Abstract
Background:
Agitation is an array of syndromes and types of behaviors that are common in patients with psychiatric disorders. In Europe, the estimation of prevalence of agitation has been difficult due to the lack of standard studies or systematic data collection done on this syndrome.
Objective:
An observational, cross-sectional, multicenter study aimed to assess the prevalence of agitation episodes in psychiatric emergencies in different European countries.
Method:
For 1 week, all episodes of acute agitation that were attended to at the psychiatric emergency room (ER) or Acute Inpatient Unit (AIU) in the 27 participating centers were registered. The clinical characteristics and management of the agitation episode were also described. A descriptive analysis was performed.
Results:
A total of 334 agitation episodes out of 7295 psychiatric emergencies were recorded, giving a prevalence rate of 4.6% (95% CI: 4.12-5.08). Of them, 172 [9.4% (95% CI: 8.2-10.9)] were attended at the ER and 162 [2.8% (95% CI: 2.4-3.3)] at AIU. Only data from 165 episodes of agitation (those with a signed informed consent form) was registered and described in this report. The most common psychiatric conditions associated with agitation were schizophrenia, bipolar disorder and personality disorder. The management of agitation included from non-invasive to more coercive measures (mechanical, physical restraint or seclusion) that were unavoidable in more than half of the agitation episodes (59.5%).
Conclusion:
The results show that agitation is a common symptom in the clinical practice, both in emergency and inpatient psychiatric departments. Further studies are warranted to better recognize (using a standardized definition) and characterize agitation episodes.
Keywords: Agitation, Aggression, Bipolar disorder, Emergency, Epidemiology, Quality of care, Schizophrenia
INTRODUCTION
Agitation is an array of syndromes and behavior types that are common in patients with major psychiatric disorders, such as schizophrenia, schizoaffective disorder and the manic phase of bipolar disorder. There are several levels of agitation from mild to severe, with rapid fluctuations, which can further escalate to aggressive behavior in a relatively short period of time. Episodes of acute agitation usually require psychiatric emergency visits, admission to a psychiatric inpatient ward and continued hospitalization [1-4]. Agitation may be due to the natural course of the underlying disease or because of non-compliance with chronic medication. However, there are other contributing factors for agitated behavior in patients with underlying psychotic disorders which can either be present or not at each episode of acute agitation. Other conditions, such as substance use disorders or iatrogenic causes, may concur as well [5-7].
About 2 million emergency department visits per year may involve agitated patients in the United States (US), with schizophrenia or bipolar disorders as the underlying causes in 21% and 13% of these visits, respectively [2, 8-10]. Agitation was present in 52% of the patients treated at the psychiatric emergency services and specific anti-agitation medication was necessary in 47% of them to reduce agitation as observed in a retrospective review of 400 charts from 9 US centers by the Psychiatric Emergency Research Collaboration (PERC)-01. Likewise, 179 (45%) of the patients were admitted to an inpatient or observation unit [11].
In Europe, there are about 164.8 million adult patients affected with mental disorders [12]. Some of these patients, namely those with schizophrenia, bipolar disorder, personality disorder, general anxiety disorder, panic disorder or major depression diagnoses, may suffer from some type of agitation in their lifetime [10, 13, 14]. However, agitation is a heterogeneous concept present in multiple diagnostic areas in psychiatry and there is no uniformly accepted definition for it [13, 15]. At present, there is a lack of direct epidemiological studies assessing the prevalence, clinical impact, and short/ long time consequences of acute agitation. The estimation of prevalence of “agitation” is difficult due to the lack of standard studies or systematic data collection done on this syndrome, except for a few cross-sectional studies [16-21]. Existing data is derived from patients visiting emergency settings or admitted to Acute Inpatient Units (AIU), which differ in the populations analyzed, the rating scales used, or the organization of services.
The collaboration of the patient is essential for the clinical management of the episode of agitation associated with the psychiatric disorder [22]. Behavioral and psychological techniques (e.g. de-escalation, physical or mechanical restrains) and nonspecific sedating agents (benzodiazepines and/or antipsychotics) are used to calm the patient rapidly, allowing the collection of clinical history details and a risk evaluation of the patient [22, 23]. Early identification of milder forms of agitation and prompt management might prevent progression to more severe agitation and aggressive behavior.
Several consensus guidelines have been published to direct physicians in the management of agitation in the acute setting [3, 24], with the most recent being that of the American Association for Emergency Psychiatry (AAEP) which covers all interventional aspects on the evaluation and treatment of agitation and has improved the consistency and safety in the management of patients [25]. Recently, a panel of 24 international experts have published a consensus on the assessment and treatment decisions for psychiatric agitation has that provides some useful recommendations for daily clinical practice based on the current knowledge of agitation [26]. However, data on the epidemiology and management of acute agitation at the psychiatric emergency services in Europe is scarce, probably due to the lack of standard studies or systematic data collection.
This observational, cross-sectional, multicenter, international study (STAGE study) is aimed to assess the proportion of episodes of acute agitation that were attended to at the psychiatric emergency room (ER) from the total of psychiatric emergencies attended to in a week, and the proportion of acute agitation episodes that were seen to at the AIU from the total of beds occupied in a week, in patients with psychiatric disorders in several European countries. For the purpose of this study it was assumed that the sum of occupied daily beds in a week was a surrogate of total attended psychiatric cases in AIU. In addition, we aimed to describe the patient’s demographic and clinical characteristics (gender, age, underlying psychiatric disease, history of substance use, current antipsychotic treatment, or severity of agitation) as well as the assessment and management of the episode of agitation.
PATIENTS AND METHODS
Study Design
This was a prospective, observational, cross-sectional, non-interventional study conducted at 27 general hospitals from 6 European countries (Spain [n=15], Austria [n=1], Germany [n=3], Greece [n=2], Portugal [n=3] and Romania [n=3]). All of the centers had a psychiatric ER, a 24-hour available psychiatrist and an AIU for psychiatric hospitalization for acute agitation episodes.
The study was conducted after obtaining approval from the appropriate Institutional Ethics Committee and in accordance with the Declaration of Helsinki, Good Clinical Practices, and local ethical and legal requirements. All participants provided written informed consent to participate prior to the enrollment in the study. In case the patient was unable to provide consent due to an agitation episode, it was accepted to do so when he/she became competent.
