Abstract
Posterior reversible encephalopathy syndrome (PRES) is a recently described, scarcely documented clinical entity. PRES is caused by various factors, the most common being hypertension, followed by nonhypertensive causes such as renal diseases and immunosuppressive therapy. Recently, some cases have been reported about the association of increased use of cytotoxic and immunosuppressive agents in cancer patients, and relevant reports have increased with advances in radiological examinations. Here, we report a case of gallbladder cancer with liver metastasis undergoing gemcitabine- and cisplatin-based chemotherapy who presented with complaints of seizures, headache, and bilateral lower limb weakness. Thorough clinical examination, biochemical analysis, and radiological evaluation led to diagnosis of PRES. It is important to recognize this syndrome which will facilitate early diagnosis and prompt symptomatic management. Removal of causative agent is an important aspect of management. Studies are needed to identify factors of adverse prognostic significance and to develop neuroprotective strategies.
Keywords: Cisplatin, Gemcitabine, posterior reversible encephalopathy syndrome
INTRODUCTION
Hinchey et al. in 1996 described clinico-radiological entity called posterior reversible encephalopathy syndrome (PRES), characterized by symptoms of headache, disturbance of consciousness, altered mental status, seizures, and visual disturbance.[1] Its global incidence is unknown due to rarity, mean age ranging across reported cases being 39–47 years. There is marked female preponderance. PRES has been frequently associated with hypertensive encephalopathy, eclampsia and use of immunosuppressive drugs, renal failure, and general anesthesia.[2] Various cytotoxic, immunosuppressive, and biological agents have been indicted in the development of PRES[3] with reported mortality of 15%. PRES is typically reversible once the cause is removed. However, permanent neurological impairment or death occurs in a minority of patients.[4] We report a similar case which presented with characteristic clinical and radiologic findings of PRES due to gemcitabine and cisplatin infusion and showed minimal neurologic improvement but ultimately led to death due to malignancy, without full neurologic recovery.
While the pathogenesis of hypertensive PRES has been proposed to be a breakdown of cerebral blood pressure and autoregulatory failure. Mechanism by which immunosuppressive and cytotoxic agents causes PRES has been proposed to be related to the alteration of the blood–brain barrier due to direct impairment of the endothelium.[5,6]
PRES is also probably related to the persistent hypoperfusion due to focal vasoconstriction, as a consequence of upregulation of vascular endothelial growth factor.[7] This causes angiogenesis and a transient increase in vascular permeability due to endothelial dysfunction.[4,8]
CASE REPORT
A 40-year-old female, 2 months ago, noticed a painful lump on the right side of abdomen. On examination, three finger breadth hepatomegaly was present. Ultrasonography of abdomen and pelvis as well as contrast-enhanced computed tomography of abdomen confirmed significant gallbladder thickening with 13 cm × 13 cm mass in segment four, five, and six of liver extending up to gallbladder fossa suggestive of metastatic lesion. Subsequent biopsy from gallbladder confirmed the diagnosis as adenocarcinoma. She was registered as a case of carcinoma gallbladder with liver metastasis (Stage IV).
In view of metastatic disease, the patient was started on intravenous (IV) gemcitabine (1.2 g on day 1, 8, and 15) with cisplatin 40 mg (IV) on day 1. Patient completed four cycles of chemotherapy with occasional complaints of nausea, vomiting, and loose stools which were managed symptomatically.
Ten days after completion of the 4th cycle of chemotherapy, the patient presented with complaints of convulsions and altered mental status. On admission, patient was normotensive, and serum electrolyte was normal, but renal function test was deranged. On 2nd day of admission, patient became aphasic with complaints of bilateral lower limb weakness.
Patient underwent magnetic resonance imaging (MRI) brain which revealed altered signal intensity, involving meninges along gyri of parieto-occipital lobe and subcortical white matter of right parietal lobe with T2/fluid-attenuated inversion recovery (FLAIR) hypersensitivity [Figures 1 and 2] and abnormal contrast enhancement on both side of midline with glutamine peak on MRI favoring PRES. Patient was started on anticonvulsant therapy and mannitol infusion along with steroids. Patient showed a good symptomatic response in the form of improved mental status. Patient on day 7 was given oral anticonvulsant and discharged, on follow-up after 2 weeks, she had bilateral lower limb weakness though aphasia had subsided. Patient succumbed to malignancy within 2 months of diagnosis of PRES.
Figure 1.
