Abstract
AIM
To determine the overall and comparative risk of procedure related perforation of balloon assisted enteroscopy (BAE) in Crohn’s disease (CD).
METHODS
Systematic review (PROSPERO #CRD42015016381) of studies reporting on CD patients undergoing BAE. Seventy-three studies reporting on 1812 patients undergoing 2340 BAEs were included. Primary outcome of interest was the overall and comparative risk of procedure related perforation of diagnostic BAE in CD. Secondary outcomes of interest were risk of procedure related perforation of diagnostic double balloon enteroscopy (DBE), risk of procedure related perforation of therapeutic BAE, efficacy of stricture dilation, and clinical utility of endoscopically assessing small bowel disease activity.
RESULTS
Per procedure perforation rate of diagnostic BAE in CD was 0.15% (95%CI: 0.05-0.45), which was similar to diagnostic BAE for all indications (0.11%; IRR = 1.41, 95%CI: 0.28-4.50). Per procedure perforation rate of diagnostic DBE in CD was 0.12% (95%CI: 0.03-0.44), which was similar to diagnostic DBE for all indications (0.22%; IRR = 0.54, 95%CI: 0.06-0.24). Per procedure perforation rate of therapeutic BAE in CD was 1.74% (95%CI: 0.85-3.55). Eighty-six percent of therapeutic perforations were secondary to stricture dilation. Dilation was attempted in 207 patients and 30% required surgery during median follow-up of 18 months. When diagnostic BAE assessed small bowel disease activity, changes in medical therapy resulted in endoscopic improvement in 77% of patients.
CONCLUSION
Diagnostic BAE in CD has a similar rate of perforation as diagnostic BAE for all indications and can be safely performed in assessment of mucosal healing.
Keywords: Crohn’s disease, Balloon, Enteroscopy, Safety, Perforation, Stricture
Core tip: Crohn’s disease (CD) affects the small bowel in up to 60% of patients, but evaluation of small bowel disease is often difficult. Balloon assisted enteroscopy (BAE) can evaluate the small bowel but its safety and diagnostic utility is not established. This systematic review includes 73 studies reporting on 1812 patients undergoing 2340 procedures to evaluate its safety and possible utility. We found that diagnostic BAE in CD had a similar rate of perforation as diagnostic BAE for all indications, suggesting BAE is a safe method for small bowel evaluation in CD.
INTRODUCTION
Crohn’s disease (CD) is a debilitating chronic inflammatory bowel disease (IBD), which if left untreated, leads to penetrating complications (strictures, fistulae, abscesses)[1-3]. Frequent disease activity assessment with the intent of adjusting therapy has been demonstrated to significantly reduce the risk of disease related complications[4-10]. Small bowel involvement in CD is reported to occur in up to 60% of patients, with nearly 30% of patients having isolated small bowel disease[11-13]. Conventional upper and lower endoscopy, however, are limited in their ability to assess small bowel disease activity[14-18], and clinical or biochemical markers of disease activity infrequently correlate with small bowel mucosal inflammation[19]. The presence of inflammation cannot be reliably excluded by radiological imaging alone[20], and video capsule endoscopy (VCE) carries a risk for capsule retention in structuring or penetrating disease and it lacks therapeutic capability[21-24].
Balloon assisted enteroscopy (BAE) offers the advantage of providing both diagnostic (mucosal biopsies) and therapeutic (stricture dilation) potential, but its use in CD is currently limited to symptomatic patients with negative ileocolonoscopy, VCE, and/or cross sectional imaging, and the feasibility and diagnostic utility of routine BAE in clinical practice for CD is yet to be established[20,25-29]. Therefore, we performed a systematic review of the literature to quantify the safety and therapeutic utility of this endoscopic technique. We anticipate these data will help to better characterize the growing importance of BAE in CD.
MATERIALS AND METHODS
Data sources and search strategy
The following databases were searched in October 2015: MEDLINE (PubMed, January 1946 to October 3, 2015); Cochrane Central Register of Controlled Trials (Wiley, 2015); and Embase (Embase.com, January 1974 to October 3, 2015). The search included indexed terms and text words to capture the following concepts: CD and balloon enteroscopy. There were no language or study design restrictions. The search strategy was adjusted for the syntax appropriate for each database. The reference lists of included articles and review articles were examined for additional relevant studies. The full search strategy, a priori, is available at the international prospective register of systematic reviews (PROSPERO #CRD42015016381).
Study selection and extraction
Studies were included for analysis if they met the following inclusion criteria: Randomized controlled trials, cohort studies, published meeting abstracts, or case series of 5 or more consecutive patients with CD, undergoing BAE for diagnostic or therapeutic purposes. Review articles and studies with fewer than 5 patients with CD were excluded. Studies with insufficient data for adverse outcomes and follow-up were excluded only after attempting to contact the primary author(s). The included population was patients of all ages with CD undergoing BAE for diagnostic and/or therapeutic purposes with clearly reported adverse outcomes. Comparative studies to assess diagnostic performance, therapeutic utility, and safety of BAE were included.
Two reviewers (Arulanandan A and Dulai PS) independently evaluated each of the articles for eligibility. Inclusion decisions for each article were made independently based on the eligibility criteria, with disagreements being resolved by a third reviewer (Kalmaz D) and consensus. A reviewer (Arulanandan A contacted the primary author(s) as required to obtain any necessary missing data from the original publications and because no language restrictions were applied, publications were translated into English as required. The reviewers followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses standards for systematic review.
Outcomes
Our primary outcome of interest was the safety of diagnostic BAE [single (SBE) or double (DBE) balloon enteroscopy) in CD, for which we calculated per procedure perforation rate and compared that to per procedure perforation rate when using diagnostic BAE for all indications. The expected rate of perforation when utilizing diagnostic BAE for all indications was derived from a Japanese database of 29068 patients[30].
Secondary outcome of interest was the safety of diagnostic DBE in CD, for which we calculated per procedure perforation rate and compared that to per procedure perforation rate when using diagnostic DBE for all indications. The expected rate of perforation when utilizing diagnostic DBE for all indications was derived from a systematic review of 9047 DBEs[31]. Other outcomes of interest were risk of procedure related perforation of therapeutic BAE, efficacy of stricture dilation, and clinical utility of endoscopically assessing small bowel disease activity.
Statistical analysis
We used the random-effects model described by DerSimonian and Laird to calculate pooled rates (and 95%CI) of perforation with BAE, stratified by indication (diagnostic vs therapeutic)[32]. Due to lack of consistent reporting in multiple studies, we did not perform a quantitative meta-analysis of factors associated with perforation, but rather discussed them qualitatively. The STATA “incidence ratio (IR)” command (version 10.0; STATA, College Station, TX, United States) was used to make comparisons for perforation rates, and the relative rates for perforation were calculated as incidence rate ratios (IRRs).
RESULTS
Patient and study characteristics
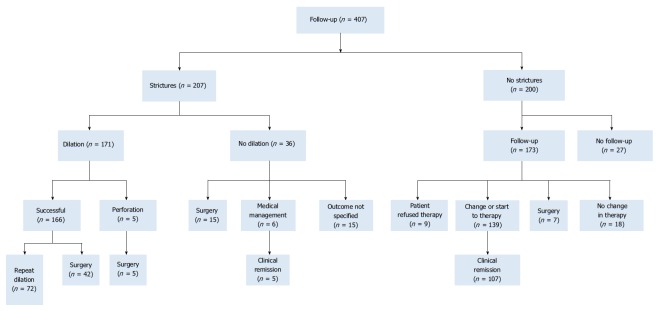
Of the 638 studies identified, 73 studies reporting on 1812 CD patients undergoing 2340 BAE procedures (DBE: n = 2027, SBE: n = 187, BAE not-specified: n = 126) were included in the final analysis[28,33-104] (Figure 1, Tables 1 and 2). The majority of studies involved international institutions (85%)[28,33,34,36-40,42-47,51-56,58,61-78,80-93,96,97,99-105], reporting retrospectively (74%)[34,35,37-43,47-51,53-57,59,60,62,63,65,67-69,71-73,75-85,87-91,93-96,99,101,102,104], on their experience with BAE. Of the 1812 patients included in the analysis, 597 (33%) were newly diagnosed with CD and 1215 (67%) had a known diagnosis of CD prior to undergoing BAE. Among the patients with known CD where the indication for the procedure was clearly documented, BAE was performed primarily for monitoring of disease activity (61%), known strictures (16%), or small bowel obstruction (4%). One thousand nine hundred and thirty-eight BAE (83%) were diagnostic and 402 BAE (17%) were therapeutic procedures.
Figure 1.
Studies identified and reasons for exclusion. VCE: Video capsule endoscopy; SE: Spiral enteroscopy; IBD: Inflammatory bowel disease; BAE: Balloon-assisted enteroscopy; CD: Crohn’s disease.
Table 1.