Patient Eligibility
Consecutive patients, aged ≥18 and ≤ 65 years, with primary diagnosis of psychiatric disease, that were attended to for at least one episode of acute agitation at the psychiatric ER or AIU were included. Acute agitation episode was defined as “a state of motor restlessness accompanied by mental tension, which has the following core psychiatric signs: hostility, tension, excitement, uncooperativeness and impulsivity, that can result in uncontrolled behavior with self-inflicted injury, aggressiveness to others or threat of property damage [27]”.
Patients with an abstinence syndrome due to recognized substance dependence or with an agitation episode of organic origin or secondary to cranial-encephalic traumatism were excluded. As it was a non-interventional study all care provided to the patients was at the discretion of the participating physician.
Assessments
During 7 consecutive days (from Monday to Sunday) the investigators registered all episodes of acute agitation that met the inclusion criteria and were attended to in the psychiatric ER (number of episodes of agitation/number of total psychiatric emergencies) or in the AIU (number of episodes of agitation/number of beds occupied) at the participating centers. All episodes of agitation were registered even if a patient had suffered more than one episode during hospitalization.
The acute agitation episode was followed until the event resolved without further need of medical/psychiatric attention, or until the patient was discharged from the ER/AIU or was derived for inpatient admission due to a psychiatric diagnosis needing hospital care.
Data were obtained from patient`s clinical records including the demographic characteristics, underlying psychiatric disease, history of substance abuse, current antipsychotic treatment, therapies received at ER/ AIU, assessment of the episode of agitation at admission and at discharge from the ER/AIU, and patient satisfaction with the treatment received (de-escalation, pharmacological or other).
The agitation was assessed using the Excited Component of the Positive and Negative Syndrome (PANSS-EC) scale, the Clinical Global Impression-Severity (CGI-S) scale and the Clinical Global Impression-Global Improvement (CGI-I) scale. Patient satisfaction was measured through a 0-10 visual analogue scale (VAS).
Statistical Analysis
All of the episodes of agitation that met the selection criteria were taken into account for the analysis of the prevalence of agitation, while only the data collected from the patients that signed the informed consent form was analyzed for the description of the episodes. A descriptive analysis was performed. Median values were used instead of means when data were not normally distributed. Confidence intervals were calculated based on a binomial distribution. Multiple comparison for non-normal distributed variables were compared pair wise by Mann-Whitney U test and p-values corrected by Benjamini & Hochberg method [28]. All statistical analyses were performed with R software (version 3.2.2).
RESULTS
Patients and Eligibility
During one week from March 10th to December 7th 2014, 334 episodes of agitation that met the selection criteria were identified from a total of 7295 psychiatric emergencies that were attended to at psychiatric ER or beds that were occupied at AIU in the participating centers. Assuming the sum of occupied daily beds in a week as a proxy of total attended psychiatric cases in AIU, the overall prevalence (ER + AIU) was 4.6% (95% CI: 4.12-5.08). By country, the number of episodes of agitation attended to was as follows: Spain (83 out of 3165; 2.6%), Germany (29 out of 935; 3.1%), Austria (36 out of 225, 16%), Portugal (65 out of 1466, 4.4%), Greece (6 out of 214, 2.8%) and Romania (115 out of 1290, 8.9%). More specifically, 172 [9.4% (95% CI: 8.2-10.9)] of the 1826 psychiatric emergencies attended to in the ER, and 162 [2.8% (95% CI: 2.4-3.3)] of the 5880 occupied beds at the AIU, were due to an episode of acute agitation.
Despite having 334 episodes that met the selection criteria, a signed informed consent form was obtained in only 165 episodes. Thus, 165 episodes of acute agitation requiring psychiatric care (67 at the ER and 98 at the AIU) were included in the descriptive analyses. All episodes were attended to by a psychiatrist.
A higher proportion of episodes (63.0%) were reported by male patients. Median age of participants was 41 (range: 18-65) years. In half (50.3%; n=83) of the episodes the patient had a primary diagnosis of schizophrenia, and in almost a quarter (24.2%; n=40) the patient had a bipolar disorder diagnosis. Both disorders generally presented as a single diagnosis in the majority of patients. Other prevalent primary psychiatric disorders were personality disorders (n=24; 14.5%) and substance use disorders (n=27; 16.4%). Particularly, substance use disorder rarely presented as a single disorder in one episode, and was commonly associated with other psychiatric diagnoses (dual disease). Other psychiatric diagnoses were present in 45 (27.3%) episodes of agitation, including autism, mental retardation, affective disorder or anorexia,.
In one third (32.7%) of the episodes the patient reported alcohol consumption, tobacco smoking in almost half (49.7%), and cannabis consumption in 12.7% of the episodes. Consumption of other drugs (e.g. cocaine or club drugs) was reported in <5% of the episodes. In most of the episodes (150/165; 90.9%), the patients stated that they had received prior psychoactive treatment, mainly consisting of antipsychotics (131/165; 79.4%), hypnosedatives (90/165; 54.5%), mood stabilizers (72/165; 43.6%) or antidepressants (55/165; 33.3%). No data was collected on patient`s adherence to treatment. Patient socio-demographic characteristics by clinical setting are summarized in Table 1.