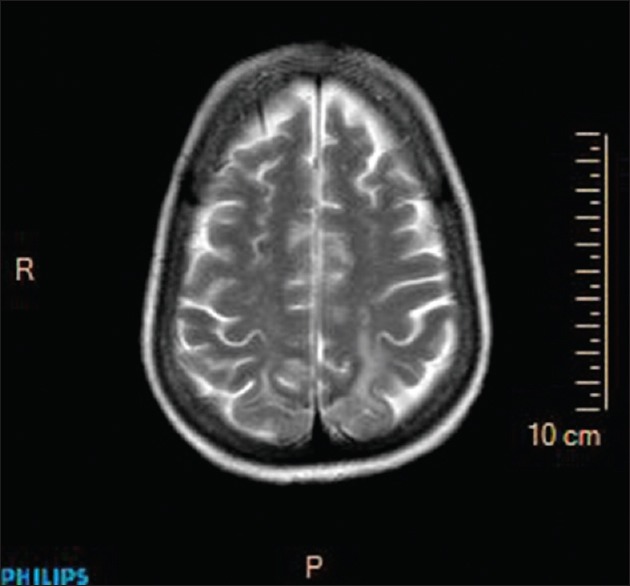
T2-weighed magnetic resonance imaging
Figure 2.
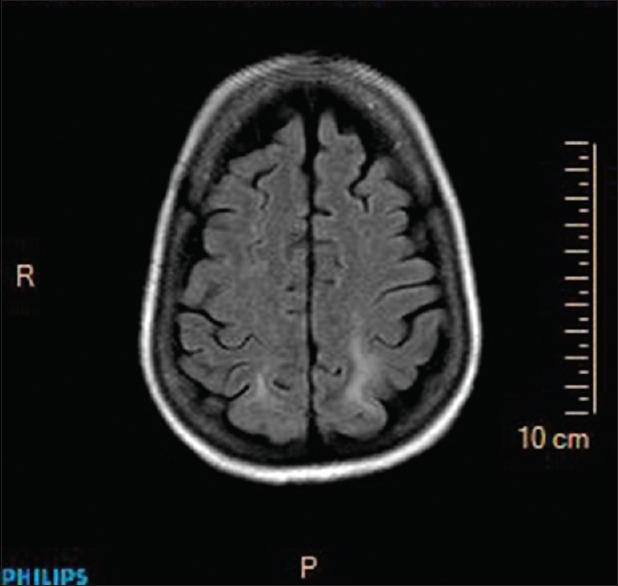
Fluid-attenuated inversion recovery hypersensitivity
DISCUSSION
PRES usually occurs in a setting of uncontrolled hypertension. Nonhypertensive causes of PRES such as antineoplastic agents, for example, combination chemotherapy, dexamethasone, erythropoietin, and autologous stem cells transplant are being increasingly recognized.
No single antineoplastic agent has been consistently associated with PRES, but high-dose, multidrug chemotherapy is more frequently associated.,[9] which is characteristically seen in our case.
Gemcitabine is a nucleoside analog that has a structure similar to the naturally occurring nucleoside deoxycytidine. Although more lipophilic, it is unclear if gemcitabine can cross the blood–brain barrier. Neurologic toxicities with gemcitabine are uncommon and include peripheral neuropathy (3%) and somnolence (9%). Few reports have shown that PRES redeveloped after readministration of gemcitabine.[3,10]
Case reports in literature acknowledge that PRES as a neurological adverse effect of Cisplatin.[11] There are two neurological patterns, first consists of focal neurological deficits with or without seizures which are not dose dependent, no radiological pattern, and cerebrospinal fluid analysis is normal. The second pattern consists of PRES, with the characteristic symptoms as described above and the typical neuroradiological abnormalities.
Differential diagnosis includes chemotherapy-related multifocal demyelination syndrome, cancer metastasis, cerebrovascular accident, venous thrombosis, and paraneoplastic demyelinating syndromes. Most of these conditions can be easily differentiated from PRES as they are irreversible with distinct imaging patterns on MRI.
A lumbar puncture may be necessary in patients with PRES to rule out infectious and inflammatory etiologies.[12] Radiation necrosis can lead to widespread white matter abnormalities, cytotoxic edema, which causes true diffusion restriction on MRI and not vasogenic edema, which is typically seen in PRES [Figure 3].
Figure 3.
