT CGG CCC CAT GGG | C. Krusei | 18/1433 |
| Non Eub | ACT CCT ACG GGA GGC AGC | None | None |
First number represents type of rRNA (18S); second number represents the position of first base of target sequence.
All probes were labeled with FITC or CY3.
Conventional Candida detection methods
Carbohydrates assimilation and fermentation reactions
The most conventional method to identify Candida in a mycology laboratory is using carbohydrate assimilation and fermentation reactions. Traditionally, liquid media in test tubes are used for the assimilation of glucose, maltose, sucrose, lactose, rhamnose and trehalose, whereas glucose, maltose, sucrose, lactose are used for fermentation.[65] The test tubes are incubated and examined for growth after 7 and 14 days. These tests can now be performed easily on automated systems including the Auxacolor (Sanofic Diagnositcs Pasteur), API 20C AUX (bioMerieux-Vitek, Inc., Hazelwood, Missouri), the Uni-Yeast-Tek kit and Yeast Star (CLARC laboratories). The tests either utilize the production of color (Uni-Yeast-Tek and Auxacolor) or an increase in turbidity (API 20C AUX) in various wells having different substrates to produce a distinctive biochemical profile. A numerical code is generated for each isolate depending on the biochemical reaction profile. Identification of species is made by referring to a list of numerical profiles provided by the manufacturer. The API 20C AUX system is one of the first systems that is commercially available for the detection of Candida. It is faster than classical assimilation and fermentation methods but still requires up to 72-h incubation.[66–69] Auxacolor and API Candida are an improved version of API 20C AUX and can produce results after 24-h incubation. These two systems are intended to identify the most commonly encountered clinical pathogens; the Auxacolor system is capable of identifying 26 species, while API Candida systems can only identify 15 species.[66–69] These methods provide good identification results for more common species with an accuracy of 78.8% to 91.8% for API Candida, 85.7% to 91.2% for Auxacolor, 62.1% to 99.3% for API 20C, 89.7% for Vitek Yeast Biochemical Card (YBC), 99.8% for Uni-Yeast-Tek and 79.3% for Yeast Star.[67–71] On the other hand, there were many reports showing that all of these systems either misidentified various fungal species or provided inconclusive results.[70,71] The API Candida system misi-dentified 7.5% of Candida spp. (12 of 159 isolates) and 14.5% of isolates (23 of 159) required further testing to validate their identification. About 27.2% isolates of C. guilliermondii were incorrectly identified as S. cerevisiae, whereas one of 11 was misidentified as either C. famata or C. parapsilosis.[67,70] API Candida systems also misidentified 10% of C. tropicalis isolates as C. albicans and 5% as C. famata. The Auxacolor system did not identify 8.1% (13 of 159) isolates; four isolates of C. lusitaniae, three of S. cerevisiae, two of C. guilliermondii, two of Trichosporon beigelii, one of C. albicans and one of C. tropicalis.[67,70] Morphological and culture-based Candida detection techniques are concurrently employed along with assimilation-/fertilization-based testing to confirm species identification that would further increase the identification time.
Culture-based Candida detection
Clinical specimens are routinely cultured on Sabouraud glucose agar (SGA) for fungal growth. The pathogen isolates are tested using assimilation/fermentation methods or are further cultured on Dalmau Plate, Corn meal-Tween 80 agar (CTA) for morphological identification on species level.[72,73] The development of a chromogenic medium improves the Candida differentiation method based on albicans and 100% of C. krusei the color/texture (Figure 2). The medium contains chromogenic substrates that react with enzymes produced by different pathogens and produce colonies of varying color and morphology. Chromogenic media culture kits are commercially available by various manufacturers including, but not limited to, BBL CHROMagar Candida (CHROMagar; Becton Dickinson Canada Inc.), Bio-Rad CandiSelect 4 (CandiSelect; Bio-Rad), Oxoid OCCA (OCCA; Oxoid Ltd.) and CHROMagar Candida (CMA, CHROMagar Company, Paris, France).[74] CHROMagar Candida has been used to successfully identify 95% of C. albicans, 94% of C. glabrata, 100% of C. Tropicalis and 100% of C. krusei isolates from other yeast spp. based on their color and morphology.[73,75] The CHROMagar has the ability to efficiently detect more than one yeast spp. from a clinical specimen; 43 out of 234 positive cultures contained a mixture of yeast spp. as detected by CHROMagar. On the other hand, 47% of these mixed cultures were not identified by SGA alone.[75] Adam et al. [74] compared the performance of three commercially available chromogenic media CHROMagar, CandiSelect and OCCA.[74] CHROMagar and CandiSelect have accurately identified 100% of C. albicans and C. krusei isolates, whereas OCCA identified 92% of C. albicans and 56% of C. krusei after 48-h incubation. Furthermore, CHROMagar, CandiSelect and OCCA correctly identified 50%, 60% and 40% of C. Tropicalis and 88%, 75% and 50% of C. glabrata respectively. There were few discrepancies found in all of the three media; CHROMagar falsely identified 1 C. tropicalis isolate as C. glabrata; CandiSelect falsely identified 1 C. glabrata as C. tropicalis and OCCA falsely identified 1 C. albicans as C. tropicalis, 1 C. tropicalis as C. albicans and 1 C. tropicalis as C. glabrata.[74] In another report, although CHROMagar identified 98.8% of C. albicans and 100% of C. krusei, only 66.7% of C. tropicalis (4 of 6) were correctly identified. It also identified C. glabrata with 98% sensitivity and 92.1% specificity, but some other stains of Candida (three stains of C. parapsilosis, two stains of C. lusitaniae, five out of nine stains of C. cerevisiae) also grew to pink colonies, similar to C. glabrata. Although the pink coloration of these species did not exactly match C. glabrata, there were high chances of a mistake without experienced laboratory staff.[73] Similar results were reported by Sivakumar et al., [76] where CHROMagar misidentified three out of eight C. tropicalis as C. albicans, whereas C. glabrata could not be identified without experience. To overcome these shortcomings, a new scheme of using CTA (morphology) and CMA (color, morphology) at the same time was proposed and C. tropicalis was detected with >99% confidence.[72] C. glabrata was more efficiently identified by using combination of CTA and CMA as shown Figure 3.[72]
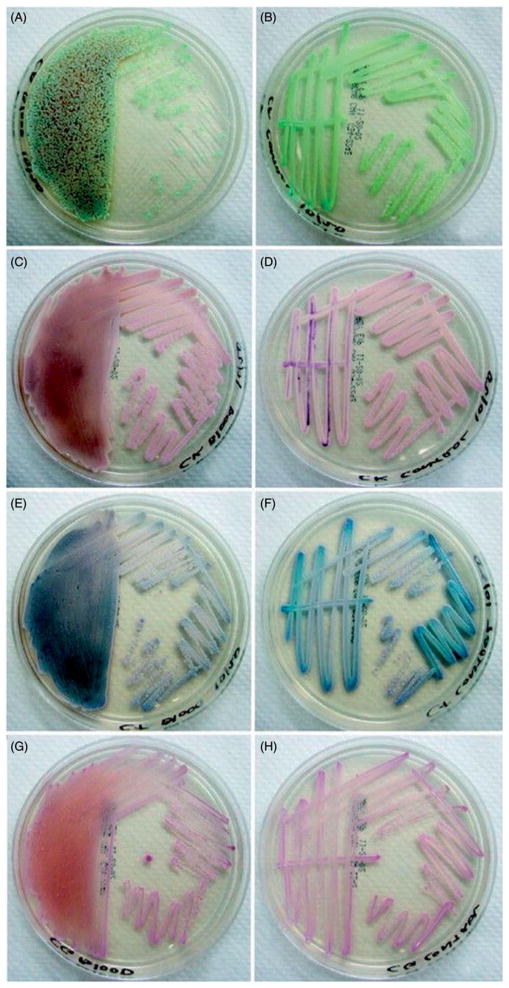
Figure 3.
Appearance of colonies on CHROMagar (Left: 1× magnification) and Corn meal-Tween 80 agar (Right: 400× magnification) after 48 h of incubation. (A) C. albicans. (B) C. dubliniensis. (C) C. tropicalis. (D) T. beigelii. (E) C. krusei. (F) C. glabrata. (G) C. parapsilosis. (H) C. neoformans. Reproduced with the permission from.[72]
C. albicans and C. dubliniensis grow germ tubes (GT) that can be used as characteristic morphological feature for rapid identification of these two Candida species.[77–79] Yeast cells can be transformed into GTs in human blood, sera, plasma and cerebrospinal fluids (CSF). Corn meal agar medium and corn meal broth are usually used as GT culture media. C. albicans developed into GTs in all of 111 test stains in 1–2 h at optimal conditions (75% corn meal broth, 37 °C).[80] Although the GT test can be used as a rapid identification test, it cannot differentiate between C. albicans and C. dubliniensis. CHROMagar defines light green color for C. albicans and dark green color for C. dubliniensis. However, it was found that CHROMagar did not give light green color for C. albicans in 49 out of 98 oral swabs from HIV-infected patients and showed green to dark green coloration similar to C. dubliniensis. A novel chromogenic medium CHROM-Pal medium (CH-P) is proposed that is modified form of CHROMagar supplemented with Pal’s agar. CH-P medium accurately differentiated C. albicans from C. dubliniensis with more than 95% detection efficiency.[81] CH-P medium has given very promising initial results, but it should be further analyzed with a wide range of rare Candida species. Notwithstanding the progress being made on chromogenic detection methods, there will probably be considerable limitations in specificity and sensitivity owing in part to differential gene expression of the targeted enzyme or substrate induced by changing environmental factors.
