Abstract
Chronic exposure to psychosocial stress has adverse effects on cardiovascular health, however the stress-sensitive neurocircuitry involved remains to be elucidated. The anatomical and physiological characteristics of the locus coeruleus (LC)-norepinephrine (NE) system position it to contribute to stress-induced cardiovascular disease. This review focuses on cardiovascular dysfunction produced by social stress and a major theme highlighted is that differences in coping strategy determine individual differences in social stress-induced cardiovascular vulnerability. The establishment of different coping strategies and cardiovascular vulnerability during repeated social stress has recently been shown to parallel a unique plasticity in LC afferent regulation, resulting in either excitatory or inhibitory input to the LC. This contrasting regulation of the LC would translate to differences in cardiovascular regulation and may serve as the basis for individual differences in the cardiopathological consequences of social stress. The advances described suggest new directions for developing treatments and/or strategies for decreasing stress-induced cardiovascular vulnerability.
Introduction
The cardiovascular response to psychosocial stress, resulting in transient increases in blood pressure and heart rate, is functional in the acute sense. However, there is overwhelming evidence that chronic stress has adverse effects on cardiovascular health. Epidemiological studies such as INTERHEART revealed that those who reported “permanent stress” at work or at home were more than two times more likely to suffer from a myocardial infarction (Rosengren et al., 2004). Furthermore, marital stress was associated with a nearly 3-fold increased risk of coronary artery disease (Orth-Gomer et al., 2000). The association between stress and cardiovascular disease is unmistakable and can be replicated in preclinical animal studies, however the stress-sensitive neurocircuitry that contributes to increased cardiovascular disease risk remains to be elucidated.
One system that has been implicated in the association between stress and cardiovascular disease is the brain norepinephrine (NE) system that arises from the pontine nucleus, locus coeruleus (LC). This review begins with an introduction to the anatomical and physiological characteristics of the LC-NE system that position it to be a major stress response system. Evidence that the LC processes cardiovascular information and in turn can impact cardiovascular function are discussed. Because social stress is most relevant for humans, this review focuses on cardiovascular vulnerability produced by social stress as predicted by the rodent resident-intruder model and the role of the LC-NE system in cardiovascular vulnerability in that model. A major theme highlighted in this review is that individual differences in coping strategy determine individual differences in social stress-induced cardiovascular vulnerability. Moreover, the recent discovery that the establishment of different coping strategies and cardiovascular vulnerability during repeated stress is paralleled by a unique plasticity in LC afferent regulation is discussed. The advances described suggest new directions for developing treatments and/or strategies for decreasing stress-induced cardiovascular vulnerability.
The locus coeruleus-norepinephrine stress response system
The hallmark of stress is generally considered to be activation of the hypothalamic-pituitary-adrenal (HPA) axis, with plasma glucocorticoid levels serving as the endpoint of that activation. However, sustained activation of the brain NE system may also be considered a hallmark of stress in that it is initiated by many of the same challenges in parallel with the HPA axis. Given its physiological attributes and connectivity, activation of the LC-NE system during stress has been suggested to serve as an arousal and cognitive limb of the stress response. Evidence discussed below however, underscores cardiovascular consequences of stress-related activation of the brain norepinephrine system. The coordination of cardiovascular and cognitive responses to stress may underlie co-morbidity of cardiovascular and affective symptoms of stress-related disorders.
Anatomical features of the LC-NE system
The pontine nucleus, LC is a primary source of norepinephrine in brain (Grzanna and Molliver, 1980; Swanson and Hartman, 1976). Recent studies using novel, selective tract tracing tools have refined our knowledge of the topography of LC neurons with respect to their afferent inputs and efferent projections (Robertson et al., 2013; Schwarz and Luo, 2015). However, for the most part the nucleus is still characterized by it homogeneous expression of norepinephrine in all neurons and its widespread, highly collateralized projection system that is a major source of NE in the forebrain (Aston-Jones et al., 1995; Swanson and Hartman, 1976). Notably, the LC serves as the primary source of NE in forebrain regions such as the hippocampus and cortex that govern cognition, memory and complex behaviors. With regard to cardiovascular function, the LC exerts both indirect (via the nucleus ambiguus (Amb)-rostroventrolateral medulla (RVLM) circuit) (Jones and Yang, 1985; McKitrick and Calaresu, 1996) and direct projections to the preganglionic sympathetic neurons within the intermediolateral nucleus of the spinal cord, a common pathway for stress induced cardiovascular responses (Jones and Yang, 1985; Spyer, 1992). Furthermore, there is clear evidence for projections from the LC to the central nucleus of the amygdala (CNA), another stress-sensitive brain region with cardiovascular impact (Kravets et al., 2015; Mason and Fibiger, 1979). Tract tracing studies have also provided evidence for LC projections to the medial part of the rostral dorsal motor vagal nucleus (DMV) and lateral part of the intermediate DMV, the location of preganglionic parasympathetic cardiac neurons (Ter Horst et al., 1991). Consistent with this, LC neurons are transsynaptically labeled from the heart (Standish et al., 1995). Evidence discussed below support the idea that LC exerts an inhibitory regulation on cardiac parasympathetic neurons and excitatory regulation on preganglionic sympathetic neurons.
Sources of LC afferents have been debated as a result of differences in retrograde tracers and whether the injection was limited to the cell body region (Aston-Jones et al., 1991). Because the dendrites of LC neurons can extend for several hundred microns outside of the nuclear zone, neurons with axons terminating in pericoerulear areas can synaptically contact LC dendrites and impact on LC activity although they may not be labeled by injections into the nuclear LC (Shipley et al., 1996). As a result, studies that limit retrograde tracers to the LC nucleus reveal a very limited number of afferents that include the dorsal cap of the paraventricular hypothalamic nucleus, the nucleus prepositus hypoglossi and nucleus paragigantocellularis (PGi) in the ventrolateral medulla (Aston-Jones et al., 1990). Because the PGi is a source of inputs to the preganglionic sympathetic neurons it is positioned to coordinate peripheral sympathetic activity with central noradrenergic activity (Van Bockstaele and Aston-Jones, 1995). The PGi is a major source of enkephalinergic innervation of the LC (Drolet et al., 1990). The importance of this input in stress-coping strategy and stress-related cardiovascular vulnerability is discussed below. In contrast to the restricted number of LC afferents identified by tracer injections limited to the nucleus LC, injections of retrograde tracers in pericoerulear regions where LC dendrites extend, combined with anterograde labeling from putative afferents and electron microscopy to verify synaptic connections reveal relatively numerous LC afferents (Luppi et al., 1995; Van Bockstaele et al., 2001; Van Bockstaele et al., 1998; Van Bockstaele et al., 1999). Of these, the central nucleus of the amygdala is relevant to cardiovascular function and as discussed below conveys cardiovascular-related information to the LC (Curtis et al., 2002). This is also a major source of the stress-related neuropeptide, corticotropin-releasing factor (CRF), afferents to the LC and a primary route through which stressors activate the LC-NE system (Curtis et al., 2002; Van Bockstaele et al., 1998).
Physiological Characteristics of LC neurons
The rate and pattern of LC neuronal discharge have implicated the LC-NE system in the regulation of arousal and attention (Aston-Jones and Bloom, 1981a, b; Aston-Jones and Cohen, 2005; Foote et al., 1980; Williams and Marshall, 1987). LC neurons fire spontaneously and their rate of discharge correlates positively with the state of arousal (Aston-Jones and Bloom, 1981a; Foote et al., 1980). This relationship is more than correlation as selective chemical activation or inhibition of LC neurons is sufficient to impact on cortical and hippocampal network activity, indicating a degree of causality between LC discharge rate and forebrain indices of arousal (Berridge and Foote, 1991; Berridge et al., 1993). Notably, LC activation has been demonstrated to be necessary for cortical activation by stimuli including hypotensive stress (Page et al., 1993) (Lechner et al., 1997) (see below). Thus, this is a route by which autonomic challenges can affect cortical functions.
In addition to rate, the pattern of LC neuronal firing is relevant to behavior. LC neurons fire in both a tonic and a phasic pattern with the latter characterized by synchronous bursting. Salient sensory stimuli elicit a burst of LC discharge that typically precedes orientation to the eliciting stimuli (Aston-Jones and Bloom, 1981b; Foote et al., 1980). This feature of LC neurons has suggested that sensory-evoked activation of the LC-NE system resets or redirects attention towards salient environmental stimuli.
