Abstract
Objectives:
In contrast to two-dimensional planar images, a measuring point is hardly repeatedly determined in a CBCT image when alveolar bone loss is assessed. Thus, the aim of the present study was to propose a six-site measuring method, which is closely related to anatomical structure, for the evaluation of alveolar bone loss in CBCT images.
Methods:
150 measuring points in 11 molars and 14 premolars from 6 patients (2 males and 4 females) were included. CBCT images of the teeth were acquired prior to periodontal surgery. Four observers measured the distances between cemento–enamel junctions and the apical bases of the periodontal bone defect at the mesio–buccal, mid-buccal, disto–buccal, mesio–lingual/palatal, mid-lingual/palatal and disto–lingual/palatal sites in CBCT images. Direct measurements of the six sites were correspondingly obtained in the subsequent periodontal surgeries. Differences between the distances measured in the CBCT images and during the surgery were analysed. Interobserver and intraobserver variances were tested.
Results:
No statistically significant difference was found between the surgical and CBCT measurements (p = 0.84). Diagnostic coincidence rates of four observers were 86.7%, 87.3%, 88.7% and 88.0%, respectively. The interobserver (p = 0.95) and intraobserver (p = 0.30) variances were not significant.
Conclusions:
The six-site measuring method validated in the present study may be a useful three-dimensional measuring method for the evaluation of periodontal disease.
Keywords: periodontitis, alveolar bone level, three-dimensional imaging, CBCT
Introduction
Radiographic evaluation of periodontal bone loss is important for the diagnosis, treatment planning and prognosis evaluation of periodontitis.1 Commonly used radiographic examinations employ bitewing, periapical and panoramic radiographs.1,2 However, the methods suffer from the inherent drawbacks of plain radiographs, such as magnification, distortion and superimposition of adjacent anatomical structures.2–4 These drawbacks often limit the usefulness of these radiographs.1
CBCT is a recently developed imaging technique that can provide three-dimensional (3D) images similar to spiral CT images but gives a relatively low radiation dose to patients and a relatively high-quality image of the hard tissue.2,5 Since CBCT overcomes the inherent drawbacks from plain radiograph, it has been widely used in dentistry including periodontics.5,6 Because alveolar bone loss is an important index for the progress of periodontitis, many studies have focused on CBCT assessments of alveolar bone heights and bony defects and concluded that CBCT images are acceptable for the measurement of alveolar bone changes.7–10 These studies only identified the usefulness of CBCT images in staging periodontitis but did not further investigate whether these measurements could be repeatedly carried out in follow-up CBCT images since the same measuring point has rarely been determined in different 3D images.11,12 Furthermore, there are no specific guidelines about how to analyse this type of 3D images.11
To get a relatively accurate measurement of alveolar bone changes from a series of CBCT images, a six-site measuring method has been proposed in the present study. This method was established on the basis of clinical probing locations that are commonly used in the assessment of the alveolar bone level.13,14 Thus, the aim of the present study was to investigate the accuracy and repeatability of the method for alveolar bone level evaluation in CBCT images.
Methods and materials
Subjects
Patients who visited the Department of Periodontology at Peking University School and Hospital of Stomatology from May 2009 to October 2010 and had a diagnosis of chronic periodontitis or aggressive periodontitis were included in the study. Patients who had severe systematic disease or patients who smoked more than 10 cigarettes per day and had stopped smoking for less than 2 years were excluded. Basic therapy included oral hygiene instruction, plus scaling and root planning with ultrasonic devices and hand instruments. Periodontal probing depth and attachment loss were recorded during clinical measurements. Periodontal surgery was considered for sites with periodontal probing depth ≥5 mm. CBCT scanning was performed for affected teeth before surgery.
The study protocol was approved by the Ethics Committee of Peking University Health Science Center, Beijing, China.
Acquisition and measurements of CBCT images
Prior to surgery, CBCT scanning was performed on the affected teeth using a 3D Accuitomo system (J. Morita MFG Corp., Kyoto, Japan) with a field of view of 4 × 4 cm, tube voltage of 75–85 kVp and tube current of 5 mA. The voxel size used was 0.125 × 0.125 × 0.125 mm. CBCT images were reconstructed with 1.0-mm thickness and 1.0-mm intervals.