Table 1. Socio-demographic and baseline characteristics by clinical setting (ER or AIU)ǂ.
| ER | AIU | |
|---|---|---|
| Total of episodes, (%) | 67 | 98 |
| Men (%) | 39 (58.2) | 65 (66.3) |
| Age (years), median (range) | 39.0 (23.0- 65.0) | 41.0 (18.0-65.0) |
|
Current diagnosis, n (%) Schizophrenia* single diagnosis Bipolar affective disorders* single diagnosis Personality disorder* single diagnosis Substance use disorder* single diagnosis Other (autism, mental retardation, affective disorder, anorexia, etc) Unknown |
25 (37.3) 22 (32.8) 19 (28.4) 12 (17.9) 15 (22.4) 8 (11.9) 11 (16.4) 0 23 (34.3) 3 (4.5) |
53 (54.1) 43 (43.9) 21 (21.4) 19 (19.4) 9 (9.2) 6 (6.1) 16 (16.3) 4 (4.1) 22 (22.4) 4 (4.1) |
|
Psychoactive treatment Antipsychotics Mood stabilizers Hypnosedatives Antidepressants |
58 (86.6) 44 (65.7) 23 (34.3) 37 (55.2) 23 (34.3) |
92 (93.9) 87 (88.8) 49 (50.0) 53 (54.1) 32 (32.7) |
|
Drug consumption reported by patient, n (%) Alcohol Tobacco Cannabis Cocaine Club drugs (LSD, ketamine, etc) Other drugs (amphetamines, opioids, etc) |
24 (35.8) 34 (50.7) 11 (16.4) 2 (3.0) 4 (6.0) 3 (4.5) |
30 (30.6) 48 (49.0) 10 (10.2) 6 (6.1) 0 4 (4.1) |
|
Onset of agitation episode, n (%) Morning shift (≥8- < 16 h) Afternoon shift (≥16 - < 24 h) Evening shift (≥0 - < 8 h) |
34 (50.7%) 23 (34.3%) 10 (14.9%) |
60 (61.2%) 27 (27.6%) 11 (11.2%) |
| Hours duration episode, median (range) | 3.18 (0.42, 51.0) | 1.62 (0.25, 110) |
ǂ Data from the 165 episodes of acute agitation that were reported by the patients signing the informed consent form. *As single diagnosis or combined with other disorders; ER: Emergency Room; AIU: Acute Inpatient Unit
Characteristics of the Episode of Agitation: Onset, Intensity, Duration, Psychiatric Diagnosis
The onset of agitation was considered from the first documentation of agitated behavior by the clinician. The onset of the agitation episode was more frequent during the morning (between 8 am and 16 pm; n= 94; 57.0%) than in the evening (between 16 - 24 pm; n= 50; 30.3%). Overall, the occurrence of agitation episodes was slightly higher on Mondays (35/165; 21.2%) than the rest of the week (between 10-15% each day from Tuesday to Sunday). The busiest day at the AIU was Monday (24/98; 24.5%) but it was Friday at the ER (14/67; 20.9%). The median duration of the onset of agitation was 2 (0.25-110) hours (Table 1).
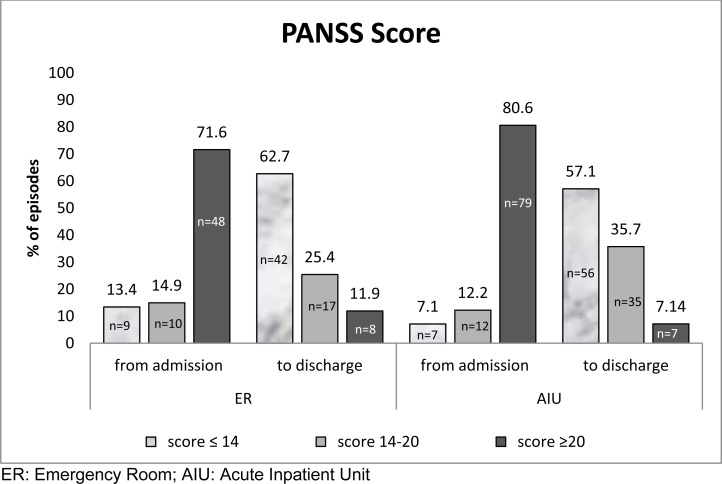
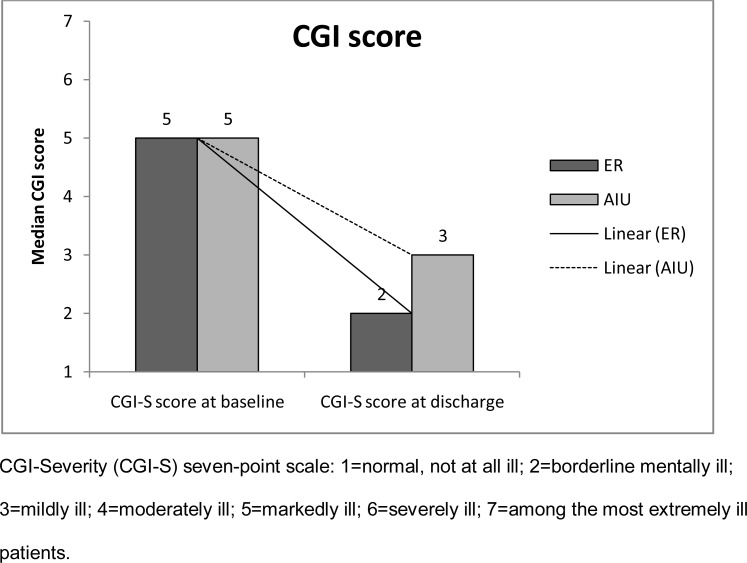
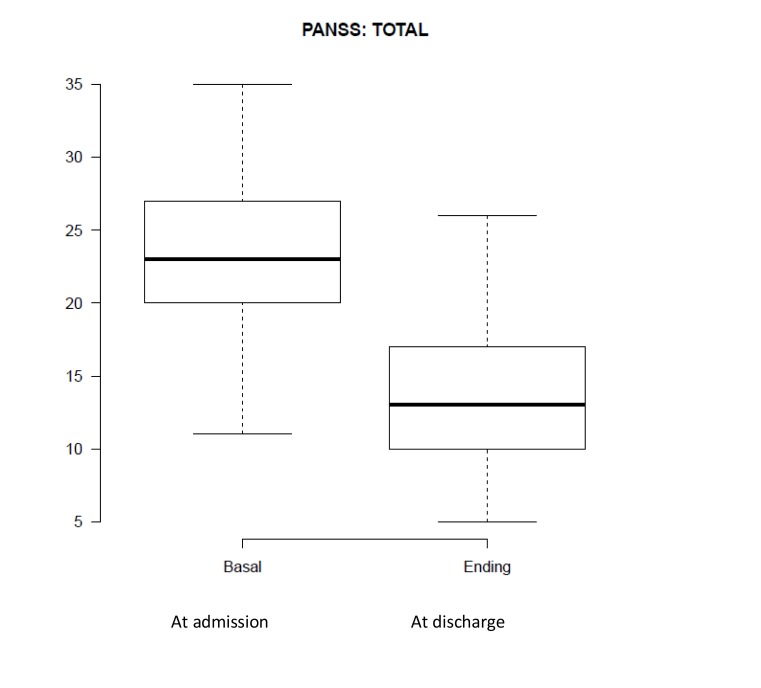
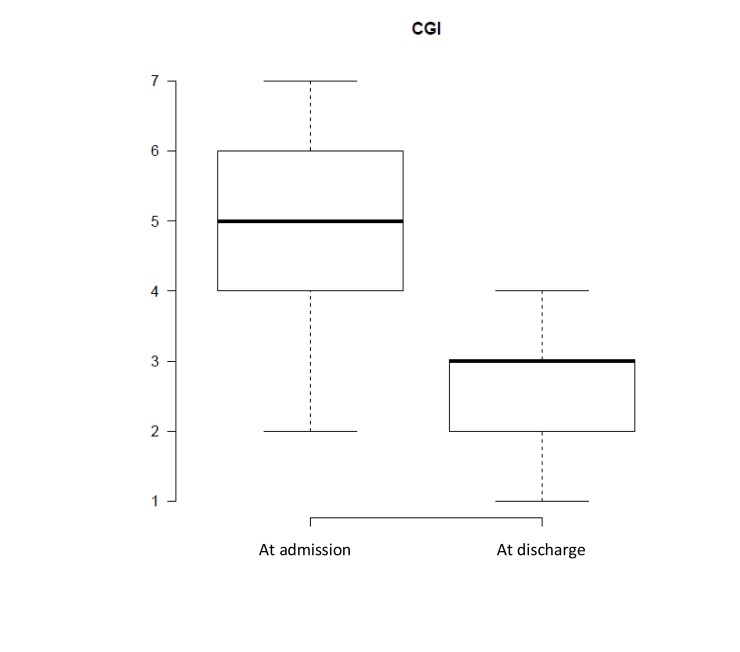
At admission, the median baseline score was 5 according to CGI-S (range: 2 - 7) and 23 (range: 11 - 35) according to PANSS-EC assessment. At admission, the patients presented a score ≥20 points as per PANSS-EC in a high proportion of episodes (77%; 127/165), while in a 13.3% (22/165) of episodes the score was >14 and <20 and in a 9.7% (16/165) of episodes was ≤14 points. Figs. (1 and 2) depicts clinical improvement from admission to discharge at ER and AIU according to PANSS and CGI-S scales, respectively.