Shifts in the pattern of LC discharge between phasic and high tonic discharge modes are thought to differentially bias behavior. Phasic LC discharge is associated with focused attention and staying on-task, whereas high tonic discharge is associated with labile attention and going off-task (see for reviews (Aston-Jones and Cohen, 2005; Bouret and Sara, 2005)) (Rajkowski et al., 1994; Usher et al., 1999). In contrast, high tonic LC discharge rate is thought to promote behavioral flexibility by disengaging animals from attention to specific stimuli and ongoing behaviors and favoring scanning for stimuli that promote alternate behaviors that would lead to more rewarding outcomes (Aston-Jones and Cohen, 2005). Shifts between phasic and tonic LC firing patterns would promote rapid adjustments in a dynamic environment.
LC-NE activation is a cognitive limb of the stress response that occurs in parallel with the HPA initiated endocrine response. The same stressors that initiate the HPA response to stress also activate the LC-NE system, including shock, auditory stress, immunological challenges, autonomic stressors, restraint and social stress. This has been determined using different endpoints of LC activity including NE turnover, NE release, LC neuronal activity, c-fos expression or tyrosine hydroxylase expression (Beck and Fibiger, 1995; Bonaz and Tache, 1994; Britton et al., 1992; Campeau and Watson, 1997; Cassens et al., 1981; Cassens et al., 1980; Chan and Sawchenko, 1995; Chang et al., 2000; Curtis et al., 2012; Dun et al., 1995; Duncan et al., 1993; Funk and Amir, 2000; Graham et al., 1995; Ishida et al., 2002; Kollack-Walker et al., 1997; Korf et al., 1973; Lacosta et al., 2000; Makino et al., 2002; Rusnak et al., 2001; Sabban and Kvetnansky, 2001; Smagin et al., 1994; Smith et al., 1992; Smith et al., 1991; Thierry et al., 1968; Valentino et al., 1991). The parallel activation of the HPA and LC-NE system would coordinate endocrine and cognitive limbs of the stress response (Valentino and Van Bockstaele, 2008). Electrophysiological recordings in anesthetized and unanesthetized rats have demonstrated that acute stress (including hypotensive stress, see below) and exposure to CRF shifts LC discharge towards a high tonic state that would favor heightened arousal, disengagement from ongoing behavior, labile attention and cognitive flexibility (Curtis et al., 2012; Valentino and Foote, 1987; Valentino and Foote, 1988; Valentino and Wehby, 1988; Zitnik et al., 2015). Consistent with this, CRF microinfused directly into the LC increases cognitive flexibility in an attentional set-shifting task (Snyder et al., 2012). These responses are adaptive in coping with an immediate threat. However, these same consequences of increased LC-NE activity would appear pathological outside of the context of stress and would translate to hyperarousal, loss of concentration, restlessness and poor performance on tasks that require focused attention. Notably, these are characteristic symptoms of stress-related psychiatric disorders such as PTSD and major depression and hyperactivity of the LC-NE system has been implicated in these disorders (Southwick et al., 1999; Wong et al., 2000).
Cross-talk between the LC and cardiovascular system
LC responses to cardiovascular stimuli
The anatomy of the LC-NE system discussed above supports reciprocal communication with cardiovascular-related centers. LC neurons receive and process cardiovascular-related information and conversely changes in LC activity impact on cardiovascular function. The most well characterized cardiovascular response of LC neurons is its activation by hypotensive stress. Hypovolemia, as would occur with hemorrhage, was demonstrated to increase the discharge rates of rat LC neurons and this is reliably reproduced by the intravenous infusion of a dose of the hypotensive agent, sodium nitroprusside that decreases blood pressure by 30–50% (Elam et al., 1985; Svensson, 1987). The same hypotensive challenge also activates the HPA axis and so provides an example of how the same stressor activates both stress response systems in parallel (Plotsky and Vale, 1984). As has been seen with other acute stressors, during hypotensive stress, the pattern of LC discharge shifts towards a high tonic state that would support increased arousal, scanning attention and behavioral flexibility (Valentino and Wehby, 1988). LC neuronal responses to hypotensive challenge translate to increased forebrain NE release and cortical EEG activation, indicative of arousal. The LC response to hypotension is necessary for the cortical response because silencing the LC bilaterally with local infusion of clonidine prevents this effect (Page et al., 1993). Activation of the LC-NE system by hypotension would be adaptive, for example, serving to maintain arousal and cognitive flexibility in animals that are injured and hemorrhaging.
The response of LC neurons to hypotension is mediated by local CRF release. Indeed, the initial studies to support a functional role of endogenous CRF in the LC were those that demonstrated that local microinfusion of CRF antagonists into the LC prevented LC neuronal activation by hypotensive stress (Valentino et al., 1991). The finding that this same manipulation prevented cortical activation by hypotensive challenge demonstrated that a function of CRF neurotransmission in the LC during hypotension was to increase arousal (Page et al., 1993).
A primary source of CRF that mediates LC activation during hypotensive stress is the central nucleus of the amygdala (CNA). This was demonstrated in lesion studies and through functional neuroanatomy (Curtis et al., 2002). However, the role of CRF neurons in the PGi in this response could not be ruled out, as it was not possible to determine the effects of lesioning this nucleus because this often results in death.
An important component of the LC response to hypotensive stress is an inhibition that occurs with stress termination that promotes recovery of LC neuronal activity back to pre-stress levels (Curtis et al., 2001; Valentino et al., 1991). This inhibition becomes exaggerated when the CRF excitatory influence is abrogated by the administration of a CRF antagonist into the LC (Curtis et al., 2001). Indeed the administration of some CRF antagonists reveals an inhibition that is apparent even during the hypotensive challenge (Valentino et al., 1991). Intra-LC administration of the opioid antagonist, naloxone, prevents this inhibition and slows recovery of LC neurons from hypotensive stress-induced excitation, providing evidence that this is an opioid-mediated effect (Curtis et al., 2001). These findings suggested a model whereby hypotensive stress engages CNA-CRF afferents that shift LC activity to a high tonic state as well as endogenous opioid afferents, which serve to restrain this excitation, promoting recovery of LC activity to pre-stress levels when hypotension is terminated. Thus, during hypotension, LC activity is fine-tuned by a convergence of CRF and opioid afferents with opposing actions. Later studies demonstrated a similar dual component response of LC neurons to predator stress (Curtis et al., 2012). The most prominent opioid input to the LC that could account for this inhibition is a PGI-enkephalin (ENK) input that densely innervates the LC (Drolet et al., 1992). Notably, LC neurons have a high expression of μ-opioid receptor (MOR) to respond to ENK innervation (Mansour et al., 1994; Tempel and Zukin, 1987).
Cardiovascular responses to LC activation
The LC has a reciprocal relationship with the autonomic nervous system, so that in addition to cardiovascular stimuli activating the LC, LC-NE activation also produces a cardiovascular response. Noxious sensory stimuli produce a parallel and nearly identical increase in LC-NE activity and peripheral sympathetic nerve activity indicating a relationship between the central noradrenergic system that controls arousal and the peripheral sympathetic nervous system (Elam et al., 1986). For years, however, studies have been equivocal regarding the functional effect of LC activation on peripheral cardiovascular output. Electrical stimulation of LC neurons has been commonly reported to elicit cardiovascular and noradrenergic changes consistent with increased sympathetic nervous system activity (Crawley et al., 1980). Furthermore, peptidergic activation of LC by corticotropin releasing factor or thyrotropin releasing hormone results in a significant pressor response (Brown, 1986; Paakkari et al., 1987). In contrast, chemical activation of LC neurons by the excitatory neurotransmitter, L-glutamate, has been reported to produce a depressor response and bradycardia in some studies (Sved and Felsten, 1987), while others report significant increases in blood pressure (Chen and Huang, 1997). Based on these contrasting findings, it was suggested that evidence obtained from electrical stimulation was the result of activating non-noradrenergic cells or fibers of passage within the LC (Crawley et al., 1980). We now understand these conflicting effects of LC activation on sympathetic output likely arose in part from differences in the effect of LC activation in awake versus anesthetized animals, the impact of different types of anesthesia, or different strains of rodents (Chen and Huang, 1997; Kawamura et al., 1978; Sved and Felsten, 1987).
More recent advances using optogenetic technology have further clarified the role of the LC in cardiovascular activation. For example, optogenetic stimulation of LC neurons revealed a direct influence on cardioinhibitory vagal neurons (Wang et al., 2014). In this study, photostimulation of LC neurons resulted in an increase in frequency of inhibitory postsynaptic currents in cardiac vagal neurons. In addition to the cardioinhibitory DMV, the nucleus ambiguus (Amb) also serves to decrease blood pressure and heart rate by suppressing the sympathoexcitatory rostroventrolateral medulla (RVLM) (McKitrick and Calaresu, 1996). Similar to the DMV, the LC also projects to the Amb and inhibits its activity (Jones and Yang, 1985; Samuels and Szabadi, 2008a, b) thereby removing the inhibitory influence over the RVLM. Recent optogenetic studies revealed the cardiovascular response to LC activation. Optogenetic activation of astrocytes within the LC was used to promote the release of L-lactate into the LC, thereby activating LC neurons. Furthermore, this study revealed that, like L-glutamate, intra-LC L-lactate produced increased heart rate and blood pressure (Tang et al., 2014). Therefore, as functional evidence of the aggregate of the inhibitory influence on parasympathetic neurons and excitatory influence on sympathetic neurons, selective stimulation of the LC has been shown to result in peripheral catecholamine release and increased heart rate and blood pressure (Drolet and Gauthier, 1985; Gurtu et al., 1984; Kawamura et al., 1978).