Overall, culture-based techniques are the most widely used methods for Candida detection in clinical applications. However, due to their time-consuming nature, it makes culture-based techniques unsuitable for rapid Candida testing.
Blood culture for Candida detection
Blood culture is one of the standard methods for fungal detection. The general technique of blood culture is based on taking 10 ml of blood injected into two or more blood bottles with specific media to culture either aerobic or anaerobic organisms.[33] If a vial test is positive, the Gram-stain can be determined in subsequent steps of the bacteria/fungal analysis.[33] Also, the blood can be subcultured onto agar plates to create distinctive colonies. A combination of blood culture and CHROMagar provides a better technique for the colony formation and detection of various Candida sub-types.[82] Horvath et al.[82] have investigated whether the colony size and shape if taken directly from blood culture were modified. In this regard, 50 clinically isolated samples from blood culture were isolated and cultured in CHROMagar.[82] Direct isolation yielded more rapid growth of colonies in the CHROMagar and consequently provided faster Candida detection analysis, despite the fact that it did not show significant changes in the colony color, shape and size (Figure 4).
Figure 4.
Detection and comparison of colonies of Candida on blood agar and CHROMagar. Growth of C. albicans (A and B), C. krusei (C and D), C. tropicalis (E and F), and C. glabrata (G and H) on CHROMagar, with direct isolation from blood culture bottled medium (A, C, E and G) compared to that seen with inoculation from culture on standard solid medium (B, D, F and H). Reproduced with the permission from.[82]
One of the most frequently used blood culture media for Candida detection is BacT/ALERT®. With the leverage of liquid emulsion sensor and colorimetric analysis, BacT/ALERT® provides color modification when the pH changes as a response to increasing CO2 concentrations.[83] Other types of blood cultures that are commonly used for Candida detection, are BD Bactec™ FX blood culture (BC) and VersaTREK™ system (aerobic redox medium).[84] BC is a fully automated culturing machine integrated with fluorescent sensors, which provides high-throughput sample analysis. VersaTREK is a type of stir bar aerobic bottle, which has the magnet bar at the bottom of the bottle. By stirring, the oxygen will distribute around the media evenly yielding uninterrupted, continuous mixing, which provides consistent fungal growth in the bottle.[85] Despite significant advances in automation and throughput analysis, blood culturing is a very time-consuming method, thus, not suitable for rapid Candida detection. In addition, it is not easily amenable to miniaturized POC use by patients or care givers.
Serological detection of Candida
Antigenic detection of Candida infections has been developed over the past 30 to 40 years and provides a viable target for Candida detection. However, there is not a general consensus on a specific antibody detection convention.[86,87] Diagnosis by serological methods is resourceful due to the following: (1) the intrinsic nature of the humoral response to Candida infection, and the production of a multitude of antibodies to many different epitopes, (2) the high sensitivity of each antigen or antibody test allows for rapid detection of Candida infection [86] and (3) antibodies can be produced in vitro to meet the demand for novel tests for antigens with highly sensitive diagnostic application.[88] The current antigen and antibody diagnostic methods require serum samples from patient blood.[86,89] Since Candida is a common skin commensal organism, exposure confers development of antibodies regardless of infection.[90] This suggests that antigenic diagnosis of Candida is a better means of a quick diagnostic tool rather than the detection of anti-Candida antibodies in sera.
Some of the simple fungal antigen testing methods include the latex-agglutination tests.[91–93] This method utilizes latex or glass beads that are coated with an antigen-specific antibody within a buffer suspension. Though an older test, latex agglutination has made re-emergence with developments in antigen-specific monoclonal antibodies in serological testing.[92,94] Mitsutaki et al.[90] evaluated polycolonal anti-Candida antibody Cand-Tec, and monoclonal anti-Candida antibody Pastorex with latex agglutination systems. It was demonstrated that the Cand-Tec assay showed a 76.9% detection rate to the enolase antigen; whereas the Pastorex assay showed a lower (25.6%) detection rate. In the monoclonal antibody system, no superficial Candida infections were detected, unlike the polycolonal system. Another diagnostic tool, western blotting (immunoblotting),[90,95] is used to detect specific fungal antigens or host antibodies present in sera. The method separates the proteins by size with gel electrophoresis, and then, the gel is blotted onto absorbent paper. On the paper, patient serum is screened for Candida antigens by precipitation upon contact with specific antibodies. Similarly, antibodies against fungal antigens can be separated and used as assays for antigen detection in sera.[95] Other antigen–antibody paper tests include the immunoprecipitation and immunodiffusion assays.[91,96,97] These assays determine the presence of antibodies against fungal antigens on the basis of antibody–antigen precipitation.
Beginning in the early 1990s, enzyme-linked immunosorbent assays (ELISA) were developed to detect antibodies against Candida and showed high specificity and sensitivity. ELISA is a standard method based on antibody/antigen detection for a wide range of infectious and opportunistic diseases and can vary in protocol depending on which identification aspect is sought.[86,96–101] The assay uses a probe substrate that upon reaction with an enzyme conjugated to a specific antibody or antigen generates a fluorophore that can be spectrophotometrically analyzed as a result of substrate catalysis.[98–100] Laín et al.[99] found that an IgG ELISA had 81.0% sensitivity to an antienolase IgG antibody and showed 88.9% sensitivity to IgG antibody against an N-terminal hyphal wall protein.[98] The ease and practicality of these tests for anti-Candida IgG antibodies enables the development of a sensitive tool for early diagnosis of infection. Clancy et al.[86] recently used IgG ELISA to measure responses from a panel of antigens to accurately determine early infection markers of candidiasis. ELISA can also play a role for the evaluation of patient antibody responses as a quantification tool of antibody titer, and Fujita et al.[97] used this to show the various stages of diagnosis during the disease course, as well as mapped the increase in antibody titer against Candida. Although a useful tool, ELISA still must be further developed to a high level of consistency before becoming a standard for the antibody detection of Candida infection.
Several monoclonal antibodies have been produced against specific Candida antigens.[88,102,103] Reiss et al.[88] found that monoclonal antibodies directed against mannan components of the Candida cell wall were useful in antigen detection tests. Many of the antibodies produced confer the same reactivity as in vivo host antibodies.[102] A disadvantage to monoclonal antibody detection methods results from the high specificity of the monoclonal antibody epitope to the particular fungal antigen. This limited scope of the full antigenic epitope is prone to bias the ability of monoclonal antibody tests to detect antigens from the multiple strains of Candida as shown by Marot-Lebond et al.[92] Although minimal, monoclonal antibody testing has shown cross reactivity to other non-Candida antigens, which risks false-positive results.[104,105] Recently, in 2007, Rodriguez et al.[105] described a monoclonal antibody that cross-reacted with an overexpressed nuclear pore complex protein, Nup88, found in oral squamous cell carcinomas. This suggests that due to cross reactivity of the antibody, risk of generating false-positive results exists.
Polyclonal and monoclonal antibodies are also being used for immunofluorescence analysis of Candida. The production of specific antibodies for Candida has proved to be extremely difficult as antibodies often cross react with other fungi. Generally speaking, the antibodies specific for Candida spp. are useful in differentiating infections caused by various Candida spp. from other fungi.[106] Scientists have successfully produced a monoclonal antibody (Mab), 3H8, specific to C. albicans.[107] The 3H8 antibody recognizes mannoprotein, antigen present on the C. albicans cell wall, whereas this antigen is partially cryptic in cell walls of other Candida spp. (C. glabrata, C. parapsilosis, C. tropicalis and C. krusei).[107–109] The 3H8 Mab was used in successful identification of C. albicans from various body tissues, including lung, kidney, thyroid, small bowel and esophagus tissue.[109] Bikandi et al.[110] have accurately differentiated C. albicans from C. dubliniensis based on their immunofluorescence using 3H8 Mab. Jarvensivu et al.[111] have also reported the specific immunohistochemical identification of C. albicans using 3H8 Mab. These results are promising and antibodies can help in rapid Candida detection, but these antibodies should be tested with many clinical samples and blood cultures specimens before reaching any conclusion. Secondly, tremendous effort is needed to produce specific antibodies for other species of Candida. Overall, immunoassay-based techniques provide rapid tests. However, the main drawbacks are low specificity and cross-reactivity with other antibodies/antigens.