Study demographics n (%)
| BAE studies, n = 73 | DBE, n = 60 | SBE, n = 11 | |
| Patients, n = 1812 | n = 1509 | n = 187 | |
| Published manuscripts | 47 (64) | 39 (65) | 8 (72) |
| United States center | 11 (15) | 9 (15) | 0 (0) |
| Prospective | 19 (26) | 14 (23) | 6 (55) |
| Published pre-2010 | 18 (25) | 17 (28) | 1 (10) |
| Crohn’s patients per study | |||
| 5-10 | 26 (36) | 23 (38) | 3 (27) |
| 11-25 | 25 (34) | 20 (33) | 5 (45) |
| > 25 | 22 (30) | 17 (28) | 3 (27) |
| Age, mean ± SD | 42.9 ± 15.4 | 42.4 ± 15.5 | 45.0 ± 15.8 |
Three studies and 116 patients were solely reported as “balloon assisted enteroscopy”; 1 study included both DBE and SBE. DBE: Double balloon enteroscopy; SBE: Single balloon enteroscopy; BAE: Balloon assisted enteroscopy.
Table 2.
Studies involved international institutions on their experience with balloon assisted enteroscopy
| Study | Published manuscript | 2010-present | United States | Prospective | Mean age | Patients | Procedures | Therapeutic | Perforations |
| Akarsu et al[90] | X | X | 47.8 | 39 | 39 | 0 | 0 | ||
| Aktas et al[95] | X | X | 53 | 58 | 58 | 0 | 0 | ||
| Aktas et al[92] | X | X | X | 51 | 31 | 31 | 2 | 0 | |
| Arihiro et al[96] | X | 56.3 | 32 | 32 | 9 | 1 | |||
| Bartel et al[41] | X | X | 52.6 | 38 | 38 | 0 | 0 | ||
| Bartel et al[49] | X | X | 54.3 | 7 | 7 | 7 | 1 | ||
| Bartel et al[50] | X | X | 62.7 | 15 | 15 | 0 | 0 | ||
| Chen et al[84] | X | X | 51 | 8 | 8 | 0 | 0 | ||
| Choi et al[82] | X | X | 43.5 | 7 | 7 | 0 | 0 | ||
| de Ridder et al[97] | X | X | X | 15 | 14 | 14 | 0 | 0 | |
| Despott et al[33] | X | X | 46.4 | 11 | 13 | 13 | 1 | ||
| Di Caro et al[51] | X | 52 | 7 | 7 | 0 | 0 | |||
| Di Nardo et al[98] | X | X | X | 13 | 26 | 26 | 5 | 0 | |
| Ding et al[85] | X | 39 | 12 | 22 | 22 | 1 | |||
| Domagk et al[52] | X | X | X | 52 | 11 | 11 | 0 | 0 | |
| Dutta et al[99] | X | X | 42 | 14 | 14 | 0 | 0 | ||
| Fan et al[28] | X | X | X | Not reported | 77 | 308 | 0 | 0 | |
| Gill et al[34] | X | X | 52.7 | 20 | 20 | 10 | 2 | ||
| Halloran et al[35] | X | X | 44.8 | 21 | 40 | 40 | 1 | ||
| Hirai et al[91] | X | X | 36 | 65 | 110 | 110 | 1 | ||
| Huang et al[53] | X | 10 | 7 | 7 | 0 | 0 | |||
| Jang et al[42] | X | X | 32.7 | 24 | 32 | 0 | 0 | ||
| Jeon et al[54] | X | 36.4 | 30 | 39 | 0 | 0 | |||
| Lakatos et al[55] | X | 51.6 | 6 | 6 | 0 | 0 | |||
| Li et al[43] | X | 49 | 13 | 13 | 0 | 0 | |||
| Liu et al[56] | X | 8.5 | 5 | 5 | 0 | 0 | |||
| Lurix et al[57] | X | X | 59 | 5 | 5 | 0 | 0 | ||
| Maaser et al[58] | X | X | X | 54.9 | 59 | 59 | 0 | 0 | |
| Mann et al[59] | X | X | 59 | 9 | 9 | 0 | 0 | ||
| Mann et al[60] | X | X | 59 | 23 | 23 | 0 | 0 | ||
| Manner et al[61] | X | 56 | 20 | 20 | 0 | 0 | |||
| Manno et al[100] | X | X | X | 61 | 11 | 11 | 1 | 0 | |
| May et al[44] | X | X | X | 53 | 9 | 9 | 0 | 0 | |
| Mensink et al[36] | X | X | X | 53 | 50 | 50 | 0 | 0 | |
| Milewski et al[62] | X | X | 45 | 75 | 75 | 12 | 0 | ||
| Moreels et al[63] | X | Not reported | 6 | 6 | 0 | 0 | |||
| Morise et al[89] | 13 | 76 | 76 | 0 | 0 | ||||
| Morishima et al[37] | X | X | 36 | 17 | 35 | 35 | 0 | ||
| Moschler et al[64] | 35.4 | 193 | 193 | 0 | 0 | ||||
| Nakano et al[47] | X | X | X | 64 | 36 | 36 | 36 | 0 | |
| Navaneethan et al[94] | X | X | 56.8 | 49 | 59 | 9 | 1 | ||
| Ohmiya et al[38] | X | X | X | 41 | 23 | 23 | 23 | 0 | |
| Parker et al[65] | X | 48 | 11 | 11 | 0 | 0 | |||
| Pata et al[66] | X | Not reported | 16 | 16 | 4 | 0 | |||
| Peng et al[67] | X | X | X | 53 | 15 | 15 | 0 | 0 | |
| Pohl et al[39] | X | Language1 | 19 | 21 | 21 | 0 | |||
| Qing et al[68] | X | 36 | 7 | 7 | 0 | 0 | |||
| Rahman et al[48] | X | Not reported | 55 | 55 | 3 | 1 | |||
| Roushan et al[83] | X | X | X | Not reported | 7 | 7 | 0 | 0 | |
| Russo et al[101] | X | X | 47.2 | 6 | 6 | 0 | 0 | ||
| Safatle et al[93] | X | 57 | 9 | 9 | 0 | 0 | |||
| Schulz et al[69] | X | 48.6 | 11 | 11 | 0 | 0 | |||
| Seiderer et al[70] | X | X | 50.8 | 10 | 10 | 0 | 0 | ||
| Shen et al[71] | X | X | 33.9 | 8 | 8 | 0 | 0 | ||
| Shi et al[72] | X | X | 13 | 35 | 35 | 0 | 0 | ||
| Sidhu et al[73] | X | X | 61.2 | 39 | 39 | 0 | 0 | ||
| Sun et al[74] | X | 52 | 7 | 7 | 0 | 0 | |||
| Takenaka et al[45] | X | X | 52 | 10 | 10 | 0 | 0 | ||
| Tsujikawa et al[102] | X | X | X | 31 | 17 | 17 | 7 | 0 | |
| Uchida et al[75] | X | 48.9 | 6 | 9 | 1 | 0 | |||
| Urs et al[76] | X | X | 12.9 | 5 | 5 | 0 | 0 | ||
| Urs et al[77] | X | 12.7 | 7 | 13 | 0 | 0 | |||
| Watanabe et al[88] | X | X | 10.5 | 10 | 20 | 0 | 0 | ||
| Watanabe et al[78] | X | Not reported | 59 | 60 | 0 | 0 | |||
| Westerhoff[79] | X | Not reported | 18 | 18 | 0 | 0 | |||
| Wiarda et al[46] | X | Not reported | 18 | 18 | 0 | 0 | |||
| Xu et al[87] | X | X | X | 36 | 21 | 21 | 0 | 0 | |
| Yamada et al[40] | X | X | Not reported | 46 | 128 | 27 | 0 | ||
| Yoshida et al[103] | X | 37 | 10 | 10 | 5 | 0 | |||
| Yu et al[86] | X | X | Not reported | 36 | 108 | 0 | 0 | ||
| Zhang et al[80] | X | X | X | 31.6 | 5 | 5 | 0 | 0 | |
| Zhi et al[81] | X | X | Language1 | 7 | 7 | 0 | 0 | ||
| Zhu et al[104] | X | 36.3 | 23 | 23 | 0 | 0 |
Language: Unable to translate full manuscript, data was extracted from abstract which did not disclose age.
The 3 prospective randomized controlled trials identified in our search reported on a total of 37 CD patients[44,52,61]. Two of these studies compared DBE to SBE and found DBE to have comparable[52] or superior efficacy and diagnostic yield[44], while the other suggested that fluoroscopy increases insertion depth[61]. The largest prospective cohort study included 193 patients from 62 endoscopic centers in Germany over a 2-year span and had no perforations in CD patients[64].
Safety of BAE
The rate of perforation with diagnostic BAE in CD (1.5 per 1000 procedures) was similar to that reported when utilizing diagnostic BAE for all indications (1.1 per 1000 procedures, IRR = 1.41, 95%CI: 0.28-4.50). The rate of perforation with diagnostic DBE in CD (1.2 per 1000 procedures) was similar to that reported when utilizing diagnostic DBE for all indications (2.2 per 1000 procedures, IRR = 0.54, 95%CI: 0.06-2.24). The rate of perforation with therapeutic BAE in CD was 1.74% (Tables 3 and 4).
Table 3.
