Abstract
Background:
Arthroscopic treatment of calcific deposits of rotator cuff tears has been described with successful results in the general population. However, despite the high frequency of this condition, there is no information in the literature regarding arthroscopic treatment of rotator cuff calcifications in athletes.
Purpose:
To analyze the time to return to sport, clinical outcomes, and complications of complete arthroscopic removal of intratendinous calcific deposits and repair of the tendon lesion without acromioplasty in athletes.
Study Design:
Case series; Level of evidence, 4.
Methods:
This study retrospectively evaluated 24 consecutive patients with a mean age of 36.2 years. The mean follow-up was 59 months (range, 24-108 months). Patients completed a questionnaire focused on the time to return to sport and treatment course. Pre- and postoperative functional assessment was performed using the Constant score and University of California Los Angeles (UCLA) score. Pain was assessed by visual analog scale (VAS). Radiographs and magnetic resonance imaging (MRI) were performed to evaluate the recurrence of calcifications and the indemnity of the supraspinatus tendon repair.
Results:
Of the 24 patients, 23 (95.8%) were able to return to sports; 91.3% returned to the same level. The mean time to return to play was 5.3 months (range, 3-9 months): 26% of patients (6/23) returned to sports in less than 4 months, 61% (14/24) returned between 4 and 6 months, and 13% (3/24) returned after the sixth month. The mean Constant score increased from 26.9 preoperatively to 89.7 postoperatively (P < .001), and the UCLA score increased from 17.3 preoperatively to 33.2 postoperatively (P < .001). Significant improvement was obtained for pain (mean VAS, 8.4 [before surgery] vs 0.6 [after]; P < .001). The overall majority (91.6%) of patients were satisfied with their result. MRI examination at last follow-up (79% of patients) showed no tendon tears.
Conclusion:
In athletes with calcifying tendinitis of the supraspinatus tendon with failed nonoperative treatment, complete arthroscopic removal of calcific deposits and tendon repair without acromioplasty results in significant pain relief and improvement in functional outcomes. Most patients return to the same level of proficiency regardless of the type of sport and the level of competition before injury, with 91.6% of patients satisfied with their results.
Keywords: return to sports, athletes, calcifying tendinitis, rotator cuff, arthroscopy
Calcific tendinopathy is one of the most frequent causes of nontraumatic pain in the shoulder.32 The prevalence rates range between 7.8% in asymptomatic patients and 42.5% in patients with subacromial impingement syndrome.9,16 Many different treatment modalities with favorable clinical outcomes have been described for rotator cuff calcifications. These include physical therapy, subacromial corticosteroid injections, lavage and aspiration, and high-energy extracorporeal shockwave therapy.4,5,14,15,17,18,22,33 Although this condition is typically temporal in nature, pain and symptoms occasionally persist despite nonsurgical measures, and more aggressive management options become necessary.22,23,32
Arthroscopic treatment of calcific deposits of rotator cuff tears (RCTs) has been described with successful results in the general population.‡ However, despite the high frequency of this condition, there is no information in the literature regarding arthroscopic treatment of rotator cuff calcifications in athletes. Furthermore, some technical aspects such as the importance of removing all of the calcium, the need for suturing the residual tendon lesions after removal of the deposits, and the benefits of acromioplasty are largely debated.§ This further complicates the choice of appropriate treatment in this subgroup of patients. We previously published the results of arthroscopic removal and rotator cuff repair without acromioplasty in a series of 26 patients.27 We found that this technique leads to a significant improvement in most patients, and 96.2% of them were satisfied with their results. However, return to play is an important outcome in many patients with calcific tendinitis, and this was not addressed in that previous study. This is the first study describing functional outcomes with arthroscopic treatment of rotator cuff calcifications in athletes. This study includes a detailed evaluation of time to return to sports, the level achieved by patients, and the relation between final functional outcomes and the level of competition before surgery.
The purpose of this study was to analyze the time to return to sport, clinical outcomes, and complications of complete arthroscopic removal of intratendinous calcific deposits and repair of the tendon lesion without acromioplasty in athletes.