Nucleic acid detection of candida
Nucleic acid (NA)-based detection plays an important role in the identification of fungal analytes by providing sensitive and specific bioassays. There are major reasons that make this technique one of the most robust approaches [112]: (1) all living organisms have NAs in their cell body; (2) NAs regardless if they are single stranded or double stranded, they consist of only four different base pairs, which are relatively easy to detect; (3) NAs are easy to manipulate; and (4) there are very well established technologies existing that can replicate specific sequences of NAs at relatively low cost.[112] The use of molecular diagnostics for the detection of specific sequence of fungus has been reviewed.[113,114] NA-based detection or molecular diagnostics can be implemented based on hybridization techniques, microarrays and amplification. One of the most challenging steps when using these techniques is sample preparation. This consists of DNA extraction and purification steps to release the intracellular DNA from the fungus, concentration of the target DNA and removal of potential inhibitors, debris and contaminants.[115]
DNA microarray techniques have emerged as a viable platform for Candida detection. Thousands of gene-specific probes are attached to the surface of solid substrate, such as silicon wafer, glass or nylon. These probes are designed in a way to be complementary to target organism genome DNA sequences. Then, the sequences are queried by a label (fluorescent or radioactive labels). Once the sample is added to the microarray, either in bulk or with the help of some liquid handling device such as microfluidics, hybridization takes place. The array is then scanned to visualize the fluorescent pattern tilled on the surface of the substrate, and the pattern is determined using microarray reader. Various microarrays have been developed to detect Candida.[116–118] Leinberger et al.[118] have developed a microarray for the identification and detection of 12 different spp. of Candida and Aspergillus. Oligonucleotic probes were designed to detect the internal transcribed spacer (ITS) region of the rRNA gene. The whole process after DNA extraction took 4 h and showed a robust platform for clinical diagnostics by testing 21 unknown clinical patient samples on a micro-array. The microarray was simultaneously amplified with multiplex polymerase chain reaction (PCR) and labeled with a fluorescent dye for the sensitive detection of Candida. In a similar example, Spiess et al.[117] developed a microarray with multiplex PCR to detect 14 fungal Candida spp. from high-risk patient samples (22 patients) including blood, bronchoalveolar lavage and tissues. Although the assay is rapid, their sensitivity is often lower than amplification techniques.[119]
Since quantities of the NAs are relatively small, amplification techniques are routinely employed. Amplification techniques can be divided into two groups, namely (i) isothermal and (ii) nonisothermal [163] techniques.[112] Since its first publication in 1986,[120] PCR is the most commonly known because of a nonisothermal amplification technique for the detection of bio-analytes and it has been exploited for Candida detection.[121–124] The process is based on three different reactions to amplify DNA by leveraging thermal cycling: (1) denaturation that makes double-stranded DNA into the single-stranded template at stringent temperature conditions, (2) annealing, which matches specifically designed primers to attach a single-stranded DNA template at stringent temperatures and (3) extension using polymerase enhances the polymerase reaction activity by generating a new strand, which is complementary to the single-strand sequence. Various PCR techniques have been developed based on different applications, such as multiplexed PCR (for the detection of various analytes in a sample), real-time PCR (for monitoring amplification in real time format), reverse-transcriptase PCR (RT-PCR) for the amplification of RNA templates, and nested PCR for increasing the specificity by using two pairs of primers to avoid unexpected primer binding and nonspecific amplification.
The requirement to use three different temperatures during PCR switched the attention into the development of isothermal amplification. There are various different isothermal amplification techniques that were used for NA amplification and detection such as (1) loop-mediated isothermal amplification (LAMP), (2) NA sequence-based amplification (NASBA), (3) rolling circle amplification (RCA) and (4) strand displacement amplification (SDA). Table 3 shows the different amplification methods used for Candida detection. For example, Inàcio et al.[85] used the LAMP technique for amplification of the 26S rRNA gene in clinically relevant Candida yeast. The amplification occurred at 64 °C for 90 min with the sensitivity as low as 50 fg. In another example, Widjojoatmodjo et al.[125] employed NASBA for the detection of 19 different Candida subtypes from 18s rRNA sequences at 41 °C with the detection limit of 0.01 CFU/ml. In the similar effort, Zhou et al.[126] detected 18 different Candida subtypes Candida based on RCA amplification in 2 h by synthesizing an RCA padlock probe. Overall, NA-based detection methods are the most accurate and precise techniques for screening Candida and various fungi. However, these methods are multistep and require sample purification, NA extraction prior to the detection step, a time-consuming process.
Table 3.
Commercially available platforms for Candida detection.
| Product name | Cost/test | Sensitivity | Specificity | References |
|---|---|---|---|---|
| SeptiFast | 100–180$ | 75% | 92% | [130] |
| SepsiTest | 83.5 $ | 87.0% | 85.8% | [131] |
| VYOO | TBD | Range of 38.0–60.0% | 77% | [147] |
| Magicplex sepsis real-time test | TBD | 65.0% | 92.0%, | [133] |
| T2Dx | TBD | 91.1% | 99.4% | [156] |
| T2MR | TBD | 91.1% | 99.4% | [148] |
| Unimedi Candida | TBD | 82% | 96% | [128,157] |
| Bruker Autoflex III MALDI-TOF | TBD | 91.7% | 97% | [132,158] |
Nonconventional detection for Candida: lab chip (LOC) devices for Candida detection
With the development of micro total analysis systems (μTAS), various (LOC) devices have been developed for pathogen detection.[38,127–146, 164] Microfluidic LOC devices enhance early detection and identification of fungi in the blood stream. This technology allows for a device to be used in resource-constrained settings where there are no centralized laboratories available for implementing conventional culturing techniques.[132,133,147,148] However, the development of fungal detection based on NA requires various steps, including cell lysis, NA extraction and purification, together with the removal of possible inhibitors of PCR amplification.[149] For example, Cai et al. [150] have developed a microfluidic platform based on SlipChip® to simultaneously detect multiple fungi including Candida spp. such as C. glabrata, C. albicans, C. krusei, C. parapsilosis and other pathogens from blood samples. This was performed by combining multiplex PCR amplification and dielectrophoresis (DEP) for the separation of 20 different pathogens and fungi from blood samples followed by fluorescent detection within 3 h (Figure 5A).
Figure 5.
Microchips for Candida detection. (A) Integration of SlipChip and Dielectrophoresis (DEP) for fungal separation and PCR amplification. (a) Schematic workflow process of fungal and pathogen detections from blood sample taken from patient using multiplex PCR. (b) Photograph of the chip loaded with food dye. (c–f) Water diluted sample, containing blood were mixed properly with the blood cell ghost (BCGs), fungal and pathogens and was injected into the channels. (g–k) The top plate consists of PCR mixture and the bottom plate has the pathogens and fungal spp. that are separated by the DEP and the contaminant is washed away. The bottom plate is slip back to be mixed with the captured pathogens and then initiates PCR reaction followed by fluorescent detection. (B) (a–c) Image of the advanced liquid logic chip, its reader and fully assembled microwell cartridge showing location of sample, reagent wells, and other solutions. (d) Schematic of the on/off magnet to merge the droplets, extend the droplet into the column, and split two droplets. (e) The droplet logic has been used for extraction, washing, purification and elution of DNA from beads over the magnet. (C) Fraunhofer iVD platform. (a–b) Schematic and image of the Fraunhofer iVD cartridge consists of the total internal reflectance fluorescence (TRIF) optical sensor as well as electrochemical sensor. The cartridge was fabricated based on half microtiter plate (credit card size) and has various micropumps and eight reservoirs for sample and reagent storage. The amplified product is pumped to the TRIF sensor or electrochemical sensor for further analysis. (c) Images of TRIF sensor for various pathogen; E. coli, S. aureus, P. aeroginose, and C. albican. Reproduced with the permission from [150,153,161].
Digital microfluidics has also emerged as a robust platform for fungal detection. Boles et al.[151] have developed droplet-based microfluidic leveraging electrowetting concept to control and manipulate droplet samples for implication of various concepts such as merging liquid, mixing and moving to different regions of the chip. By combining the magnetic force and electro-wetting, the ability to merge, extend and move droplets to each direction allows for the implementation of various steps required for PCR, such as DNA extraction, purification and transfer to different thermal zones. Using this technique, Schell et al.[152] have employed an advanced liquid logic chip for the detection of C. albicans from blood samples collected from 16 candidemia patients. The DNA extraction was implemented off-chip and the purified DNA was applied to the biochip. Using this method, sensitivity of 56% (compared to 69% of conventional PCR real-time analysis) has been achieved within 45 min (Figure 5B). Other types of highly integrated LOC platforms have also been developed for in vitro Candida diagnosis. Schumacher et al.[153] have developed a Fraunhofer ® LOC platform for in vitro diagnosis of various fungi and pathogens using PCR by leveraging optical sensing and electrochemical sensing in a single platform (Figure 5C).