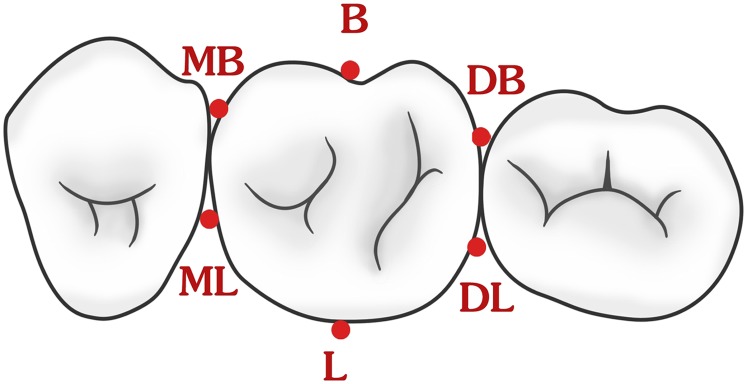
Distance between the cemento–enamel junction (CEJ) and the apical base of the periodontal bone defect (ABD) was measured using a six-site measuring method. The selected six sites were the mesio–buccal (MB) site, mid-buccal (B) site, disto–buccal (DB) site, mesio–lingual/palatal (ML) site, mid-lingual/palatal (L) and disto–lingual/palatal (DL) site. In the CBCT images, B and L points were chosen at the mid-buccal/lingual site in the surface. Points in proximal surfaces, i.e. the points of MB, DB, ML and DL, were located at the four sites close to the touch points between adjacent teeth. The schematic diagram of the six points is shown in Figure 1. Measurements of distances between CEJ and ABD were made at the six sites. The six sites were determined by observers according to the definition aforementioned with the help of a cursor on a 17-inch flat-panel monitor (L1750; Hewlett–Packard®, Palo Alto, CA). The four observers used i-Dixel-3DX software (J. Morita MFG Corp.) to view the images. Among the four observers, three observers were post-graduate students majoring in dental and maxillofacial radiology; one was a post-graduate student majoring in periodontology. Observers were trained and measuring procedure calibrated before performing the radiographic measurements.
Figure 1.
The diagram of the six measurements points for one molar tooth. B, mid-buccal; DB, disto–buccal; DL, disto–lingual/palatal; L, mid-lingual/palatal; MB, mesio–buccal; ML, mesio–lingual/palatal.
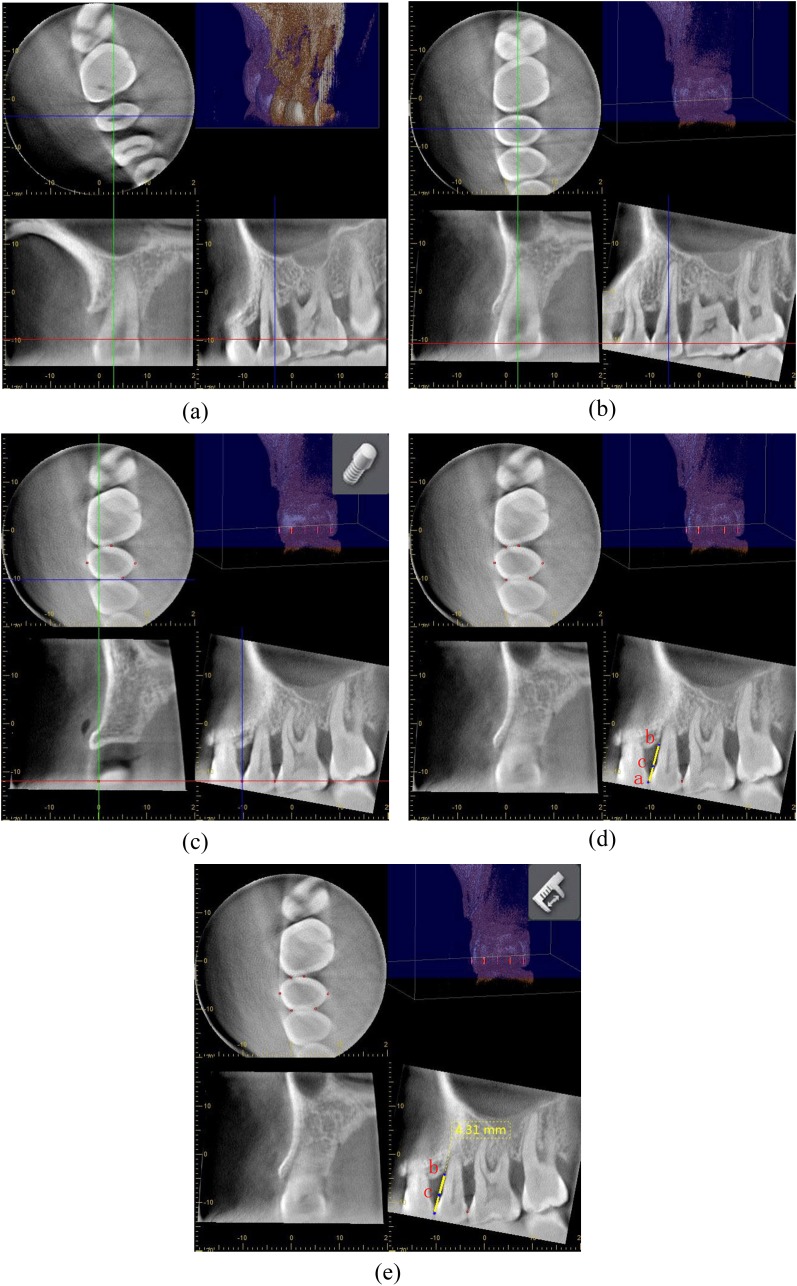
Detailed information about the measuring procedure is shown in Figure 2. First, the image of the test tooth was opened in the i-Dixel 3DX volume viewer (Figure 2a), and then the images were rotated to make the occlusal plane parallel to the red cursor (horizontal plane) and to make the median sagittal plane perpendicular to the horizontal plane (parallel to the blue cursor) (Figure 2b). Second, the aforementioned six sites were located based on the diagram of the six points shown in Figure 1. To make sure that all the points could be viewed three-dimensionally, i.e. in the axial, coronal and sagittal planes, the implant button (a cylindrical