Diagnostic and therapeutic procedures n (%)
| Procedures, n = 2340 | Perforations, n = 10 | Rate (%) | |
| Diagnostic BAE | 1938 (83) | 3 (30) | 0.15 |
| Therapeutic BAE | 402 (17) | 7 (70) | 1.70 |
| Diagnostic DBE | 1666 (71) | 2 (20) | 0.12 |
BAE: Balloon assisted enteroscopy; DBE: Double balloon enteroscopy.
Table 4.
Balloon assisted enteroscopy cases with procedure related perforation
| Study | Demographics | Site and characteristics of perforation | Therapy | Procedure | Outcome after perforation |
| Despott et al[33] | Long standing CD (> 30 yr) with 5 prior SB resections currently on azathioprine and steroids | 3 jejunal strictures (2 inflammatory, 1 fibrotic) with severe ulcerations at stricture sites | Dilated to maximum of 16.5 mm | DBE - Technically difficult due to adhesion-related angulations and fixation, and strictures were significantly ulcerated | Perforation diagnosed within 8 h, patient had laparotomy and temporary jejunostomy. Patient made full recovery and jejunostomy was reversed. |
| Gill et al[34] | Retained video capsule in patient with known CD | Non-obstructing jejunal stricture with mild inflammation and ulceration at the stricture site | Dilated to 15 mm | DBE - otherwise not specified | Underwent surgery, outcome otherwise not specified. |
| Gill et al[34] | Known CD patient had previously responded well to dilation up to 15 mm | Distal obstructing ileal stricture with mild inflammation and ulceration at the stricture site | Dilated to 15 mm | DBE - otherwise not specified | Underwent surgery, outcome otherwise not specified. |
| Halloran et al[35] | Known CD patient who had undergone prior surgical resection. | Scarred bowel loop adhesion site | Not specified | DBE - Perforation occurred with overtube advancement and straightening of a scarred bowel loop | Outcome not specified. |
| Ding et al[85] | Known CD patient | SB stricture, otherwise not specified | Dilation related perforation, otherwise not specified | DBE - Dilation related perforation, otherwise not specified | Perforation diagnosed within 12 h, patient had laparotomy and resection with ileostomy. |
| Bartel et al[49] | Retained video capsule in patient with known CD | SB stricture, otherwise not specified | Not specified | DBE - Otherwise not specified | Emergent surgical intervention, otherwise outcome not specified. |
| Rahman et al[48] | Known CD patient | Ulcer at anastomosis site | Not specified | DBE - Perforation directly related to ulcer at anastomosis | Patient made full recovery after surgical resection and primary reanastomosis. |
| Navaneethan et al[94] | Known CD patient | Not specified | Not specified | Not specified | Underwent surgery, outcome otherwise not specified |
| Arihiro et al[96] | Known CD patient | SB stricture, otherwise not specified | Dilation related perforation, otherwise not specified | SBE - Dilation related perforation, otherwise not specified | Patient improved over time without any surgical intervention. |
| Hirai et al[91] | Known CD patient | SB stricture, otherwise not specified | Dilation related perforation, otherwise not specified | DBE - Dilation related perforation, otherwise not specified | Patient had emergency partial ileal resection and made a full recovery. |
CD: Crohn’s disease; SB: Small bowel; DBE: Double balloon enteroscopy; SBE: Single balloon enteroscopy.
Among 1812 patients who underwent a total of 2340 procedures, there were 8 reported perforations with DBE (per procedure 0.39%, 95%CI: 0.12-0.66, per patient 0.53%, 95%CI: 0.16-0.90)[33-35,48,49,85,91,94,96], 1 reported perforation with SBE (per procedure and per patient 0.53%, 95%CI: 0.0-1.57)[96], and 1 perforation with BAE not otherwise specified. Of the 8 DBE perforations, 5 were during dilation of de novo CD strictures and the other 3 were during diagnostic evaluations of an adhesion site, an anastomosis stricture, and a site that was not specified. The 1 SBE perforation was during dilation of a de novo CD stricture site. This equated to an overall per procedure and per patient perforation rate of 0.43% (95%CI: 0.16-0.67) and 0.55% (95%CI: 0.21-0.89), respectively, for BAE in CD including both diagnostic and therapeutic procedures[94]. There was minimal heterogeneity among studies (I2 = 0).
Follow-up and impact of BAE on medical and surgical management
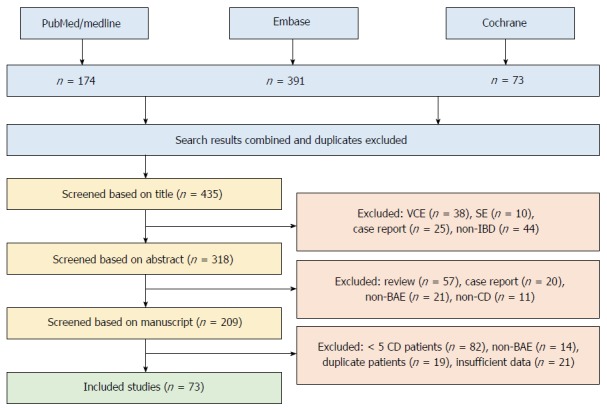
Follow-up after BAE was reported in 407 patients with a median follow-up period of 18 mo (range 10-70)[28,33-40,85,86,88,91] (Figure 2). Stricture dilation was performed in 171 patients, resulting in 5 perforations (all at de novo CD stricture sites) and 166 technically successful dilations. Dilation was not attempted in 36 patients due to: inability to insert scope up to stricture site (n = 8), inability to maintain guide wire or through-the-scope balloon at correct position of the stricture (n = 5), stricture length or severe angulation (n = 4), severe inflammation (n = 6), the presence of intra-abdominal adhesions that prohibited advancement of the DBE (n = 2), a perforation during overtube advancement at an anastomotic site (n = 1), and/or non-obstructing or severely ulcerated strictures (n = 10). During follow-up, of the 166 patients where stricture dilation was technically successful, 72 (43%) required repeat stricture dilation and 42 (25%) patients required surgery for persistent symptoms.
Figure 2.
Outcome and impact of balloon-assisted enteroscopy in patients with follow-up.
Of the remaining 200 patients, 173 had clearly reported outcomes regarding changes in medical therapy and treatment response[28,36,86,88,91]. Based on BAE findings, 139 (80%) patients either initiated therapy with an immunomodulator (azathioprine or methotrexate, n = 83), initiated therapy with an anti-tumor necrosis factor agent (n = 52), or they were switched from one anti-tumor necrosis factor agent to another (n = 4). Seven (4%) patients required surgery, and the remaining either refused a step-up in medical therapy (n = 9, 5%) or they had no change in medical therapy needed (n = 18, 10%). Of the 139 patients where a change in medical therapy was performed, 92 (66%) achieved clinical remission at the first follow-up (as defined by the CD activity index)[28,36,86,88]. Repeat BAE was performed in 133 patients with a majority achieving endoscopic improvement in disease activity or complete healing of mucosal lesions (62%)[28,36,86,88]. A third follow-up BAE was performed in 113 patients, and rates of complete or nearly-complete mucosal healing improved from 29% (n = 33) to 43% (n = 57) with changes in therapy based on BAE results[86].
DISCUSSION
In our systematic review of 1812 CD patients undergoing 2340 BAE, the rate of perforation with diagnostic BAE in CD was similar to that seen when utilizing diagnostic BAE for other indications. The rate of perforation with diagnostic DBE in CD was also similar to that seen when utilizing diagnostic DBE for other indications. Additionally, findings from diagnostic BAE in conjunction with changes in medical therapy resulted in improved clinical and endoscopic disease activity in a majority of patients. Diagnostic BAE demonstrated a meaningful change in clinical care with a similar safety profile in CD compared to other indications.
Therapeutic BAE also exhibited significant clinical utility as approximately 70% of patients in our study avoided surgery after stricture dilation, albeit with higher rates of perforation. This increased risk of perforation with stricture dilation in CD[106] must be weighed against the therapeutic benefits achieved. Efforts need to focus on risk stratification of small bowel strictures to determine which patients may be more suitable for small bowel resection as compared to endoscopic dilation. Prior studies have demonstrated that both length and location are useful prognostic factors, and short strictures located in the large bowel or at the site of prior anastomosis are likely to be most amendable to endoscopic dilation as compared to complex or lengthy de-novo strictures[107-109]. Within our study at least three of the six perforations during stricture dilation were at ulcerated sites, and at least two of the perforations were in patients with previous stricture dilations. As the alternative to symptomatic strictures is surgical resection or strictureplasty, our results suggest that stricture dilation via BAE can be done in accessible, short-length symptomatic strictures, and it has better performance in anastomotic strictures, but it may need to be avoided in presence of significant CD-related inflammation.
The relative excess risk of endoscopy associated perforations among IBD patients as compared to non-IBD patients has previously been demonstrated, with disease severity and steroid use (a surrogate for disease activity) being two of the strongest predictors for a procedure related perforation[30,110-112]. Within our systematic review, the total rate of perforation with BAE in CD (4.27 per 1000 procedures) when including both diagnostic and therapeutic procedures was nearly 4 times that reported with diagnostic BAE for all indications (1.1 per 1000 procedures), and the significant majority of this risk was seen in therapeutic procedures.