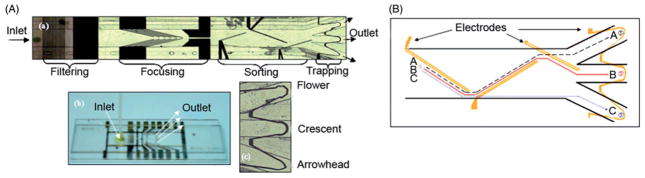
Microchip PCR has the robust ability to identify and quantify various species in biosamples. However, the main drawback is that these technologies are unable to determine the viability of the fungus or other pathogens. Another alternative is based on Raman spectroscopy that measures the distinct vibration spectrum of various molecules and structures such as DNA, cells and live/dead fungus.[24] This technique has been implemented for the detection of various Candida spp. which have been cultured on Sabouraud medium or blood culture. A modification of Raman spectroscopy, surface-enhanced Raman spectroscopy (SERS), employs metal nanoparticles (gold or silver) to enhance the intensity of Raman scattering. These metal nanoparticles are either attached chemically to the fungus/bacteria wall, or settle down in the proximity of pathogen. Combining the SERS technique for detection and DEP method for cell separation on a chip can provide rapid tools for multiplex Candida detection. Cheng et al.[24] have fabricated a microfluidic chip by combining planar electrodes into 3D DEP gates with latex beads to separate various pathogens such as C. albicans E. coli and Lactobacillus (Figure 6).
Figure 6.
Integrated DEP and SERS chip for Candida detection. (A) Microimage of integrated DEP chip consists of several sections of filtering, focusing, sorting and separation. (B) Schematic representation of 3D electrode configuration for the separation of different particles including C. albicans which is detected by SERS. Reproduced with the permission from [24].
A combination of field effect transistor (FET) and single wall carbon nanotube (SWCNT) has also been used for Candida detection. Villamizar et al.[32] have fabricated SWCNT-FET transistor based on chemical vapor deposition (CVD) on a silicon chip. The source and drain electrodes were screen-printed electrodes and have been fabricated using Ag ink. Monoclonal anti-Candida antibodies have been immobilized on the surface of SWCNT, and the selectivity of the assay has been analyzed with Cryptococcus albidus and Saccharomyces cerevisiae. A limit of detection (LOD) of 50 CFU/ml has been achieved within 1 h.
Nucleic magnetic resonance (NMR) is another useful technique for the diagnosis of biomolecules based on nuclei absorbance and the remittance of electromagnetic radiation in the presence of a magnetic field. NMR has the ability to detect the target with high sensitivity in highly turbid samples such as urine, blood, serum, without implementing any filtration or purification step. Miniaturization of NMR can target and quantify multiplex bioanalytes such as various proteins and fungi. Lee et al.[154] have developed NMR-chip for multiplex target detection utilizing self-amplification of magnetic nanoparticles. Magnetic nanoparticles bind to the target through affinity ligand such as an antibody and form a magnetic cluster. The magnetic cluster corresponds to a decrease in bulk spin-spin relaxation time of surrounding molecules. The assay consists of NMR electronics, RF microcoils for NMR measurement and a microfluidic network for sample and permanent magnets. A 1.0 pM sensitivity has been achieved for multiple targets including S. aureus and others, as well as mammalian cells which was in agreement with benchmark detection using an NMR system. In a similar approach, a new device has been introduced by T2 Biosystem Inc. for the detection of the Candida amplicon by using a simple PCR tube for sample handling instead of a microfluidic chip and has a sensitivity of 10 CFU/ml.[23] Supernatant removal has been implemented off-chip by centrifugation followed by chemical lysis. Following the PCR, magnetic beads that have been attached to the PCR amplicon are incubated for 20–30 min before NMR T2 measurement. Table 3 shows comparison of various commercially available platforms for Candida detection. These platforms are categorized based on their sensitivity, specificity and cost per test. One of the more successful commercial systems is the T2X platform, made by T2 Biosystem that utilizes T2 magnetic resonance (T2MR) approach. Particles coated with target-specific agent form clusters when bound to a specific pathogens. These clusters alter the microscopic environment of the water molecules around the target, which can be monitored in the presence of the magnetic field. As low as 1 CFU/ml of Candida is reported to be detected within 3–5 h without the need for sample purification steps.[137]
Summary and future perspective
Various technologies have been reviewed for Candida detection with significant development observed in rapid and more effective clinical diagnostics. Although cell culture-based methods are still the gold standard for Candida detection, NA-based diagnostic assays utilizing various amplification approaches provide a more sensitive and faster test analysis for fungal detection. One of the attractive amplification methods is LAMP, which can potentially reduce the test time, as it does not require thermal cycling and thermal ramping. Therefore, we envision that the integration of LAMP-based approaches with microfluidic-based platforms can potentially lead to the development of compact, self-contained and rapid POC assays for Candida detection.
Microfluidics is on the brink of decentralized testing.[155–158] These devices provide the opportunity for patients to monitor their own health condition without the need to seek consultation in the doctor’s office. It is, however, important to consider the manufacturing ability to mass-produce low-cost microfluidic-based platforms as POC diagnostics that can meet the market demands and the guidelines made by public health agencies. For example, paper-based microchip technologies [115,132,147,159,160] integrated with optical/electrical sensing modalities may open a promising avenue in the development of POC diagnostics for Candida detection.
Acknowledgments
Funding information
This study was supported by College of Engineering and Computer Science, Florida Atlantic University through startup research support (to WA), and the National Institute of Health under award numbers R15AI127214 (to WA and HS), R01AI118502, F32AI102590 (to HS), Brigham and Women’s Hospital and Harvard Medical School through Bright Futures Prize, Innovation Evergreen Fund, and Fund to Sustain Research Excellence (to HS), National Science and Engineering Council of Canada (NSERC) through a NSERC Postdoctoral Scholarship (to MS), and Scientific WAQF Fund at King Abdulaziz University (KAU), Jeddah under grant number 17/1436 (to HS and AM). We would also like to thank The Graduate Research and Inquiry Program (GRIP), Florida Atlantic University to provide student research support to Chad Coarsey.
Footnotes
Disclosure statement
The authors report no declarations of interest.
References
- 1.De Hoog G, Guarro J, Gene J, et al. Atlas of clinical fungi Centraalbureau voor Schimmelcultures. Universitat Rovira i Virgili, Amer Society for Microbiology; 2000. pp. 164–174. [Google Scholar]
- 2.Fridkin SK, Jarvis WR. Epidemiology of nosocomial fungal infections. Clin Microbiol Rev. 1996;9:499–511. doi: 10.1128/cmr.9.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guarro J, Gené J, Stchigel AM. Developments in fungal taxonomy. Clin Microbiol Rev. 1999;12:454–500. doi: 10.1128/cmr.12.3.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phaff HJ. Yeasts eLS. 2001. pp. 1–11. [Google Scholar]
- 5.Kulp K. Handbook of Cereal Science and Technology, Revised and Expanded. CRC; 2000. [Google Scholar]
- 6.Christian V, Shrivastava R, Shukla D, et al. Degradation of xenobiotic compounds by lignin-degrading white-rot fungi: enzymology and mechanisms involved. Indian J Exp Biol. 2005;43:301. [PubMed] [Google Scholar]
- 7.Fincham J. Transformation in fungi. Microbiol Rev. 1989;53:148–170. doi: 10.1128/mr.53.1.148-170.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hawkins KM, Smolke CD. Production of benzylisoquinoline alkaloids in Saccharomyces cerevisiae. Nat Chem Biol. 2008;4:564–573. doi: 10.1038/nchembio.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang B, Guo J, Yi B, et al. Heterologous production of secondary metabolites as pharmaceuticals in Saccharomyces cerevisiae. Biotechnol Lett. 2008;30:1121–1137. doi: 10.1007/s10529-008-9663-z. [DOI] [PubMed] [Google Scholar]
