Abstract
Objectives:
The purpose of this study was to determine the visibility of the mandibular canal (MC) in CBCT images and if the visibility of the MC is affected by gender, location and/or age.
Methods:
CBCT images were evaluated for the visibility of the MC by a board-certified oral and maxillofacial radiologist, a board-certified periodontist and a periodontics resident. Representative slices were examined for the first premolar (PM1), second premolar (PM2), first molar (M1) and second molar (M2) sites by all examiners. The visibility of the MC was registered as either present or absent.
Results:
360 total CBCT cross-sectional images were examined, with the MC identified in 204 sites (56%). Age had a significant effect on MC visibility, but it differed by location: for PM1, age 47–56 had lower visibility than age 65+ (p = 0.0377). Gender also had a significant effect on canal visibility, where females had lower visibility than males overall (p = 0.0178) and had the most pronounced difference for PM1 (p = 0.0054). Location had a significant effect on visibility, but it differed by age and by gender: for age 65+, M2 had lower visibility than PM1 (p = 0.0411) and PM2 (p = 0.0180), while for females, PM1 had lower visibility than M1 (p = 0.0123) and M2 (p = 0.0419).
Conclusions:
The MC was visualized only in just over half of the CBCT images. Age, gender and location had significant effects on the visibility.
Keywords: cone-beam CT, mandible, dental implants, diagnostic imaging, radiology
Introduction
According to the Third National Health and Nutrition Examination Survey 1988–1994, 70% of the US population aged 18 years and older was partially or completely edentulous.1 The primary aetiologies of tooth loss are periodontal disease and dental caries.1,2 Tooth loss affects many people psychologically, socially and physically by decreasing their quality of life.1–7 The use of dental implants is commonly the treatment of choice in restoring areas of missing teeth in partially or fully edentulous patients.5 Implant and implant prosthodontic success rates are frequently higher than natural teeth-supported traditional prostheses.1,2 Available bone height is often a major limiting factor determining implant length and placement. The posterior regions of the jaws usually have the least height of existing bone because the maxillary sinus pneumatization after tooth loss and the mandibular canal (MC) is 10 mm or more above the inferior border of the mandibular body.1 Radiographic analysis is vital for successful dental implant treatment planning.
The MC is a bilateral anatomical structure extending from the mandibular foramen to the mental foramen carrying the inferior alveolar nerve, artery and vein.8 During implant placement, the contents of the MC may be at risk.9 The available height of the potential implant site is determined by the distance between the alveolar crest of ridge and the superior cortical bone of the MC.10 Several imaging modalities have been used to assess the course of the MC, including panoramic radiography,8 conventional tomography,11 CT,12,13 intraoral periapical films and CBCT.14 Panoramic radiography lacks accuracy and reliability with regards to calculations of distances made using them.15,16 Conventional tomography provides uniformly magnified images in two dimensions, usually sagittal and coronal cross-sections, but the images are of only a few teeth in the arch.17 Blurring occurs of the areas not in focus and can make it difficult to identify structures and interpret the images.18,19 The clarity of conventional tomography has increased as a result of the increasingly complex, synchronized, polydirectional movement patterns during imaging.20 However, the patient radiation dose has also increased as a result. Medical CT provides accurate three-dimensional images of oral anatomy that have high soft- and hard-tissue contrast resolution.21 However, they are expensive and have higher radiation exposure compared with other techniques. It is well known that the greatest fear of exposure to dental X-rays is the possibility of stochastic effects, which are those effects that may result despite how the level of radiation exposure and can be as severe as radiation-induced cancer and genetic defects.20 The image quality of CBCT systems and their relatively low dose and cost as compared with conventional