Methods
Between June 2006 and January 2014, 46 patients with calcifying rotator cuff tendinitis were treated with arthroscopic excision of the calcium deposits and tendon defect repair without acromioplasty at our institution. In 2015, we reported the results of this procedure in the general population.27 In the present study, we report our results in the subgroup of athletes. We included 17 patients who were analyzed in the previous study and added 8 more who were not part of the previous cohort. Our institutional review board (IRB 00003580) approved the study protocol.
Inclusion criteria were shoulder pain persistence for more than 4 months (mean, 5.2 months) with visible calcification on conventional radiographs and failure of intensive nonoperative treatment, including physical therapy, nonsteroidal anti-inflammatory drugs, and steroid injections, for at least 3 months. Patients were required to have an intention to return to sports postoperatively. The deposits were located in the supraspinatus tendon in all cases. Patients with concomitant pathologies such as instability, rotator cuff tears, or acromioclavicular joint pathology were excluded from this study.
Demographic and clinical characteristics of patients regarding age, sex, shoulder dominance, injured side, and duration of symptoms before surgery were documented. A summary of demographic and clinical characteristics of patients is shown in Table 1.
TABLE 1.
Demographic and Clinical Characteristics of Patients and Lesions
| Sex, n | |
| Female | 14 |
| Male | 10 |
| Age, y, mean ± SD (range) | 36 ± 6.1 (26-60) |
| Dominant hand, % | 60 |
| Involved shoulder, n | |
| Right | 13 |
| Left | 11 |
| Mean follow-up, mo, mean (range) | 59 (24-108) |
| Symptom duration, mo, mean ± SD | 5.2 ± 1.8 |
| Preinjury sport level | |
| Competitive | 9 |
| Recreational | 15 |
| Type of sport | |
| G1: noncollision/nonoverhead | 13 |
| G2: high-impact/collision | 5 |
| G3: overhead | 6 |
One patient was excluded because he had a concomitant calcification of the subscapularis tendon, so 24 patients were available for final analysis (14 women, 10 men). No patient was lost to follow-up. There were 13 right shoulders and 11 left shoulders. The dominant side was involved in 60% of patients. The mean age was 36.2 years (range, 26-60 years). The French Arthroscopic Society radiographic classification21 was used to assess calcific deposits preoperatively: type A, homogeneous calcification with well-defined limits; type B, heterogeneous and fragmented calcification with well-defined limits; type C, heterogeneous calcification with poorly defined limits and sometimes with a punctate appearance; and type D, dystrophic calcifications at the tendon insertion. The preoperative evaluation showed 17 type A lesions (70.8%) and 7 type B lesions (29.2%).
All patients were evaluated with preoperative anteroposterior radiographs, axillary lateral, and supraspinatus outlet views. Each patient underwent magnetic resonance imaging (MRI) to rule out possible concomitant pathologies such as rotator cuff lesions (Figure 1).
Figure 1.
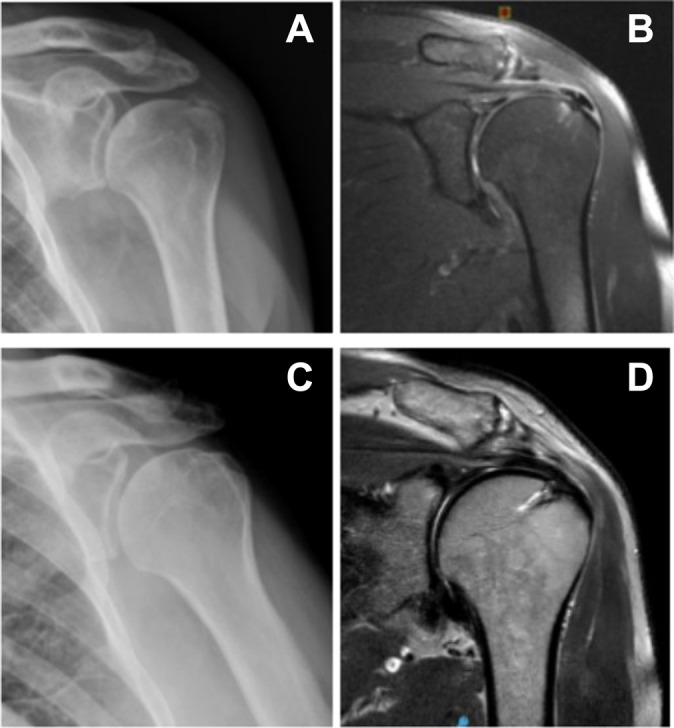
(A) Plain radiograph showing type A calcific deposit (homogeneous calcification with well-defined limits). (B) Magnetic resonance image (MRI) showing the calcific deposit in the supraspinatus tendon before surgery. (C) Postoperative plain radiograph 1 month after surgery showing the absence of residual calcifications. (D) MRI image 6 months after surgery showing complete tendon integrity.