- 10.Joseph B, Ramteke PW, Thomas G. Cold active microbial lipases: some hot issues and recent developments. Biotechnol Adv. 2008;26:457–470. doi: 10.1016/j.biotechadv.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Kendrick B. Fungi: ecological importance and impact on humans. eLS. 2001 [Google Scholar]
- 12.Murray PR, Rosenthal KS, Pfaller MA. Medical microbiology. 7. Vol. 44. Philadelphia, PA: Elsevier Saunders; 2013. Opportunistic mycoses/candidiasis; pp. 6776–6783. [Google Scholar]
- 13.Pappas PG. Opportunistic fungi: a view to the future. Am J Med Sci. 2010;340:253–257. doi: 10.1097/MAJ.0b013e3181e99c88. [DOI] [PubMed] [Google Scholar]
- 14.Michallet M, Ito JI. Approaches to the management of invasive fungal infections in hematologic malignancy and hematopoietic cell transplantation. J Clin Oncol. 2009;27:3398–3409. doi: 10.1200/JCO.2008.20.1178. [DOI] [PubMed] [Google Scholar]
- 15.Baddley JW, Stroud TP, Salzman D, et al. Invasive mold infections in allogeneic bone marrow transplant recipients. Clin Infect Dis. 2001;32:1319–1324. doi: 10.1086/319985. [DOI] [PubMed] [Google Scholar]
- 16.Person AK, Kontoyiannis DP, Alexander BD. Fungal infections in transplant and oncology patients. Hematol Oncol Clin North Am. 2011;25:193–213. doi: 10.1016/j.hoc.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Kaufman D. Fungal infections in neonates: update on prevention and treatment. Minerva Ginecol. 2007;59:311–329. [PubMed] [Google Scholar]
- 18.Smith JA, Kauffman CA. Recognition and prevention of nosocomial invasive fungal infections in the intensive care unit. Crit Care Med. 2010;38:S380–S387. doi: 10.1097/CCM.0b013e3181e6cf25. [DOI] [PubMed] [Google Scholar]
- 19.Lionakis MS, Kontoyiannis DP. Glucocorticoids and invasive fungal infections. The Lancet. 2003;362:1828–1838. doi: 10.1016/S0140-6736(03)14904-5. [DOI] [PubMed] [Google Scholar]
- 20.Sullivan D, Coleman D. Candida dubliniensis: characteristics and identification. J Clin Microbiol. 1998;36:329–334. doi: 10.1128/jcm.36.2.329-334.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zilberberg MD, Shorr AF, Kollef MH. Secular trends in candidemia-related hospitalization in the United States, 2000–2005. Infect Control Hosp Epidemiol. 2008;29:978–980. doi: 10.1086/591033. [DOI] [PubMed] [Google Scholar]
- 22.Ferwerda G, Meyer-Wentrup F, Kullberg BJ, et al. Dectin-1 synergizes with TLR2 and TLR4 for cytokine production in human primary monocytes and macrophages. Cell Microbiol. 2008;10:2058–2066. doi: 10.1111/j.1462-5822.2008.01188.x. [DOI] [PubMed] [Google Scholar]
- 23.Neely LA, Audeh MJ, Blanco M, et al., inventors. T2 Biosystems, Inc, assignee. NMR systems and methods for the rapid detection of analytes. 8409807 B2. United States patent US. 2012
- 24.Cheng IF, Chang HC, Hou D, et al. An integrated dielectrophoretic chip for continuous bioparticle filtering, focusing, sorting, trapping, and detecting. Biomicrofluidics. 2007;1:021503. doi: 10.1063/1.2723669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naglik JR, Challacombe SJ, Hube B. Candida albicans secreted aspartyl proteinases in virulence and pathogenesis. Microbiol Mol Biol Rev. 2003;67:400–428. doi: 10.1128/MMBR.67.3.400-428.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whiteway M, Oberholzer U. Candida morphogenesis and host-pathogen interactions. Curr Opin Microbiol. 2004;7:350–357. doi: 10.1016/j.mib.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Jarvis WR. Epidemiology of nosocomial fungal infections, with emphasis on Candida species. Clin Infect Dis. 1995;20:1526–1530. doi: 10.1093/clinids/20.6.1526. [DOI] [PubMed] [Google Scholar]
- 28.Jarvis WR, Martone WJ. Predominant pathogens in hospital infections. J Antimicrob Chemother. 1992;29:19. doi: 10.1093/jac/29.suppl_a.19. [DOI] [PubMed] [Google Scholar]
- 29.Richards MJ, Edwards JR, Culver DH, et al. Nosocomial infections in medical intensive care units in the United States. Crit Care Med. 1999;27:887. doi: 10.1097/00003246-199905000-00020. [DOI] [PubMed] [Google Scholar]
- 30.Richards MJ, Edwards JR, Culver DH, et al. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000;21:510–515. doi: 10.1086/501795. [DOI] [PubMed] [Google Scholar]
- 31.Edmond MB, Wallace SE, McClish DK, et al. Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis. 1999;29:239–244. doi: 10.1086/520192. [DOI] [PubMed] [Google Scholar]
- 32.Villamizar RA, Maroto A, Riusa FX, et al. Fast detection of Salmonella Infantis with carbon nanotube field effect transistors. Biosens Bioelectron. 2008;24:279–283. doi: 10.1016/j.bios.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 33.Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006;19:788–802. doi: 10.1128/CMR.00062-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morgan J, Meltzer MI, Plikaytis BD, et al. Excess mortality, hospital stay, and cost due to candidemia: a case-control study using data from population-based candidemia surveillance. Infect Control. 2005;26:540–547. doi: 10.1086/502581. [DOI] [PubMed] [Google Scholar]
- 35.Wey SB, Mori M, Pfaller MA, et al. Hospital-acquired candidemia. The attributable mortality and excess length of stay. Arch Inter Med. 1988;148:2642. doi: 10.1001/archinte.148.12.2642. [DOI] [PubMed] [Google Scholar]
- 36.Fraser VJ, Jones M, Dunkel J, et al. Candidemia in a tertiary care hospital: epidemiology, risk factors, and predictors of mortality. Clin Infect Dis. 1992;15:414–421. doi: 10.1093/clind/15.3.414. [DOI] [PubMed] [Google Scholar]
- 37.Leleu G, Aegerter P, Guidet B. Systemic candidiasis in intensive care units: a multicenter, matched-cohort study. J Critical Care. 2002;17:168–175. doi: 10.1053/jcrc.2002.35815. [DOI] [PubMed] [Google Scholar]
- 38.Méan M, Marchetti O, Calandra T. Bench-to-bedside review: Candida infections in the intensive care unit. Crit Care. 2008;12:204. doi: 10.1186/cc6212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saghrouni F, Ben Abdeljelil J, Boukadida J, et al. Molecular methods for strain typing of Candida albicans: a review. J Appl Microbiol. 2013;114:1559–1574. doi: 10.1111/jam.12132. [DOI] [PubMed] [Google Scholar]
- 40.Jain N, Mathur P, Misra MC, et al. Rapid identification of yeast isolates from clinical specimens in critically Ill trauma ICU patients. J Lab Physicians. 2012;4:30. doi: 10.4103/0974-2727.98667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zilberberg MD, Kollef MH, Arnold H, et al. Inappropriate empiric antifungal therapy for candidemia in the ICU and hospital resource utilization: a retrospective cohort study. BMC Infect Dis. 2010;10:150. doi: 10.1186/1471-2334-10-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rex JH, Pfaller MA, Barry AL, et al. Antifungal susceptibility testing of isolates from a randomized, multicenter trial of fluconazole versus amphotericin B as treatment of nonneutropenic patients with candidemia. NIAID Mycoses study group and the Candidemia study group. Antimicrob Agents Chemother. 1995;39:40–44. doi: 10.1128/aac.39.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wingard JR, Merz WG, Rinaldi MG, et al. Association of Torulopsis glabrata infections with fluconazole prophylaxis in neutropenic bone marrow transplant patients. Antimicrob Agents Chemother. 1993;37:1847–1849. doi: 10.1128/aac.37.9.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Canuto MM, Rodero FG. Antifungal drug resistance to azoles and polyenes. Lancet Infect Dis. 2002;2:550–563. doi: 10.1016/s1473-3099(02)00371-7. [DOI] [PubMed] [Google Scholar]
- 45.Rangel-Frausto MS, Wiblin T, Blumberg HM, et al. National epidemiology of mycoses survey (NEMIS): variations in rates of bloodstream infections due to Candida species in seven surgical intensive care units and six neonatal intensive care units. Clin Infect Dis. 1999;29:253–258. doi: 10.1086/520194. [DOI] [PubMed] [Google Scholar]
- 46.Pfaller MA, Diekema DJ, Jones RN, et al. International surveillance of bloodstream infections due to Candida species: frequency of occurrence and in vitro susceptibilities to fluconazole, ravuconazole, and voriconazole of isolates collected from 1997 through 1999 in the SENTRY antimicrobial surveillance program. J Clin Microbiol. 2001;39:3254–3259. doi: 10.1128/JCM.39.9.3254-3259.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agarwal S, Manchanda V, Verma N, et al. Yeast identification in routine clinical microbiology laboratory and its clinical relevance. Indian J Med Microbiol. 2012;29:172. doi: 10.4103/0255-0857.81794. [DOI] [PubMed] [Google Scholar]