Our results demonstrate that diagnostic BAE is a safe tool in monitoring small bowel disease activity and may have a role in guiding medical treatment to achieve clinical remission and mucosal healing. The rate of perforation with diagnostic BAE in CD (1.55 per 1000) was also similar to that reported with lower endoscopy in IBD patients (1.89 per 1000)[112]. Other modalities have been demonstrated to have a reasonable diagnostic accuracy for assessing small bowel disease activity in CD[22,113-124], but they have several technical and practical limitations that prevent their routine use in clinical practice[48,113,114,121,125-127]. In our pooled analysis, findings from BAE in conjunction with changes in medical therapy resulted in improved clinical and endoscopic disease activity in a substantial majority of patients. Although further prospective studies are needed to understand the positioning of BAE in disease activity assessment and treating to a target of mucosal healing in CD, these data suggest that BAE may be a useful tool for assessing small bowel disease activity and treatment response in CD.
Our study has highlighted several key findings but it also has several limitations. There is an inherent selection bias in patients who undergo BAE that undoubtedly affects our results. The majority of analyzed studies were retrospective with variable objectives, different inclusion criteria, and limited follow-up data. Additionally, the lack of prospective studies comparing BAE to cross-sectional imaging in evaluation of small bowel disease makes evaluating the utility of diagnostic BAE difficult. Lastly, BAE has a high rate of incomplete enteroscopy[64], which likely was not portrayed in our results, as completion rates were not consistently documented. Strengths of our study included the extensive search performed and the large number of patients and procedures analyzed.
Diagnostic BAE in CD has a similar perforation rate as diagnostic BAE in other indications and may help safely guide medical therapy via assessment of mucosal healing. Therapeutic BAE may help avoid surgery in patients with symptomatic strictures, but the rate of perforation with therapeutic procedures is higher and thus providers must exercise caution when utilizing this endoscopic technique. Further efforts should focus on risk stratification of patients to ensure optimal safety and diagnostic yield and further studies are needed to identify patient and stricture characteristics at highest risk for procedure related complications.
COMMENTS
Background
Crohn’s disease (CD) often affects the small bowel, but conventional upper and lower endoscopy are limited in their evaluation of small bowel disease activity or ability to perform interventions. Balloon assisted enteroscopy (BAE) allows for direct visualization and sampling of the small bowel, however its safety and role in CD remain to be established.
Research frontiers
This systematic review reveals that diagnostic BAE in CD has similar perforation rates as diagnostic BAE for all indications, suggesting that BAE is a safe way to evaluate small bowel CD. Further randomized controlled trials are warranted to confirm these findings as well as to identify anatomical characteristics that are at highest risk for procedure related complications.
Innovations and breakthroughs
The research demonstrates that BAE has a similar perforation rate in diagnostic evaluation of small bowel CD vs other indications. This systematic review is the most up-to-date overview of this subject matter.
Applications
Diagnostic BAE in CD has a similar perforation rate as in other indications, thus it can be safely performed in diagnostic evaluation of small bowel CD.
Peer-review
The present manuscript is well written. The efficacy, safety and long-term prognosis of balloon dilation using BAE should be separately shown between patients with small bowel strictures and patients with anastomotic strictures. This should be analyzed in the manuscript.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: All authors have no relevant conflicts of interest.
Data sharing statement: There are no additional data.
Peer-review started: May 18, 2016
First decision: June 20, 2016
Article in press: August 1, 2016
P- Reviewer: Kobayashi Y, Lakatos PL, Ogata H, Pinho R S- Editor: Ma YJ L- Editor: A E- Editor: Zhang FF
References
- 1.Loftus EV. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–1517. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 2.Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn’s disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777–782. doi: 10.1136/gut.49.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, Gendre JP. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8:244–250. doi: 10.1097/00054725-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Khanna R, Levesque BG, Bressler B, Zou G, Stitt L, Greenberg GR, Panaccione R, Bitton A, Pare P, Vermeire S, et al. 1053 Early Combined Immunosuppression for the Management of Crohn’s Disease: A Community-Based Cluster Randomized Trial. Gastroenterology. 2014;146:S–187. doi: 10.1016/S0016-5085(14)60664-8. [DOI] [Google Scholar]
- 5.Froslie KF, Jahnsen J, Moum BA, Vatn MH, Group I. Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology. 2007;133:412–422. doi: 10.1053/j.gastro.2007.05.051. [DOI] [PubMed] [Google Scholar]
- 6.Schnitzler F, Fidder H, Ferrante M, Noman M, Arijs I, Van Assche G, Hoffman I, Van Steen K, Vermeire S, Rutgeerts P. Mucosal healing predicts long-term outcome of maintenance therapy with infliximab in Crohn’s disease. Inflamm Bowel Dis. 2009;15:1295–1301. doi: 10.1002/ibd.20927. [DOI] [PubMed] [Google Scholar]
- 7.Rutgeerts P, Diamond RH, Bala M, Olson A, Lichtenstein GR, Bao W, Patel K, Wolf DC, Safdi M, Colombel JF, et al. Scheduled maintenance treatment with infliximab is superior to episodic treatment for the healing of mucosal ulceration associated with Crohn’s disease. Gastrointest Endosc. 2006;63:433–432; quiz 464. doi: 10.1016/j.gie.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 8.Baert F, Moortgat L, Van Assche G, Caenepeel P, Vergauwe P, De Vos M, Stokkers P, Hommes D, Rutgeerts P, Vermeire S, et al. Mucosal healing predicts sustained clinical remission in patients with early-stage Crohn’s disease. Gastroenterology. 2010;138:463–468; quiz e10-11. doi: 10.1053/j.gastro.2009.09.056. [DOI] [PubMed] [Google Scholar]
- 9.Bouguen G, Levesque BG, Pola S, Evans E, Sandborn WJ. Endoscopic assessment and treating to target increase the likelihood of mucosal healing in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2014;12:978–985. doi: 10.1016/j.cgh.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Bouguen G, Levesque BG, Feagan BG, Kavanaugh A, Peyrin-Biroulet L, Colombel JF, Hanauer SB, Sandborn WJ. Treat to target: a proposed new paradigm for the management of Crohn’s disease. Clin Gastroenterol Hepatol. 2015;13:1042–1050.e2. doi: 10.1016/j.cgh.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Steinhardt HJ, Loeschke K, Kasper H, Holtermüller KH, Schäfer H. European Cooperative Crohn’s Disease Study (ECCDS): clinical features and natural history. Digestion. 1985;31:97–108. doi: 10.1159/000199186. [DOI] [PubMed] [Google Scholar]
- 12.Mekhjian HS, Switz DM, Melnyk CS, Rankin GB, Brooks RK. Clinical features and natural history of Crohn’s disease. Gastroenterology. 1979;77:898–906. [PubMed] [Google Scholar]