or medical CT have increased the accessibility and use of three-dimensional imaging in dentistry.22 According to Pauwels et al23, the effective dose from CBCT examinations ranges from 45 to 83 µSv, although Hatcher24 reports that the effective dose from CBCT examinations can range as high as 206 µSv. Comparatively, the effective dose from one panoramic radiograph is approximately 10–14 µSv and the effective dose of a complete series of intraoral radiographs can range from 34.9 µSv (when using photo stimulable phosphor plates or F-speed film and the use of a rectangular collimator) to 388 µSv (when using a D-speed film and a round collimator).25 Radiation exposure following maxillomandibular imaging with medical CTs ranges from 474 to 1160 µSv.23 CBCT imaging allows for the visualization of dental structures and bone of the maxillofacial region in three dimensions with high resolution and can be utilized for multiple areas of the jaw.3–6 Many studies have demonstrated the use of CBCT imaging in clinical dentistry with regards to periodontics and implant surgery.15,26 At present, CBCT is one of the most frequently used imaging modalities for implant treatment planning.27 Identification of patient anatomy and potential risks of intrusion into vital structures are two of the most commonly cited uses of a CBCT.19 According to the American Academy of Oral and Maxillofacial Radiology, CBCTs should be considered as the imaging modality of choice for dental implant treatment planning, as the deficiencies of two-dimensional imaging techniques for accurate location of the MC are well documented.21 Furthermore, when evaluating the various tomographic techniques for pre-implant treatment planning, the posterior mandible has often been chosen as the test for accurate localization of the MC.14,20 Although the CBCT has been demonstrated to be superior to conventional imaging techniques for depicting the MC,28 the literature is controversial with regards to the accuracy of CBCT images visualizing the MC. Some studies suggest CBCT imaging offers a clear image of the mandibular anatomy and the precise location of the MC,29,30 reporting that a defined MC can be detected on the majority of exams.31 Yet, other studies demonstrate that the identification of the MC can be quite difficult using CBCT.32,33 The radiographic appearance usually involves a radiolucent zone lined by superior and inferior corticated borders of different variations, which may explain why the MC is hard to visualize in some cases.34 In 2011, Oliveira-Santos et al33 determined that the MC was readily visible in only 53% of the hemimandibles studied. The purpose of this retrospective radiographic study was to determine the frequency of the visualization of the MC on a CBCT cross-sectional image and to determine if the visibility of the MC is affected by the gender, location and/or age of the subject.
Methods and materials
The Institutional Review Board of Indiana University approved the study. CBCT images from the Indiana University School of Dentistry Imaging Facility were screened for inclusion in the study. Inclusion criteria were subjects 18 years of age, or older with a diagnosis of partial edentulism in the site of the mandibular second molar (M2), first molar (M1), second premolar (PM2) and first premolar (PM1) regions. All images were screened, deidentified and selected for evaluation by a periodontics resident (MM). Subjects' age and gender were collected for this study. CBCT imaging (i-CAT, Imaging Sciences International, Hatfield, PA) was performed with voxel size of 0.3 mm and exposure cycle of 8.5 s. Cross-sectional images perpendicular to the occlusal plane were deidentified and reformatted (1-mm thickness) using a compatible tomography imaging software (InVivo 5; Anatomage, San Jose, CA). All cross-sectional images were examined by a board-certified oral and maxillofacial radiologist (EP), a board-certified periodontist (SB) and a third-year periodontics resident (MM). The visibility of the MC on the cross-sectional images was assessed in one of four mandibular regions. The visibility of the MC was registered as either positive or negative. The visibility was registered as positive if it was undoubtedly differentiated from its surroundings, e.g. marrow spaces, bony lesions (Figures 1–3).
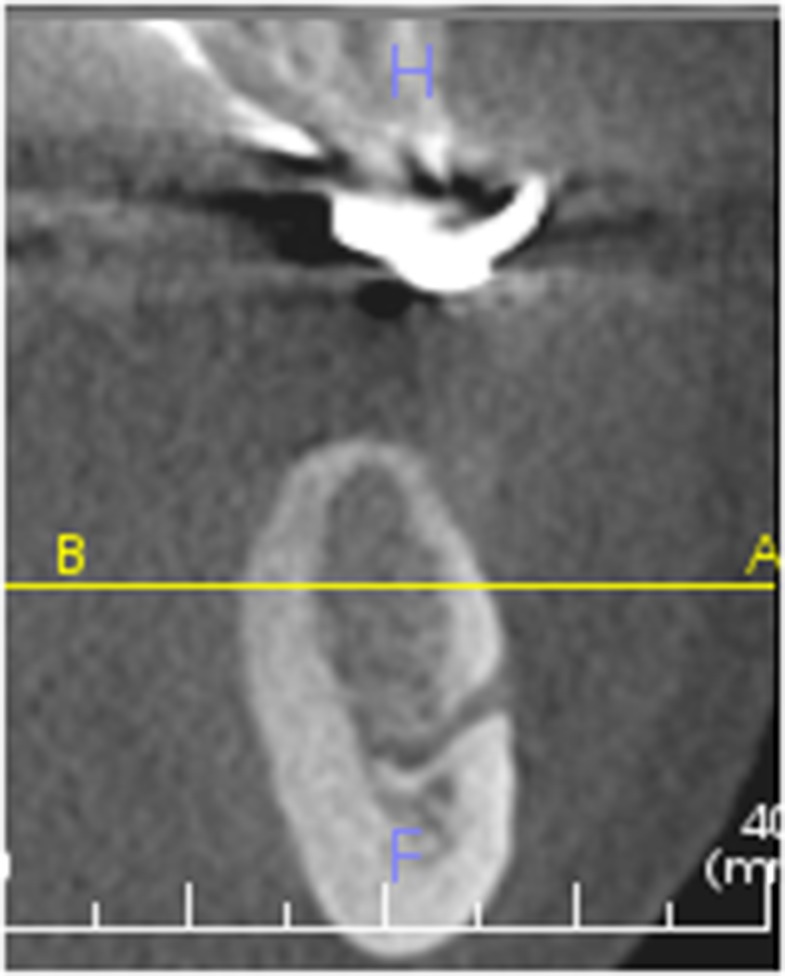
Figure 1.