- 48.Larone DH. Medically important fungi: a guide to identification. 2. New York: Elsevier Science Publishing Co; 1987. [Google Scholar]
- 49.Koneman EW, Roberts GD. Practical laboratory mycology. Baltimore, MD: Williams & Wilkins; 1985. [Google Scholar]
- 50.Adams AEM, Stearns TIM. Fluorescence microscopy methods for yeast. Methods in cell biology, volume 31: Vesicular transport, Part A: Vesicular transport. 1989:357. doi: 10.1016/s0091-679x(08)61620-9. [DOI] [PubMed] [Google Scholar]
- 51.Hageage GJ, Harrington BJ. Use of calcofluor white in clinical mycology. Lab Med. 1984;15:109–112. [Google Scholar]
- 52.Perry JL, Miller GR. Quality control slide for potassium hydroxide and cellufluor fungal preparations. J Clin Microbiol. 1989;27:1411–1412. doi: 10.1128/jcm.27.6.1411-1412.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ruiz-Herrera J. Fungal cell wall: structure, synthesis, and assembly. Boca Raton, Florida: CRC press; 1991. [Google Scholar]
- 54.Harrington BJ, Hageage GJ. Calcofluor white: a review of its uses and applications in clinical mycology and parasitology. Lab Med. 2003;34:361–367. [Google Scholar]
- 55.Harrington BJ, Williams DL. Rapid, presumptive identification of Torulopsis (Candida) Glabrata and Candida Krusei using Calcofluor White. Lab Med. 2007;38:227–231. [Google Scholar]
- 56.Baselski VS, Robison MK, Pifer LW, et al. Rapid detection of Pneumocystis carinii in bronchoalveolar lavage samples by using Cellufluor staining. J Clin Microbiol. 1990;28:393–394. doi: 10.1128/jcm.28.2.393-394.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sautter RL, Kwee HG. Calcofluor white stain for fungi. Am J Clin Pathol. 1987;87:295. doi: 10.1093/ajcp/87.2.295a. [DOI] [PubMed] [Google Scholar]
- 58.Lischewski A, Kretschmar M, Hof H, et al. Detection and identification of Candida species in experimentally infected tissue and human blood by rRNA-specific fluorescent in situ hybridization. J Clin Microbiol. 1997;35:2943–2948. doi: 10.1128/jcm.35.11.2943-2948.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bisha B, Kim HJ, Brehm-Stecher BF. Improved DNA-FISH for cytometric detection of Candida spp. J Appl Microbiol. 2011;110:881–892. doi: 10.1111/j.1365-2672.2011.04936.x. [DOI] [PubMed] [Google Scholar]
- 60.Rigby S, Procop GW, Haase G, et al. Fluorescence in situ hybridization with peptide nucleic acid probes for rapid identification of Candida albicans directly from blood culture bottles. J Clin Microbiol. 2002;40:2182–2186. doi: 10.1128/JCM.40.6.2182-2186.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Trnovsky J, Merz W, Della-Latta P, et al. Rapid and accurate identification of Candida albicans isolates by use of PNA FISHFlow. J Clin Microbiol. 2008;46:1537–1540. doi: 10.1128/JCM.00030-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gherna M, Merz WG. Identification of Candida albicans and Candida glabrata within 1.5 hours directly from positive blood culture bottles with a shortened peptide nucleic acid fluorescence in situ hybridization protocol. J Clin Microbiol. 2009;47:247–248. doi: 10.1128/JCM.01241-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Borekci G, Ersoz G, Otag F, et al. Identification of Candida species from blood cultures with fluorescent in situ hybridization (FISH), polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) and conventional methods. Balkan Med J. 2010;27:183–191. [Google Scholar]
- 64.Kempf VAJ, Trebesius K, Autenrieth IB. Fluorescent in situ hybridization allows rapid identification of micro-organisms in blood cultures. J Clin Microbiol. 2000;38:830–838. doi: 10.1128/jcm.38.2.830-838.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rij KV. A taxonomic study. New York, NY: Elsevier Science Publishers BV; 1984. The yeasts. [Google Scholar]
- 66.Espinel-Ingroff A, Stockman L, Roberts G, et al. Comparison of RapID yeast plus system with API 20C system for identification of common, new, and emerging yeast pathogens. J Clin Microbiol. 1998;36:883–886. doi: 10.1128/jcm.36.4.883-886.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davey KG, Chant PM, Downer CS, et al. Evaluation of the AUXACOLOR system, a new method of clinical yeast identification. J Clin Pathol. 1995;48:807–809. doi: 10.1136/jcp.48.9.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.El-Zaatari M, Pasarell L, McGinnis MR, et al. Evaluation of the updated Vitek yeast identification data base. J Clin Microbiol. 1990;28:1938–1941. doi: 10.1128/jcm.28.9.1938-1941.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fenn JP, Segal H, Barland B, et al. Comparison of updated Vitek yeast biochemical card and API 20C yeast identification systems. J Clin Microbiol. 1994;32:1184–1187. doi: 10.1128/jcm.32.5.1184-1187.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Campbell CK, Davey KG, Holmes AD, et al. Comparison of the API Candida system with the AUXACOLOR system for identification of common yeast pathogens. J Clin Microbiol. 1999;37:821–823. doi: 10.1128/jcm.37.3.821-823.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Verweij PE, Breuker IM, Rijs AJ, et al. Comparative study of seven commercial yeast identification systems. J Clin Pathol. 1999;52:271–273. doi: 10.1136/jcp.52.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Koehler AP, Chu KC, Houang ETS, et al. Simple, reliable, and cost-effective yeast identification scheme for the clinical laboratory. J Clin Microbiol. 1999;37:422–426. doi: 10.1128/jcm.37.2.422-426.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Willinger B, Manafi M. Evaluation of CHROMagar Candida for rapid screening of clinical specimens for Candida species. Mycoses. 2002;42:61–65. doi: 10.1046/j.1439-0507.1999.00406.x. [DOI] [PubMed] [Google Scholar]
- 74.Adam HJ, Richardson SE, Roscoe M, et al. An implementation strategy for the use of chromogenic media in the rapid, presumptive identification of Candida species. Open Mycol J. 2010;4:33–38. [Google Scholar]
- 75.Pfaller MA, Houston A, Coffmann S. Application of CHROMagar Candida for rapid screening of clinical specimens for Candida albicans, Candida tropicalis, Candida krusei, and Candida (Torulopsis) glabrata. J Clin Microbiol. 1996;34:58–61. doi: 10.1128/jcm.34.1.58-61.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sivakumar VG, Shankar P, Nalina K, et al. Use of CHROMagar in the differentiation of common species of Candida. Mycopathologia. 2009;167:47–49. doi: 10.1007/s11046-008-9149-5. [DOI] [PubMed] [Google Scholar]
- 77.Sudbery P, Gow N, Berman J. The distinct morphogenic states of Candida albicans. Trends Microbiol. 2004;12:317–324. doi: 10.1016/j.tim.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 78.Whiteway M, Bachewich C. Morphogenesis in Candida albicans*. Annu Rev Microbiol. 2007;61:529–553. doi: 10.1146/annurev.micro.61.080706.093341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kadosh D, Johnson AD. Induction of the Candida albicans filamentous growth program by relief of transcriptional repression: a genome-wide analysis. Mol Biol Cell. 2005;16:2903–2912. doi: 10.1091/mbc.E05-01-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nakamoto S. Germ tube formation of Candida albicans in corn meal broth using the non-slip slide glass incubation method. Yonago Acta Medica. 1998;41:65–72. [Google Scholar]
- 81.Sahand IH, Maza JL, Eraso E, et al. Evaluation of CHROM-Pal medium for the isolation and direct identification of Candida dubliniensis in primary cultures from the oral cavity. J Med Microbiol. 2009;58:1437–1442. doi: 10.1099/jmm.0.011320-0. [DOI] [PubMed] [Google Scholar]
- 82.Horvath LL, Hospenthal DR, Murray CK, et al. Direct isolation of Candida spp. from blood cultures on the chromogenic medium CHROMagar Candida. J Clin Microbiol. 2003;41:2629–2632. doi: 10.1128/JCM.41.6.2629-2632.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.BacT/ALERT® MB, BioMerieux. [cited 2015 Dec 26]. Available from: http://www.biomerieux-usa.com/clinical/bact-alert-3d-healthcare.
- 84.TREK Diagnostic System. [cited 2015 Feb 04]. Available from: http://www.trekds.com/products/ver-satrek/media.asp.