Patient sport level was divided into competitive sport (regular sport with competition and practice 2 times/week) and recreational sport (regular sport without competition 2 times/week).31 The distinctive types of shoulder-dependent sport were subdivided according to Allain et al1: noncollision/nonoverhead shoulder sport (G1), high-impact/collision sport (G2), overhead sport (G3).
Pre- and postoperative clinical assessment was performed using the Constant score and the University of California Los Angeles shoulder scale (UCLA) score. Pain evaluation was carried out using a visual analog scale (VAS). Furthermore, all patients were asked to describe the subjective result of the intervention as excellent, good, fair, or poor.
Patients were also asked whether they had been able to practice their previous sports and whether they had been able to perform them at the same level as they had before the calcification. Throughout follow-up, all patients were evaluated with radiographs and MRIs to evaluate the recurrence of calcifications and the indemnity of the supraspinatus tendon repair. Oblique coronal, oblique sagittal, and transverse views of T2-weighted images on MRI were used to classify postoperative cuff integrity into 5 categories according to Sugaya et al32: type 1, repaired cuff appeared to have sufficient thickness compared with normal cuff, with homogeneously low intensity on each image; type 2, sufficient thickness compared with normal cuff associated with partial high-intensity area; type 3, insufficient thickness with less than half the thickness when compared with normal cuff but without discontinuity, suggesting a partial-thickness delaminated tear; type 4, presence of a minor discontinuity in only 1 or 2 slices on both oblique coronal and sagittal images, suggesting a small, full-thickness tear; and type 5, presence of a major discontinuity observed in more than 2 slices on both oblique coronal and sagittal images, suggesting a medium or large full-thickness tear. Intraoperative and postoperative complications were documented
Surgical Technique
We utilized the same surgical technique published in our previous publication (see the Video Supplement).27 A lateral portal was established in the subacromial space, and after localization of the calcific deposits, they were completely excised with a motorized shaver. The tendon tears created with the shaver were repaired completely.
Suture anchor repair was undertaken in the case of a relatively large full-thickness defect and partial tears of greater than 50% tendon thickness after removal of calcific material, and side-to-side repair was performed in tears of less than 50% tendon thickness to avoid potential propagation of rotator cuff tear. No subacromial decompression or distal clavicle resection was accomplished in any patient.
Postoperative Rehabilitation
Postoperative protocol consisted of sling immobilization for 3 to 4 weeks depending on the type of repair performed. A standardized rehabilitation protocol for rotator cuff repairs was used with progressive range of motion exercises as tolerated. Return to sports and heavy manual work was allowed when the patient was pain free, full shoulder range of motion had been achieved, and shoulder strength was near 100%, which usually occurred at 3 to 6 months.
Statistical Analysis
Pre- and postoperative scores were compared using the Student t test for independent samples. Continuous variables are presented as means ± standard deviations, whereas categorical variables as absolute and relative frequencies. The statistical analysis was performed using the software STATA version 12 (Stata Corp). A P value <.05 was considered statistically significant.
Results
The mean follow-up period was 59 months (range, 24-108 months). A summary of clinical results is shown in Table 2.
TABLE 2.