- 13.Voderholzer WA, Beinhoelzl J, Rogalla P, Murrer S, Schachschal G, Lochs H, Ortner MA. Small bowel involvement in Crohn’s disease: a prospective comparison of wireless capsule endoscopy and computed tomography enteroclysis. Gut. 2005;54:369–373. doi: 10.1136/gut.2004.040055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Travis SP, Stange EF, Lémann M, Oresland T, Chowers Y, Forbes A, D’Haens G, Kitis G, Cortot A, Prantera C, et al. European evidence based consensus on the diagnosis and management of Crohn’s disease: current management. Gut. 2006;55 Suppl 1:i16–i35. doi: 10.1136/gut.2005.081950b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sandborn WJ, Feagan BG, Hanauer SB, Lochs H, Löfberg R, Modigliani R, Present DH, Rutgeerts P, Schölmerich J, Stange EF, et al. A review of activity indices and efficacy endpoints for clinical trials of medical therapy in adults with Crohn’s disease. Gastroenterology. 2002;122:512–530. doi: 10.1053/gast.2002.31072. [DOI] [PubMed] [Google Scholar]
- 16.Ajlouni Y, Iser JH, Gibson PR. Endoscopic balloon dilatation of intestinal strictures in Crohn’s disease: safe alternative to surgery. J Gastroenterol Hepatol. 2007;22:486–490. doi: 10.1111/j.1440-1746.2006.04764.x. [DOI] [PubMed] [Google Scholar]
- 17.Hassan C, Zullo A, De Francesco V, Ierardi E, Giustini M, Pitidis A, Taggi F, Winn S, Morini S. Systematic review: Endoscopic dilatation in Crohn’s disease. Aliment Pharmacol Ther. 2007;26:1457–1464. doi: 10.1111/j.1365-2036.2007.03532.x. [DOI] [PubMed] [Google Scholar]
- 18.Hommes DW, van Deventer SJ. Endoscopy in inflammatory bowel diseases. Gastroenterology. 2004;126:1561–1573. doi: 10.1053/j.gastro.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 19.Kopylov U, Yablecovitch D, Lahat A, Neuman S, Levhar N, Greener T, Klang E, Rozendorn N, Amitai MM, Ben-Horin S, et al. Detection of Small Bowel Mucosal Healing and Deep Remission in Patients With Known Small Bowel Crohn’s Disease Using Biomarkers, Capsule Endoscopy, and Imaging. Am J Gastroenterol. 2015;110:1316–1323. doi: 10.1038/ajg.2015.221. [DOI] [PubMed] [Google Scholar]
- 20.Dulai PS, Levesque BG, Feagan BG, D’Haens G, Sandborn WJ. Assessment of mucosal healing in inflammatory bowel disease: review. Gastrointest Endosc. 2015;82:246–255. doi: 10.1016/j.gie.2015.03.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Triester SL, Leighton JA, Leontiadis GI, Gurudu SR, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn’s disease. Am J Gastroenterol. 2006;101:954–964. doi: 10.1111/j.1572-0241.2006.00506.x. [DOI] [PubMed] [Google Scholar]
- 22.Dionisio PM, Gurudu SR, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohn’s disease: a meta-analysis. Am J Gastroenterol. 2010;105:1240–1248; quiz 1249. doi: 10.1038/ajg.2009.713. [DOI] [PubMed] [Google Scholar]
- 23.Tae CH, Shim KN. Should capsule endoscopy be the first test for every obscure gastrointestinal bleeding? Clin Endosc. 2014;47:409–414. doi: 10.5946/ce.2014.47.5.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheifetz AS, Kornbluth AA, Legnani P, Schmelkin I, Brown A, Lichtiger S, Lewis BS. The risk of retention of the capsule endoscope in patients with known or suspected Crohn’s disease. Am J Gastroenterol. 2006;101:2218–2222. doi: 10.1111/j.1572-0241.2006.00761.x. [DOI] [PubMed] [Google Scholar]
- 25.Mönkemüller K, Weigt J, Treiber G, Kolfenbach S, Kahl S, Röcken C, Ebert M, Fry LC, Malfertheiner P. Diagnostic and therapeutic impact of double-balloon enteroscopy. Endoscopy. 2006;38:67–72. doi: 10.1055/s-2005-921190. [DOI] [PubMed] [Google Scholar]
- 26.Fry LC, Bellutti M, Neumann H, Malfertheiner P, Monkemuller K. Utility of double-balloon enteroscopy for the evaluation of malabsorption. Dig Dis. 2008;26:134–139. doi: 10.1159/000116771. [DOI] [PubMed] [Google Scholar]
- 27.Jovanovic I, Vormbrock K, Zimmermann L, Djuranovic S, Ugljesic M, Malfertheiner P, Fry LC, Mönkemüller K. Therapeutic double-balloon enteroscopy: a binational, three-center experience. Dig Dis. 2011;29 Suppl 1:27–31. doi: 10.1159/000331125. [DOI] [PubMed] [Google Scholar]
- 28.Fan R, Zhong J, Wang ZT, Li SY, Zhou J, Tang YH. Evaluation of “top-down” treatment of early Crohn’s disease by double balloon enteroscopy. World J Gastroenterol. 2014;20:14479–14487. doi: 10.3748/wjg.v20.i39.14479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murphy SJ, Kornbluth A. Double balloon enteroscopy in Crohn’s disease: where are we now and where should we go? Inflamm Bowel Dis. 2011;17:485–490. doi: 10.1002/ibd.21373. [DOI] [PubMed] [Google Scholar]
- 30.Odagiri H, Matsui H, Fushimi K, Kaise M, Yasunaga H. Factors associated with perforation related to diagnostic balloon-assisted enteroscopy: analysis of a national inpatient database in Japan. Endoscopy. 2015;47:143–146. doi: 10.1055/s-0034-1390891. [DOI] [PubMed] [Google Scholar]
- 31.Xin L, Liao Z, Jiang YP, Li ZS. Indications, detectability, positive findings, total enteroscopy, and complications of diagnostic double-balloon endoscopy: a systematic review of data over the first decade of use. Gastrointest Endosc. 2011;74:563–570. doi: 10.1016/j.gie.2011.03.1239. [DOI] [PubMed] [Google Scholar]
- 32.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 33.Despott EJ, Gupta A, Burling D, Tripoli E, Konieczko K, Hart A, Fraser C. Effective dilation of small-bowel strictures by double-balloon enteroscopy in patients with symptomatic Crohn’s disease (with video) Gastrointest Endosc. 2009;70:1030–1036. doi: 10.1016/j.gie.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Gill RS, Kaffes AJ. Small bowel stricture characterization and outcomes of dilatation by double-balloon enteroscopy: a single-centre experience. Therap Adv Gastroenterol. 2014;7:108–114. doi: 10.1177/1756283X13513995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Halloran BP, Melmed GY, Jamil LH, Lo SK, Vasiliauskas EA, Mann NK. Double balloon enteroscopy-assisted stricture dilation delays surgery in patients with small bowel crohn’s disease. Gastrointest Endosc. 2013;(1):AB280. [Google Scholar]
- 36.Mensink PB, Aktas H, Zelinkova Z, West RL, Kuipers EJ, van der Woude CJ. Impact of double-balloon enteroscopy findings on the management of Crohn’s disease. Scand J Gastroenterol. 2010;45:483–489. doi: 10.3109/00365520903563774. [DOI] [PubMed] [Google Scholar]
- 37.Morishima K, Ohmiya N, Nakamura M, Shirai O, Takenaka H, Miyahara R, Watanabe O, Ando T, Kawashima H, Itoh A, et al. The evaluation of the postoperative Crohn’s jejunoileitis and balloon dilation for the strictures by using double balloon enteroscopy (DBE) Gastrointest Endosc. 2009;69:AB198. doi: 10.1016/j.gie.2009.03.433. [DOI] [Google Scholar]
- 38.Ohmiya N, Arakawa D, Nakamura M, Honda W, Shirai O, Taguchi A, Itoh A, Hirooka Y, Niwa Y, Maeda O, et al. Small-bowel obstruction: diagnostic comparison between double-balloon endoscopy and fluoroscopic enteroclysis, and the outcome of enteroscopic treatment. Gastrointest Endosc. 2009;69:84–93. doi: 10.1016/j.gie.2008.04.067. [DOI] [PubMed] [Google Scholar]
- 39.Pohl J, May A, Nachbar L, Ell C. Diagnostic and therapeutic yield of push-and-pull enteroscopy for symptomatic small bowel Crohn’s disease strictures. Eur J Gastroenterol Hepatol. 2007;19:529–534. doi: 10.1097/MEG.0b013e328012b0d0. [DOI] [PubMed] [Google Scholar]
- 40.Yamada K, Ohmiya N, Nagura A, Ishihara M, Ohara K, Ohno E, Kawashima H, Miyahara R, Itoh A, Hirooka Y, et al. Usefulness of endoscopic diagnosis of postoperative small-bowel lesions and balloon dilation for strictures in patients with crohn’s disease at double-balloon enteroscopy. Gastrointest Endosc. 2012;(1):AB251. doi: 10.1016/j.gie.2012.04.229. [DOI] [Google Scholar]
- 41.Bartel MJ, Kroner T, Stark ME, Lukens F. Yield of double balloon enteroscopy for chronic GI symptoms suggestive of crohn’s disease with negative colonoscopy. Gastroenterology. 2014;(1):S–40. doi: 10.1016/S0016-5085(14)60141-4. [DOI] [Google Scholar]
- 42.Jang HJ, Choi MH, Eun CS, Choi H, Choi KY, Park DI, Park JH, Chang DK, Kim JO, Ko BM, et al. Clinical usefulness of double balloon enteroscopy in suspected Crohn’s disease: the KASID multi-center trial. Hepatogastroenterology. 2014;61:1292–1296. [PubMed] [Google Scholar]