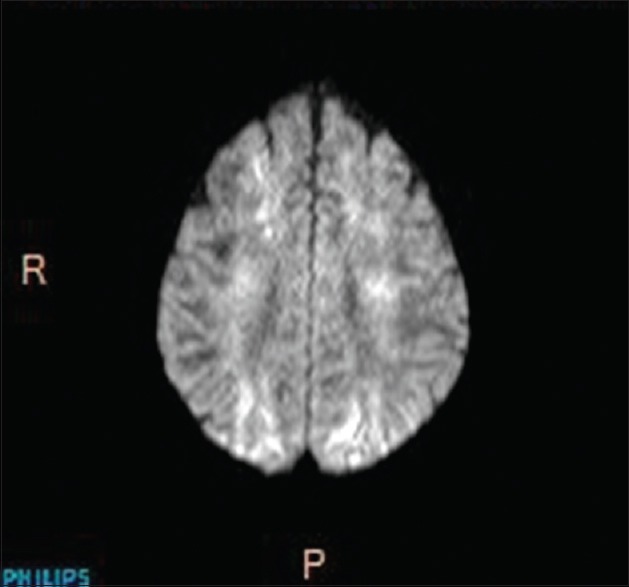
Diffusion-weighed image
MRI is superior to computed tomography for the diagnosis of PRES. Four main MRI patterns of PRES are:[13]
Holohemispheric watershed pattern (23%)
Superior frontal sulcus pattern (27%)
Dominant parietal-occipital pattern (22%) [Figure 4]
Partial or asymmetric expression of the primary patterns (28%).
Figure 4.
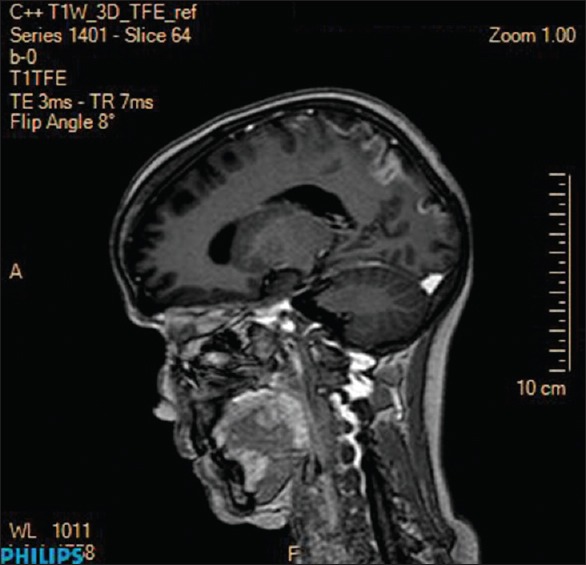
Dominant parieto-occipital pattern
Other differential diagnosis and their characteristic features are:[14]
Acute cerebral ischemia: Unilateral, systematically arranged lesions with a decreased diffusion coefficient that points to a cytotoxic edema
Pontine encephalopathies related to metabolic disorders or mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes syndrome: Lesions are localized to the brain stem, and the apparent diffusion coefficient is raised
Acute disseminated encephalomyelitis: This condition has a distinctive clinical context, often following a viral infection or vaccination. There is often lesion enhancement, which may be nodular or ring-shaped
Creutzfeldt–Jakob disease: Lesions with a raised diffusion coefficient, affecting the basal ganglia and the cerebral cortex
Gliomatosis cerebri: Spectroscopy demonstrates a tumor-type profile with marked elevation of myo-inositol
Progressive multifocal leukoencephalopathy: There may be single or multiple lesions, which may be unilateral or bilateral and asymmetrical, involving predominantly the subcortical white matter (short fibers) or the parietal and occipital regions.
Prompt correction of the underlying cause is crucial to decrease the risk of ischemia or bleeding and therefore to avoid permanent disability or death.[1] Patients should be routinely evaluated for hyperthermia, hypoglycemia, and metabolic disturbances, in particular hypomagnesemia, which require prompt correction. Patients with persistent seizure activity should be given IV benzodiazepines. Those with continuing seizure activity should receive standard complementary IV anticonvulsant drugs. Patients with refractory status epilepticus need midazolam, propofol, or thiopental in titrated doses until remission of the clinical seizure activity. In case of hypertensive emergency, the aim is to decrease the mean arterial pressure by 20–25% within the first 2 h and to bring the blood pressure down to 160/100 mmHg within the first 6 h. IV antihypertensive includes labetalol, nicardipine, or fenoldopam if available.
PRES is a potentially reversible condition. Despite the severe clinical symptoms and signs, most patients make a full recovery. However, failure to recognize the syndrome and delay in withdrawal of the offending agent may result in catastrophic CNS injury or death. Recurrences have been reported in 6% of cases. Death has been reported in up to 15% of patients. In our case, despite the removal of causative agent, patient failed to make a full recovery.