Summary of Clinical Results: Pre- and Postoperative VAS Pain, Constant, and UCLA Scoresa
| Preoperative | Postoperative | P Value | |
|---|---|---|---|
| Constant | 26.9 ± 12.6 | 89.7 ± 1.3 | <.001 |
| UCLA | 17.3 ± 6 | 33.2 ± 4.5 | <.001 |
| VAS | 8.4 ± 1.3 | 0.6 ± 0.3 | <.001 |
| Subjective results, n | |||
| Excellent | 8 | ||
| Good | 14 | ||
| Fair | 2 | ||
| Poor | 0 |
aData are reported as mean ± SD unless otherwise indicated. UCLA, University of California Los Angeles; VAS, visual analog scale.
Repair using a suture anchor was performed in 21 patients (87.5%), and side-to-side repair in 3 patients (12.5%). In the suture anchor group, there were 14 complete tears and 8 partial tears (grade 3 after total calcium removal according to Ellman classification). In the side-to-side repair group, all repaired defects were grade 2 according to Ellman classification.
All functional scores improved significantly after surgery. The mean Constant score increased from 26.9 preoperatively to 89.7 postoperatively (P < .001), and the UCLA score increased from 17.3 preoperatively to 33.2 postoperatively (P < .001). The pain scores improved significantly from a mean 8.4 before surgery to 0.6 after the operation (P < .001). With subjective evaluation, 91.6% of patients reported having an excellent or good result (8 excellent, 14 good), and 8.4% (n = 2) reported fair results. No patient scored his or her result as poor.
Of the 24 patients, 23 (95.8%) were able to return to sports. The patient who did not manage to return to sports was a runner who had a concomitant femoroacetabular impingement and attributed inability to resume sports to hip pain. The mean time to return to play was 5.3 months (range, 3-9 months): 26% of patients (6/23) returned to sports in less than 4 months after surgery, 61% (14/23) returned to sports between 4 and 6 months after surgery, and 13% (3/23) returned to sports after the sixth month. Of the 23 patients who returned to sports, 21 (91.3%) were able to return to the same level they were at previous to surgery. Two patients could not return to the same sport level. The first patient was a tennis player who although could continue playing had to decrease the frequency and intensity of competition because he felt discomfort in the operated shoulder. The other patient was a weightlifter who noted that he could not lift the same amount of weight as before the injury. As shown in Table 3, the final functional outcomes were not related to level of competition before surgery. Regarding type of sports, patients belonging to group G1 (noncollision/nonoverhead sports) returned significantly faster to sports than other patients (P < .001).
TABLE 3.
Results According to Type of Sport and Level of Competitiona
| n | Mean Time to Return, mo | Constant Score, Mean ± SD | |
|---|---|---|---|
| Type of sport | |||
| G1: noncollision/ nonoverhead | 12 | 4.3 | 90.8 ± 2.3 |
| G2: high-impact/collision | 5 | 5.8 | 86.2 ± 1.6 |
| G3: overhead | 6 | 6.2 | 88.3 ± 1.3 |
| P value | <.01 | NS | |
| Level of competition | |||
| Competitive | 8 | 5.6 | 87.4 ± 1.6 |
| Recreational | 15 | 4.9 | 90.4 ± 2.3 |
| P value | NS | NS |
aNS, not significant.
No residual calcifications were observed in postoperative radiographs. Postoperative tendon integrity evaluation with MRI was possible in 79% (19/24) of patients. All of these patients showed integrity of the rotator cuff tendons. The postoperative MRI Sugaya classification32 results showed 11 patients with type 1 repair and 8 patients with type 2 repair.
Repair using suture anchors was performed in 21 patients (87.5%), and side-to-side repair in 3 patients (12.5%). In the suture anchor group, there were 19 complete tears and 2 partial bursal tears grade 3 after total calcium removal according to Ellman classification.7 In the side-to-side repair group, all the repaired defects were grade 2 according to Ellman classification.
In the postoperative period, a frozen shoulder was observed in 2 patients (8.3%). Both patients were treated satisfactorily with physical therapy and 1 corticosteroid subacromial injection.
Discussion
One of the main expectations of athletes, whatever their age or level of play, is to return to sports after treatment if possible at the same level as before injury. Despite favorable results in the general population,‖ there are no studies in the literature evaluating arthroscopic treatment of rotator cuff calcifications in athletes.