Stress coping strategy and individual differences in stress vulnerability
For humans, stressors of a social nature are prevalent. The rodent resident-intruder stress has been used and modified by many laboratories to model human social stress. This stress involves placement of a rodent into the cage of an aggressive “resident” conspecific that will attack the intruder (Koolhaas et al., 1997). Repeated resident-intruder stress results in HPA dysfunction, decreased social interaction, anxiety-like behaviors, anhedonia, self-administration of drugs of abuse and decreased heart rate variability, alterations in circadian rhythm amplitudes and long lasting pro-arrhythmic effects (Carnevali et al., 2013b; Miczek et al., 2004; Rygula et al., 2005; Tornatzky and Miczek, 1994; Wood et al., 2012; Wood et al., 2010). Substantial individual variability exists in the consequences of resident-intruder stress. For mice this is best seen as differences in social interaction following the stress, such that vulnerable mice exhibit low levels of social interaction relative to resilient mice that show levels that are comparable to controls (Krishnan et al., 2007). For rats, individual differences in the consequences of resident-intruder stress for HPA function, anhedonia, drug self-administration and heart rate variability align with individual differences in coping strategies (Chaijale et al., 2013b; Wood et al., 2012; Wood et al., 2010; Wood et al., 2015). Repeated resident-intruder stress exposure results in the emergence of two distinct populations defined by their latency to assume the subordinate defeat posture (Wood et al., 2010). Notably, this latency is distributed bimodally rather than normally, underscoring that these are distinct populations and not extremes of a single population. Analysis of defeat latency over days of resident-intruder stress indicates that rats typically start off with relatively short latencies and that the resistance to defeat becomes established in certain rats after repeated exposures. Furthermore, this increase in defeat latency over subsequent stress exposures parallels the emergence of active coping upright postures in the intruder rat. Rats that exhibit short defeat latencies (SL rats) show significantly more anhedonia in sucrose preference tests, immobility in the forced swim test, propensity for self-administration of drugs of abuse and decreased heart rate variability. They also exhibit HPA dysregulation that is comparable to that reported in depression, compared to rats that resist or that have a long latency to defeat (LL rats) (Wood et al., 2012; Wood et al., 2010; Wood et al., 2015).
The neurobiological mechanisms underlying the development of the two distinct coping strategies have yet to be elucidated. However, recent functional neuroanatomical studies implicate a unique plasticity of LC afferent regulation that becomes established with the development of these styles (Reyes et al., 2015b). The initial exposure to resident-intruder stress, when rats generally exhibit a short latency to defeat, activates LC neurons and CRF-CNA afferents, as well as ENK-PGi afferents to the LC as determined by c-fos expression in these neurons. This is consistent with the electrophysiological evidence discussed above that acute stress increases LC discharge and engages both CRF and opioid afferents to the LC. However, by the fifth stressor exposure, when the SL and LL phenotypes have developed, c-fos expression in LC neurons and CRF-CNA afferents is maintained only in SL rats. In this subordinate population, activation of ENK-PGi neurons that project to the LC is lost with repeated resident-intruder stress. Opposing effects occur for LL rats, where activation of ENK-PGi afferents to the LC is maintained and activation of CRF-CNA inputs is lost. As a result, LC neurons of LL rats are not activated (as indicated by c-fos expression) above control levels following the fifth exposure to resident-intruder stress. Postsynaptic changes in CRF1 receptors and MOR in LC neurons are consistent with these presynaptic effects (Chaijale et al., 2013a). For example Western blots reveal higher levels of MOR and lower CRF1 receptor levels in LC tissue punches of LL rats compared to SL or control rats. These convergent findings suggest that the development of the LL coping strategy is associated with a shift in the balance of LC afferent regulation to favor the ENK-MOR inhibitory influence. By contrast, the SL strategy is maintained through a loss of ENK-MOR inhibition. Whether the stress-induced afferent plasticity is causal to the development of different coping strategies and vulnerability phenotypes requires further characterization. However, the findings that administration of CRF antagonists prior to resident-intruder stress bias populations to the LL coping strategy and attenuate some of the consequences, including cardiovascular consequences supports this idea (see below) (Wood et al., 2012).
Role of the LC in individual differences in cardiovascular responses to social defeat
The robust, ethologically relevant nature of social stress is evident by the vast and long-lasting repercussions that occur following social defeat exposure. In addition to the endocrine and behavioral deficits that are common following social stress, this robust sympathomimetic stressor also elicits cardiovascular consequences. Intense sympathetic activation elicits 30 times the number of arrhythmias (ventricular premature beats) during social defeat as compared to other non-social stressors (i.e. restraint or foot shock) (Sgoifo et al., 1999). The long-term consequences of social defeat clearly define the ability of this naturalistic stressor to promote cardiovascular dysfunction (for a review see (Sgoifo et al., 2014)). For example, repeated social stress disrupts the circadian rhythm of heart rate (Carnevali et al., 2013b; Meerlo et al., 1999; Sgoifo et al., 2002) and is capable of promoting atherosclerosis (Black and Garbutt, 2002). Social stress also decreases resting heart rate variability (HRV) (Wood et al., 2012), an indication of decreased parasympathetic and increased sympathetic drive that is indicative of enhanced cardiovascular disease risk (Novak et al., 1997; Tsuji et al., 1996). As evidence of the pathological consequences of this autonomic imbalance, social defeat produces maladaptive cardiac hypertrophy (Carnevali et al., 2013b; Gelsema et al., 1994). Furthermore, a recent study conducted a comprehensive analysis of cardiac electrophysiological variables in socially defeated rats where high density epicardial mapping analysis revealed a shortening of the effective refractory period, a decreased transversal conduction velocity of the wavefront and increased ventricular myocardial excitability in defeated rats compared with controls (Carnevali et al., 2013b). These cardiac electrophysiological variables are important determinants of arrhythmias and were attributed to increased cardiac sympathetic drive in rats with a history of social stress exposure (Carnevali et al., 2013b). In addition, social defeat has been shown to produce cardiac fibrosis, another contributing factor to cardiac arrhythmias (Costoli et al., 2004).
Studies assessing individual differences revealed that rodents are not uniformly sensitive to the cardiovascular consequences of stress, but rather susceptibility is related to coping strategy. The reduction in resting HRV 24–48 hours after social stress was exaggerated in rats displaying passive coping responses (Wood et al., 2012). Furthermore, chronic recordings revealed long-lasting elevations in resting systolic pressure following defeat selectively in rats displaying passive coping responses (Lombard et al., unpublished manuscript). In a related study, active coping determined by countering the resident’s attacks was related to a reduced and shorter lasting disruption of heart rate circadian rhythms compared to rats adopting a passive coping response (Meerlo et al., 1999). Furthermore, when coping style was determined prior to chronic intermittent stress there was an association between passive coping and hypertension (Hawley et al., 2010). Alternatively, the cardiovascular responsivity of rats exhibiting either high or low aggression is also distinctly different; with high aggression rats displaying reduced vagal antagonism and increased tachyarrhythmias compared with non-aggressive rats (Carnevali et al., 2013a) Taken together, these studies indicate that the behavioral coping response is associated with cardiovascular susceptibility to stress.