object with diameter of 0.5 mm and height of 0.5 mm) was used to fix the insertion point in the multiple planes (Figure 2c). Measurements of distances between CEJ and ABD were completed in accordance with the six sites. Take the MB site for example, CEJ was defined as the point where the image of the enamel disappeared. ABD characterizes the base of periodontal bone loss in the selected plane. The following is a summary of the measuring procedure: (1) define the contour point in the displayed mesial surface as point a and the ABD point as point b; (2) connect points a and b by a straight line; (3) draw a horizontal line through the CEJ so that the two straight lines intersect each other. The intersection of the two lines was defined as point c (Figure 2d); (4) measure the distance between points c and b, which is recorded as the distance between the CEJ and ABD (Figure 2e). The observers did not know any information about the teeth before surgery. All images were reviewed by one observer 1 month later for the evaluation of intraobserver agreement. Measurements were made to the nearest 0.01 mm with a linear measurement tool in a quiet and dark room. Test or adjacent teeth with crowns were not included because of beam-hardening artefacts.
Figure 2.
(a–e) The measuring procedure of CBCT images. (a) The CBCT images of the test tooth was opened in the i-Dixel 3DX volume viewer (J. Morita MFG Corp., Kyoto, Japan). (b) The images were rotated to make the occlusal plane parallel to the red cursor (horizontal plane) and the median sagittal plane perpendicular to the horizontal plane (parallel to the blue cursor). (c) The aforementioned six sites which can be viewed three-dimensionally were located in the images, and the implant button was used. (d) Defining the contour point in the displayed mesial surface as point a, the apical base of the periodontal bone defect point as point b; connect points a and b by a straight line. Drawing a horizontal line through the cemento–enamel junction, the two straight lines intersect each other, define the intersection as point c. (e) Measuring the distance between points c and b, which is recorded as the distance from CEJ to ABD. For colour image see online.