Fig. (1).
Severity of agitation according to PANSS-EC Score from admission to discharge at ER and AIU.
Fig. (2).
CGI-S score change from admission to discharge at ER and AIU.
Figs. (3 and 4) present the clinical study results in the 5 PANSS-EC and CGI-S scales, respectively.
Fig. (3).
Severity of agitation according to PANSS-EC.
Fig. (4).
Severity of agitation according to CGI scale.
There were no notable differences in the severity of agitation between episodes attended to at the emergency unit or at AIU. Patient clinical characteristics are summarized by clinical setting in Table 1.
Therapeutic Management Strategies (Pharmacological and Non-pharmacological)
The management of the episodes ranged from non-invasive to more coercive measures such as physical or mechanical restraint or seclusion, that were unavoidable in 25 (15.2%), 44 (26.7%) and 29 (17.6%) episodes, and had a median duration of 10 (range: 5 - 130), 210 (range: 0 - 2400) and 150 (range: 20 - 4320) minutes, respectively. Verbal de-escalation was employed in 139 (84.2%) episodes for a median of 30 minutes (range: 5 - 620).
Benzodiazepines (n=86; 52.1%) were used in over half of the episodes, and first- (n=53; 32.1%) or second-generation (n=51; 30.9%) antipsychotics were used in nearly one third. A combination of these drugs (benzodiazepines + antipsychotics) was used in 39 (58.2%) of the episodes at the ER and in 27 (27.6%) of the episodes at the AIU.
Table 2 summarizes management of agitation episode by clinical setting.
Table 2. Management of agitation episode by clinical setting (ER or AIU)ǂ.
| ER | AIU | |
|---|---|---|
| Total, N | 67 | 98 |
|
Non-pharmacological, n (%) Verbal de-escalation Physical restrains Mechanical restrains Isolation/seclusion |
58 (86.6) 14 (20.9) 19 (28.4) 17 (25.4) |
81 (82.7) 11 (11.2) 25 (25.5) 12 (12.2) |
|
Time employed, median minutes (max, min) Verbal de-escalation Physical restrains Mechanical restrains Isolation/seclusion |
30.0 (5-600) 12.5 (5-30) 150 (0-2400) 150 (20-4320) |
25.0 (5-620) 10.0 (5-130) 265 (10-1055) 155 (30-885) |
|
Pharmacological First generation antipsychotics Second generation antipsychotics Benzodiazepines |
27 (40.3) 22 (32.8) 38 (56.7) |
26 (26.5) 29 (29.6) 48 (49.0) |
ǂ Data from the 165 episodes of acute agitation that were reported by the patients signing the informed consent form.
ER: Emergency Room; AIU: Acute Inpatient Unit
Patient Satisfaction
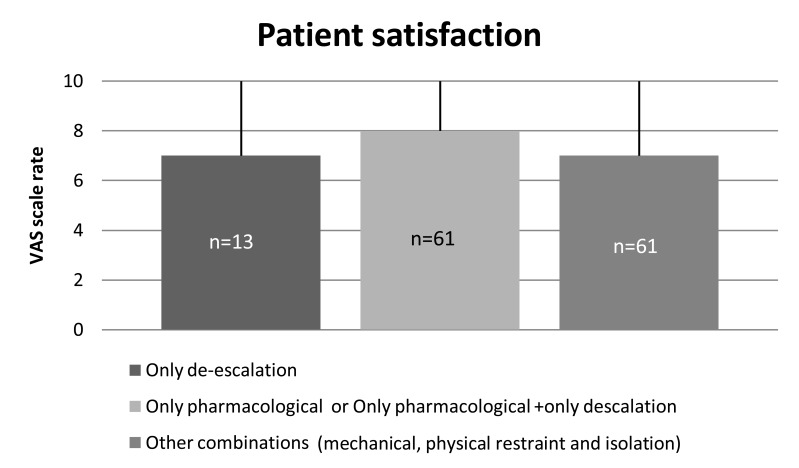
One hundred and thirty-five patients rated their satisfaction for the medical care received (“only de-escalation” vs. “only pharmacological or pharmacological + only de-escalation” vs. “other combinations” that could include mechanical, physical restraint and/or seclusion) on a VAS. Median satisfaction score was 7 (range: 0-10). Differences in the rating of satisfaction obtained among the medical care options did not reach statistical significance (p=0.068) (Fig. 5).