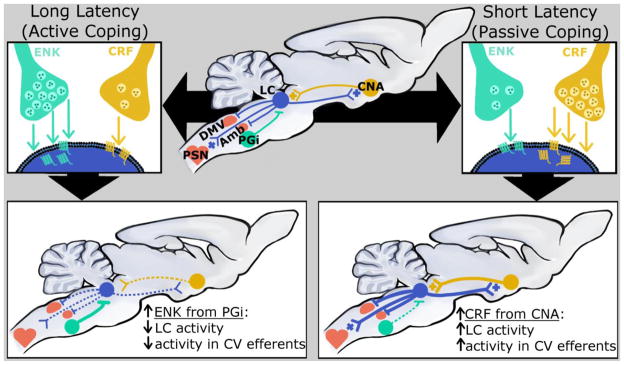
The LC plays a principal role in stress-related behaviors and cardiovascular function; therefore distinctions within the LC may provide insight into susceptibility to stress-related cardiac pathology. As discussed above, LC efferents target several cardiovascular centers of the brain, inhibiting parasympathetic centers such as the DMV and Amb and activating preganglionic sympathetic neurons (PSN). In active coping rats, the afferent regulation of LC that is biased towards PGi-ENK would translate to decreased activity of the LC’s cardiovascular efferents (Figure 1). This would reduce inhibition of the parasympathetic DMV and Amb and suppress excitation of PSN, promoting resilience to stress-related cardiovascular pathology. Furthermore, restraint stress has been shown to increase ENK expression in the ventrolateral medulla, the region containing PGi neurons (Boone and McMillen, 1994). Within this region, ENK serves to inhibit sympathetic nerve activity, resulting in hypotension and bradycardia (Punnen et al., 1984). Therefore, beyond the cardioprotective effects of ENK within the LC, if ENK levels were also increased within the PGi/ventrolateral medulla in the active coping rats, this would contribute to a cardioprotective decrease in SNS activity. In contrast, the passive coping phenotype is characterized by exaggerated CNA-CRF afferent regulation and thus hyperactivity of LC neurons. This distinction in LC regulation would translate to exaggerated inhibition of parasympathetic centers and enhanced sympathetic drive, thereby increasing cardiovascular vulnerability. In support of this, daily administration of a CRF antagonist before social stress not only shifted the population of rats towards the LL, active coping strategy, but also attenuated the reduction in HRV (Wood et al., 2012). While Reyes and colleagues (Reyes et al., 2015a) provided evidence of the CNA afferents as a distinct regulator of the LC in SL passive rats, the LC also projects to the CNA, which contributes to the cardiovascular response to stress (Kravets et al., 2015; Mason and Fibiger, 1979). For example, stimulation of the CNA elicits increased blood pressure in conscious rats (Chiou et al., 2009) and lesions of the CNA attenuate the pressor response to acute stress (Sanders et al., 1994). Therefore, the increased excitatory drive from the LC to the CNA that would be anticipated in passive coping rats may likely contribute to the exaggerated sympathetic activation in this susceptible phenotype. Taken together, these studies suggest that exaggerated LC activation may, in part, drive the enhanced cardiovascular vulnerability. In support of this, recent findings using intracerebroventricular administration of DSP-4 to partially lesion LC-NE projections prior to social defeat identified that an intact LC is necessary for the chronic increases in resting blood pressure to develop in the passive coping SL rats (Lombard et al., unpublished manuscript). In sum, these findings support a central role for LC regulation of cardiovascular vulnerability.
Figure 1.
Schematic depicting distinct engagement of CRF and ENK afferents to the LC and the resulting adaptations in receptors that are associated with different coping strategies (top). This contrasting regulation of the LC in passive versus active coping rats would translate to differences in cardiovascular (CV) regulation (bottom). Top: The LC is regulated by CRF-excitatory afferents from the CNA and enkephalinergic-inhibitory afferents from the PGi. LC efferents inhibit parasympathetic centers (DMV and Amb) and excite preganglionic sympathetic neurons (PSN). In response to repeated social defeat stress, an active coping strategy is associated with a bias towards PGi-ENK afferents to the LC resulting in internalization and upregulation of MORs. In addition, the CRF influence from the CNA is decreased in LL rats. In passive coping (SL) rats, the CNA-CRF afferents are engaged, resulting in CRF1 internalization in LC dendrites and the PGi-ENK influence is reduced. Bottom: Distinctions in afferent regulation of the LC during social stress would determine how the LC regulates CV efferents. In the active coping phenotype, diminished LC activity would translate to reduced inhibition of the parasympathetic DMV and Amb and reduced excitation of the PSN. This would promote resilience to stress-related cardiovascular vulnerability. In the passive coping phenotype the hyperactive LC would inhibit parasympathetic tone and enhance sympathetic drive, resulting in increased cardiovascular vulnerability. The selective bias towards either an excitatory or inhibitory afferent to LC may serve as the basis for individual differences in the cardiopathological consequences of social defeat.
Dotted lines indicate reduced activity of neuronal projections; thick lines indicate increased activity of neuronal projection. Excitatory and inhibitory projections are denoted by a + or a solid line perpendicular to the projection (−).
Conclusion
Identifying adaptations within the brain that are related to coping strategy will be critical to understanding the etiology of susceptibility to stress-induced cardiovascular disease. In particular, evidence of distinct regulation of LC afferents in passive versus active coping rats (Reyes et al., 2015a) may provide a window into the neurobiological changes driving susceptibility to cardiopathological conditions. In agreement with this, a study in humans combined measurements of HRV with fMRI and demonstrated that the high frequency index of HRV, a reflection of cardiovagal output (Novak et al., 1997), was negatively correlated with activity of the LC (Napadow et al., 2008), underscoring the inhibitory effect that the LC has on parasympathetic tone.
Hyperactivity of the LC has also been implicated in stress-related psychiatric disorders such as depression and PTSD (Southwick et al., 1997; Wong et al., 2000). Preclinical studies in rodents reveal that social stress is capable of producing depressive-like or anxiety-like behaviors comorbid with cardiovascular disturbances and together suggest that LC dysregulation may be involved in this comorbid condition (Carnevali et al., 2013b; Wood et al., 2012). In patients suffering from PTSD, HRV is reduced compared with non-PTSD controls (Agorastos et al., 2013; Shah et al., 2013), contributing to the increased risk of developing cardiovascular disease in these psychiatric disorders (Wood, 2014; Wood and Bhatnagar, 2015). A recent study expanded on these findings by comparing predeployment HRV in active-duty marines with postdeployment development of PTSD (Minassian et al., 2014). This study showed that marines are significantly more likely to develop PTSD if they start off with lower HRV. Therefore, if mechanisms capable of reducing HRV are engaged before stress, such as exaggerated LC activity, this may increase susceptibility to stress-related disorders. Studies evaluating the permissive role that the LC may play in enhancing vulnerability to stress-related disorders will shed light on neurobiological mechanisms driving stress-induced cardiovascular disease and the high rate of comorbidity with psychiatric disorders.
Highlights.
Social stress exposure is a risk factor for cardiovascular disease.
The anatomical and physiological characteristics of the locus coeruleus-norepinephrine system position it to contribute to stress-induced cardiovascular disease.
Individual differences in coping strategies during social stress parallel unique plasticity in LC afferent regulation.
Contrasting regulation of the LC would result in differences in cardiovascular regulation, likely contributing to individual differences in the cardiovascular consequences of stress.