Intrasurgical measurements
The patients were injected with a local anaesthesia, flaps were reflected, defects were debrided thoroughly and direct surgical measurements were made. Distances between the CEJ and ABP were measured at the six sites (Figure 3). A manual periodontal probe (UNC-15; HU-Friedy, Chicago, IL) graded in millimetres was used. Measurements were made to the nearest 1 mm. All measurements were completed by an experienced periodontist (JXH) using the probe in a line parallel to the long axis of the tooth. The intrasurgical measurements were regarded as “reference standard”.
Figure 3.
Representative images of intrasurgical measurements of the first maxillary molar in the left side. (a) measurements of mesiobuccal (MB) site; (b) measurements of mid-buccal (B) site; and (c) measurements of disto-buccal (DB) site.
Data analysis
To evaluate the accuracy of site-based image assessment with clinical measurement, diagnostic coincidence rates were calculated via an introduced variable D-value.
D-value = intrasurgical measurement—measurement in CBCT images.
If the D-value ranged from −1 to 1 mm (−1 and 1 mm included), measurement in CBCT image was thought to be consistent with surgical measurement. If not, they were not consistent. Diagnostic coincidence rates were calculated.
Statistical analysis was performed with the IBM SPSS® Statistics 20 (IBM Corporation, Armonk, NY; formerly SPSS Inc., Chicago, IL). One-way analysis of variance was applied to find out whether the measurement of CBCT images differed significantly from the intrasurgical measurement. The D-values of all the observers were also tested via one-way analysis of variance. To test the linear correlation between the tooth category, site, observer and D-values, multiple linear regression analysis was applied. D-value was employed as the dependent variable, and tooth category (molar or premolar), site, observer were employed as independent variables. Paired-samples t-test was employed to test the intraobserver variances. A statistical significance was considered when p < 0.05.
Results
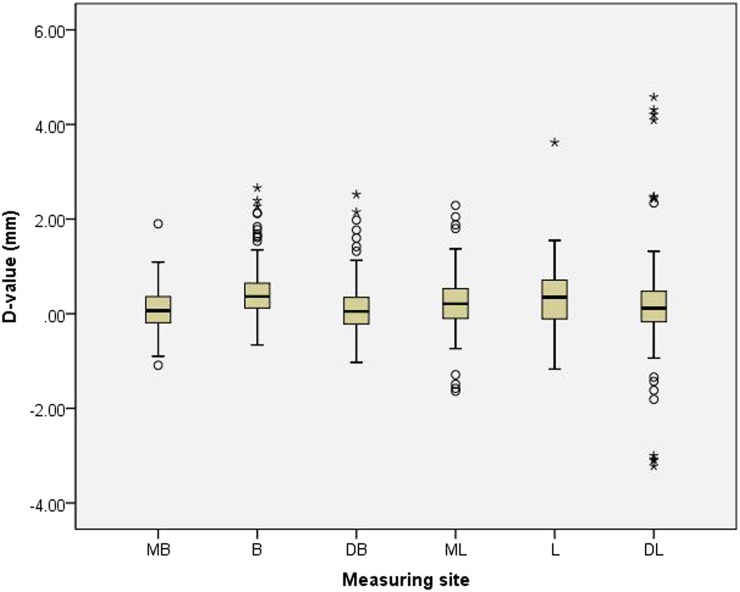
A total of 150 measuring sites in 11 molars and 14 premolars from 6 patients (2 males and 4 females) were examined. Diagnostic coincidence rates of four observers were 86.7%, 87.3%, 88.7% and 88.0%, respectively. There was no significant difference between the measurement of CBCT images and intrasurgical measurement (p = 0.84), as well as no significant differences among D-values of all the observers (p = 0.95). The data distribution of the six measuring sites is shown in Figure 4. Tables 1 and 2 demonstrate the mean D-values and standard deviation of premolars and molars from the four observers (Table 2). Multiple linear regression analysis showed that independent variables such as tooth category, site and observer had no linear influence on D-values. The intraobserver variance was not significant (p = 0.30).
Figure 4.
The box plot of D-values of six measuring sites. There was no statistical significance among the measurements of all the six sites (p > 0.5). Symbols indicate outliers, which show the discrete degree of data. B, mid-buccal; DB, disto-buccal; DL, disto-lingual/palatal; L, mid-lingual/palatal; MB, mesio–buccal; ML, mesio–lingual/palatal.