Mental foramen visible at PM1 41 × 52 mm (96 × 96 dots per inch).
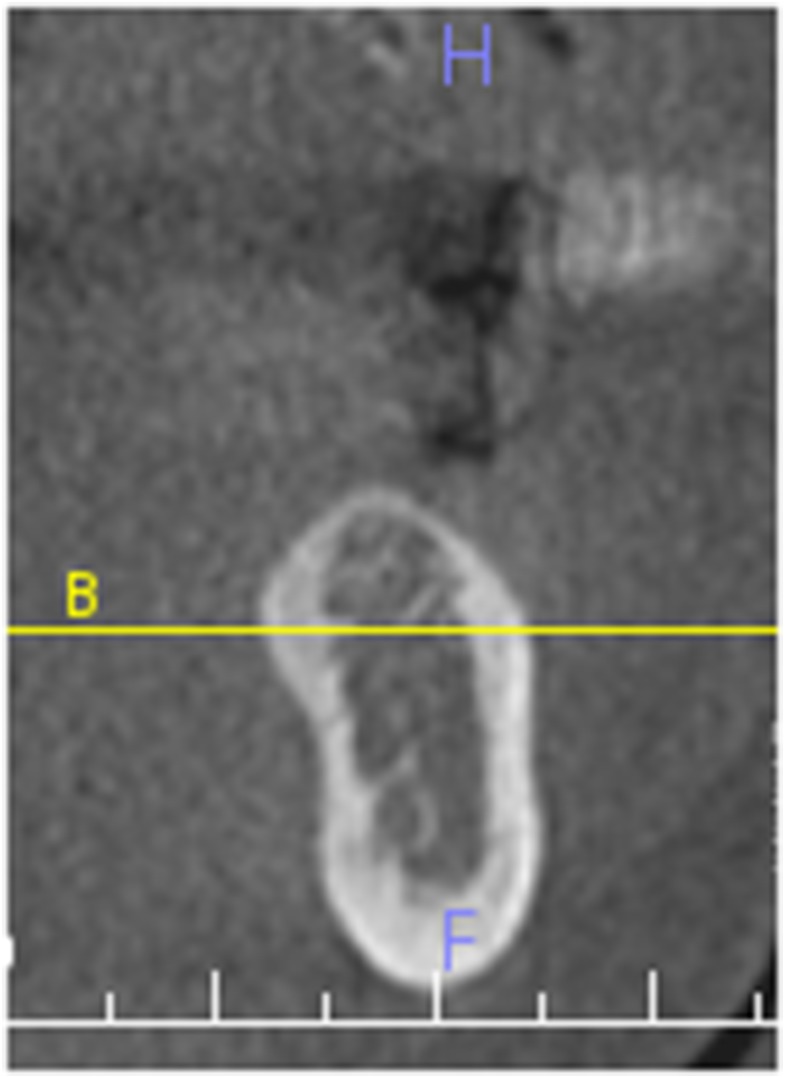
Figure 3.
Mandibular canal not distinguished from other anatomical structures at PM1 30 × 51 mm (96 × 96 dots per inch).