- 43.Li X, Chen H, Dai J, Gao Y, Ge Z. Predictive role of capsule endoscopy on the insertion route of double-balloon enteroscopy. Endoscopy. 2009;41:762–766. doi: 10.1055/s-0029-1215009. [DOI] [PubMed] [Google Scholar]
- 44.May A, Färber M, Aschmoneit I, Pohl J, Manner H, Lotterer E, Möschler O, Kunz J, Gossner L, Mönkemüller K, et al. Prospective multicenter trial comparing push-and-pull enteroscopy with the single- and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol. 2010;105:575–581. doi: 10.1038/ajg.2009.712. [DOI] [PubMed] [Google Scholar]
- 45.Takenaka K, Ohtsuka K, Kitazume Y, Nagahori M, Fujii T, Saito E, Watanabe M. Comparing MR enterocolonography to enteroscopy in Crohn’s disease, especially focusing on small intestinal findings [Internet] J Crohns Colitis. 2014;8:S170–S171. [Google Scholar]
- 46.Wiarda BM, Mensink PBF, Heine DGN, Stolk M, Dees J, Hazenberg H, Stoker J, Van Der Woude CJ, Kuipers EJ. Small bowel Crohn’s disease: MR enteroclysis and capsule endoscopy compared to balloon-assisted enteroscopy. Abdom Imaging. 2012;37:397–403. doi: 10.1007/s00261-011-9816-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nakano M, Oka S, Tanaka S, Aoyama T, Watari I, Hayashi R, Miyaki R, Nagai K, Sanomura Y, Yoshida S, et al. Clinical usefulness of classification by transabdominal ultrasonography for detection of small-bowel stricture. Scand J Gastroenterol. 2013;48:1041–1047. doi: 10.3109/00365521.2013.822546. [DOI] [PubMed] [Google Scholar]
- 48.Rahman A, Ross A, Leighton JA, Schembre D, Gerson L, Lo SK, Waxman I, Dye C, Semrad C. Double-balloon enteroscopy in Crohn’s disease: findings and impact on management in a multicenter retrospective study. Gastrointest Endosc. 2015;82:102–107. doi: 10.1016/j.gie.2014.12.039. [DOI] [PubMed] [Google Scholar]
- 49.Bartel MJ, Stauffer J, Kroner T, Stark ME, Lukens F. Lodged foreign bodies in the small bowel-proceed to surgery or perform double balloon enteroscopy first? Gastroenterology. 2014;(1):S–1051. doi: 10.1016/S0016-5085(14)63830-0. [DOI] [Google Scholar]
- 50.Bartel MJ, KroNer T, Stark ME, Lukens F. What is the significance of small bowel strictures diagnosed by double balloon enteroscopy? analysis of a large prospectively collected database. Gastrointest Endosc. 2014;(1):AB149–AB150. doi: 10.1016/j.gie.2014.02.124. [DOI] [Google Scholar]
- 51.Di Caro S, May A, Heine DGN, Fini L, Landi B, Petruzziello L, Cellier C, Mulder CJ, Costamagna G, Ell C, et al. The European experience with double-balloon enteroscopy: Indications, methodology, safety, and clinical impact. Gastrointest Endosc. 2005;62:545–550. doi: 10.1016/j.gie.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 52.Domagk D, Mensink P, Aktas H, Lenz P, Meister T, Luegering A, Ullerich H, Aabakken L, Heinecke A, Domschke W, et al. Single- vs. double-balloon enteroscopy in small-bowel diagnostics: a randomized multicenter trial. Endoscopy. 2011;43:472–476. doi: 10.1055/s-0030-1256247. [DOI] [PubMed] [Google Scholar]
- 53.Huang Y, Shao CH, Leung YK. [Application of double balloon enteroscopy in pediatric patients] Zhonghua Erke Zazhi. 2010;48:599–602. [PubMed] [Google Scholar]
- 54.Jeon SR, Kim JO, Kim HG, Lee TH, Kim WJ, Ko BM, Cho JY, Lee JS, Lee MS. Double-balloon enteroscopy in Crohn’s disease with small bowel involvement: The characteristics and clinical significance [Internet] J Crohns Colitis. 2013;7:S112–S113. [Google Scholar]
- 55.Lakatos PL, Fuszek P, Horvath HC, Zubek L, Haller P, Papp J. Double-balloon enteroscopy for the diagnosis and treatment of obscure bleeding, inflammatory bowel diseases and polyposis syndromes: we see more but do we know more? Hepatogastroenterology. 2008;55:133–137. [PubMed] [Google Scholar]
- 56.Liu W, Xu C, Zhong J. The diagnostic value of double-balloon enteroscopy in children with small bowel disease: report of 31 cases. Can J Gastroenterol. 2009;23:635–638. doi: 10.1155/2009/281040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lurix EG, Charles RJ, Ukleja A. A tertiary care center experience with double-balloon enteroscopy. Gastrointest Endosc. 2011;(1):AB464. doi: 10.1016/j.gie.2011.03.1110. [DOI] [Google Scholar]
- 58.Maaser C, Schmedt A, Bokemeyer M, Kannengiesser K, Ullerich H, Lugering A, Domagk D, Domschke W, Kucharzik T. Long-term efficacy and safety of double balloon enteroscopy prospective and retrospective data from a single center study. Scand J Gastroenterol. 2010;45:992–999. doi: 10.3109/00365521003710182. [DOI] [PubMed] [Google Scholar]
- 59.Mann NK, Jamil LH, Lo SK. High completion rates in double balloon enteroscopy (DBE) are possible in a north american patient population. Gastrointest Endosc. 2012;(1):AB264–AB265. doi: 10.1016/j.gie.2012.04.273. [DOI] [Google Scholar]
- 60.Mann NK, Jamil LH, Lo SK. Total enteroscopy should be used to validate capsule endoscopy and other imaging technologies of the small intestine. Gastroenterology. 2014;(1):S–39. doi: 10.1016/S0016-5085(14)60137-2. [DOI] [Google Scholar]
- 61.Manner H, May A, Pohl J, Farber M, Ell C. Impact of fluoroscopy on oral double-balloon enteroscopy: Results of a randomized trial in 156 patients. Endoscopy. 2010;42:820–826. doi: 10.1055/s-0030-1255727. [DOI] [PubMed] [Google Scholar]
- 62.Milewski J, Zuk K, Nasierowska-Guttmejer A, Rydzewska G. Double balloon enteroscopy (DBE) in suspected small-bowel crohn’s disease-one center experience. Gastrointest Endosc. 2013;(1):AB279–AB280. doi: 10.1016/j.gie.2013.03.699. [DOI] [Google Scholar]
- 63.Moreels TG, Mensink P, Kuipers EJ, Escher JC, Pelckmans PA. Small bowel evaluation by double-balloon enteroscopy in pediatric patients: Results of two university hospital endoscopy units. Gastrointest Endosc. 2009;69:AB172. doi: 10.1016/j.gie.2009.03.328. [DOI] [Google Scholar]
- 64.Moschler O, May A, Muller MK, Ell C. Complications in and performance of double-balloon enteroscopy (DBE): Results from a large prospective DBE database in Germany. Endoscopy. 2011;43:484–489. doi: 10.1055/s-0030-1256249. [DOI] [PubMed] [Google Scholar]
- 65.Parker C, Perowne R, Nylander D, Panter S. Yield of double balloon enteroscopy in the investigation of possible or recurrent Crohn’s disease [Internet] J Crohns Colitis. 2013;7:S54. [Google Scholar]
- 66.Pata C, Akyuz U, Erzin Y, Mercan A. Double-balloon enteroscopy: The diagnosis and management of small bowel diseases. Turk J Gastroenterol. 2010;21:353–359. doi: 10.4318/tjg.2010.0120. [DOI] [PubMed] [Google Scholar]
- 67.Peng J, Leng AM, Wu RY, Yang HX, Yuan WJ, Zou YY, Zhang GY. [The diagnostic value of double-balloon enteroscopy in 67 cases with obscure abdominal pain] Zhonghua Neike Zazhi. 2009;48:111–113. [PubMed] [Google Scholar]
- 68.Qing C, An H. Clinical analysis of 93 case double-ballon enteroscopy in smal bowel diseases. J Gastroenterol Hepatol. 2013;28:723. doi: 10.1111/jgh.12363_3. [DOI] [Google Scholar]
- 69.Schulz C, Mönkemüller K, Salheiser M, Bellutti M, Schütte K, Malfertheiner P. Double-balloon enteroscopy in the diagnosis of suspected isolated Crohn’s disease of the small bowel. Dig Endosc. 2014;26:236–242. doi: 10.1111/den.12142. [DOI] [PubMed] [Google Scholar]
- 70.Seiderer J, Herrmann K, Diepolder H, Schoenberg SO, Wagner AC, Göke B, Ochsenkühn T, Schäfer C. Double-balloon enteroscopy versus magnetic resonance enteroclysis in diagnosing suspected small-bowel Crohn’s disease: results of a pilot study. Scand J Gastroenterol. 2007;42:1376–1385. doi: 10.1080/00365520701397867. [DOI] [PubMed] [Google Scholar]
- 71.Shen R, Sun B, Gong B, Zhang S, Cheng S. Double-balloon enteroscopy in the evaluation of small bowel disorders in pediatric patients. Dig Endosc. 2012;24:87–92. doi: 10.1111/j.1443-1661.2011.01175.x. [DOI] [PubMed] [Google Scholar]
- 72.Shi H, Ren J, Dong W. Double-balloon enteroscopy in the diagnosis and management of small-bowel diseases. Hepatogastroenterology. 2011;58:477–486. [PubMed] [Google Scholar]