Acknowledgments
Efforts of SKW were supported by a Scientist Development Grant from the American Heart Association 15SDG22430017 and the National Institute of Health (NIGMS) grant 5P20GM103641. Efforts of RJV were supported by 093981 and DA009082
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agorastos A, Boel JA, Heppner PS, Hager T, Moeller-Bertram T, Haji U, Motazedi A, Yanagi MA, Baker DG, Stiedl O. Diminished vagal activity and blunted diurnal variation of heart rate dynamics in posttraumatic stress disorder. Stress. 2013;16:300–310. doi: 10.3109/10253890.2012.751369. [DOI] [PubMed] [Google Scholar]
- Aston-Jones G, Bloom FE. Activity of norepinephrine-containing locus coeruleus neurons in behaving rats anticipates fluctuations in the sleep-waking cycle. J Neurosci. 1981a;1:876–886. doi: 10.1523/JNEUROSCI.01-08-00876.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aston-Jones G, Bloom FE. Norepinephrine-containing locus coeruleus neurons in behaving rats exhibit pronounced responses to non-noxious environmental stimuli. J Neurosci. 1981b;1:887–900. doi: 10.1523/JNEUROSCI.01-08-00887.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aston-Jones G, Cohen JD. An integrative theory of locus coeruleus-norepinephrine function: adaptive gain and optimal performance. Annual review of neuroscience. 2005;28:403–450. doi: 10.1146/annurev.neuro.28.061604.135709. [DOI] [PubMed] [Google Scholar]
- Aston-Jones G, Shipley MT, Chouvet G, Ennis M, Van Bockstaele EJ, Pieribone V, Shiekhattar R, Akaoka H, Drolet G, Astier B, Charlety P, Valentino R, Williams JT. Afferent regulation of locus coeruleus neurons: Anatomy, physiology and pharmacology. Prog Brain Res. 1991;85:47–75. doi: 10.1016/s0079-6123(08)63799-1. [DOI] [PubMed] [Google Scholar]
- Aston-Jones G, Shipley MT, Ennis M, Williams JT, Pieribone VA. Restricted afferent control of locus coeruleus neurons revealed by anatomical, physiological and pharmacological studies. In: Marsden CA, Heal DJ, editors. The Pharmacology of Noradrenaline in the Central Nervous System. Oxford University Press; Oxford, Great Britain: 1990. pp. 187–247. [Google Scholar]
- Aston-Jones G, Shipley MT, Grzanna R. The locus coeruleus, A5 and A7 noradrenergic cell groups. In: Paxinos G, editor. The Rat Brain. Academic Press; 1995. pp. 183–213. [Google Scholar]
- Beck CHM, Fibiger HC. Conditioned fear-induced changes in behavior and in the expression of the immediate early gene c-fos: with and without diazepam pretreatment. J Neurosci. 1995;15:709–720. doi: 10.1523/JNEUROSCI.15-01-00709.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge CW, Foote SL. Effects of locus coeruleus activation on electroencephalographic activity in the neocortex and hippocampus. J Neurosci. 1991;11:3135–3145. doi: 10.1523/JNEUROSCI.11-10-03135.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge CW, Page ME, Valentino RJ, Foote SL. Effects of locus coeruleus inactivation on electroencephalographic activity in neocortex and hippocampus. Neuroscience. 1993;55:381–383. doi: 10.1016/0306-4522(93)90507-c. [DOI] [PubMed] [Google Scholar]
- Black PH, Garbutt LD. Stress, inflammation and cardiovascular disease. J Psychosom Res. 2002;52:1–23. doi: 10.1016/s0022-3999(01)00302-6. [DOI] [PubMed] [Google Scholar]
- Bonaz B, Tache Y. Water-avoidance stress-induced c-fos expression in the rat brain and stimulation of fecal output: role of corticotropin-releasing factor. Brain Res. 1994;641:21–28. doi: 10.1016/0006-8993(94)91810-4. [DOI] [PubMed] [Google Scholar]
- Boone JB, Jr, McMillen D. Differential effects of prolonged restraint stress on proenkephalin gene expression in the brainstem. Brain Res Mol Brain Res. 1994;27:290–298. doi: 10.1016/0169-328x(94)90012-4. [DOI] [PubMed] [Google Scholar]
- Bouret S, Sara SJ. Network reset: a simplified overarching theory of locus coeruleus noradrenaline function. Trends Neurosci. 2005;28:574–582. doi: 10.1016/j.tins.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Britton KT, Segal DS, Kuczenski R, Hauger R. Dissociation between in vivo hippocampal norepinephrine response and behavioral/neuroendocrine responses to noise stress in rats. Brain Res. 1992;574:125–130. doi: 10.1016/0006-8993(92)90808-m. [DOI] [PubMed] [Google Scholar]
- Brown M. Corticotropin releasing factor: central nervous system sites of action. Brain Res. 1986;399:10–14. doi: 10.1016/0006-8993(86)90595-0. [DOI] [PubMed] [Google Scholar]
- Campeau S, Watson SJ. Neuroendocrine and behavioral response and brain pattern of c-fos induction associated with audiogenic stress. J Neuroendocrinol. 1997;9:577–588. doi: 10.1046/j.1365-2826.1997.00593.x. [DOI] [PubMed] [Google Scholar]
- Carnevali L, Trombini M, Porta A, Montano N, de Boer SF, Sgoifo A. Vagal withdrawal and susceptibility to cardiac arrhythmias in rats with high trait aggressiveness. PLoS One. 2013a;8:e68316. doi: 10.1371/journal.pone.0068316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnevali L, Trombini M, Rossi S, Graiani G, Manghi M, Koolhaas JM, Quaini F, Macchi E, Nalivaiko E, Sgoifo A. Structural and electrical myocardial remodeling in a rodent model of depression. Psychosom Med. 2013b;75:42–51. doi: 10.1097/PSY.0b013e318276cb0d. [DOI] [PubMed] [Google Scholar]
- Cassens G, Kuruc A, Roffman M, Orsulak PJ, Schildkraut JJ. Alterations in brain norepinephrine metabolism and behavior induced by environmental stimuli previously paired with inescapable shock. Brain Res. 1981;2:387–407. doi: 10.1016/0166-4328(81)90020-6. [DOI] [PubMed] [Google Scholar]
- Cassens G, Roffman M, Kuruc A, Orsulak PJ, Schildkraut JJ. Alterations in brain norepinephrine metabolism induced by environmental stimuli previously paired with inescapable shock. Science. 1980;209:1138–1139. doi: 10.1126/science.7403874. [DOI] [PubMed] [Google Scholar]
- Chaijale NN, Curtis AL, Wood SK, Zhang XY, Bhatnagar S, Reyes BA, Van Bockstaele EJ, Valentino RJ. Social stress engages opioid regulation of locus coeruleus norepinephrine neurons and induces a state of cellular and physical opiate dependence. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2013a;38:1833–1843. doi: 10.1038/npp.2013.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaijale NN, Curtis AL, Wood SK, Zhang XY, Bhatnagar S, Reyes BA, Van Bockstaele EJ, Valentino RJ. Social Stress Engages Opioid Regulation of Locus Coeruleus Norepinephrine Neurons and Induces a State of Cellular and Physical Opiate Dependence. Neuropsychopharmacology. 2013b doi: 10.1038/npp.2013.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan RKW, Sawchenko PE. Hemodynamic regulation of tyrosine hydroxylase messenger RNA in medullary catecholamine neurons: a c-fos-guided hybridization histochemical study. Neuroscience. 1995;66:377–390. doi: 10.1016/0306-4522(94)00600-a. [DOI] [PubMed] [Google Scholar]
- Chang MS, Sved AF, Zigmond MJ, Austin MC. Increased transcription of the tyrosine hydroxylase gene in individual locus coeruleus neurons following footshock stress. Neuroscience. 2000;101:131–139. doi: 10.1016/s0306-4522(00)00352-3. [DOI] [PubMed] [Google Scholar]
- Chen YY, Huang ZS. Stimulation of locus coeruleus increases arterial pressure in rabbits. Zhongguo yao li xue bao = Acta pharmacologica Sinica. 1997;18:437–440. [PubMed] [Google Scholar]
- Chiou RJ, Kuo CC, Liang KC, Yen CT. State-dependent amygdala stimulation-induced cardiovascular effects in rats. The Chinese journal of physiology. 2009;52:432–440. doi: 10.4077/cjp.2009.amh046. [DOI] [PubMed] [Google Scholar]
- Costoli T, Bartolomucci A, Graiani G, Stilli D, Laviola G, Sgoifo A. Effects of chronic psychosocial stress on cardiac autonomic responsiveness and myocardial structure in mice. Am J Physiol Heart Circ Physiol. 2004;286:H2133–2140. doi: 10.1152/ajpheart.00869.2003. [DOI] [PubMed] [Google Scholar]
- Crawley JN, Maas JW, Roth RH. Evidence against specificity of electrical stimulation of the nucleus locus coeruleus in activating the sympathetic nervous system in the rat. Brain Res. 1980;183:301–311. doi: 10.1016/0006-8993(80)90466-7. [DOI] [PubMed] [Google Scholar]
- Curtis AL, Bello NT, Connally KR, Valentino RJ. Corticotropin-releasing factor neurons of the central nucleus of the amygdala mediate locus coeruleus activation by cardiovascular stress. J Neuroendocrinol. 2002;14:667–682. doi: 10.1046/j.1365-2826.2002.00821.x. [DOI] [PubMed] [Google Scholar]