Robust data regarding the outcome of chemotherapy-associated PRES are lacking in literature. Multiple Risk factors, precipitating factors, patient-related factors, and prognostic factors have been identified but still validated scales are lacking to triage patient into various risk groups. Hence, to determine the magnitude of this syndrome, a special registry should be considered for future tailoring of management guidelines.
It is imperative to have knowledge of this rare entity, for early recognition and withdrawal of the offending agent which is a key step in the management of affected patients. Although terminology suggests reversibility, permanent neurological damage has been reported, as seen in our case, hence “potentially reversible encephalopathy syndrome” seems a better terminology.
AUTHORS' CONTRIBUTION
Rohit Santosh Kabre contributed to concept and manuscript preparation while Krishna Marotirao Kamble helped in manuscript editing.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Dr. Vibhor Jain, DMRD.
REFERENCES
- 1.Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494–500. doi: 10.1056/NEJM199602223340803. [DOI] [PubMed] [Google Scholar]
- 2.Ito Y, Arahata Y, Goto Y, Hirayama M, Nagamutsu M, Yasuda T, et al. Cisplatin neurotoxicity presenting as reversible posterior leukoencephalopathy syndrome. AJNR Am J Neuroradiol. 1998;19:415–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Rajasekhar A, George TJ., Jr Gemcitabine-induced reversible posterior leukoencephalopathy syndrome: A case report and review of the literature. Oncologist. 2007;12:1332–5. doi: 10.1634/theoncologist.12-11-1332. [DOI] [PubMed] [Google Scholar]
- 4.Bartynski WS. Posterior reversible encephalopathy syndrome, part 2: Controversies surrounding pathophysiology of vasogenic edema. AJNR Am J Neuroradiol. 2008;29:1043–9. doi: 10.3174/ajnr.A0929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shimono T, Miki Y, Toyoda H, Egawa H, Uemoto S, Tanaka K, et al. MR imaging with quantitative diffusion mapping of tacrolimus-induced neurotoxicity in organ transplant patients. Eur Radiol. 2003;13:986–93. doi: 10.1007/s00330-002-1594-9. [DOI] [PubMed] [Google Scholar]
- 6.Horbinski C, Bartynski WS, Carson-Walter E, Hamilton RL, Tan HP, Cheng S. Reversible encephalopathy after cardiac transplantation: Histologic evidence of endothelial activation, T-cell specific trafficking, and vascular endothelial growth factor expression. AJNR Am J Neuroradiol. 2009;30:588–90. doi: 10.3174/ajnr.A1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature. 1992;359:843–5. doi: 10.1038/359843a0. [DOI] [PubMed] [Google Scholar]
- 8.Belogolovkin V, Levine SR, Fields MC, Stone JL. Postpartum eclampsia complicated by reversible cerebral herniation. Obstet Gynecol. 2006;107(2 Pt 2):442–5. doi: 10.1097/01.AOG.0000173981.55388.4b. [DOI] [PubMed] [Google Scholar]
- 9.Shah-Khan FM, Pinedo D, Shah P. Reversible posterior leukoencephalopathy syndrome and anti-neoplastic agents: A review. Oncol Rev. 2007;1:152–61. [Google Scholar]
- 10.Larsen FO, Hansen SW. Severe neurotoxicity caused by gemcitabine treatment. Acta Oncol. 2004;43:590–1. doi: 10.1080/02841860410018494. [DOI] [PubMed] [Google Scholar]
- 11.Nomura K, Ohno R, Hamaguchi K, Hata T, Hatanaka H, Matsuyama H. Clinicopathological report of cisplatin encephalopathy. Rinsho Shinkeigaku. 1995;35:64–9. [PubMed] [Google Scholar]
- 12.Savarese DM, Gordon J, Smith TW, Litofsky NS, Licho R, Ragland R, et al. Cerebral demyelination syndrome in a patient treated with 5-fluorouracil and levamisole. The use of thallium SPECT imaging to assist in noninvasive diagnosis – A case report. Cancer. 1996;77:387–94. doi: 10.1002/(SICI)1097-0142(19960115)77:2<387::AID-CNCR23>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 13.Bartynski WS, Boardman JF. Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2007;28:1320–7. doi: 10.3174/ajnr.A0549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamy C, Oppenheim C, Méder JF, Mas JL. Neuroimaging in posterior reversible encephalopathy syndrome. J Neuroimaging. 2004;14:89–96. [PubMed] [Google Scholar]