- 73.Sidhu R, McAlindon ME, Hardcastle S, Sanders DS. Double balloon enteroscopy in the era of capsule endoscopy: Necessity or luxury? Gut. 2011;60:A253. doi: 10.1136/gut.2011.239301.537. [DOI] [Google Scholar]
- 74.Sun B, Shen R, Cheng S, Zhang C, Zhong J. The role of double-balloon enteroscopy in diagnosis and management of incomplete small-bowel obstruction. Endoscopy. 2007;39:511–515. doi: 10.1055/s-2007-966376. [DOI] [PubMed] [Google Scholar]
- 75.Uchida K, Yoshiyama S, Inoue M, Koike Y, Yasuda H, Fujikawa H, Okita Y, Araki T, Tanaka K, Kusunoki M. Double balloon enteroscopy for pediatric inflammatory bowel disease. Pediatr Int. 2012;54:806–809. doi: 10.1111/j.1442-200X.2012.03661.x. [DOI] [PubMed] [Google Scholar]
- 76.Urs AN, Rao PC, Arian Z, Thomson M. Double-balloon enteroscopy in children-a tertiary care experience. Arch Dis Child. 2011;96:A15–A16. doi: 10.1136/adc.2011.212563.30. [DOI] [Google Scholar]
- 77.Urs AN, Martinelli M, Rao P, Thomson MA. Diagnostic and therapeutic utility of double-balloon enteroscopy in children. J Pediatr Gastroenterol Nutr. 2014;58:204–212. doi: 10.1097/MPG.0000000000000192. [DOI] [PubMed] [Google Scholar]
- 78.Watanabe O, Ando T, Ishiguro K, Maeda O, Miyake N, Nakamura M, Miyahara R, Ohmiya N, Goto H. Symptoms in patients with Crohn’s disease are related to the presence of strictures rather than to that of active ulcers in the small bowel by the examination of double-balloon enteroscopy. Gastrointest Endosc. 2010;71:AB375–AB376. doi: 10.1016/j.gie.2010.03.1032. [DOI] [Google Scholar]
- 79.Westerhoff M, Pai R, Wilcox R, Semrad C, Noffsinger A, Hart J. Small bowel pathology revealed by double balloon enteroscopy. Lab Invest. 2009;89:152A. doi: 10.1038/labinvest.2008.138. [DOI] [Google Scholar]
- 80.Zhang SH, Xu J, Qing Q, Zhi FC, Bai Y, Xu ZM, Jiang B, Zhang YL, Chen Y. [Value of deep small-bowel endoscopy in the diagnosis of Crohn’s disease] Nanfang Yike Daxue Xuebao. 2011;31:637–640. [PubMed] [Google Scholar]
- 81.Zhi FC, Xiao B, Jiang B, Wan TM, Guo Y, Zhou D, Wang LH, Chen JF, Xie L, Pan DS, et al. Double-balloon enteroscopy in detecting small intestinal bleeding [Internet] Zhonghua Yixue Zazhi. 2005;118:1834–1837. [PubMed] [Google Scholar]
- 82.Choi DH, Jeon SR, Kim JO, Kim HG, Lee TH, Lee WC, Kang BS, Cho JH, Jung Y, Kim WJ, et al. Double-balloon enteroscopy in elderly patients: is it safe and useful? Intest Res. 2014;12:313–319. doi: 10.5217/ir.2014.12.4.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Roushan N, Froutan H, Taslimi R, Kalani M, Ganji A, Darvish Moghaddam S, Farahvash MJ, Khazaeipour Z. Double-balloon Enteroscopy: The results of a new experience in Iran. Med J Islam Repub Iran. 2014;28:19. [PMC free article] [PubMed] [Google Scholar]
- 84.Chen LH, Chen WG, Cao HJ, Zhang H, Shan GD, Li L, Zhang BL, Xu CF, Ding KL, Fang Y, et al. Double-balloon enteroscopy for obscure gastrointestinal bleeding: a single center experience in China. World J Gastroenterol. 2010;16:1655–1659. doi: 10.3748/WJG.v16.i13.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ding NS, Yip W, Hanna M, Saunders B, Thomas-Gibson S, Humphries A, Hart A. Five year outcomes of Crohn’s anastamotic strictures treated with balloon dilatation. J Crohns Colitis. 2015;9 Suppl 1:S285. doi: 10.1093/ecco-jcc/jju027.530. [DOI] [Google Scholar]
- 86.Yu LF, Zhong J, Cheng SD, Tang YH, Miao F. Low-dose azathioprine effectively improves mucosal healing in Chinese patients with small bowel Crohn’s disease. J Dig Dis. 2014;15:180–187. doi: 10.1111/1751-2980.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xu N, Li NE, Cao XL, Wang L, Li XT, Huang LY. The benefit of double-balloon enteroscopy combined with abdominal contrast-enhanced CT examination for diagnosing small-bowel obstruction. Acta Endoscopica. 2013;43:242–247. doi: 10.1007/s10190-013-0342-4. [DOI] [Google Scholar]
- 88.Watanabe O, Ando T, Ishiguro K, Maeda O, Miyake N, Nakamura M, Miyahara R, Ohmiya N, Goto H. Recurrence of Ulcers After Small Bowel Resection in Patients With Crohn’s Disease: Efficacy of Infliximab As Assessed by Double-Balloon Endoscopy. Gastrointest Endosc. 2010;71:AB376. doi: 10.1016/j.gie.2010.03.1033. [DOI] [Google Scholar]
- 89.Morise K, Ando T, Watanabe O, Nakamura M, Miyahara R, Maeda O, Ishiguro K, Hirooka Y, Goto H. Clinical utility of a new endoscopic scoring system for Crohn’s disease. World J Gastroenterol. 2015;21:9974–9981. doi: 10.3748/wjg.v21.i34.9974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Akarsu M, Akkaya Özdinç S, Celtik A, Akpınar H. Diagnostic and therapeutic efficacy of double-balloon endoscopy in patients with small intestinal diseases: single-center experience in 513 procedures. Turk J Gastroenterol. 2014;25:374–380. doi: 10.5152/tjg.2014.5191. [DOI] [PubMed] [Google Scholar]
- 91.Hirai F, Beppu T, Takatsu N, Yano Y, Ninomiya K, Ono Y, Hisabe T, Matsui T. Long-term outcome of endoscopic balloon dilation for small bowel strictures in patients with Crohn’s disease. Dig Endosc. 2014;26:545–551. doi: 10.1111/den.12236. [DOI] [PubMed] [Google Scholar]
- 92.Aktas H, De Ridder L, Haringsma J, Kuipers EJ, Mensink PB. Complications of single-balloon enteroscopy: A prospective evaluation of 166 procedures. Endoscopy. 2010;42:365–368. doi: 10.1055/s-0029-1243931. [DOI] [PubMed] [Google Scholar]
- 93.Safatle-Ribeiro AV, Arraes LR, Ishida RK, Kawaguti FS, Iriya K, Ribeiro U, De Moura EG, Sakai P. Promptly indication of balloon assisted enteroscopy increases the diagnostic yield in patients with current overt obscure gastrointestinal bleeding. Gastrointest Endosc. 2011;(1):AB458. doi: 10.1016/j.gie.2011.03.1087. [DOI] [Google Scholar]
- 94.Navaneethan U, Vargo J, Menon KVN, Sanaka M, Tsai CJ. Impact of device-assisted enteroscopy on the diagnosis and management of suspected and established small bowel crohn’s disease. Am J Gastroenterol. 2012;107:S124. doi: 10.1038/ajg.2012.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Aktas H, Mensink P, Biermann K, Fry LC, Van Der Woude CJ, Malfertheiner P, Monkemuller K. Additional yield of histological sampling in patients with suspected small bowel pathology during balloon assisted enteroscopy. Gastrointest Endosc. 2010;71:AB378. doi: 10.1016/j.gie.2010.03.1041. [DOI] [Google Scholar]
- 96.Arihiro S, Kato T, Tajiri H. Single-balloon enteroscopy for diagnosis and treatment of small intestine. Dig Endosc. 2010;22:A28. doi: 10.1111/j.1443-1661.2010.01003.x. [DOI] [Google Scholar]
- 97.de Ridder L, Mensink PB, Lequin MH, Aktas H, de Krijger RR, van der Woude CJ, Escher JC. Single-balloon enteroscopy, magnetic resonance enterography, and abdominal US useful for evaluation of small-bowel disease in children with (suspected) Crohn’s disease. Gastrointest Endosc. 2012;75:87–94. doi: 10.1016/j.gie.2011.07.036. [DOI] [PubMed] [Google Scholar]
- 98.Di Nardo G, Oliva S, Aloi M, Casciani E, Alessandri C, Di Camillo C, Del Giudice E, Valitutti F, Isoldi S, Cucchiara S. Usefulness of single-balloon enteroscopy in pediatric Crohn’s disease. Dig Liver Dis. 2011;43:S405–S406. doi: 10.1016/S1590-8658(11)60630-0. [DOI] [Google Scholar]
- 99.Dutta AK, Sajith KG, Joseph AJ, Simon EG, Chacko A. Learning curve, diagnostic yield and safety of single balloon enteroscopy. Trop Gastroenterol. 2012;33:179–184. doi: 10.7869/tg.2012.45. [DOI] [PubMed] [Google Scholar]
- 100.Manno M, Riccioni ME, Cannizzaro R, Andreoli A, Marmo R, Pennazio M. Diagnostic and therapeutic yield of single balloon enteroscopy in patients with suspected small-bowel disease: Results of the Italian multicentre study. Dig Liver Dis. 2013;45:211–215. doi: 10.1016/j.dld.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 101.Russo E, Hoare JM. Single-balloon enteroscopy performed on routine endoscopy lists under conscious sedation. A retrospective report on a single UK centre’s experience. Gastroenterology. 2011;(1):S558. doi: 10.1016/S0016-5085(11)62311-1. [DOI] [Google Scholar]
