Introduction
The cancer of the larynx accounts for 30–40 % of the head and neck carcinomas and 1–2.5 % of the whole human malignancies. Squamous cell carcinoma is the predominant histological type and it represents 90–95 % of the newly diagnosed cases. Other histologies include neuroendocrine carcinoma, adenocarcinoma, adenoid cystic carcinoma, sarcomas, primary lymphoma, plasmacytoma and metastatic malignancies. Extramedullary plasmacytoma of the Larynx constitutes only 0.4–0.45 % of the malignant tumours of the larynx and <1 % of all Head and Neck malignancies. It presents with change in voice, breathing difficulty, stridor or dysphagia similar to carcinoma larynx. We report a case of plasmacytoma of the larynx which was mimicking carcinoma larynx and later on evaluation was found to have Multiple myeloma [1–4].
Case Report
A 44 year old female presented with history of hoarseness for 3 months and stridor and an emergency tracheostomy was done. She did not had any history dysphagia or tiredness. She had no addictions nor co-morbidities. On evaluation there was a mucosa covered smooth swelling over left aryetenoid, aryepiglottic fold and left pyriform sinus and the left hemilarynx was fixed. There was no pallor or lymphnode enlargement. CT evaluation was showing a soft tissue lesion involving left pyriform sinus, left arytenoids and AEF with thyroid cartilage destruction and extralryngeal spread. The clinical examination and the radiological findings were in favor of carcinoma larynx. Direct laryngoscopy and biopsy was attempted three times and an ultrasound guided FNAC was done once, but the histopathology reports were inconclusive. Her haematological and biochemical parameters were normal.
An open biopsy was done under frozen control and the report turned out to be plasmacytoma. The microscopic study revealed intense basophilic plasma cells which invade the submucosal tissues and there was CD138-positive immunohistochemistry, that is characteristic of EMP (Fig. 1). Then a bone marrow aspiration was done and the result was a myeloid: erythroid ratio of 6:1, with both series having normoblastic maturation and there was 45 % plasma cells including immature forms. The findings were compatible with a diagnosis of Multiple myeloma. She was referred to Medical Oncologist for further management.
Fig. 1.
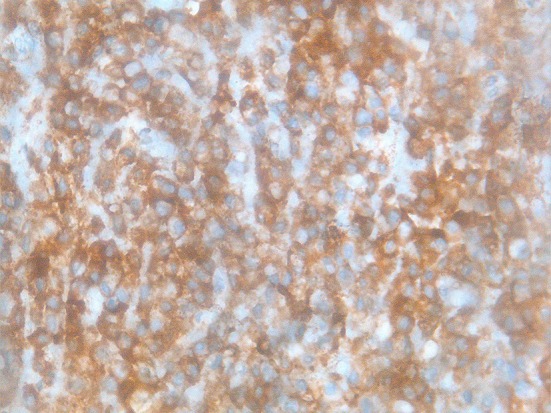
Histopathological picture showing plasma cells
Discussion: The incidence of myeloma is approximately 3.5 per one lakh population. Solitary plasmacytoma constitutes around 2 % of all cases of myeloma. Solitary plasmacytoma is defined as a localized accumulation of neoplastic monoclonal plasma cells without evidence of a systemic plasma cell proliferative disorder. Solitary plasmacytoma can be classified based on location; plasmacytoma of the bone or extramedullary plasmacytoma (EMP) [3–5].
Eighty percentage of exramedullary plasmacytoma occur in the head and neck, usually in the upper respiratory tract. Extramedullary plasmacytoma of the Larynx represents 0.4–0.45 % of the malignant tumours of the larynx and <1 % of all Head and Neck malignancies. Most patients are male, with a reported male to female ratio of 3: 1. According to Alexiou et al. it occurs in the upper aerodigestive tract in more than 80 % of patients, most often in the nasal cavity, paranasal sinuses, nasopharynx, tonsils, and larynx. They also documented a male predominance and an advanced age at presentation for extramedullary plasmacytoma. Saad et al. reported that the most common sites of presentation of laryngeal plasmacytomas are in decreasing order of frequency are the epiglottis, vocal cords, ventricular bands, the arytenoids and finally the subglottic space. EMP is typically presents as a well-localized submucosal swelling, sometimes with polypoidal configuration. Presenting symptoms of EMP of head and neck are frequently secondary to local destruction and tumor mass [2, 6–8].
According to the data from Slovenia Cancer registry, during the 31-year period (1969–1999), among the 181,000 new cancer patients registered, only 1356 had plasma cell neoplasms (0.75 %) and among them only 26 patients were reported with EMP [9].
In patients with solitary plasmacytoma, progression to multiple myeloma is common and approximately 5 % of all patients with multiple myeloma have an initial diagnosis of solitary plasmacytoma. In a study by Alexiou et al. 16 % of patients with extramedullary plasmacytoma progressed to multiple myeloma [6, 7].