- Curtis AL, Bello NT, Valentino RJ. Endogenous opioids in the locus coeruleus function to limit the noradrenergic response to stress. J Neurosci. 2001;21:RC152. doi: 10.1523/JNEUROSCI.21-13-j0001.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis AL, Leiser SC, Snyder K, Valentino RJ. Predator stress engages corticotropin-releasing factor and opioid systems to alter the operating mode of locus coeruleus norepinephrine neurons. Neuropharmacology. 2012;62:1737–1745. doi: 10.1016/j.neuropharm.2011.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drolet G, Akaoka H, Van Bockstaele EJ, Aston-Jones G, Shipley MT. Opioid afferents to the locus coeruleus from the rostral medulla as detected by retrograde transport combined with immunohistochemistry. Soc Neurosci Abstr. 1990;16:1027. [Google Scholar]
- Drolet G, Gauthier P. Peripheral and central mechanisms of the pressor response elicited by stimulation of the locus coeruleus in the rat. Can J Physiol Pharmacol. 1985;63:599–605. doi: 10.1139/y85-100. [DOI] [PubMed] [Google Scholar]
- Drolet G, Van Bockstaele EB, Akaoka H, et al. Robust enkephalin innervation of the locus coeruleus from the rostral medulla. J Neurosci. 1992;12:3162–3174. doi: 10.1523/JNEUROSCI.12-08-03162.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dun NJ, Dun SL, Shen E, Tang H, Huang R, Chiu TH. c-fos expression as a marker of central cardiovascular neurons. Biol Signals. 1995;4:117–123. doi: 10.1159/000109431. [DOI] [PubMed] [Google Scholar]
- Duncan GE, Johnson KB, Breese GR. Topographic patterns of brain activity in response to swim stress: assessment by 2-deoxyglucose uptake and expression of fos-like immunoreactivity. J Neurosci. 1993;13:3932–3943. doi: 10.1523/JNEUROSCI.13-09-03932.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elam M, Svensson TH, Thoren P. Differentiated cardiovascular afferent regulation of locus coeruleus neurons and sympathetic nerves. Brain Res. 1985;358:77–84. doi: 10.1016/0006-8993(85)90950-3. [DOI] [PubMed] [Google Scholar]
- Elam M, Thoren P, Svensson TH. Locus coeruleus neurons and sympathetic nerves: activation by visceral afferents. Brain Res. 1986;375:117–125. doi: 10.1016/0006-8993(86)90964-9. [DOI] [PubMed] [Google Scholar]
- Foote SL, Aston-Jones G, Bloom FE. Impulse activity of locus coeruleus neurons in awake rats and monkeys is a function of sensory stimulation and arousal. Proc Natl Acad Sci US A. 1980;77:3033–3037. doi: 10.1073/pnas.77.5.3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk D, Amir S. Circadian modulation of fos resonses to odor of the red fox, a rodent predator, in the rat olfactory system. Brain Res. 2000;866:262–267. doi: 10.1016/s0006-8993(00)02249-6. [DOI] [PubMed] [Google Scholar]
- Gelsema AJ, Schoemaker RG, Ruzicka M, Copeland NE. Cardiovascular effects of social stress in borderline hypertensive rats. J Hypertens. 1994;12:1019–1028. [PubMed] [Google Scholar]
- Graham JC, Hoffman GE, Sved AF. c-fos expression in brain in response to hypotension and hypertension in conscious rats. J Auton Nerv Sys. 1995;55:92–104. doi: 10.1016/0165-1838(95)00032-s. [DOI] [PubMed] [Google Scholar]
- Grzanna R, Molliver ME. The locus coeruleus in the rat: an immunohistochemical delineation. Neuroscience. 1980;5:21–40. doi: 10.1016/0306-4522(80)90068-8. [DOI] [PubMed] [Google Scholar]
- Gurtu S, Pant KK, Sinha JN, Bhargava KP. An investigation into the mechanism of cardiovascular responses elicited by electrical stimulation of locus coeruleus and subcoeruleus in the cat. Brain Res. 1984;301:59–64. doi: 10.1016/0006-8993(84)90402-5. [DOI] [PubMed] [Google Scholar]
- Hawley DF, Bardi M, Everette AM, Higgins TJ, Tu KM, Kinsley CH, Lambert KG. Neurobiological constituents of active, passive, and variable coping strategies in rats: integration of regional brain neuropeptide Y levels and cardiovascular responses. Stress. 2010;13:172–183. doi: 10.3109/10253890903144621. [DOI] [PubMed] [Google Scholar]
- Ishida Y, Hashiguchi H, Takeda R, Ishizuka Y, Mitsuyama Y, Kannan H, Nishimori T, Nakahara D. Conditioned-fear stress increases Fos expression in monoaminergic and GABAergic neurons of the locus coeruleus and dorsal raphe nuclei. Synapse. 2002;45:46–51. doi: 10.1002/syn.10086. [DOI] [PubMed] [Google Scholar]
- Jones BE, Yang TZ. The efferent projections from the reticular formation and the locus coeruleus studied by anterograde and retrograde axonal transport in the rat. J Comp Neurol. 1985;242:56–92. doi: 10.1002/cne.902420105. [DOI] [PubMed] [Google Scholar]
- Kawamura H, Gunn CG, Frohlich ED. Cardiovascular alteration by nucleus locus coeruleus in spontaneously hypertensive rat. Brain Res. 1978;140:137–147. doi: 10.1016/0006-8993(78)90243-3. [DOI] [PubMed] [Google Scholar]
- Kollack-Walker S, Watson SJ, Akil H. Social stress in hamsters: defeat activates specific neurocircuits within the brain. J Neurosci. 1997;17:8842–8865. doi: 10.1523/JNEUROSCI.17-22-08842.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koolhaas JM, De Boer SF, De Rutter AJ, Meerlo P, Sgoifo A. Social stress in rats and mice. Acta Physiol Scand Suppl. 1997;640:69–72. [PubMed] [Google Scholar]
- Korf J, Aghajanian GK, Roth RH. Increased turnover of norepinephrine in the rat cerebral cortex during stress: role of the locus coeruleus. Neuropharmacology. 1973;12:933–938. doi: 10.1016/0028-3908(73)90024-5. [DOI] [PubMed] [Google Scholar]
- Kravets JL, Reyes BA, Unterwald EM, Van Bockstaele EJ. Direct targeting of peptidergic amygdalar neurons by noradrenergic afferents: linking stress-integrative circuitry. Brain Struct Funct. 2015;220:541–558. doi: 10.1007/s00429-013-0674-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan V, Han MH, Graham DL, Berton O, Renthal W, Russo SJ, Laplant Q, Graham A, Lutter M, Lagace DC, Ghose S, Reister R, Tannous P, Green TA, Neve RL, Chakravarty S, Kumar A, Eisch AJ, Self DW, Lee FS, Tamminga CA, Cooper DC, Gershenfeld HK, Nestler EJ. Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell. 2007;131:391–404. doi: 10.1016/j.cell.2007.09.018. [DOI] [PubMed] [Google Scholar]
- Lacosta S, Merali Z, Anisman H. Central monoamine activity following acute and repeated systemic interleukin-2 administration. Neuroimmunomodulation. 2000;8:83–90. doi: 10.1159/000026457. [DOI] [PubMed] [Google Scholar]
- Lechner S, Curtis A, Brons R, Valentino R. Locus coeruleus activation by colon distention: role of corticotropin-releasing factor and excitatory amino acids. Brain Res. 1997;756:114–124. doi: 10.1016/s0006-8993(97)00116-9. [DOI] [PubMed] [Google Scholar]
- Lombard CM, Melson MN, Muniz BL, Sanner C, Fadel JR, Wood CS, Wilson LB, Wood SK. The role of the locus coeruleus in the cardiovascular response to social stress is associated with coping strategy unpublished manuscript. [Google Scholar]
- Luppi PH, Aston-Jones G, Akaoka H, Chouvet G, Jouvet M. Afferent projections to the rat locus coeruleus demonstrated by retrograde and anterograde tracing with cholera-toxin B subunit and phaseolus vulgaris leucoagglutinin. Neuroscience. 1995;65:119–160. doi: 10.1016/0306-4522(94)00481-j. [DOI] [PubMed] [Google Scholar]
- Makino S, Smith MA, Gold PW. Regulatory role of glucocorticoids and glucocorticoid receptor mRNA levels on tyrosine hydroxylase gene expression in the locus coeruleus during repeated immobilization stress. Brain Res. 2002;943:216–223. doi: 10.1016/s0006-8993(02)02647-1. [DOI] [PubMed] [Google Scholar]
- Mansour A, Fox CA, Thompson RC, Akil H, Watson SJ. mu-Opioid receptor mRNA expression in the rat CNS: comparison to mu-receptor binding. Brain research. 1994;643:245–265. doi: 10.1016/0006-8993(94)90031-0. [DOI] [PubMed] [Google Scholar]
- Mason ST, Fibiger HC. Regional topography within noradrenergic locus coeruleus as revealed by retrograde transport of horseradish peroxidase. J Comp Neurol. 1979;187:703–724. doi: 10.1002/cne.901870405. [DOI] [PubMed] [Google Scholar]
- McKitrick DJ, Calaresu FR. Nucleus ambiguus inhibits activity of cardiovascular units in RVLM. Brain Res. 1996;742:203–210. doi: 10.1016/s0006-8993(96)00971-7. [DOI] [PubMed] [Google Scholar]