Table 1.
The mean D-values and standard deviations (SDs) of the molars
| Observer | Molar
(MD ± SD) |
|||||
|---|---|---|---|---|---|---|
| MB | B | DB | ML | L | DL | |
| 1 | 0.13 ± 0.62 | 0.58 ± 0.74 | 0.29 ± 0.83 | 0.31 ± 0.88 | 0.29 ± 0.46 | −0.02 ± 1.10 |
| 2 | 0.00 ± 0.52 | 0.68 ± 0.86 | 0.17 ± 0.75 | 0.17 ± 0.73 | 0.37 ± 0.50 | −0.07 ± 1.15 |
| 3 | 0.21 ± 0.74 | 0.59 ± 0.93 | 0.13 ± 0.74 | 0.36 ± 0.78 | 0.34 ± 0.45 | −0.04 ± 1.11 |
| 4 | 0.10 ± 0.60 | 0.54 ± 0.73 | 0.54 ± 0.77 | 0.39 ± 0.69 | 0.32 ± 0.35 | −0.10 ± 1.08 |
B, mid-buccal; DB, disto-buccal; DL, disto-lingual/palatal; L, mid-lingual/palatal; MD, the mean of D-value; MB, mesio–buccal; ML, mesio–lingual/palatal.
Table 2.
The mean D-values and standard deviations (SDs) of premolars
| Observer | Premolar
(MD ± SD) |
|||||
|---|---|---|---|---|---|---|
| MB | B | DB | ML | L | DL | |
| 1 | 0.07 ± 0.40 | 0.48 ± 0.52 | 0.18 ± 0.53 | 0.16 ± 0.55 | 0.19 ± 0.66 | 0.52 ± 1.46 |
| 2 | 0.07 ± 0.40 | 0.42 ± 0.47 | 0.06 ± 0.67 | 0.15 ± 0.61 | 0.23 ± 0.77 | 0.42 ± 1.40 |
| 3 | 0.09 ± 0.34 | 0.41 ± 0.61 | 0.01 ± 0.55 | 0.11 ± 0.62 | 0.12 ± 0.70 | 0.31 ± 1.40 |
| 4 | 0.03 ± 0.31 | 0.34 ± 0.48 | 0.06 ± 0.64 | 0.22 ± 0.57 | 0.42 ± 1.15 | 0.38 ± 1.45 |
B, mid-buccal; DB, disto-buccal; DL, disto-lingual/palatal; L, mid-lingual/palatal; MD, the mean of D-value; MB, mesio–buccal; ML, mesio–lingual/palatal.
Discussions
The results from the present study suggest that the six measuring sites provide useful alveolar bone information for premolars and molars. In the search of literature, we found that most of the studies focusing on the measurement accuracy of periodontal bone loss/defect were in vitro studies.7–9,15–20 Only one in vivo study was performed on the measurement accuracy of bone defects on the maxillary molar.21 Although there are a few more in vivo studies with regard to periodontal bone height measurement using CBCT, two of which are case reports,22,23 others compared different methods of measuring guided tissue regeneration-treated bone defects and furcation lesions.24–27 Thus, the present study is the first in vivo study for the evaluation of alveolar bone levels in premolar.21,24,25
CBCT can provide a 3D view of periodontal bone situation, and therefore CBCT may be a useful and practical tool for the clinical evaluation of periodontal bone changes over time.26,28,29 However, compared with the plain two-dimensional periapical or bitewing radiographs, the big challenge for CBCT images to evaluate alveolar bone levels is how to find the same measuring site after a period of time.1 Furthermore, the selected measuring sites should fulfil the following criteria. First, they should be feasible for clinical use, in other words, the sites are easily accessed; second, it is precise enough for a measurement; third, no interobserver or intraobserver variability is present for a measurement.30,31 The six-site method proposed by the present study seems to be a proper choice according to the required criteria. In fact, the six sites were established on the basis of probing location clinically used for the assessment of alveolar bone level.13,14 This makes the method practical and easy to use.