Fig. (5).
Patient satisfaction with treatment.
DISCUSSION
To our knowledge, this is the first epidemiological study to estimate the prevalence of acute agitation in the emergency services (ER and AIU) from the total psychiatric emergencies attended to in a population of patients with primary psychiatric disorder in Europe. Nearly 5 out of every 100 emergencies attended to at the ER and AIU services in a week were due to an acute agitation episode. Particularly, acute agitation constituted 9.4% of all the emergencies attended at the ER and 2.8% of the beds occupied in the AIU in a week.
Unlike previous studies, we used a standard definition for agitation as recommended by Batagglia et al. [27] which confers consistency and uniformity of results across the different centers and countries. A period of one week was chosen to measure prevalence of agitation because it provides an idea of the circadian prevalence of agitation. Since prevalence of agitation may vary from week to week and month to month, each site was able to select the most suitable week for data collection so different periods of time were covered to assess such prevalence globally.
The results from the descriptive analysis of our study population provide a good picture of the burden of acute agitation for the emergency services. About 50% of the patients attending the emergency services for acute agitation were male patients (63.0%), with a median age of 41 years, and a primary diagnosis of schizophrenia (46.7%). Almost a quarter (24.2%; 40 patients) had bipolar disorder. One out of three patients in our study had a history of alcohol consumption and one out of six reported cannabis consumption. Moreover, a substance use disorder was associated with the underlying psychiatric diagnosis in around 16% of the agitation episodes (Table 1). Similar findings have been reported by other authors, which observed that psychotic pathology (70%) and bipolar disorders (13%) were the most prevalent diagnostics that are associated with agitation attended to at the emergency services, and there is a substance intoxication cause involved in about 15-20% of the episodes [18, 29]. Curran et al. observed increased visits to ER in patients with schizophrenia presenting certain comorbid disorders such as substance use disorders [30].
In our study we observed a high percentage (77%) of severe agitation episodes, with over 50% of agitations needing physical restraint, which can reflect the likelihood of missed lower-acuity episodes. Probably there was an inconsistent selection of candidates between screeners and a significant number of patients were excluded because they didn’t seem to be clearly ‘agitated’ to the screeners. Possible reasons for these result might be the absence of previous training in the PANSS-EC scale, the different criteria used for identifying “agitated patients” through the variety of countries included, or the choice of the Battaglia’s definition for agitation which might not be the most appropriate. These numbers may not reflect the real numbers of agitation in the ERs and AUIs and constitute a limitation for generalizing the results of our study. However, this fact reflects the difficulty to perform adequate epidemiological studies and opens important questions regarding the identification and management of agitation.
The assessment of the severity of agitation at the earliest possible point in time may help identify patients at acute risk and suggest effective treatment interventions. Depending on their severity, the agitation episodes may escalate unpredictably to aggressive behavior, needing to apply non-coercive measures such as first verbal de-escalation and/or oral medication or more coercive/restraint measures in the late phases. The majority of patients need medication that calms them without inducing sleep [31] and targets towards the underlying pathology. In about 91% of the agitation episodes attended to in our study the patients were receiving treatment for their baseline psychiatric disorder, the onset of acute agitation was mainly during the morning and the occurrence was slightly higher after the weekend. These might reflect bad compliance with the psychotropic treatment, but it can also result from the intermittent nature of the agitated behavior despite receiving adequate treatment for the primary psychiatric condition. A rapid, effective and safe intervention is essential to return the agitated person to a less agitated state. The Expert Consensus Guidelines for Treatment of Behavioral Emergencies recommend to consider the speed of onset when choosing a route of administration [32]. The guidelines also recommend treating the underlying cause instead of simply medicating with antipsychotics or benzodiazepines, except when they are used for rapid tranquilization. Considering that the majority of patients had underlying schizophrenia or bipolar disorders, it seems that, in our study, benzodiazepines were frequently used (in over half of the episodes) probably seeking the patient’s sedation. Perhaps hospital practice guidelines might be revised to adjust to the AAEP guidelines as much as possible. In addition, they should consider the results from recent clinical trials with new inhaled formulations that have demonstrated significant reductions in agitation two hours after the patients had received a dose and without inducing significant sedation [22]. The recently published expert consensus recommendations are in line with this and advocate for oral or inhaled formulations over intramuscular routes in mildly agitated patients [26].
The use of more invasive measures, such as mechanical, physical restraint or seclusion was necessary in 26.7%, 15.2%, and 17.6% of the patients, respectively in our study. Similar rates have been reported for Spain by other authors with 25.7% and 39% of patients requiring mechanical [18] or physical restraints [33], respectively. Restrain and seclusion is in some episodes unavoidable, and the use of physical restrain alone or in combination with pharmacotherapy is still used by about 30% of the emergency departments [34]. To mitigate some of the negative consequences derived from the use of restrain and seclusion, the AAEP has provided consensus guidelines [35]. Coercive measures might be necessary to relieve the individual’s distress and to protect care providers and others in close proximity, but they have raised much controversy about their long-term effectiveness and safety implications, as well as concerns about the significant staff involvement that these measures require [25]. Katsakou et al. observed that among involuntary patients it was important to diminish the patient’s perceived coercion at admission to increase their satisfaction with overall treatment [36]. In this sense, to avoid the restrain process the AAEP consensus guidelines promote the early use of de-escalation techniques as well [37]. In our study, verbal de-escalation was employed in 84.2% of the agitation episodes and for a median of 30 minutes, and patient satisfaction with treatment was the highest when de-escalation and pharmacological treatment options were used.