- Meerlo P, Sgoifo A, De Boer SF, Koolhaas JM. Long-lasting consequences of a social conflict in rats: behavior during the interaction predicts subsequent changes in daily rhythms of heart rate, temperature, and activity. Behav Neurosci. 1999;113:1283–1290. doi: 10.1037//0735-7044.113.6.1283. [DOI] [PubMed] [Google Scholar]
- Miczek KA, Covington HE, 3rd, Nikulina EM, Jr, Hammer RP. Aggression and defeat: persistent effects on cocaine self-administration and gene expression in peptidergic and aminergic mesocorticolimbic circuits. Neuroscience and biobehavioral reviews. 2004;27:787–802. doi: 10.1016/j.neubiorev.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Minassian A, Geyer MA, Baker DG, Nievergelt CM, O’Connor DT, Risbrough VB Marine Resiliency Study T. Heart rate variability characteristics in a large group of active-duty marines and relationship to posttraumatic stress. Psychosom Med. 2014;76:292–301. doi: 10.1097/PSY.0000000000000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napadow V, Dhond R, Conti G, Makris N, Brown EN, Barbieri R. Brain correlates of autonomic modulation: combining heart rate variability with fMRI. Neuro Image. 2008;42:169–177. doi: 10.1016/j.neuroimage.2008.04.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak V, Saul JP, Eckberg DL. Task Force report on heart rate variability. Circulation. 1997;96:1056–1057. [PubMed] [Google Scholar]
- Orth-Gomer K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman MA. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA. 2000;284:3008–3014. doi: 10.1001/jama.284.23.3008. [DOI] [PubMed] [Google Scholar]
- Paakkari I, Siren AL, Nurminen ML, Svartstrom-Fraser M. Injection of thyrotropin releasing hormone into the locus coeruleus increases blood pressure. Eur Heart J. 1987;8(Suppl B):147–151. doi: 10.1093/eurheartj/8.suppl_b.147. [DOI] [PubMed] [Google Scholar]
- Page ME, Berridge CW, Foote SL, Valentino RJ. Corticotropin-releasing factor in the locus coeruleus mediates EEG activation associated with hypotensive stress. Neurosci Lett. 1993;164:81–84. doi: 10.1016/0304-3940(93)90862-f. [DOI] [PubMed] [Google Scholar]
- Plotsky PM, Vale W. Hemorrhage-induced secretion of corticotropin-releasing factor-like immunoreactivity into the rat hypophyseal portal circulation and its inhibition by glucocorticoids. Endocrinology. 1984;114:164–169. doi: 10.1210/endo-114-1-164. [DOI] [PubMed] [Google Scholar]
- Punnen S, Willette R, Krieger AJ, Sapru HN. Cardiovascular response to injections of enkephalin in the pressor area of the ventrolateral medulla. Neuropharmacology. 1984;23:939–946. doi: 10.1016/0028-3908(84)90008-x. [DOI] [PubMed] [Google Scholar]
- Rajkowski J, Kubiak P, Aston-Jones G. Activity of locus coeruleus neurons in monkey: phasic and tonic changes correspond to altered vigilance. Brain Res Bull. 1994;35:607–616. doi: 10.1016/0361-9230(94)90175-9. [DOI] [PubMed] [Google Scholar]
- Reyes BA, Zitnik G, Foster C, Van Bockstaele EJ, Valentino RJ. Social Stress Engages Neurochemically-Distinct Afferents to the Rat Locus Coeruleus Depending on Coping Strategy(1,2,3) eNeuro. 2015a;2 doi: 10.1523/ENEURO.0042-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes BA, Zitnik GA, Foster C, Van Bockstaele EJ, Valentino RJ. Social Stress Engages Neurochemically-Distinct Afferents to the Rat Locus Coeruleus Depending on Coping Strategy. [accepted October 20, 2015];eNeuro. 2015b doi: 10.1523/ENEURO.0042-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson SD, Plummer NW, de Marchena J, Jensen P. Developmental origins of central norepinephrine neuron diversity. Nat Neurosci. 2013;16:1016–1023. doi: 10.1038/nn.3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi-amorn C, Sato H, Yusuf S investigators I. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- Rusnak M, Kvetnansky R, Jelokova J, Palkovits M. Effect of novel stressors on gene expression of tyrosine hydroxylase and monoamine transporters in brainstem noradrenergic neurons of long-term repeatedly immobilized rats. Brain Res. 2001;899:20–35. doi: 10.1016/s0006-8993(01)02126-6. [DOI] [PubMed] [Google Scholar]
- Rygula R, Abumaria N, Flugge G, Fuchs E, Ruther E, Havemann-Reinecke U. Anhedonia and motivational deficits in rats: impact of chronic social stress. Behav Brain Res. 2005;162:127–134. doi: 10.1016/j.bbr.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Sabban EL, Kvetnansky R. Stress-triggered activation of gene expression in catecholaminergic systems: dynamics of transcriptional events. Trends Neurosci. 2001;24:91–98. doi: 10.1016/s0166-2236(00)01687-8. [DOI] [PubMed] [Google Scholar]
- Samuels ER, Szabadi E. Functional neuroanatomy of the noradrenergic locus coeruleus: its roles in the regulation of arousal and autonomic function part I: principles of functional organisation. Curr Neuropharmacol. 2008a;6:235–253. doi: 10.2174/157015908785777229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuels ER, Szabadi E. Functional Neuroanatomy of the Noradrenergic Locus Coeruleus: Its Roles in the Regulation of Arousal and Autonomic Function Part II: Physiological and Pharmacological Manipulations and Pathological Alterations of Locus Coeruleus Activity in Humans. Curr Neuropharmacol. 2008b;6:254–285. doi: 10.2174/157015908785777193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders BJ, Wirtz-Nole C, DeFord SM, Erling BF. Central amygdaloid lesions attenuate cardiovascular responses to acute stress in rats with borderline hypertension. Physiol Behav. 1994;56:709–713. doi: 10.1016/0031-9384(94)90231-3. [DOI] [PubMed] [Google Scholar]
- Schwarz LA, Luo L. Organization of the Locus Coeruleus-Norepinephrine System. Curr Biol. 2015;25:R1051–1056. doi: 10.1016/j.cub.2015.09.039. [DOI] [PubMed] [Google Scholar]
- Sgoifo A, Carnevali L, Grippo AJ. The socially stressed heart. Insights from studies in rodents. Neurosci Biobehav Rev. 2014;39:51–60. doi: 10.1016/j.neubiorev.2013.12.005. [DOI] [PubMed] [Google Scholar]
- Sgoifo A, Koolhaas JM, Musso E, De Boer SF. Different sympathovagal modulation of heart rate during social and nonsocial stress episodes in wild-type rats. Physiol Behav. 1999;67:733–738. doi: 10.1016/s0031-9384(99)00134-1. [DOI] [PubMed] [Google Scholar]
- Sgoifo A, Pozzato C, Meerlo P, Costoli T, Manghi M, Stilli D, Olivetti G, Musso E. Intermittent exposure to social defeat and open-field test in rats: acute and long-term effects on ECG, body temperature and physical activity. Stress. 2002;5:23–35. doi: 10.1080/102538902900012387. [DOI] [PubMed] [Google Scholar]
- Shah AJ, Lampert R, Goldberg J, Veledar E, Bremner JD, Vaccarino V. Posttraumatic stress disorder and impaired autonomic modulation in male twins. Biol Psychiatry. 2013;73:1103–1110. doi: 10.1016/j.biopsych.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipley MT, Fu L, Ennis M, Liu W, Aston-Jones G. Dendrites of locus coeruleus neurons extend preferentially into two pericoerulear zones. J Comp Neurol. 1996;365:56–68. doi: 10.1002/(SICI)1096-9861(19960129)365:1<56::AID-CNE5>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- Smagin GN, Swiergiel AH, Dunn AJ. Sodium nitroprusside infusions activate cortical and hypothalamic noradrenergic systems in rats. Neurosci Res Comm. 1994;14:85–91. [Google Scholar]
- Smith MA, Banerjee S, Gold PW, Glowa J. Induction of c-fos mRNA in rat brain by conditioned and unconditioned stressors. Brain Res. 1992;578:135–141. doi: 10.1016/0006-8993(92)90240-a. [DOI] [PubMed] [Google Scholar]
- Smith MA, Brady LS, Glowa J, Gold PW, Herkenham M. Effects of stress and adrenalectomy on tyrosine hydroxylase mRNA levels in the locus ceruleus by in situ hybridization. Brain Res. 1991;544:26–32. doi: 10.1016/0006-8993(91)90881-u. [DOI] [PubMed] [Google Scholar]
- Snyder K, Wang WW, Han R, McFadden K, Valentino RJ. Corticotropin-releasing factor in the norepinephrine nucleus, locus coeruleus, facilitates behavioral flexibility. Neuropsychopharmacology. 2012;37:520–530. doi: 10.1038/npp.2011.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick SM, Bremner JD, Rasmusson A, Morgan CA, 3rd, Arnsten A, Charney DS. Role of norepinephrine in the pathophysiology and treatment of posttraumatic stress disorder. Biol Psychiatry. 1999;46:1192–1204. doi: 10.1016/s0006-3223(99)00219-x. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Krystal JH, Bremner JD, Morgan CA, 3rd, Nicolaou AL, Nagy LM, Johnson DR, Heninger GR, Charney DS. Noradrenergic and serotonergic function in posttraumatic stress disorder. Arch Gen Psychiatry. 1997;54:749–758. doi: 10.1001/archpsyc.1997.01830200083012. [DOI] [PubMed] [Google Scholar]