Diagnostic coincidence rate was introduced to study the accuracy of the six-site measuring method in evaluating periodontal bone levels. Since there is no gold standard or a gauge for the clinical assessment of periodontal disease,14,31 precision to ±1 mm of a manual periodontal probe was acceptable in clinical experience.26,32–34 Thus, when the radiographic measurements of the studied alveolar bone levels were in the range of the clinical measurements ±1 mm, the radiographic measurement was considered accurate.9 The diagnostic coincidence rates from the present study were >85% for all the measuring sites by the four observers. This implies that the six-site method provides a favourable diagnostic efficiency. Interobserver and intraobserver variability was also not found by the use of the six-site method. Since the four observers were post-graduates at different grades, the results also imply that calibration and observers' training on how to make a measurement in CBCT images before one study is more important than the observers' clinical experience. This was in accordance with the previous studies.10,35
To make the clinical measuring sites closely relate to the measuring sites identified in CBCT images to the maximum extent, some studies had pre-defined the measuring sites. In their vitro studies, gutta-percha, metal spheres or engineered notch were often used for the determination of measuring sites clinically and in CBCT images.7,9,15 This reduces the measuring differences obtained from the different measuring method, but it is not practical in clinics. In the in vivo study by Feijo et al,21 a 12-point method was suggested for the measurement of the horizontal alveolar bone defect. However, only one observer assessed the bone levels and no data on interobserver and intraobserver variability were provided in the study. Repitition test of the method was not validated.
Although the measurement accuracy of the alveolar bone levels in the studied CBCT images has been identified, Figure 4 shows a relatively large standard deviation in the measurements of DL site when compared with other sites. One possible reason may be the loss of the distal tooth, which makes it harder to identify the exact DL site in the CBCT images. The other reason may be due to the fact that the lingual side is not in a direct vision for locating a measuring site. Limited sample size may also lead to large variations among patients. Other studies also suggest that it is difficult to duplicate precisely the site and angulation of measurement from one visit to another.7,9
Statistical analysis indicates that no significant difference exists between the tomographic and surgical measurements of alveolar bone levels and that the overall measurement is a little bit underestimated except for the points in the distal of premolars. This is in line with the previous studies in which the measurement accuracy of alveolar bone levels in intraoral radiograph and CBCT images was compared with and confirmed by a direct surgical measurement.9,24,26 This may imply that the severity of alveolar bone loss is heavier in a real patient than a measurement in CBCT images.
In conclusion, the six-site measuring method proposed in the present study may be a useful 3D measuring method for the evaluation of periodontal disease.
Acknowledgments
Acknowledgments
The authors would like to gratefully acknowledge Dr Charles Hildebolt for the serious discussion on the subject and kind offer for language editing. Special thanks also goes to Dr Xiao-Yan Yan and Dr Da-Jin Liu, Department of Epidemiology and Biostatistics, Peking University Health Science Center, Beijing, China, for performing the statistical analysis of the study and to Dr Shuai Hao, Editor and Journalist of Stomatology Today, China Medical Tribune, for drawing and offering Figure 1.
Contributor Information
Yu-Jiao Guo, Email: amberring@126.com.
Gang Li, Email: kqgang@bjmu.edu.cn.