- 85.João Inácio OFaIS-M. Efficient identification of clinically relevant Candida yeast species by use of an assay combining Panfungal loop-mediated isothermal DNA amplification with hybridization to species-specific oligonucleotide probes. J Clin Microbiol. 2008;46:713–720. doi: 10.1128/JCM.00514-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Clancy CJ, Nguyen ML, Cheng S, et al. Immunoglobulin G responses to a panel of Candida albicans antigens as accurate and early markers for the presence of systemic candidiasis. J Clin Microbiol. 2008;46:1647–1654. doi: 10.1128/JCM.02018-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Medical microbiology. 7. Philadelphia, PA: Elsevier Saunders; 2013. [Google Scholar]
- 88.Reiss E, De Repentigny L, Kuykendall R, et al. Monoclonal antibodies against Candida tropicalis mannan: antigen detection by enzyme immunoassay and immunofluorescence. J Clin Microbiol. 1986;24:796–802. doi: 10.1128/jcm.24.5.796-802.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Philip A, Odabasi Z, Matiuzzi G, et al. Syscan3, a kit for detection of anti-candida antibodies for diagnosis of invasive candidiasis. J Clin Microbiol. 2005;43:4834–4835. doi: 10.1128/JCM.43.9.4834-4835.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mitsutake K, Miyazaki T, Tashiro T, et al. Enolase antigen, mannan antigen, Cand-Tec antigen, and beta-glucan in patients with candidemia. J Clin Microbiol. 1996;34:1918–1921. doi: 10.1128/jcm.34.8.1918-1921.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Stickle D, Kaufman L, Blumer SO, et al. Comparison of a newly developed latex agglutination test and an immunodiffusion test in the diagnosis of systemic candidiasis. Appl Microbiol. 1972;23:490–499. doi: 10.1128/am.23.3.490-499.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Marot-Leblond A, Beucher B, David S, et al. Development and evaluation of a rapid latex agglutination test using a monoclonal antibody to identify Candida dubliniensis colonies. J Clin Microbiol. 2006;44:138–142. doi: 10.1128/JCM.44.1.138-142.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fujita S, Hashimoto T. Detection of serum Candida antigens by enzyme-linked immunosorbent assay and a latex agglutination test with anti-Candida albicans and anti-Candida krusei antibodies. J Clin Microbiol. 1992;30:3132–3137. doi: 10.1128/jcm.30.12.3132-3137.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Matthews R, Burnie J. Diagnosis of systemic candidiasis by an enzyme-linked dot immunobinding assay for a circulating immunodominant 47-kilodalton antigen. J Clin Microbiol. 1988;26:459–463. doi: 10.1128/jcm.26.3.459-463.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Manning-Zweerink M, Maloney C, Mitchell T, et al. Immunoblot analyses of Candida albicans-associated antigens and antibodies in human sera. J Clin Microbiol. 1986;23:46–52. doi: 10.1128/jcm.23.1.46-52.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kostiala I, Kostiala A, Larinkari U, et al. Antibodies against antigens of Candida albicans in patients with fungaemia and bacteraemia, studied by ELISA, precipitation, passive haemagglutination and immunofluorescence techniques. J Med Microbiol. 1981;14:483–492. doi: 10.1099/00222615-14-4-483. [DOI] [PubMed] [Google Scholar]
- 97.Fujita S, Matsubara F, Matsuda T. Enzyme-linked immunosorbent assay measurement of fluctuations in antibody titer and antigenemia in cancer patients with and without candidiasis. J Clin Microbiol. 1986;23:568–575. doi: 10.1128/jcm.23.3.568-575.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Laín A, Elguezabal N, Brena S, et al. Diagnosis of invasive candidiasis by enzyme-linked immunosorbent assay using the N-terminal fragment of Candida albicans hyphal wall protein 1. BMC Microbiol. 2007;7:35. doi: 10.1186/1471-2180-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Laín A, Moragues MD, Ruiz JCG, et al. Evaluation of a novel enzyme-linked immunosorbent assay to detect immunoglobulin G antibody to enolase for serodiagnosis of invasive candidiasis. Clin Vaccine Immunol. 2007;14:318–319. doi: 10.1128/CVI.00396-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Van Deventer A, Van Vliet H, Hop W, et al. Diagnostic value of anti-Candida enolase antibodies. J Clin Microbiol. 1994;32:17–23. doi: 10.1128/jcm.32.1.17-23.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pisa D, Ramos M, Molina S, et al. Evolution of antibody response and fungal antigens in the serum of a patient infected with Candida famata. J Med Microbiol. 2007;56:571–578. doi: 10.1099/jmm.0.47042-0. [DOI] [PubMed] [Google Scholar]
- 102.Strockbine NA, Largen MT, Buckley HR. Production and characterization of three monoclonal antibodies to Candida albicans proteins. Infect Immun. 1984;43:1012–1018. doi: 10.1128/iai.43.3.1012-1018.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ponton J, Marot-Leblond A, Ezkurra P, et al. Characterization of Candida albicans cell wall antigens with monoclonal antibodies. Infect Immun. 1993;61:4842–4847. doi: 10.1128/iai.61.11.4842-4847.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Schneider J, Moragues D, MartÃnez N, et al. Cross-reactivity between Candida albicans and human ovarian carcinoma as revealed by monoclonal antibodies PA10F and C6. Br J Cancer. 1998;77:1015. doi: 10.1038/bjc.1998.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rodriguez MJ, Schneider J, Moragues MD, et al. Cross-reactivity between Candida albicans and oral squamous cell carcinoma revealed by monoclonal antibody C7. Anticancer Res. 2007;27:3639–3643. [PubMed] [Google Scholar]
- 106.Kaufman L, Kovacs JA, Reiss E. Manual of clinical laboratory immunology. Washington, DC: American Society for Microbiology; 1997. Clinical immunomycology; pp. 575–583. [Google Scholar]
- 107.Marcilla A, Monteagudo C, Mormeneo S, et al. Monoclonal antibody 3H8: a useful tool in the diagnosis of candidiasis. Microbiology. 1999;145:695–701. doi: 10.1099/13500872-145-3-695. [DOI] [PubMed] [Google Scholar]
- 108.Yeo SF, Wong B. Current status of nonculture methods for diagnosis of invasive fungal infections. Clin Microbiol Rev. 2002;15:465–484. doi: 10.1128/CMR.15.3.465-484.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jarvensivu A, Hietanen J, Rautemaa R, et al. Candida yeasts in chronic periodontitis tissues and subgingival microbial biofilms in vivo. Oral Dis. 2004;10:106–112. doi: 10.1046/j.1354-523x.2003.00978.x. [DOI] [PubMed] [Google Scholar]
- 110.Bikandi J, San Millán R, Moragues MD, et al. Rapid identification of Candida dubliniensis by indirect immunofluorescence based on differential localization of antigens on C. dubliniensis blastospores and Candida albicans germ tubes. J Clin Microbiol. 1998;36:2428–2433. doi: 10.1128/jcm.36.9.2428-2433.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jarvensivu A, Rautemaa R, Sorsa T, et al. Specificity of the monoclonal antibody 3H8 in the immunohistochemical identification of Candida species. Oral Dis. 2006;12:428–433. doi: 10.1111/j.1601-0825.2006.01228.x. [DOI] [PubMed] [Google Scholar]
- 112.Chang CM, Chang WH, Wang CH, et al. Nucleic acid amplification using microfluidic systems. Lab Chip. 2013;13:1225–1242. doi: 10.1039/c3lc41097h. [DOI] [PubMed] [Google Scholar]
- 113.Simon D, Atkins IMC. Fungal molecular diagnostics: a mini review. J Appl Genet. 2004;45:3–15. [PubMed] [Google Scholar]
- 114.Arvanitis M, Anagnostou T, Fuchs BB, et al. Molecular and nonmolecular diagnostic methods for invasive fungal infections. Clin Microbiol Rev. 2014;27:490–526. doi: 10.1128/CMR.00091-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zourob M, Elwary S, Turner AP. Principles of bacterial detection: biosensors, recognition receptors and microsystems. New York (NY): Springer Science & Business Media; 2008. [Google Scholar]
- 116.Campa D, Tavanti A, Gemignani F, et al. DNA micro-array based on arrayed-primer extension technique for identification of pathogenic fungi responsible for invasive and superficial mycoses. J Clin Microbiol. 2008;46:909–915. doi: 10.1128/JCM.01406-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Spiess B, Seifarth W, Hummel M, et al. DNA micro-array-based detection and identification of fungal pathogens in clinical samples from neutropenic patients. J Clin Microbiol. 2007;45:3743–3753. doi: 10.1128/JCM.00942-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Leinberger DM, Schumacher U, Autenrieth IB, et al. Development of a DNA microarray for detection and identification of fungal pathogens involved in invasive mycoses. J Clin Microbiol. 2005;43:4943–4953. doi: 10.1128/JCM.43.10.4943-4953.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Reiss E, Tanaka K, Bruker G, et al. Molecular diagnosis and epidemiology of fungal infections. Med Mycol. 1997;36:249–257. [PubMed] [Google Scholar]
- 120.Mullis K, Faloona F, Scharf S, et al. Specific enzymatic amplification of DNA in vitro: the polymerase chain reaction. Cold Spring Harbor Symp Quant Biol. 1986;51:263–273. doi: 10.1101/sqb.1986.051.01.032. [DOI] [PubMed] [Google Scholar]
- 121.Kan VL. Polymerase chain reaction for the diagnosis of candidemia. J Infect Dis. 1993;168:779–783. doi: 10.1093/infdis/168.3.779. [DOI] [PubMed] [Google Scholar]