Noteworthy, in our study the median satisfaction score was 7 (range: 0-10), which represent a good feedback of the patients reading the clinical attendance. This important point is found in very few published studies, even though patient preference should always be taken into account in the decision of the management and treatment of patients. Therefore, improvements in health care attention can increase the quality of life of the patients.
The aim of the study was to obtain comprehensive information on the prevalence and to include different countries with different geographical and cultural characteristics. As a result, the number of centers per country included in the study was not well-balanced, which constitutes a limitation of the study. The majority of the agitation episodes and centers came from Spain, Romania or Portugal. For Spain, the good size of the sample analyzed (83 agitation episodes attended) and the diversity of centers included (15 centers), together with the uniformity (that is inherent to the Spanish health care system) regarding the procedures for assessment and management at the psychiatric emergency services confer representativeness and robustness to the results. Despite the limitations intrinsic to the different sample sizes or methodology used in these studies, the results are in line with the limited data published in Spain. Particularly, some naturalistic studies have described the daily clinical practice at a psychiatric ER in Spain. Pascual et al. described 100 patients from one center [33], San et al. [38] reported the results from 92 patients attending psychiatric ER at several centers and Escobar et al. from 278 patients from 16 centers in Spain [18]. Similarly to our findings, around half of the patients attending the psychiatric ER were psychotic patients and presented a moderate to severe disease according to PANSS-EC. Other studies have assessed only bipolar disorder [19] with similar results. Romania and Portugal were also highly represented with 115 and 65 episodes of agitation recorded in 3 centers each and, as far as we know, our study provides the first epidemiological data for acute agitation in these two countries. The other participating countries (Germany, Austria, and Greece) were poorly represented. There are similar findings from these countries in the literature but there are substantial differences between the emergency national health systems of each country which make the comparison difficult [21, 39].
CONCLUSION
The results of our study reveal that acute agitation is a frequent symptom in patients with underlying primary psychiatric diagnosis and a main reason for attending the health services in terms of use of primary emergency services, such as ER and AIU. Patient`s characteristics are similar to previous studies in other countries and management for acute agitation seem to follow the current consensus guidelines published. Unfortunately, the information on demographic and clinical characteristics was recorded from only 165 out of the 334 episodes that met the selection criteria for agitation, which constitutes a limitation of our study and decreases the external validity of the study. In addition, the overall prevalence of agitation in emergency settings might be higher than our results have reflected, due to a possible selection bias that have overlooked milder agitation episodes and that preclude to generalize our results. More extensive training on early identification and management of agitation is warranted to better recognize (using a standardized definition) and characterize agitation episodes in the population of patients attending emergency and inpatient psychiatric departments. Further investigations should be done through like-wise studies at a larger scale to obtain more accurate data on the prevalence of agitation episodes and to optimize the use of healthcare resources.
TRIAL REGISTRATION
This is not a controlled trial.
ACKNOWLEDGEMENTS
The physicians listed below cared for the patients in this study. The authors thank them for their cooperation and support:
Dr. Maria Rocío Martín-Santos. Hospital Clínic de Barcelona (Barcelona-Spain); Dr. Isabel Flórez Fernández. Hospital Univ.Son Espases (Palma de Mallorca-Spain); Dr. Lorena García Fernández. Hospital Univ. Sant Joan d’Alacant (Alicante-Spain); Dr. Alfredo de la Rubia Martínez. Hospital de Mérida (Mérida-Spain); Dr. Juan Carlos Berenguer Reula. Hospital Ntra. Sra. de la Candelaria (Sta. Cruz de Tenerife-Spain); Dr. Fernando Uribe Ladrón de Cegama. Hospital Clínico Univ. de Valladolid (Valladolid-Spain); Dr. Mario Páramo Fernández. Hospital Provincial de Conxo (Santiago de Compostela - Spain); Dr. Jesús Artal Simón. Hospital Marqués de Valdecilla (Santander - Spain); Dr. Javier Correas Lauffer. Hospital Univ. del Henares (Coslada- Spain); Dr.Juan Luís Prados Ojeda. Hospital Univ. Reina Sofia (Córdoba - Spain); Dr. José Ignacio Eguiluz Urruchurtu. Hospital de Cruces (Barakaldo - Spain); Dr. Francisco C. Ruiz. Hospital San Telmo (Palencia - Spain); Dr. Jose Andres Martin Zurimendi. Hospital Galdakao (Bilbao - Spain); Dr. Maria Luisa Figueira. Hospital Santa María (Lisboa - Portugal); Dr. António Reis Marques. Hospital Universitario de Coimbra (Coimbra - Portugal); Dr. Johannes Thome. Klinik und Poliklinik für Psychiatrie und Psychotherapie der Universität Rostock (Rostock-Germany); Dr. Thomas Schömig Department of Psychiatry, Psychotherapy Asklepios Klinik Nord (Hamburg-Germany); Dr. Thomas Barth Klinik für Psychiatrie, Verhaltensmedizin und Psychosomatik (Chemnitz-Germany); Dr. Ursula Hämmerer Klinik für Psychiatrie, Verhaltensmedizin und Psychosomatik (Chemnitz-Germany); Dr. Michael Lehofer. Landeskrankenhaus Siegmund Freud Graz (Graz-Austria); Dr. Siegfried Kasper. Medical University of Vienna, Department of Psychiatry and Psychotherapy (Vienna-Austria); Clinical Division of Biological Psychiatry, Vienna General Hospital (Vienna-Austria); Dr Christian Geretsegger. University Clinic of Psychiatry and Psychotherapie of Salzburg (Salzburg-Austria); Dr. Aggelopoulos Ilias. University General Hospital of Athens "Eginitio" / A’ Psychiatric ward (Athens - Greece);Dr. Pitsa Theodoropoulou. General Hospital of Athens "Sismanoglio", Psychiatric clinic (Athens - Greece); Dr. Margarita Sestrini. General Hospital of Athens "Sismanoglio", Psychiatric clinic (Athens - Greece); Dr. Adela Ciobanu Psychiatric Clinical Hospital Dr. Al. Obregia. (Bucharest-Romania); Dr. Elena Dinu. Psychiatric Hospital Voila (Campina-Romania).
This study was founded by Ferrer International SA., Spain and performed with the services of the CRO ANAGRAM-ESIC. Writing assistance was provided by Ana Del Campo (Pivotal SL).