- 102.Tsujikawa T, Saitoh Y, Andoh A, Imaeda H, Hata K, Minematsu H, Senoh K, Hayafuji K, Ogawa A, Nakahara T, et al. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: Preliminary experiences. Endoscopy. 2008;40:11–15. doi: 10.1055/s-2007-966976. [DOI] [PubMed] [Google Scholar]
- 103.Yoshida A, Takatsuka K, Ueno F, Kobayashi K, Iwabuchi S. Therapeutic single-balloon enteroscopy for small intestinal stenosis may modify outcome of patients with crohn’s disease receiving infliximab. Am J Gastroenterol. 2010;105:S421. doi: 10.1038/ajg.2010.320-9. [DOI] [Google Scholar]
- 104.Zhu M, Tang J, Jin XW, Mao GP, Ning SB, Zhang J, Li YF. Single balloon enteroscopy for diagnosis and treatment of small intestinal diseases. Shijie Huaren Xiaohua Zazhi. 2013;21:4189–4193. doi: 10.11569/wcjd.v21.i36.4189. [DOI] [Google Scholar]
- 105.Di Nardo G, Oliva S, Aloi M, Rossi P, Casciani E, Masselli G, Ferrari F, Mallardo S, Stronati L, Cucchiara S. Usefulness of single-balloon enteroscopy in pediatric Crohn’s disease. Gastrointest Endosc. 2012;75:80–86. doi: 10.1016/j.gie.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 106.Morar PS, Faiz O, Warusavitarne J, Brown S, Cohen R, Hind D, Abercrombie J, Ragunath K, Sanders DS, Arnott I, et al. Systematic review with meta-analysis: endoscopic balloon dilatation for Crohn’s disease strictures. Aliment Pharmacol Ther. 2015;42:1137–1148. doi: 10.1111/apt.13388. [DOI] [PubMed] [Google Scholar]
- 107.Mueller T, Rieder B, Bechtner G, Pfeiffer A. The response of Crohn’s strictures to endoscopic balloon dilation. Aliment Pharmacol Ther. 2010;31:634–639. doi: 10.1111/j.1365-2036.2009.04225.x. [DOI] [PubMed] [Google Scholar]
- 108.Endo K, Takahashi S, Shiga H, Kakuta Y, Kinouchi Y, Shimosegawa T. Short and long-term outcomes of endoscopic balloon dilatation for Crohn’s disease strictures. World J Gastroenterol. 2013;19:86–91. doi: 10.3748/wjg.v19.i1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Foster EN, Quiros JA, Prindiville TP. Long-term follow-up of the endoscopic treatment of strictures in pediatric and adult patients with inflammatory bowel disease. J Clin Gastroenterol. 2008;42:880–885. doi: 10.1097/MCG.0b013e3181354440. [DOI] [PubMed] [Google Scholar]
- 110.Navaneethan U, Parasa S, Venkatesh PG, Trikudanathan G, Shen B. Prevalence and risk factors for colonic perforation during colonoscopy in hospitalized inflammatory bowel disease patients. J Crohns Colitis. 2011;5:189–195. doi: 10.1016/j.crohns.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 111.Navaneethan U, Kochhar G, Phull H, Venkatesh PG, Remzi FH, Kiran RP, Shen B. Severe disease on endoscopy and steroid use increase the risk for bowel perforation during colonoscopy in inflammatory bowel disease patients. J Crohns Colitis. 2012;6:470–475. doi: 10.1016/j.crohns.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 112.Mukewar S, Costedio M, Wu X, Bajaj N, Lopez R, Brzezinski A, Shen B. Severe adverse outcomes of endoscopic perforations in patients with and without IBD. Inflamm Bowel Dis. 2014;20:2056–2066. doi: 10.1097/mib.0000000000000154. [DOI] [PubMed] [Google Scholar]
- 113.Hall B, Holleran G, Chin JL, Smith S, Ryan B, Mahmud N, McNamara D. A prospective 52 week mucosal healing assessment of small bowel Crohn’s disease as detected by capsule endoscopy. J Crohns Colitis. 2014;8:1601–1609. doi: 10.1016/j.crohns.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 114.Efthymiou A, Viazis N, Mantzaris G, Papadimitriou N, Tzourmakliotis D, Raptis S, Karamanolis DG. Does clinical response correlate with mucosal healing in patients with Crohn’s disease of the small bowel? A prospective, case-series study using wireless capsule endoscopy. Inflamm Bowel Dis. 2008;14:1542–1547. doi: 10.1002/ibd.20509. [DOI] [PubMed] [Google Scholar]
- 115.Small bowel mucosal healing and deep remission in patients with known small bowel Crohn’s disease. J Crohns Colitis 2015; 9 Suppl 1: S178. [DOI] [Google Scholar]
- 116.Kopylov U, Nemeth A, Koulaouzidis A, Makins R, Wild G, Afif W, Bitton A, Johansson GW, Bessissow T, Eliakim R, et al. Small bowel capsule endoscopy in the management of established Crohn’s disease: clinical impact, safety, and correlation with inflammatory biomarkers. Inflamm Bowel Dis. 2015;21:93–100. doi: 10.1097/MIB.0000000000000255. [DOI] [PubMed] [Google Scholar]
- 117.Sakuraba H, Ishiguro Y, Hasui K, Hiraga H, Fukuda S, Shibutani K, Takai Y. Prediction of maintained mucosal healing in patients with Crohn’s disease under treatment with infliximab using diffusion-weighted magnetic resonance imaging. Digestion. 2014;89:49–54. doi: 10.1159/000356220. [DOI] [PubMed] [Google Scholar]
- 118.Tielbeek JA, Löwenberg M, Bipat S, Horsthuis K, Ponsioen CY, D’Haens GR, Stoker J. Serial magnetic resonance imaging for monitoring medical therapy effects in Crohn’s disease. Inflamm Bowel Dis. 2013;19:1943–1950. doi: 10.1097/MIB.0b013e3182905536. [DOI] [PubMed] [Google Scholar]
- 119.Ordás I, Rimola J, Rodríguez S, Paredes JM, Martínez-Pérez MJ, Blanc E, Arévalo JA, Aduna M, Andreu M, Radosevic A, et al. Accuracy of magnetic resonance enterography in assessing response to therapy and mucosal healing in patients with Crohn’s disease. Gastroenterology. 2014;146:374–382.e1. doi: 10.1053/j.gastro.2013.10.055. [DOI] [PubMed] [Google Scholar]
- 120.Van Assche G, Herrmann KA, Louis E, Everett SM, Colombel JF, Rahier JF, Vanbeckevoort D, Meunier P, Tolan D, Ernst O, et al. Effects of infliximab therapy on transmural lesions as assessed by magnetic resonance enteroclysis in patients with ileal Crohn’s disease. J Crohns Colitis. 2013;7:950–957. doi: 10.1016/j.crohns.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 121.Kani K, Kato S, Kobayashi T, Yamamoto R, Nagoshi S, Yakabi K. Prospective comparison of computed tomography enterography (CTE) and double balloon enteroscopy (DBE) for the assessment of disease activity and mucosal healing in the small intestinal involvements in patients with crohn’s disease. Gastroenterology. 2013;(1):S424. doi: 10.1016/S0016-5085(13)61561-9. [DOI] [Google Scholar]
- 122.Jensen MD, Nathan T, Rafaelsen SR, Kjeldsen J. Diagnostic accuracy of capsule endoscopy for small bowel Crohn’s disease is superior to that of MR enterography or CT enterography. Clin Gastroenterol Hepatol. 2011;9:124–129. doi: 10.1016/j.cgh.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 123.Solem CA, Loftus EV, Fletcher JG, Baron TH, Gostout CJ, Petersen BT, Tremaine WJ, Egan LJ, Faubion WA, Schroeder KW, et al. Small-bowel imaging in Crohn’s disease: a prospective, blinded, 4-way comparison trial. Gastrointest Endosc. 2008;68:255–266. doi: 10.1016/j.gie.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 124.Jensen MD, Kjeldsen J, Rafaelsen SR, Nathan T. Diagnostic accuracies of MR enterography and CT enterography in symptomatic Crohn’s disease. Scand J Gastroenterol. 2011;46:1449–1457. doi: 10.3109/00365521.2011.613947. [DOI] [PubMed] [Google Scholar]
- 125.Niv E, Fishman S, Kachman H, Arnon R, Dotan I. Sequential capsule endoscopy of the small bowel for follow-up of patients with known Crohn’s disease. J Crohns Colitis. 2014;8:1616–1623. doi: 10.1016/j.crohns.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 126.Lim YJ, Yang CH. Non-steroidal anti-inflammatory drug-induced enteropathy. Clin Endosc. 2012;45:138–144. doi: 10.5946/ce.2012.45.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bjarnason I, Price AB, Zanelli G, Smethurst P, Burke M, Gumpel JM, Levi AJ. Clinicopathological features of nonsteroidal antiinflammatory drug-induced small intestinal strictures. Gastroenterology. 1988;94:1070–1074. doi: 10.1016/0016-5085(88)90568-9. [DOI] [PubMed] [Google Scholar]