- 122.Jordan JA. PCR identification of four medically important Candida species by using a single primer pair. J Clin Microbiol. 1994;32:2962–2967. doi: 10.1128/jcm.32.12.2962-2967.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Einsele H, Hebart H, Roller G, et al. Detection and identification of fungal pathogens in blood by using molecular probes. J Clin Microbiol. 1997;35:1353–1360. doi: 10.1128/jcm.35.6.1353-1360.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Burnie JP, Golband N, Matthews RC. Semiquantitative polymerase chain reaction enzyme immunoassay for diagnosis of disseminated candidiasis. Eur J Clin Microbiol Dis. 1997;16:346–350. doi: 10.1007/BF01726361. [DOI] [PubMed] [Google Scholar]
- 125.Widjojoatmodjo MN, Borst A, Schukkink RAF, et al. Nucleic acid sequence-based amplification (NASBA) detection of medically important Candida species. J Microbiol Meth. 1999;38:81–90. doi: 10.1016/s0167-7012(99)00079-2. [DOI] [PubMed] [Google Scholar]
- 126.Zhou X, Kong F, Sorrell TC, et al. Practical method for detection and identification of Candida, Aspergillus, and Scedosporium spp. by use of rolling-circle amplification. J Clin Microbiol. 2008;46:2423–2427. doi: 10.1128/JCM.00420-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Prasad JK, Feller I, Thomson PD. A ten-year review of Candida sepsis and mortality in burn patients. Surgery. 1987;101:213–216. [PubMed] [Google Scholar]
- 128.Kurita H, Kamata T, Zhao C, et al. Usefulness of a commercial enzyme-linked immunosorbent assay kit for Candida mannan antigen for detecting Candida in oral rinse solutions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:531–534. doi: 10.1016/j.tripleo.2008.12.025. [DOI] [PubMed] [Google Scholar]
- 129.Lehmann LE, Hunfeld K-P, Emrich T, et al. A multiplex real-time PCR assay for rapid detection and differentiation of 25 bacterial and fungal pathogens from whole blood samples. Med Microbiol Immunol. 2008;197:313–324. doi: 10.1007/s00430-007-0063-0. [DOI] [PubMed] [Google Scholar]
- 130.Ilyas A, Asghar W, Allen PB, et al. Electrical detection of cancer biomarker using aptamers with nanogap break-junctions. Nanotechnology. 2012;23:275502. doi: 10.1088/0957-4484/23/27/275502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wan Y, Tan J, Asghar W, et al. Velocity effect on aptamer-based circulating tumor cell isolation in microfluidic devices. J Phys Chem B. 2011;115:13891–13896. doi: 10.1021/jp205511m. [DOI] [PubMed] [Google Scholar]
- 132.Pulcrano G, Iula DV, Vollaro A, et al. Rapid and reliable MALDI-TOF mass spectrometry identification of Candida non-albicans isolates from bloodstream infections. J Microbiol Methods. 2013;94:262–266. doi: 10.1016/j.mimet.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 133.Sackmann EK, Fulton AL, Beebe DJ. The present and future role of microfluidics in biomedical research. Nature. 2014;507:181–189. doi: 10.1038/nature13118. [DOI] [PubMed] [Google Scholar]
- 134.Asghar W, El Assal R, Shafiee H, et al. Preserving human cells for regenerative, reproductive, and transfusion medicine. Biotechnol J. 2014;9:895–903. doi: 10.1002/biot.201300074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Asghar W, El Assal R, Shafiee H, et al. Engineering cancer microenvironments for in vitro 3-D tumor models. Mater Today. 2015;18:539–553. doi: 10.1016/j.mattod.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Asghar W, Ramachandran PP, Adewumi A, et al. Rapid nanomanufacturing of metallic break junctions using focused ion beam scratching and electromigration. J Manufact Sci Eng. 2010;132:030911. [Google Scholar]
- 137.Asghar W, Velasco V, Kingsley JL, et al. Selection of functional human sperm with higher DNA integrity and fewer reactive oxygen species. Adv Healthc Mater. 2014;3:1671–1679. doi: 10.1002/adhm.201400058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Asghar W, Wan Y, Ilyas A, et al. Electrical fingerprinting, 3D profiling and detection of tumor cells with solid-state micropores. Lab on a Chip. 2012;12:2345–2352. doi: 10.1039/c2lc21012f. [DOI] [PubMed] [Google Scholar]
- 139.Ilyas A, Asghar W, Ahmed S, et al. Electrophysiological analysis of biopsy samples using elasticity as an inherent cell marker for cancer detection. Anal Methods. 2014;6:7166–7174. [Google Scholar]
- 140.Ilyas A, Asghar W, Kim YT, et al. Parallel recognition of cancer cells using an addressable array of solid-state micropores. Biosens Bioelectron. 2014;62:343–349. doi: 10.1016/j.bios.2014.06.048. [DOI] [PubMed] [Google Scholar]
- 141.Wang L, Asghar W, Demirci U, et al. Nanostructured substrates for isolation of circulating tumor cells. Nano today. 2013;8:374–387. doi: 10.1016/j.nantod.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Asghar W, Islam M, Wadajkar AS, et al. PLGA micro-and nanoparticles loaded into gelatin scaffold for controlled drug release. IEEE Trans Nanotechnol. 2012;11:546–553. [Google Scholar]
- 143.Ramachandran A, Liu Y, Asghar W, et al. Characterization of DNA-nanopore interactions by molecular dynamics. Am J Biomed Sci. 2009;1:344–351. [Google Scholar]
- 144.Vidyala SD, Asghar W, Iqbal SM. Porous organic nano-layers for coating of solid-state devices. J Nanobiotechnol. 2011;9:18. doi: 10.1186/1477-3155-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ilyas A, Islam M, Asghar W, et al. Salt-leaching synthesis of porous PLGA nanoparticles. IEEE Trans Nanotechnol. 2013;12:1082–1088. [Google Scholar]
- 146.Ilyas A, Asghar W, Billo J, et al. From molecular electronics to proteonics: break junctions for biomarker detection. Life Science Systems and Applications Workshop (LiSSA), 2011 IEEE/NIH; 2011; Bethesda, MD: IEEE; [Google Scholar]
- 147.Sachse S, Straube E, Lehmann M, et al. Truncated human cytidylate-phosphatedeoxyguanylate-binding protein for improved nucleic acid amplification technique-based detection of bacterial species in human samples. J Clin Microbiol. 2009;47:1050–1057. doi: 10.1128/JCM.02242-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mylonakis E, Clancy CJ, Ostrosky-Zeichner L, et al. T2 magnetic resonance assay for the rapid diagnosis of candidemia in whole blood: a clinical trial. Clin Infect Dis. 2015;60:892–899. doi: 10.1093/cid/ciu959. [DOI] [PubMed] [Google Scholar]
- 149.Baeumner SJ. Microfluidic isolation of nucleic acids. Angew Chem Int Ed. 2014;53:2–16. doi: 10.1002/anie.201309580. [DOI] [PubMed] [Google Scholar]
- 150.Cai D, Xiao M, Xu P, et al. An integrated microfluidic device utilizing dielectrophoresis and multiplex array PCR for point-of-care detection of pathogens. Lab Chip. 2014;14:3917–3924. doi: 10.1039/c4lc00669k. [DOI] [PubMed] [Google Scholar]
- 151.Boles DJ, Benton JL, Siew GJ, et al. Droplet-based pyrosequencing using digital microfluidics. Anal Chem. 2011;83:8439–8447. doi: 10.1021/ac201416j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Schell WA, Benton JL, Smith PB, et al. Evaluation of a digital microfluidic real-time PCR platform to detect DNA of Candida albicans in blood. Eur J Microbiol Infect Dis. 2012;31:2237–2245. doi: 10.1007/s10096-012-1561-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Schumacher S, Nestler J, Otto T, et al. Highly-integrated lab-on-chip system for point-of-care multiparameter analysis. Lab Chip. 2012;12:464–473. doi: 10.1039/c1lc20693a. [DOI] [PubMed] [Google Scholar]
- 154.Lee H, Sun E, Ham D, et al. Chip-NMR biosensor for detection and molecular analysis of cells. Nat Med. 2008;14:869–874. doi: 10.1038/nm.1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gervais L, de Rooij N, Delamarche E. Microfluidic chips for point-of-care immunodiagnostics. Adv Mater Weinheim. 2011;23:H151–HH76. doi: 10.1002/adma.201100464. [DOI] [PubMed] [Google Scholar]
- 156.Shafiee H, Sano MB, Henslee EA, et al. Selective isolation of live/dead cells using contactless dielectrophoresis (cDEP) Lab on a Chip. 2010;10:438–445. doi: 10.1039/b920590j. [DOI] [PubMed] [Google Scholar]
- 157.Fujita SI, Takamura T, Nagahara M, et al. Evaluation of a newly developed down-flow immunoassay for detection of serum mannan antigens in patients with candidaemia. J Med Microbiol. 2006;55:537–543. doi: 10.1099/jmm.0.46314-0. [DOI] [PubMed] [Google Scholar]
- 158.Sogawa K, Watanabe M, Sato K, et al. Use of the MALDI BioTyper system with MALDI-TOF mass spectrometry for rapid identification of microorganisms. Anal Bioanal Chem. 2011;400:1905–1911. doi: 10.1007/s00216-011-4877-7. [DOI] [PubMed] [Google Scholar]
- 159.Yetisen AK, Akram MS, Lowe CR. Paper-based micro-fluidic point-of-care diagnostic devices. Lab Chip. 2013;13:2210. doi: 10.1039/c3lc50169h. [DOI] [PubMed] [Google Scholar]
- 160.Shafiee H, Asghar W, Inci F, et al. Paper and flexible substrates as materials for biosensing platforms to detect multiple biotargets. Scientific Rep. 2015;5:8719. doi: 10.1038/srep08719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Sista R, Hua Z, Thwar P, et al. Development of a digital microfluidic platform for point of care testing. Lab Chip. 2008;8:2091–2104. doi: 10.1039/b814922d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Eggimann P, Garbino J, Pittet D. Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect Dis. 2003;3:685–702. doi: 10.1016/s1473-3099(03)00801-6. [DOI] [PubMed] [Google Scholar]
- 163.Safavieh M, Kanakasabapathy MK, Tarlan F, et al. Emerging loop-mediated isothermal amplification-based microchip and microdevice technologies for nucleic acid detection. ACS Biomater Sci Eng. 2016;3:278–294. doi: 10.1021/acsbiomaterials.5b00449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Asghar W, Yuksekkaya M, Shafiee H, et al. Engineering long shelf life multi-layer biologically active surfaces on microfluidic devices for point of care applications. Sci Rep. 2016;6:21163. doi: 10.1038/srep21163. [DOI] [PMC free article] [PubMed] [Google Scholar]