References
- 1.Corbet EF, Ho DK, Lai SM. Radiographs in periodontal disease diagnosis and management. Aust Dent J 2009; 54(Suppl. 1): S27–43. doi: 10.1111/j.1834-7819.2009.01141.x [DOI] [PubMed] [Google Scholar]
- 2.Mol A. Imaging methods in periodontology. Periodontol 2000 2004; 34: 34–48. doi: 10.1046/j.0906-6713.2003.003423.x [DOI] [PubMed] [Google Scholar]
- 3.Kim TS, Obst C, Zehaczek S, Geenen C. Detection of bone loss with different X-ray techniques in periodontal patients. J Periodontol 2008; 79: 1141–9. doi: 10.1902/jop.2008.070578 [DOI] [PubMed] [Google Scholar]
- 4.Brägger U. Radiographic parameters: biological significance and clinical use. Periodontol 2000 2005; 39: 73–90. doi: 10.1111/j.1600-0757.2005.00128.x [DOI] [PubMed] [Google Scholar]
- 5.Miracle AC, Mukherji SK. Conebeam CT of the head and neck, part 2: clinical applications. AJNR Am J Neuroradiol 2009; 30: 1285–92. doi: 10.3174/ajnr.A1654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naitoh M, Yamada S, Noguchi T, Ariji E, Nagao J, Mori K, et al. Three-dimensional display with quantitative analysis in alveolar bone resorption using cone-beam computerized tomography for dental use: a preliminary study. Int J Periodontics Restorative Dent 2006; 26: 607–12. [PubMed] [Google Scholar]
- 7.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol 2006; 77: 1261–6. doi: 10.1902/jop.2006.050367 [DOI] [PubMed] [Google Scholar]
- 8.Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: an in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol 2008; 37: 252–60. doi: 10.1259/dmfr/57711133 [DOI] [PubMed] [Google Scholar]
- 9.Mol A, Balasundaram A. In vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofac Radiol 2008; 37: 319–24. doi: 10.1259/dmfr/26475758 [DOI] [PubMed] [Google Scholar]
- 10.de Faria Vasconcelos K, Evangelista KM, Rodrigues CD, Estrela C, de Sousa TO, Silva MA. Detection of periodontal bone loss using cone beam CT and intraoral radiography. Dentomaxillofac Radiol 2012; 41: 64–9. doi: 10.1259/dmfr/13676777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naji P, Alsufyani NA, Lagravère MO. Reliability of anatomic structures as landmarks in three-dimensional cephalometric analysis using CBCT. Angle Orthod 2014; 84: 762–72. doi: 10.2319/090413-652.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oz U, Orhan K, Abe N. Comparison of linear and angular measurements using two-dimensional conventional methods and three-dimensional cone beam CT images reconstructed from a volumetric rendering program in vivo. Dentomaxillofac Radiol 2011; 40: 492–500. doi: 10.1259/dmfr/15644321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savage A, Eaton KA, Moles DR, Needleman I. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J Clin Periodontol 2009; 36: 458–67. doi: 10.1111/j.1600-051X.2009.01408.x [DOI] [PubMed] [Google Scholar]
- 14.Andrade R, Espinoza M, Gómez EM, Espinoza JR, Cruz E. Intra- and inter-examiner reproducibility of manual probing depth. Braz Oral Res 2012; 26: 57–63. doi: 10.1590/S1806-83242012000100010 [DOI] [PubMed] [Google Scholar]
- 15.Pinsky HM, Dyda S, Pinsky RW, Misch KA, Sarment DP. Accuracy of three-dimensional measurements using cone-beam CT. Dentomaxillofac Radiol 2006; 35: 410–16. doi: 10.1259/dmfr/20987648 [DOI] [PubMed] [Google Scholar]
- 16.Braun X, Ritter L, Jervøe-Storm PM, Frentzen M. Diagnostic accuracy of CBCT for periodontal lesions. Clin Oral Investig 2014; 18: 1229–36. doi: 10.1007/s00784-013-1106-0 [DOI] [PubMed] [Google Scholar]
- 17.Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 395–401. doi: 10.1016/j.tripleo.2007.03.012 [DOI] [PubMed] [Google Scholar]
- 18.Cook VC, Timock AM, Crowe JJ, Wang M, Covell DA, Jr. Accuracy of alveolar bone measurements from cone beam computed tomography acquired using varying settings. Orthod Craniofac Res 2015; 18(Suppl. 1): 127–36. doi: 10.1111/ocr.12072 [DOI] [PubMed] [Google Scholar]
- 19.Fleiner J, Hannig C, Schulze D, Stricker A, Jacobs R. Digital method for quantification of circumferential periodontal bone level using cone beam CT. Clin Oral Investig 2013; 17: 389–96. doi: 10.1007/s00784-012-0715-3 [DOI] [PubMed] [Google Scholar]
