Abstract
Diabetes mellitus is a chronic disease of major global health concern due to its increasing prevalence in both developing and developed counties, with a projection increase of 214% from the year 2000 to 2030. Among the Aboriginal population of Canada (which includes the First Nations, Inuit and Metis), diabetes mellitus contribute significantly to their higher morbidity and increased health disparity when compared to the non-Aboriginal Canadians. In view of this, the Federal Government of Canada had launched the Aboriginal Diabetes Initiative (ADI) in 1999 as part of the bigger Canadian Diabetes Strategy to provide a better framework for surveillance, public education and community-based management of diabetes. Originally, ADI was intended for a 5-year cycle, but it was renewed twice in 2005 and then 2010, with a total funding of C$523 million. Given its long history of operation and the massive amount of revenue being injected, it is worthwhile to review the background information and the relevant data that had fostered the ADI; and more importantly, to critically evaluate the benefits and impact of the ADI in terms of the actual health of the Aboriginals and their social inequalities.
Keywords: Aboriginal diabetes initiative, Aboriginals, Canada, diabetes
Background
History and social demography of Aboriginals in Canada
Aboriginals refer to the original people and their descendants that are indigenous to North America. Archeological evidence traced their first inhabitation back to the Wisconsinan glaciation era some 17,000–25,000 years ago, when there was still a Bering land bridge joining Siberia of Asia and Alaska of North America which could have allowed human migration all the way from Africa to the America continents[1] [Figure 1]. Recent study by Amos and Hoffman[2] using microsatellite loci genotyping also supported this theory. The Constitution Act of Canada in 1982[3] defines three groups of Aboriginal people: The First Nations or Indian Bands who generally inhabit lands called “reserves;” the Inuit who locate in Nunavut, Northern Territories and Labrador; and the Métis Communities. Each group possess a different language, culture, and spiritual beliefs. According to the 2011 National Household Survey of Canada, about 1.4 million people were registered as Aboriginals (male: female ratio 1:1.05), comprising 4.3% of the total population in Canada. Among them, 60.8% were First Nations, 32.3% Métis, and 4.2% Inuit.[4] While 84% of them speak English and 4.7% speak French, only 17.2% have knowledge of an Aboriginal language.[5] Compared to non-Aboriginal Canadians, the Aboriginal population in 2011 is a very youthful with 56% under the age of 25, with a rate of growth of twice as fast as their Canadian cohorts.[4] This trend is projected to continue to 2026 and contrast vividly with the aging population of the Canadians, as shown by the differing age-gender pyramids [Figure 2].
Figure 1.
The out-of-Africa theory for human migration. KYA: Kilo-years. Red circle indicate the Bering land bridge which existed during the Wisconsinian era some 20,000 years ago, allowing passage all the way to Alaska of North America. Source: Stanyon et al.[1]
Figure 2.
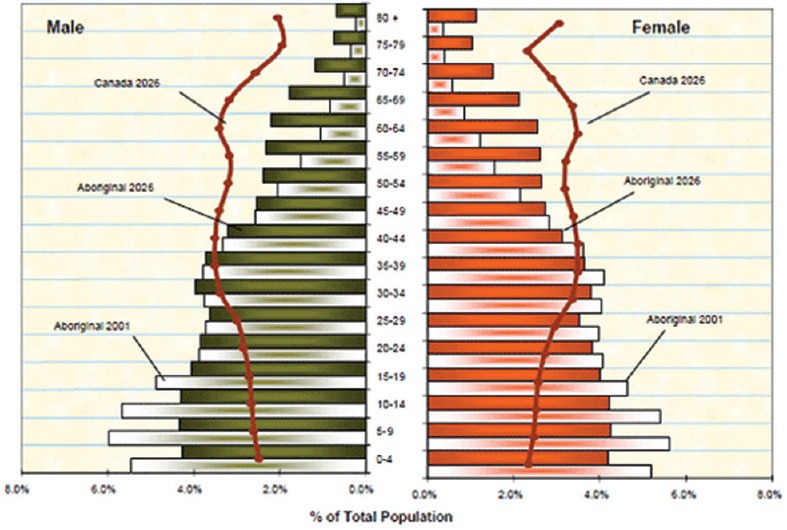
Age-gender pyramids of Aboriginal versus non-Aboriginal population of Canada projected from 2001 to 2026. Source: Aboriginal Affairs and Northern Development Canada
Diabetes in Aboriginals of Canada: Prevalence, risks factors, genetic predisposition (thrift genes), enhanced morbidity and mortality
Back in 1937, diabetes mellitus was not a detectable disease among the 1500 First Nations people who were surveyed for tuberculosis in Saskatchewan.[6] However, over the next 60 years, diabetes has emerged to be the most important noncommunicable disease for Canadian Aboriginal population.[7] Overall, the crude prevalence for diabetes ranges from 2.7% to 19%, which is 3–5 times higher than non-Aboriginal cohorts. In Northern Quebec, the age-adjusted prevalence even approached an alarming 29%.[8] First Nations aboriginals have a much higher prevalence (15.3%) than the Métis (5.8%) and Inuit (4.3%).[9] Aboriginal females are more likely to have diabetes than males, a reverse trend as compared to non-Aboriginal Canadians. By region, the First Nations in the James Bay Cree region have the highest prevalence of diabetes, followed by Northern Alberta and the British Columbia.[9] Oster et al. looked at the incidence of diabetes in Aboriginal youth <20 years of age in Alberta and reported an increasing trend from 1997 to 2005.[10]
The alarming rise of diabetes among the Aboriginal population in Canada has been attributed to various genetic, biological, environmental, and lifestyle risk factors.