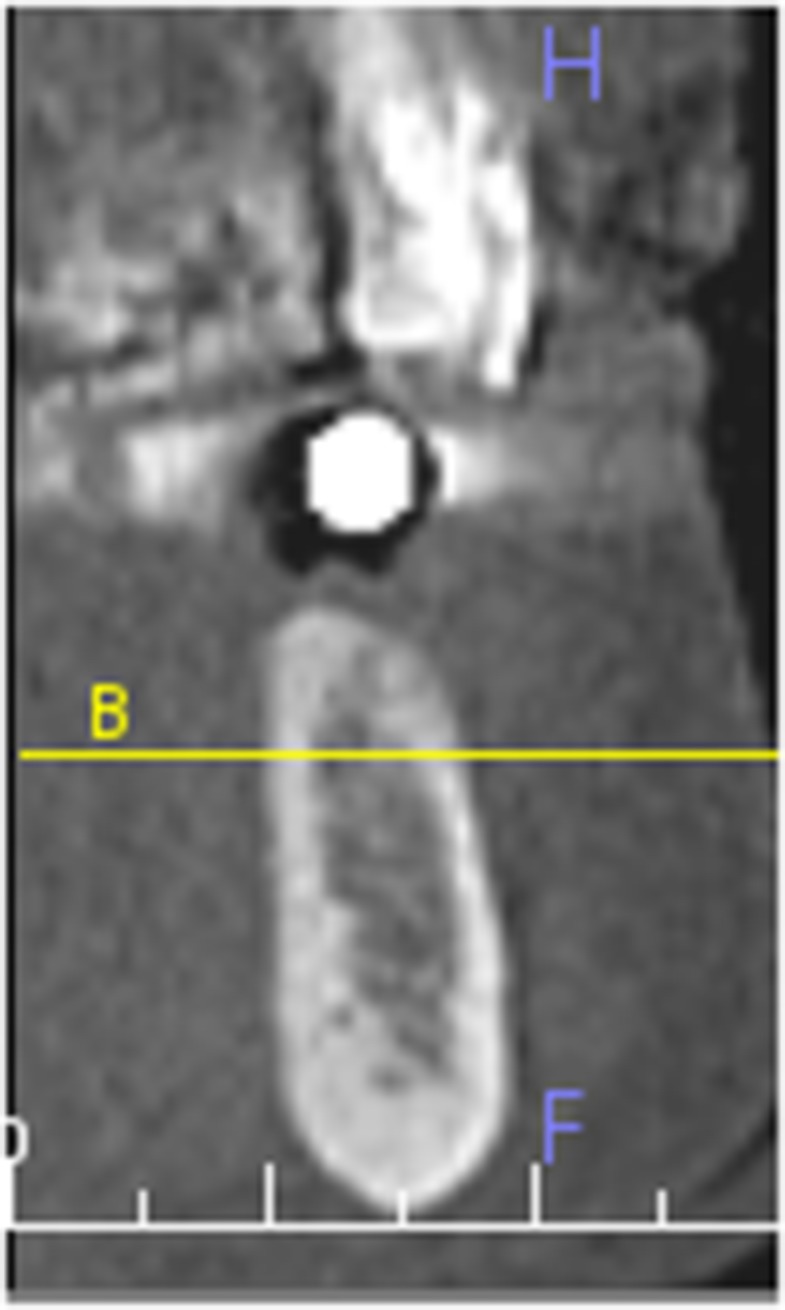
Figure 2.
Mandibular canal visible at M2 36 × 50 mm (96 × 96 dots per inch).
Sample size and statistical analyses
Based on the study by Oliviera-Santos et al,33 the assumption was made that the MC will be visible in approximately 50% of the CBCT scans. The calculations also assumed the sex distribution was relatively balanced, 60%/40% female/male or vice versa, and the expected age distribution was estimated to be approximately 80% age 50 and above and 20% below age 50. Assuming two-sided tests conducted at a 5% significance level, the study was designed to have 388 CBCT cross-sectional images for at least 80% power to detect a 15% difference in the percentage with visible MC between sexes (e.g. 42.5% visible in males vs 57.5% visible in females) within each region, and a 20% difference between age groups, both assuming no age–sex interaction. With our final sample size of 360 CBCT cross-sectional images, the power to detect age differences was still over 80%, but the power for sex differences was reduced to 76%.
The visibility of the MC was summarized using a two-level response (visible or not visible). The percentage of CBCT cross-sectional images with the MC visible was summarized overall and by gender, location and age. Age was split into quartiles for the analyses owing to a non-linear relationship between age and MC visibility. The associations of gender, age and location as well as the interactions among the three factors with the visibility of the MC were evaluated using generalized linear mixed-effects model for logistic regression. The model included random effects to account for the within-subject correlations among the locations and evaluations by multiple evaluators. An intraclass correlation coefficient (ICC) was calculated to evaluate the agreement among examiners.