- Spyer KM. Central nervous control of the cardiovascular system. In: Bannister R, Mathias CJ, editors. Autonomic Failure. 3. Oxford University Press; Oxford: 1992. pp. 54–77. [Google Scholar]
- Standish A, Enquist LW, Escardo JA, Schwaber JS. Central neuronal circuit innervating the rat heart defined by transneuronal transport of pseudorabies virus. The Journal of neuroscience: the official journal of the Society for Neuroscience. 1995;15:1998–2012. doi: 10.1523/JNEUROSCI.15-03-01998.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sved AF, Felsten G. Stimulation of the locus coeruleus decreases arterial pressure. Brain Res. 1987;414:119–132. doi: 10.1016/0006-8993(87)91332-1. [DOI] [PubMed] [Google Scholar]
- Svensson TH. Peripheral, autonomic regulation of locus coeruleus noradrenergic neurons in brain: Putative implications for psychiatry and psychopharmacology. Psychopharmacology. 1987;92:1–7. doi: 10.1007/BF00215471. [DOI] [PubMed] [Google Scholar]
- Swanson LW, Hartman BK. The central adrenergic system. An immunofluorescence study of the location of cell bodies and their efferent connections in the rat using dopamine-B-hydroxylase as a marker. J Comp Neurol. 1976;163:467–506. doi: 10.1002/cne.901630406. [DOI] [PubMed] [Google Scholar]
- Tang F, Lane S, Korsak A, Paton JF, Gourine AV, Kasparov S, Teschemacher AG. Lactate-mediated glia-neuronal signalling in the mammalian brain. Nature communications. 2014;5:3284. doi: 10.1038/ncomms4284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempel A, Zukin RS. Neuroanatomical patterns of the μ, d and k opioid receptors of rat brain as determined by quantitative in vitro autoradiography. Proc Natl Acad Sci U S A. 1987;84:4308–4312. doi: 10.1073/pnas.84.12.4308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Horst GJ, Toes GJ, Van Willigen JD. Locus coeruleus projections to the dorsal motor vagus nucleus in the rat. Neuroscience. 1991;45:153–160. doi: 10.1016/0306-4522(91)90111-z. [DOI] [PubMed] [Google Scholar]
- Thierry AM, Javoy F, Glowinski J, Kety SS. Effects of stress on the metabolism of norepinephrine, dopamine and serotonin in the central nervous system of the rat: modification of norpinephrine turnover. J Pharmacol Exp Ther. 1968;163:163–171. [PubMed] [Google Scholar]
- Tornatzky W, Miczek KA. Behavioral and autonomic responses to intermittent social stress: differential protection by clonidine and metoprolol. Psychopharmacology (Berl) 1994;116:346–356. doi: 10.1007/BF02245339. [DOI] [PubMed] [Google Scholar]
- Tsuji H, Larson MG, Venditti FJ, Jr, Manders ES, Evans JC, Feldman CL, Levy D. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation. 1996;94:2850–2855. doi: 10.1161/01.cir.94.11.2850. [DOI] [PubMed] [Google Scholar]
- Usher M, Cohen JD, Servan-Schreiber D, Rajkowski J, Aston-Jones G. The role of locus coeruleus in the regulation of cognitive performance. Science. 1999;283:549–554. doi: 10.1126/science.283.5401.549. [DOI] [PubMed] [Google Scholar]
- Valentino RJ, Foote SL. Corticotropin-releasing factor disrupts sensory responses of brain noradrenergic neurons. Neuroendocrinology. 1987;45:28–36. doi: 10.1159/000124700. [DOI] [PubMed] [Google Scholar]
- Valentino RJ, Foote SL. Corticotropin-releasing factor increases tonic but not sensory-evoked activity of noradrenergic locus coeruleus neurons in unanesthetized rats. J Neurosci. 1988;8:1016–1025. doi: 10.1523/JNEUROSCI.08-03-01016.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentino RJ, Page ME, Curtis AL. Activation of noradrenergic locus coeruleus neurons by hemodynamic stress is due to local release of corticotropin-releasing factor. Brain Res. 1991;555:25–34. doi: 10.1016/0006-8993(91)90855-p. [DOI] [PubMed] [Google Scholar]
- Valentino RJ, Van Bockstaele E. Convergent regulation of locus coeruleus activity as an adaptive response to stress. Eur J Pharmacol. 2008;583:194–203. doi: 10.1016/j.ejphar.2007.11.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentino RJ, Wehby RG. Corticotropin-releasing factor: Evidence for a neurotransmitter role in the locus coeruleus during hemodynamic stress. Neuroendocrinology. 1988;48:674–677. doi: 10.1159/000125081. [DOI] [PubMed] [Google Scholar]
- Van Bockstaele EJ, Aston-Jones G. Integration in the ventral medulla and coordination of sympathetic, pain and arousal functions. Clin Exp Hypertens. 1995;17:153–165. doi: 10.3109/10641969509087062. [DOI] [PubMed] [Google Scholar]
- Van Bockstaele EJ, Bajic D, Proudfit H, Valentino RJ. Topographic architecture of stress-related pathways targeting the noradrenergic locus coeruleus. Physiol Behav. 2001;73:273–283. doi: 10.1016/s0031-9384(01)00448-6. [DOI] [PubMed] [Google Scholar]
- Van Bockstaele EJ, Colago EEO, Valentino RJ. Amygdaloid corticotropin-releasing factor targets locus coeruleus dendrites: substrate for the coordination of emotional and cognitive limbs of the stress response. J Neuroendocrinol. 1998;10:743–757. doi: 10.1046/j.1365-2826.1998.00254.x. [DOI] [PubMed] [Google Scholar]
- Van Bockstaele EJ, Peoples J, Valentino RJ. Differential regulation of the rostrolateral peri-locus coeruleus region by limbic afferents. Biol Psych. 1999;46:1352–1363. doi: 10.1016/s0006-3223(99)00213-9. [DOI] [PubMed] [Google Scholar]
- Wang X, Pinol RA, Byrne P, Mendelowitz D. Optogenetic stimulation of locus ceruleus neurons augments inhibitory transmission to parasympathetic cardiac vagal neurons via activation of brainstem alpha1 and beta1 receptors. J Neurosci. 2014;34:6182–6189. doi: 10.1523/JNEUROSCI.5093-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JT, Marshall KC. Membrane properties and adrenergic responses in locus coeruleus neurons of young rats. The Journal of neuroscience: the official journal of the Society for Neuroscience. 1987;7:3687–3694. doi: 10.1523/JNEUROSCI.07-11-03687.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong ML, Kling MA, Munson PJ, Listwak S, Licinio J, Prolo P, Karp B, McCutcheon IE, Geracioti TD, Jr, DeBellis MD, Rice KC, Goldstein DS, Veldhuis JD, Chrousos GP, Oldfield EH, McCann SM, Gold PW. Pronounced and sustained central hypernoradrenergic function in major depression with melancholic features: relation to hypercortisolism and corticotropin-releasing hormone. Proc Natl Acad Sci U S A. 2000;97:325–330. doi: 10.1073/pnas.97.1.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood SK. Cardiac autonomic imbalance by social stress in rodents: understanding putative biomarkers. Frontiers in psychology. 2014;5:950. doi: 10.3389/fpsyg.2014.00950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood SK, Bhatnagar S. Resilience to the effects of social stress: evidence from clinical and preclinical studies on the role of coping strategies. Neurobiology of stress. 2015;1:164–173. doi: 10.1016/j.ynstr.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood SK, McFadden KV, Grigoriadis D, Bhatnagar S, Valentino RJ. Depressive and cardiovascular disease comorbidity in a rat model of social stress: a putative role for corticotropin-releasing factor. Psychopharmacology. 2012;222:325–336. doi: 10.1007/s00213-012-2648-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood SK, Walker HE, Valentino RJ, Bhatnagar S. Individual differences in reactivity to social stress predict susceptibility and resilience to a depressive phenotype: role of corticotropin-releasing factor. Endocrinology. 2010;151:1795–1805. doi: 10.1210/en.2009-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood SK, Wood CS, Lombard CM, Lee CS, Zhang XY, Finnell JE, Valentino RJ. Inflammatory Factors Mediate Vulnerability to a Social Stress-Induced Depressive-like Phenotype in Passive Coping Rats. Biol Psychiatry. 2015;78:38–48. doi: 10.1016/j.biopsych.2014.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitnik GA, Curtis AL, Wood SK, Arner J, Valentino RJ. Adolescent Social Stress Produces an Enduring Activation of the Rat Locus Coeruleus and Alters its Coherence with the Prefrontal Cortex. Neuropsychopharmacology. 2015 doi: 10.1038/npp.2015.289. [DOI] [PMC free article] [PubMed] [Google Scholar]