In our previous study, we found that in the general population with calcifying tendinitis who did not respond favorably to nonoperative treatment, complete removal of calcific deposits and tendon repair without acromioplasty resulted in significant pain relief and improvement in functional outcomes.27 Moreover, MRI examination at last follow-up (70% of patients) showed no tendon tears, and 96.2% of patients were satisfied with their results.27 In the present study, we found that in athletes with calcifying tendinitis of the supraspinatus tendon with failed nonoperative treatment, complete arthroscopic removal of calcific deposits and tendon repair without acromioplasty resulted in significant pain relief and improvement in functional outcomes. Moreover, most patients returned to the same level of proficiency regardless of the type of sport and the level of competition before injury. We also performed MRI examinations to evaluate tendon integrity (79% of patients), which showed no tendon tears. Despite the improved functional outcomes, only 33% of patients subjectively rated their shoulder as excellent, though 19.6% were satisfied with the procedure. Psychological and emotional factors may have had an effect on the majority of patients rating their shoulders as only “good.”
Currently, several controversies exist regarding surgical management of calcific tendinitis, including the extent of calcification removal, the long-term impact on the tendon, and when or if a subacromial decompression is beneficial.22,23,33 In our patients, we attempted to remove all possible calcium. Jerosch et al12 found that functional outcome was inversely related to the amount of calcification remaining. These results were later confirmed by Porcellini et al,26 who showed that patients with residual calcifications had a lower Constant score at 2- to 5-year follow-up.
Midterm follow-up shows that a significant percentage of patients remain with residual defects after calcium removal if the procedure is not accompanied by a concomitant tendon repair.3,29 Balke et al3 showed that although good clinical results after arthroscopic treatment of calcifying tendinitis persist in the midterm, the affected shoulders have significantly lower clinical scores than healthy shoulders and that the rate of partial supraspinatus tendon tears is higher after calcium removal without tendon repair compared with the contralateral shoulder. These tears could be a risk factor for progression of the lesion, particularly in the subset of athletes with high demands on the shoulder. There is a lack of studies comparing calcium removal with and without tendon repair. However, the limited evidence available suggests that repairing the defect after calcium removal has a favorable effect on tendon healing.26,34 In our study, 79% of patients were available for MRI examination at a mean follow-up of 51 months, and no tears were found.
We found that arthroscopic removal of chronic symptomatic calcifications of the supraspinatus in athletes yielded favorable outcomes and promoted fast remission of pain regardless of a concomitant acromioplasty. Our results support the findings of the American Academy of Orthopaedic Surgeons, which gave acromioplasty a “moderate” recommendation for the treatment of rotator cuff disease.24 Moreover, Marder et al20 showed that in patients with rotator cuff calcifications, the addition of acromioplasty did not add benefit and retarded return to unrestricted activity without pain. These findings are significant in the subgroup of athletes, mostly young and active patients, in whom rapid return to function and sports is a priority in the treatment. Furthermore, Familiari et al,8 in a recently published systematic review of 4 randomized controlled trials of patients undergoing arthroscopic rotator cuff repair treated with subacromial decompression, found no difference when compared with those treated without subacromial decompression.
To our knowledge, there are no studies in the literature reporting functional outcomes and return to sports after arthroscopic removal of calcification in athletes. These patients are especially at risk, in particular those who practice overhead and contact sports.25 In a recent meta-analysis, Klouche et al13 showed that the overall rate of return to sports after repair of rotator cuff tears was 84.7%, with 65.9% of participants returning to play at the same level between 4 and 17 months after surgery. In our study, 95.8% of patients were able to return to sports, and 91.3% were able to return to the same level. The mean time to return to play was 5.3 months, and 83% of patients returned before the eighth month. The authors remarked that only 49.9% of professional and competitive athletes returned to play at the same level as before injury. In our study, we found that final results were not related to the level of competition before surgery. Nevertheless, patients participating in noncollision and nonoverhead sports returned significantly faster to sports than other athletes. These types of sports imply a lower demand for the shoulder, and this could explain the faster return to sports in this subgroup of athletes.