Hughes et al. told that with EMP the computed tomography (CT) usually reveals a homogeneous laryngeal mass with well-defined margins, which appears with a mild to moderate contrast enhancement [10].
EMP is highly radiosensive and is the recommended treatment of choice, even though the optimal dose and the role of elective irradiation of regional lymphatics are debated. The reported tumour control rate with radiotherapy is 100 %. Surgery can also be considered as a first line therapy so as to avoid the long term side effects of radiotherapy. However, it is more often employed as a salvage procedure. In a large review of >400 publications between 1905 and 1997, Alexiou et al. reported that surgery alone gave the best results for extramedullary Solitary plasmacytoma, when clear surgical margins were obtained. The role of chemotherapy in the treatment of primary tumors or recurrent disease or in preventing or delaying progression to multiple myeloma is controversial.
The overall 10 year survival rate ranges from 45 to 100 %, the difference is in accordance with the rate of conversion to Multiple myeloma [7, 11–14].
Conclusion
Extramedullary plasmacytoma of the larynx is very rare. But when we come across a patient with submucosal disease in the larynx or hypopharynx, we should keep in mind the possibilities of rare histological diagnosis including plasmacytoma; otherwise the situation will lead to diagnostic dilemma and a correct diagnosis and management will be delayed.
Compliance with Ethical Standards
Conflict of interest
None.
Ethical Issues
Informed written consent has been obtained from the patient.
References
- 1.Strojan P. Extramedullary plasmacytoma of the larynx: a report of three cases. Radiol Oncol. 2002;3:225–254. [Google Scholar]
- 2.Anguiano SR, Sanchez HL, Banos MD, Benıte BM. Extramedullary plasmacytoma of the larynx: a case report of subglottic localization. Case Rep Otolaryngol. 2012;2:1–3. doi: 10.1155/2012/437264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richard A, Lebowitz RA, Morris L. Plasma cell dyscrasias and amyloidosis. Otolaryngol Clin North Am. 2003;36:747–764. doi: 10.1016/S0030-6665(03)00026-4. [DOI] [PubMed] [Google Scholar]
- 4.Knowling MA, Harwood AR, Bergsagel DE. Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of bone. J Clin Oncol. 1983;1:255–262. doi: 10.1200/JCO.1983.1.4.255. [DOI] [PubMed] [Google Scholar]
- 5.Hernandez JA, Land KJ, McKenna RW. Leukemias, myeloma, and other lymphoreticular neoplasms. Cancer. 1995;75:381–394. doi: 10.1002/1097-0142(19950101)75:1+<381::AID-CNCR2820751320>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 6.Liebross RH, Ha CS, Cox JD, et al. Clinical course of solitary extramedullary plasmacytoma. Radiother Oncol. 1999;52:245–249. doi: 10.1016/S0167-8140(99)00114-0. [DOI] [PubMed] [Google Scholar]
- 7.Alexiou C, Kau RJ, Dietzfelbinger H, et al. Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts. Cancer. 1999;85:2305–2314. doi: 10.1002/(SICI)1097-0142(19990601)85:11<2305::AID-CNCR2>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 8.Saad R, Raab S, Liu Y, Pollice P, Silverman JF. Plasmacytoma of the larynx diagnosed by fine-needle aspiration cytology: a case report. Diagn Cytopathol. 2001;24(6):408–411. doi: 10.1002/dc.1090. [DOI] [PubMed] [Google Scholar]
- 9.Strojan P, et al. Extramedullary plasmacytoma: clinical and histopathological study. Int J Radiat Oncol Biol Phys. 2002;53(3):692–701. doi: 10.1016/S0360-3016(02)02780-3. [DOI] [PubMed] [Google Scholar]
- 10.Hughes M et al (2009) Guidelines on the diagnosis and management of solitary plasmacytoma of bone, extramedullary plasmacytoma and multiple solitary plasmacytomas: 2009 update
- 11.Navalon CG, Carceller MA, Marco VS, Ferrer RR, Moya-Angeler SF, Alegria JB, et al. Solitary extramedullary plasmocytoma of tubaric tonsil. Acta Otorrinolaringol Esp (Spain) 2009;60:301–303. doi: 10.1016/j.otorri.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Jyothirmayi R, Gangadharan VP, Nair MK, et al. Radiotherapy in the treatment of solitary plasmacytoma. Br J Radiol. 1997;70:511–516. doi: 10.1259/bjr.70.833.9227234. [DOI] [PubMed] [Google Scholar]
- 13.Creach KM, et al. Radiotherapy for extramedullary plasmacytoma of the head and neck. Int J Radiat Oncol Biol Phys. 2009;73:789–794. doi: 10.1016/j.ijrobp.2008.04.077. [DOI] [PubMed] [Google Scholar]
- 14.Tsang RW, et al. Solitary plasmacytoma treated with radiotherapy: impact of tumour size on outcome. Int J Radiat Oncol Biol Phys. 2001;50(1):113–120. doi: 10.1016/S0360-3016(00)01572-8. [DOI] [PubMed] [Google Scholar]