Results
143 subjects were included in the study, 92 females (64%) and 51 males (36%). Ages ranged from 18 to 90 years, with average age 56 years. For the analyses, ages were categorized as <47, 47–56, 57–64 and 65+.
360 total CBCT cross-sectional images were examined, with the MC visible in 204 sites (56%). The ICC for agreement between evaluators was 0.53, indicating that while the overall percentages of images with the MC visible were similar for each evaluator, they did not necessarily agree on which MC were visible.
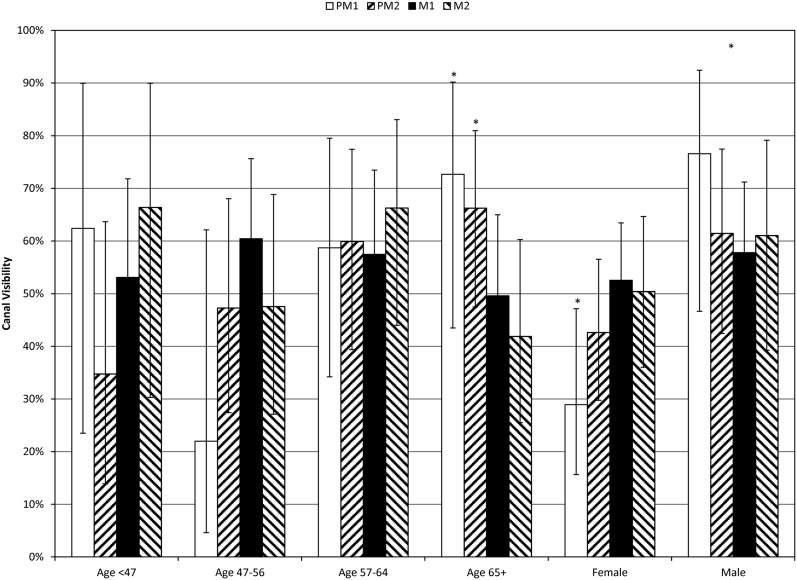
The three-way interaction between sex, age and location and the two-way interaction between age and sex were not statistically significant and were removed from the model. Age had a significant effect on MC visibility, but it differed by location (Figure 4): for PM1, age 47–56 had lower visibility than age 65+ (p = 0.0377), with no other significant differences found among ages. Gender also had a significant effect on canal visibility, where females had lower visibility than males overall (p = 0.0178) and the most pronounced difference for PM1 (p = 0.0054). Location had a significant effect on visibility, but it differed by age and by gender: for age 65+, M2 had lower visibility than PM1 (p = 0.0411) and PM2 (p = 0.0180), while for females, PM1 had lower visibility than M1 (p = 0.0123) and M2 (p = 0.0419).
Figure 4.
Canal visibility (%) by age and location, with 95% confidence interval. Significant visibility differences were found: female < male, PM1, age 47–56 < PM1 age 65+, M2 age 65+ < PM1 age 65 + and PM2 age 65+, (p = 0.0180); female PM1 < female M1 and female M2. M1, first molar; M2, second molar; PM1, first premolar; PM2, second premolar.
Discussion
It is essential to evaluate existing bone volume as part of treatment planning for dental implant placement. CBCT imaging offers many advantages in helping to evaluate bone volume, including visualization of important vital anatomical structures such as the MC. This study evaluated 360 deidentified CBCT cross-sectional images from 143 subjects by a board-certified oral and maxillofacial radiologist, a board-certified periodontist and a periodontics resident. The aims of the present study were to provide insight into the frequency at which MC can clearly be identified in a CBCT scan and if the age or sex of the person as well as the location of interest affects the visibility of the MC. Previous studies have evaluated the visibility of the MC in both conventional and computed radiography, with varied results.10,33
Angelopoulos et al10 compared digital and conventional panoramic radiographs and CBCT-reformatted panoramic images in the visibility of the MC in various regions of the mandible. CBCT imaging was found superior to the other modalities for evaluating visibility of the MC, despite the location. The most distal third of the MC was best visualized on all tested modalities, followed by the middle third and anterior third. The MC visibility was not assessed for an association with the age and sex of the subjects. The authors did not specify the percentage of sites where the MC was identifiable or not.