CONFLICT OF INTEREST
The authors declare the following conflicts of interest:
LS has been a consultant for, received grant/research support and honoraria, and been on the speakers/advisory board from Astra Zeneca, Bristol-Meyers Squibb, Eli Lilly, Ferrer, Janssen-Cilag, Lundbeck, Otsuka, Pfizer and Servier. He has obtained research funding from the Spanish Ministry of Health, the Spanish Ministry of Science and Education as well. AB is employee of Ferrer International SA. The other authors have indicated no potential conflict of interest.
REFERENCES
- 1.Allen M.H. Managing the agitated psychotic patient: a reappraisal of the evidence. J. Clin. Psychiatry. 2000;61(Suppl. 14):11–20. [PubMed] [Google Scholar]
- 2.Allen M.H., Currier G.W. Use of restraints and pharmacotherapy in academic psychiatric emergency services. Gen. Hosp. Psychiatry. 2004;26(1):42–49. doi: 10.1016/j.genhosppsych.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Allen M.H., Currier G.W., Carpenter D., Ross R.W., Docherty J.P. Expert Consensus Panel for Behavioral Emergencies 2005. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J. Psychiatr. Pract. 2005;11(Suppl. 1):5–108. doi: 10.1097/00131746-200511001-00002. [DOI] [PubMed] [Google Scholar]
- 4.De Fruyt J., Demyttenaere K. Rapid tranquilization: new approaches in the emergency treatment of behavioral disturbances. Eur. Psychiatry. 2004;19(5):243–249. doi: 10.1016/j.eurpsy.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Fiorentini A., Volonteri L.S., Dragogna F., Rovera C., Maffini M., Mauri M.C., Altamura C.A. Substance-induced psychoses: a critical review of the literature. Curr. Drug Abuse Rev. 2011;4(4):228–240. doi: 10.2174/1874473711104040228. [DOI] [PubMed] [Google Scholar]
- 6.Leventhal A.M., Zimmerman M. The relative roles of bipolar disorder and psychomotor agitation in substance dependence. Psychol. Addict. Behav. 2010;24(2):360–365. doi: 10.1037/a0019217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buckley P.F. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J. Clin. Psychiatry. 2006;67(Suppl. 7):5–9. doi: 10.4088/JCP.0706e01. [DOI] [PubMed] [Google Scholar]
- 8.Marco C.A., Vaughan J. Emergency management of agitation in schizophrenia. Am. J. Emerg. Med. 2005;23(6):767–776. doi: 10.1016/j.ajem.2005.02.050. [DOI] [PubMed] [Google Scholar]
- 9.Sankaranarayanan J., Puumala S.E. Epidemiology and characteristics of emergency departments visits by US adults with psychiatric disorder and antipsychotic mention from 2000 to 2004. Curr. Med. Res. Opin. 2007;23(6):1375–1385. doi: 10.1185/030079907X187900. [DOI] [PubMed] [Google Scholar]
- 10.Zeller S.L., Rhoades R.W. Systematic reviews of assessment measures and pharmacologic treatments for agitation. Clin. Ther. 2010;32(3):403–425. doi: 10.1016/j.clinthera.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Boudreaux E.D., Allen M.H., Claassen C., Currier G.W., Bertman L., Glick R., Park J., Feifel D., Camargo C.A., Jr, PERC The psychiatric emergency research collaboration-01: methods and results. Gen. Hosp. Psychiatry. 2009;31(6):515–522. doi: 10.1016/j.genhosppsych.2009.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wittchen H.U., Jacobi F., Rehm J., Gustavsson A., Svensson M., Jönsson B., Olesen J., Allgulander C., Alonso J., Faravelli C., Fratiglioni L., Jennum P., Lieb R., Maercker A., van Os J., Preisig M., Salvador-Carulla L., Simon R., Steinhausen H.C. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011;21(9):655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Pacciardi B., Mauri M., Cargioli C., Belli S., Cotugno B., Di Paolo L., Pini S. Issues in the management of acute agitation: how much current guidelines consider safety? Front. Psychiatry. 2013;4:26. doi: 10.3389/fpsyt.2013.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pascual J.C., Madre M., Soler J., Barrachina J., Campins M.J., Alvarez E., Pérez V. Injectable atypical antipsychotics for agitation in borderline personality disorder. Pharmacopsychiatry. 2006;39(3):117–118. doi: 10.1055/s-2006-941489. [DOI] [PubMed] [Google Scholar]
- 15.Mintzer J.E. Introduction: the clinical impact of agitation in various psychiatric disorders: management consensus and controversies. J. Clin. Psychiatry. 2006;67(Suppl. 10):3–5. [PubMed] [Google Scholar]
- 16.Bourdinaud V., Pochard F. Survey of management methods for patients in a state of agitation at admission and emergency departments in France. Encephale. 2003;29(2):89–98. [PubMed] [Google Scholar]
- 17.Dean K., Walsh E., Morgan C., Demjaha A., Dazzan P., Morgan K., Lloyd T., Fearon P., Jones P.B., Murray R.M. Aggressive behaviour at first contact with services: findings from the AESOP First Episode Psychosis Study. Psychol. Med. 2007;37(4):547–557. doi: 10.1017/S0033291706008920. [DOI] [PubMed] [Google Scholar]
- 18.Escobar R., San L., Pérez V., Olivares J.M., Polavieja P., López-Carrero C., Casillas M., Montoya A. Effectiveness results of olanzapine in acute psychotic patients with agitation in the emergency room setting: results from NATURA study. Actas Esp. Psiquiatr. 2008;36(3):151–157. [PubMed] [Google Scholar]
- 19.González-Ortega I., Mosquera F., Echeburúa E., González-Pinto A. Insight, psychosis and aggressive behaviour in mania. Eur. J. Psychiatry. 2010;24(2):70–77. doi: 10.4321/S0213-61632010000200002. [DOI] [Google Scholar]