Some limitations to this study should be mentioned. First, we did not have a control group and therefore could not compare complete arthroscopic excision of the calcium deposits and tendon defect repair without acromioplasty directly with other surgical techniques or nonoperative treatments. The number of involved patients is limited. However, we consider that our findings are particularly relevant given the limited data available in the literature on this topic. Furthermore, data from all treated patients were carefully collected, and numerous validated shoulder scores were carefully used to assess the results as well as MRI to assess tendon integrity.
Conclusion
In athletes with calcifying tendinitis of the supraspinatus tendon with failed nonoperative treatment, complete arthroscopic removal of calcific deposits and tendon repair without acromioplasty results in significant pain relief and improvement in functional outcomes. Moreover, most patients return to the same level of proficiency regardless of the type of sport and the level of competition before injury, with 91.6% of patients satisfied with their results.
Supplementary Material
Footnotes
A Video Supplement for this article is available at http://ojsm.sagepub.com/supplemental.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80:841–852. [DOI] [PubMed] [Google Scholar]
- 2. Ark JW, Flock TJ, Flatow EL, Bigliani LU. Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy. 1992;8:183–188. [DOI] [PubMed] [Google Scholar]
- 3. Balke M, Bielefeld R, Schmidt C, Dedy N, Liem D. Calcifying tendinitis of the shoulder: midterm results after arthroscopic treatment. Am J Sports Med. 2012;40:657–661. [DOI] [PubMed] [Google Scholar]
- 4. Bazzocchi A, Pelotti P, Serraino S, et al. Ultrasound imaging-guided percutaneous treatment of rotator cuff calcific tendinitis: success in short-term outcome. Br J Radiol. 2016;89:20150407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. de Witte PB, Selten JW, Navas A, et al. Calcific tendinitis of the rotator cuff: a randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med. 2013;41:1665–1673. [DOI] [PubMed] [Google Scholar]
- 6. El Shewy MT. Arthroscopic removal of calcium deposits of the rotator cuff: a 7-year follow-up. Am J Sports Med. 2011;39:1302–1305. [DOI] [PubMed] [Google Scholar]
- 7. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990;254:64–74. [PubMed] [Google Scholar]
- 8. Familiari F, Gonzalez-Zapata A, Iannò B, Galasso O, Gasparini G, McFarland EG. Is acromioplasty necessary in the setting of full-thickness rotator cuff tears? A systematic review. J Orthop Traumatol. 2015;16:167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harrison AK, Flatow EL. Subacromial impingement syndrome. J Am Acad Orthop Surg. 2011;19:701–708. [DOI] [PubMed] [Google Scholar]
- 10. Hofstee D-J, Gosens T, Bonnet M, De Waal Malefijt J. Calcifications in the cuff: take it or leave it? Br J Sports Med. 2007;41:832–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jacobs R, Debeer P. Calcifying tendinitis of the rotator cuff: functional outcome after arthroscopic treatment. Acta Orthop Belg. 2006;72:276–281. [PubMed] [Google Scholar]
- 12. Jerosch J, Strauss JM, Schmiel S. Arthroscopic treatment of calcific tendinitis of the shoulder. J Shoulder Elbow Surg. 1998;7:30–37. [DOI] [PubMed] [Google Scholar]
- 13. Klouche S, Lefevre N, Herman S, Gerometta A, Bohu Y. Return to sport after rotator cuff tear repair: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1877–1887. [DOI] [PubMed] [Google Scholar]
- 14. Lanza E, Banfi G, Serafini G, et al. Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? A systematic review with proposals for future reporting. Eur Radiol. 2015;25:2176–2183. [DOI] [PubMed] [Google Scholar]
- 15. Lee S-Y, Cheng B, Grimmer-Somers K. The midterm effectiveness of extracorporeal shockwave therapy in the management of chronic calcific shoulder tendinitis. J Shoulder Elbow Surg. 2011;20:845–854. [DOI] [PubMed] [Google Scholar]