Oliveira-Santos et al33 evaluated hemimandibles cross-sectional images taken using a similar CBCT imaging system as used in this study. The visibility of the MC was registered as either positive or negative in six regions posterior to the mental foramen by an experienced maxillofacial radiologist. The scores of the regions were then grouped together so that each hemimandible received an overall visibility score: E (easy identification of the MC—5 or 6 positive scores), D (difficult identification—3 or 4 positive scores) and VD (very difficult identification—0–2 positive scores). The authors reported that the MC was easily visible in 53% of the hemimandibles assessed. Positive identification of the MC was 65% (131/202) for dentate regions and 68% (179/262) for edentulous regions. It was also determined that the visibility of the MC at the most distal sites was greater when compared with sites near the mental foramen (similar to Angelopoulos et al10), but the associations of age and gender with MC visibility were not evaluated. The MC visibility reported in this study is similar to what was determined by Oliveira-Santos and colleagues for hemimandibles but less than what they identified for dentate and edentulous individual regions/sites.
In this study, age had a significant effect on canal visibility, but it differed by location: for PM1, age 47–56 had lower visibility than age 65+ (p = 0.0377), with no other significant differences found among ages. Furthermore, this study did not assess any sites distal to M2, as these would not normally be sites evaluated for implant placement. In both Oliveira-Santos et al33 and Angelopoulos et al10 reports, study sites included areas distal to the M2, and only the mean ages of the subjects were reported.
Waltrick et al35 verified the accuracy of linear measurements and analysed the visibility of the MC on CBCT images obtained using different voxel sizes on dry hemimandibles. The authors grouped the results as completely, partially, slightly or not visible in second premolar, first molar and second molar locations. The MC was visualized in all of the 108 images evaluated with voxel size of 0.2 mm providing the best resolution for a completely visible canal. As voxel size increased, the MC became generally less visible. In this study, all images were taken with a voxel size of 0.3 mm, which may account for some of the discrepancies in MC identification with the study by Waltrick et al.35 The previous study used dry human hemi-mandibles from an anatomy department collection compared with our study performed on living subjects. The dry mandibles were devoid of overlying soft tissue structures and bodily fluids contained in living tissues. The MC in dry specimens would be air filled and more radiolucent, making the canal more visible compared with living subjects with mandibular canals filled with neurovascular contents.
In the present study, location had a significant effect on visibility, but it differed by age and by gender: for age 65+, M2 had lower visibility than PM1 (p = 0.0411) and PM2 (p = 0.0180), while for females, PM1 had lower visibility than M1 (p = 0.0123) and M2 (p = 0.0419). It has been found that the MC in the posterior mandible normally creates a depression in the lingual cortical plate, which probably explains the better depiction of the posterior portion of the MC on radiographs.36 Many of the previous referenced studies found the best resolution of the MC in sites distal to the third molars, but no sites distal to second molars were evaluated in this study. Overall, however, we did not find that MC identification improved as one progressed more posteriorly.
The test sites in this study were reviewed by each examiner only once and are a limitation of the study. The board-certified radiologist found the MC to be visible in 52% of the sections, and the board-certified periodontist found the MC to be visible in 54% of the sections. The periodontics resident found the MC to be visible in 56% of the sections. It is possible that the MC visibility could have been different if multiple evaluations had been performed. Although all three evaluators found 50–55% of the MC to be visible, there was disagreement about which canals were visible as reflected by an ICC of 0.53. One explanation for this ICC is that most disagreement occurred in the images when the MC was marginally identifiable. One examiner may have scored the canal as present while other examiner(s) may have scored the MC as absent. However, the variability among the examiners was incorporated in the comparisons of age, sex and location; so, the analyses and conclusions from that aspect of the study are actually more robust than if based on the results on the data from a single evaluator. In addition, only single slices from the CBCT image were evaluated. In actual practice, clinicians typically scroll through multiple sections anterior and/or posterior to the planned implant site to better trace the path of the MC when identification of the MC in a particular single section is difficult.
It is important to visualize the MC in cross-sectional CBCT images for implant planning. Moreover, having this knowledge aids clinicians in making better evidence-based decisions with regards to prescribing imaging studies for patients and minimizing the radiation dose whenever possible while getting the essential information from the proper imaging modality. Identification of the MC in 56% of the CBCT cross-sectional images is similar to results reported in previous studies. Although CBCT imaging is a valuable asset in the assessment of sites for implant placement, it is unable to consistently provide visualization and identification of the MC in all instances, and careful evaluation of the implant site is necessary to avoid impingement or violation of vital structures. The conclusion of this retrospective study was that the MC was identified in just over half of the time in selected, single CBCT cross-sectional images. Age, gender and location had significant effects on the visibility of the MC. CBCT cross-sectional imaging is a valuable tool for identification of vital anatomic structures as part of treatment planning but is not without limitations for identification of all anatomic structures.