- 20.Judd L.L., Schettler P.J., Akiskal H., Coryell W., Fawcett J., Fiedorowicz J.G., Solomon D.A., Keller M.B. Prevalence and clinical significance of subsyndromal manic symptoms, including irritability and psychomotor agitation, during bipolar major depressive episodes. J. Affect. Disord. 2012;138(3):440–448. doi: 10.1016/j.jad.2011.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pajonk F.G., Schmitt P., Biedler A., Richter J.C., Meyer W., Luiz T., Madler C. Psychiatric emergencies in prehospital emergency medical systems: a prospective comparison of two urban settings. Gen. Hosp. Psychiatry. 2008;30(4):360–366. doi: 10.1016/j.genhosppsych.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Citrome L. Addressing the need for rapid treatment of agitation in schizophrenia and bipolar disorder: focus on inhaled loxapine as an alternative to injectable agents. Ther. Clin. Risk Manag. 2013;9:235–245. doi: 10.2147/TCRM.S31484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lehman A.F., Lieberman J.A., Dixon L.B., McGlashan T.H., Miller A.L., Perkins D.O., Kreyenbuhl J., American Psychiatric Association. Steering Committee on Practice Guidelines Practice guideline for the treatment of patients with schizophrenia, second edition. Am. J. Psychiatry. 2004;161(Suppl. 2):1–56. [PubMed] [Google Scholar]
- 24.Allen M.H., Currier G.W., Hughes D.H., Reyes-Harde M., Docherty J.P. Expert Consensus Panel for Behavioral Emergencies. The expert consensus guideline series. Treatment of behavioral emergencies. Postgrad. Med. 2001;(Spec No):1–88. [PubMed] [Google Scholar]
- 25.Holloman G.H., Jr, Zeller S.L. Overview of Project BETA: Best practices in evaluation and treatment of agitation. West. J. Emerg. Med. 2012;13(1):1–2. doi: 10.5811/westjem.2011.9.6865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garriga M., Pacchiarotti I., Kasper S., Zeller S.L., Allen M.H., Vázquez G., Baldaçara L., San L., McAllister-Williams R.H., Fountoulakis K.N., Courtet P., Naber D., Chan E.W., Fagiolini A., Möller H.J., Grunze H., Llorca P.M., Jaffe R.L., Yatham L.N., Hidalgo-Mazzei D., Passamar M., Messer T., Bernardo M., Vieta E. Assessment and management of agitation in psychiatry: Expert consensus. World J. Biol. Psychiatry. 2016;17(2):86–128. doi: 10.3109/15622975.2015.1132007. [DOI] [PubMed] [Google Scholar]
- 27.Battaglia J. Pharmacological management of acute agitation. Drugs. 2005;65(9):1207–1222. doi: 10.2165/00003495-200565090-00003. [DOI] [PubMed] [Google Scholar]
- 28.Benjamini Y., Drai D., Elmer G., Kafkafi N., Golani I. Controlling the false discovery rate in behavior genetics research. Behav. Brain Res. 2001;125(1-2):279–284. doi: 10.1016/S0166-4328(01)00297-2. [DOI] [PubMed] [Google Scholar]
- 29.Moritz F., Jenvrin J., Canivet S., Gerault D. Management of agitated patients in emergency departments. Reanimation. 2004;13:500–506. doi: 10.1016/S1624-0693(04)00151-3. [DOI] [Google Scholar]
- 30.Curran G.M., Sullivan G., Williams K., Han X., Collins K., Keys J., Kotrla K.J. Emergency department use of persons with comorbid psychiatric and substance abuse disorders. Ann. Emerg. Med. 2003;41(5):659–667. doi: 10.1067/mem.2003.154. [DOI] [PubMed] [Google Scholar]
- 31.Wilson M.P., Pepper D., Currier G.W., Holloman G.H., Jr, Feifel D. The psychopharmacology of agitation: consensus statement of the american association for emergency psychiatry project Beta psychopharmacology workgroup. West. J. Emerg. Med. 2012;13(1):26–34. doi: 10.5811/westjem.2011.9.6866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Valdes J., Shipley T., Rey J.A. Loxapine inhalation powder (adasuve): a new and innovative formulation of an antipsychotic treatment for agitation. P&T. 2014;39(9):621–623, 648. [PMC free article] [PubMed] [Google Scholar]
- 33.Pascual J.C., Madre M., Puigdemont D., Oller S., Corripio I., Díaz A., Faus G., Perez V., Alvarez E. A naturalistic study: 100 consecutive episodes of acute agitation in a psychiatric emergency department. Actas Esp. Psiquiatr. 2006;34(4):239–244. [PubMed] [Google Scholar]
- 34.Downey L.V., Zun L.S., Gonzales S.J. Frequency of alternative to restraints and seclusion and uses of agitation reduction techniques in the emergency department. Gen. Hosp. Psychiatry. 2007;29(6):470–474. doi: 10.1016/j.genhosppsych.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Knox D.K., Holloman G.H., Jr Use and avoidance of seclusion and restraint: consensus statement of the american association for emergency psychiatry project Beta seclusion and restraint workgroup. West. J. Emerg. Med. 2012;13(1):35–40. doi: 10.5811/westjem.2011.9.6867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Katsakou C., Bowers L., Amos T., Morriss R., Rose D., Wykes T., Priebe S. Coercion and treatment satisfaction among involuntary patients. Psychiatr. Serv. 2010;61(3):286–292. doi: 10.1176/ps.2010.61.3.286. [DOI] [PubMed] [Google Scholar]
- 37.Richmond J.S., Berlin J.S., Fishkind A.B., Holloman G.H., Jr, Zeller S.L., Wilson M.P., Rifai M.A., Ng A.T. Verbal de-escalation of the agitated patient: Consensus statement of the american association for emergency psychiatry project BETA de-escalation workgroup. West. J. Emerg. Med. 2012;13(1):17–25. doi: 10.5811/westjem.2011.9.6864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.San L., Arranz B., Querejeta I., Barrio S., De la Gándara J., Pérez V. A naturalistic multicenter study of intramuscular olanzapine in the treatment of acutely agitated manic or schizophrenic patients. Eur. Psychiatry. 2006;21(8):539–543. doi: 10.1016/j.eurpsy.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 39.Mavrogiorgou P., Brüne M., Juckel G. The management of psychiatric emergencies. Dtsch. Arztebl. Int. 2011;108(13):222–230. doi: 10.3238/arztebl.2011.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]