- 20.Takeshita WM, Vessoni Iwaki LC, Da Silva MC, Tonin RH. Evaluation of diagnostic accuracy of conventional and digital periapical radiography, panoramic radiography, and cone-beam computed tomography in the assessment of alveolar bone loss. Contemp Clin Dent 2014; 5: 318–23. doi: 10.4103/0976-237X.137930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feijo CV, Lucena JG, Kurita LM, Pereira SL. Evaluation of cone beam computed tomography in the detection of horizontal periodontal bone defects: an in vivo study. Int J Periodontics Restorative Dent 2012; 32: e162–8. [PubMed] [Google Scholar]
- 22.Songa VM, Jampani ND, Babu V, Buggapati L, Mittapally S. Accuracy of cone beam computed tomography in diagnosis and treatment planning of periodontal bone defects: a case report. J Clin Diagn Res 2014; 8: ZD23–5. doi: 10.7860/JCDR/2014/11165.5348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakajima K, Yamaguchi T, Maki K. Surgical orthodontic treatment for a patient with advanced periodontal disease: evaluation with electromyography and 3-dimensional cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2009; 136: 450–9. doi: 10.1016/j.ajodo.2007.03.042 [DOI] [PubMed] [Google Scholar]
- 24.Qiao J, Wang S, Duan J, Zhang Y, Qiu Y, Sun C, et al. The accuracy of cone-beam computed tomography in assessing maxillary molar furcation involvement. J Clin Periodontol 2014; 41: 269–74. doi: 10.1111/jcpe.12150 [DOI] [PubMed] [Google Scholar]
- 25.Walter C, Weiger R, Zitzmann NU. Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J Clin Periodontol 2010; 37: 436–41. doi: 10.1111/j.1600-051X.2010.01556.x [DOI] [PubMed] [Google Scholar]
- 26.Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol 2009; 80: 48–55. doi: 10.1902/jop.2009.080289 [DOI] [PubMed] [Google Scholar]
- 27.Walter C, Kaner D, Berndt DC, Weiger R, Zitzmann NU. Three-dimensional imaging as a pre-operative tool in decision making for furcation surgery. J Clin Periodontol 2009; 36: 250–7. doi: 10.1111/j.1600-051X.2008.01367.x [DOI] [PubMed] [Google Scholar]
- 28.Jervøe-Storm PM, Hagner M, Neugebauer J, Ritter L, Zöller JE, Jepsen S, et al. Comparison of cone-beam computerized tomography and intraoral radiographs for determination of the periodontal ligament in a variable phantom. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e95–101. doi: 10.1016/j.tripleo.2009.10.023 [DOI] [PubMed] [Google Scholar]
- 29.Ferreira PP, Torres M, Campos PS, Vogel CJ, de Araújo TM, Rebello IM. Evaluation of buccal bone coverage in the anterior region by cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2013; 144: 698–704. doi: 10.1016/j.ajodo.2013.07.010 [DOI] [PubMed] [Google Scholar]
- 30.Holtfreter B, Alte D, Schwahn C, Desvarieux M, Kocher T. Effects of different manual periodontal probes on periodontal measurements. J Clin Periodontol 2012; 39: 1032–41. doi: 10.1111/j.1600-051X.2012.01941.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hefti AF, Preshaw PM. Examiner alignment and assessment in clinical periodontal research. Periodontol 2000 2012; 59: 41–60. doi: 10.1111/j.1600-0757.2011.00436.x [DOI] [PubMed] [Google Scholar]
- 32.Khan S, Cabanilla LL. Periodontal probing depth measurement: a review. Compend Contin Educ Dent 2009; 30: 12–14, 16, 18–21; quiz 22, 36. [PubMed] [Google Scholar]
- 33.Armitage GC. Clinical evaluation of periodontal diseases. Periodontol 2000 1995; 7: 39–53. doi: 10.1111/j.1600-0757.1995.tb00035.x [DOI] [PubMed] [Google Scholar]
- 34.Armitage GC; Research, Science and Therapy Committee of the American Academy of Periodontology. Diagnosis of periodontal diseases. J Periodontol 2003; 74: 1237–47. doi: 10.1902/jop.2003.74.8.1237 [DOI] [PubMed] [Google Scholar]
- 35.Ozmeric N, Kostioutchenko I, Hägler G, Frentzen M, Jervøe-Storm PM. Cone-beam computed tomography in assessment of periodontal ligament space: in vitro study on artificial tooth model. Clin Oral Investig 2008; 12: 233–9. doi: 10.1007/s00784-008-0186-8 [DOI] [PubMed] [Google Scholar]