Contributor Information
Mahogany S Miles, Email: drmahoganymiles.perio@gmail.com.
Edwin T Parks, Email: edparks@iu.edu.
George J Eckert, Email: geckert@iu.edu.
Steven B Blanchard, Email: stblanch@iu.edu.
References
- 1.Beltrán-Aguilar ED, Barker L, Canto MT, Dye BA, Gooch BF, Griffin SO, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis–United States, 1988–1994 and 1999–2002. MMWR Surveill Summ 2005; 54: 1–43. [PubMed] [Google Scholar]
- 2.Oliver RC, Brown LJ. Periodontal diseases and tooth loss. Periodontol 2000 1993; 2: 117–27. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (1999). Total tooth loss among persons aged >or = 65 years selected states, 1995–1997. MMWR Morb Mortal Wkly Rep 1993; 48: 206–10. [PubMed] [Google Scholar]
- 4.Kida IA, Astrøm AN, Strand GV, Masalu JR. Clinical and socio-behavioral correlates of tooth loss: a study of older adults in Tanzania. BMC Oral Health 2006; 6: 5. doi: 10.1186/1472-6831-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jemt T, Lekholm U, Adell R. Osseointegrated implants in the treatment of partially edentulous patients: a preliminary study on 876 consecutively placed fixtures. Int J Oral Maxillofac Implants 1989; 4: 211–17. [PubMed] [Google Scholar]
- 6.Pjetursson BE, Tan K, Lang NP, Bragger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res 2004; 15: 625–42. doi: 10.1111/j.1600-0501.2004.01117.x [DOI] [PubMed] [Google Scholar]
- 7.Tan K, Pjetursson BE, Lang NP, Chan ES. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res 2004; 15: 654–66. doi: 10.1111/j.1600-0501.2004.01119.x [DOI] [PubMed] [Google Scholar]
- 8.Juodzbalys G, Wang H, Sabalys G. Anatomy of mandibular vital structures. Part I: mandibular canal and inferior alveolar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res 2010; 1: e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kilic C, Kamburoglu K, Ozen T, Balcioglu HA, Kurt B, Kutoglu T, et al. The position of the mandibular canal and histologic feature of the inferior alveolar nerve. Clin Anat 2010; 23: 34–42. doi: 10.1002/ca.20889 [DOI] [PubMed] [Google Scholar]
- 10.Angelopoulos C, Thomas SL, Hechler S, Parissis N, Hlavacek M. Comparison between digital panoramic radiography and cone-beam computed tomography for the identification of the mandibular canal as part of presurgical dental implant assessment. J Oral Maxillofac Surg 2008; 66: 2130–5. doi: 10.1016/j.joms.2008.06.021 [DOI] [PubMed] [Google Scholar]
- 11.Lindh C, Petersson A. Radiologic examination for location of the mandibular canal: a comparison between panoramic radiography and conventional tomography. Int J Oral Maxillofac Implants 1989; 4: 249–53. [PubMed] [Google Scholar]
- 12.Lou L, Lagravere MO, Compton S, Major PW, Flores-Mir C. Accuracy of measurements and reliability of landmark identification with computed tomography (CT) techniques in the maxillofacial area: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 402–11. doi: 10.1016/j.tripleo.2006.07.015 [DOI] [PubMed] [Google Scholar]
- 13.Naitoh M, Katsumata A, Kubota Y, Hayashi M, Ariji E. Relationship between cancellous bone density and mandibular canal depiction. Implant Dent 2009; 18: 112–18. doi: 10.1097/ID.0b013e318198da7e [DOI] [PubMed] [Google Scholar]
- 14.Lofthag-Hansen S, Gröndahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res 2009; 11: 246–55. doi: 10.1111/j.1708-8208.2008.00114.x [DOI] [PubMed] [Google Scholar]
- 15.Hatcher DC, Dial C, Mayorga C. Cone beam CT for pre-surgical assessment of implant sites. J Calif Dent Assoc 2003; 31: 825–33. [PubMed] [Google Scholar]
- 16.Mupparapu M, Singer SR. Implant imaging for the dentist. J Can Dent Assoc 2004; 70: 32. [PubMed] [Google Scholar]
- 17.Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 817–26. doi: 10.1016/j.oooo.2012.03.005 [DOI] [PubMed] [Google Scholar]
- 18.Perez LA, Brooks SL, Wang HL, Eber RM. Comparison of linear tomography and direct ridge mapping for the determination of edentulous ridge dimensions in human cadavers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 748–54. doi: 10.1016/j.tripleo.2004.10.023 [DOI] [PubMed] [Google Scholar]