- 16. Louwerens JK, Sierevelt IN, van Hove RP, van den Bekerom MP, van Noort A. Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients. J Shoulder Elbow Surg. 2015;24:1588–1593. [DOI] [PubMed] [Google Scholar]
- 17. Louwerens JK, Sierevelt IN, van Noort A, van den Bekerom MP. Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2014;23:1240–1249. [DOI] [PubMed] [Google Scholar]
- 18. Louwerens JK, Veltman ES, van Noort A, van den Bekerom MP. The effectiveness of high-energy extracorporeal shockwave therapy versus ultrasound-guided needling versus arthroscopic surgery in the management of chronic calcific rotator cuff tendinopathy: a systematic review. Arthroscopy. 2016;32:165–175. [DOI] [PubMed] [Google Scholar]
- 19. Maier D, Jaeger M, Izadpanah K, Bornebusch L, Suedkamp NP, Ogon P. Rotator cuff preservation in arthroscopic treatment of calcific tendinitis. Arthroscopy. 2013;29:824–831. [DOI] [PubMed] [Google Scholar]
- 20. Marder RA, Heiden EA, Kim S. Calcific tendonitis of the shoulder: is subacromial decompression in combination with removal of the calcific deposit beneficial? J Shoulder Elbow Surg. 2011;20:955–960. [DOI] [PubMed] [Google Scholar]
- 21. Molé D, Kempf JF, Gleyze P, Rio B, Bonnomet F, Walch G. Results of endoscopic treatment of non-broken tendinopathies of the rotator cuff. 2. Calcifications of the rotator cuff [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1993;79:532–541. [PubMed] [Google Scholar]
- 22. Oliva F, Via AG, Maffulli N. Calcific tendinopathy of the rotator cuff tendons. Sports Med Arthrosc. 2011;19:237–243. [DOI] [PubMed] [Google Scholar]
- 23. Oliva F, Via AG, Maffulli N. Physiopathology of intratendinous calcific deposition. BMC Med. 2012;10:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pedowitz RA, Yamaguchi K, Ahmad CS, et al. Optimizing the management of rotator cuff problems. J Am Acad Orthop Surg. 2011;19:368–379. [DOI] [PubMed] [Google Scholar]
- 25. Plate JF, Haubruck P, Walters J, et al. Rotator cuff injuries in professional and recreational athletes. J Surg Orthop Adv. 2013;22:134–142. [DOI] [PubMed] [Google Scholar]
- 26. Porcellini G, Paladini P, Campi F, Paganelli M. Arthroscopic treatment of calcifying tendinitis of the shoulder: clinical and ultrasonographic follow-up findings at two to five years. J Shoulder Elbow Surg. 2004;13:503–508. [DOI] [PubMed] [Google Scholar]
- 27. Ranalletta M, Rossi LA, Bongiovanni SL, Tanoira I, Piuzzi N, Maignon G. Arthroscopic removal and rotator cuff repair without acromioplasty for the treatment of symptomatic calcifying tendinitis of the supraspinatus tendon. Orthop J Sports Med. 2015;3(4):23259 67115577957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rizzello G, Franceschi F, Longo UG, et al. Arthroscopic management of calcific tendinopathy of the shoulder—do we need to remove all the deposit? Bull NYU Hosp Joint Dis. 2009;67:330–333. [PubMed] [Google Scholar]
- 29. Seil R, Litzenburger H, Kohn D, Rupp S. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy. 2006;22:521–527. [DOI] [PubMed] [Google Scholar]
- 30. Seyahi A, Demirhan M. Arthroscopic removal of intraosseous and intratendinous deposits in calcifying tendinitis of the rotator cuff. Arthroscopy. 2009;25:590–596. [DOI] [PubMed] [Google Scholar]
- 31. Stein T, Linke RD, Buckup J, et al. Shoulder sport-specific impairments after arthroscopic Bankart repair a prospective longitudinal assessment. Am J Sports Med. 2011;39:2404–2411. [DOI] [PubMed] [Google Scholar]
- 32. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–1316. [DOI] [PubMed] [Google Scholar]
- 33. Suzuki K, Potts A, Anakwenze O, Singh A. Calcific tendinitis of the rotator cuff: management options. J Am Acad Orthop Surg. 2014;22:707–717. [DOI] [PubMed] [Google Scholar]
- 34. Yoo JC, Park WH, Koh KH, Kim SM. Arthroscopic treatment of chronic calcific tendinitis with complete removal and rotator cuff tendon repair. Knee Surg Sports Traumatol Arthrosc. 2010;18:1694–1699. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