- 19.Kassebaum DK, Nummikoski PV, Triplett RG, Langlais RP. Cross-sectional radiography for implant site assessment. Oral Surg Oral Med Oral Pathol 1990; 70: 674–8. doi: 10.1016/0030-4220(90)90421-N [DOI] [PubMed] [Google Scholar]
- 20.Seeram E. Computed tomography: physical principles, clinical applications, and quality control. 3rd edn. St. Louis, MO: Saunders Elsevier; 2009. pp. 196. [Google Scholar]
- 21.Benavides E, Rios HF, Ganz SD, An CH, Resnik R, Reardon GT, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent 2012; 21: 78–86. doi: 10.1097/ID.0b013e31824885b5 [DOI] [PubMed] [Google Scholar]
- 22.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT). Part I: on subjective image quality. Eur J Radiol 2010; 75: 265–9. doi: 10.1016/j.ejrad.2009.03.042 [DOI] [PubMed] [Google Scholar]
- 23.Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 2012; 81: 267–71. doi: 10.1016/j.ejrad.2010.11.028 [DOI] [PubMed] [Google Scholar]
- 24.Hatcher DC. Operational principles for cone-beam computed tomography. J Am Dent Assoc 2010; 141(Suppl. 3): 3S–6S. [DOI] [PubMed] [Google Scholar]
- 25.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006; 35: 219–26. doi: 10.1259/dmfr/14340323 [DOI] [PubMed] [Google Scholar]
- 26.Mengel R, Kruse B, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of peri-implant defects: an in vitro study on native pig mandibles. J Periodontol 2006; 77: 1234–41. doi: 10.1902/jop.2006.050424 [DOI] [PubMed] [Google Scholar]
- 27.Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e25–31. doi: 10.1016/j.tripleo.2009.08.027 [DOI] [PubMed] [Google Scholar]
- 28.Makris N, Stamatakis H, Syriopoulos K, Tsiklakis K, van der Stel PF. Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using cone-beam computed tomography. Clin Oral Implants Res 2010; 21: 766–71. doi: 10.1111/j.1600-0501.2009.01903.x [DOI] [PubMed] [Google Scholar]
- 29.Nakagawa Y, Kobayashi K, Ishii H, Mishima A, Ishii H, Asada K, et al. Preoperative application of limited cone beam computerized tomography as an assessment tool before minor oral surgery. Int J Oral Maxillofac Surg 2002; 31: 322–6. doi: 10.1054/ijom.2001.0222 [DOI] [PubMed] [Google Scholar]
- 30.Ito K, Gomi Y, Sato S, Arai Y, Shinoda K. Clinical application of a new compact CT system to assess 3-D images for the preoperative treatment planning of implants in the posterior mandible. A case report. Clin Oral Implants Res 2001; 12: 539–42. doi: 10.1034/j.1600-0501.2001.120516.x [DOI] [PubMed] [Google Scholar]
- 31.Kamburoğlu K, Kiliç C, Ozen T, Yüksel SP. Measurements of mandibular canal region obtained by cone-beam computed tomography: a cadaveric study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: e34–42. [DOI] [PubMed] [Google Scholar]
- 32.Jung YH, Cho BH. Radiographic evaluation of the course and visibility of the mandibular canal. Imaging Sci Dent 2014; 44: 273–8. doi: 10.5624/isd.2014.44.4.273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oliveira-Santos C, Capelozza AL, Dezzoti MS, Fischer CM, Poleti ML, Rubira-Bullen IR. Visibility of the mandibular canal on CBCT cross-sectional images. J Appl Oral Sci 2011; 19: 240–3. doi: 10.1590/S1678-77572011000300011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson LC, Kosinski TF, Mentag PJ. A review of the intraosseous course of the nerves of the mandible. J Oral Implantol 1991; 17: 394–403. [PubMed] [Google Scholar]
- 35.Waltrick KB, Nunes de Abreu Junior MJ, Corrêa M, Zastrow MD, Dutra VD. Accuracy of linear measurements and visibility of the mandibular canal of cone-beam computed tomography images with different voxel sizes: an in vitro study. J Periodontol 2013; 84: 68–77. doi: 10.1902/jop.2012.110524 [DOI] [PubMed] [Google Scholar]
- 36.Gowgiel JM. The position and course of the mandibular canal. J Oral Implantol 1992; 18: 383–5. [PubMed] [Google Scholar]