Genetic and biological factors
The “thrifty gene theory” proposed by Neel in 1962[11] has remained an attractive hypothesis to explain the propensity of Aboriginals to develop diabetes mellitus and obesity. Throughout centuries, Aboriginal people maintain a hunter-gather lifestyle with no guarantee of the constant food supply, and hence via evolution they acquire this thrifty gene to conserve energy through periods of starvation and environmental hardships. This “thrifty gene” theory was later modified to the “thrifty phenotype” theory by Hales and Barker[12] which necessitated (i) a period of maternal malnutrition during pregnancy to switch on the subsequent thrift mechanisms in the fetus and, (ii) lack of starvation and exercise after birth hence predispose to obesity and diabetes. Hegele et al. identified a gene mutation (G319S) in the hepatic nuclear factor-1 alpha which translates to decreased insulin sensitivity.[13,14] This thrifty phenotype is exclusively found in the Oji-Cree Aboriginal population in Ontario and Manitoba,[15] with a 97% specificity and 95% predictability for developing Type 2 diabetes mellitus (T2DM) by 50 years of age.[14] However, this hypothesis has been challenged vigorously in view of the fact that fetuses born to mothers with T2DM have excess energy in utero still become overweight and develop T2DM themselves.[15] Apart from genetic factors, biological factors are also important. The female gender per se carries a higher risk for developing diabetes among aboriginal Canadians, and gestational diabetes is 4–10 times more prevalent than non-Aboriginal cohorts.
Environmental factors
Historically, Aboriginals live and thrive in their own ecosystem with equilibrium and sustainability in terms of food supply, transport, accommodation, and health. With the influence of modern civilization, the social and health conditions of the Aboriginal start to change and segregate according to the area they reside, whether it is on-reserve (rural) or off-reserve (urban). In other words, when food supply, mobility and access to health care are coupled to education levels, employment and earning potential of modern society, Aboriginals become disadvantaged and discriminated. To make things worse, modernization often erode into their natural ecosystem and reduce their hunting, fishing, and harvesting abilities and rendering them reliant on processed food, often of low quality due to their financial affordability. Modification of their habitat with motor-vehicle transport also drastically reduce their hunter-gather style of physical activities, which further contribute to obesity and hence T2DM.
Lifestyle factors
In the past 50 years, the influence of non-Aboriginal Canadian living has a profound impact on the Aboriginal population in terms of diet, physical activities, and other social habits. Locally harvested food (traditional food) in Aboriginal communities are typically rich in protein, essential micronutrients, vitamins, and polyunsaturated fatty acids - in particular, the long-chain omega-3 fatty acids, which guard against the development of diabetes, obesity, and cardiovascular morbidity.[16] However, the supply of traditional food to Aboriginals is often inadequate. Egeland et al. found that food insecurity occurs in 62.6% of Inuit from 36 Arctic communities in 2007 to 2008,[17] which explains why Aboriginal people often resort to ready-made and processed food in stores which are of poorer nutritional value, containing lower fibers, lower micronutrients, higher content of salt and refined sugar. Depending on the actual community and habitat, fresh fruits, and vegetables may be also a scarcity. Combined with the thrifty gene or thrifty phenotype effect, such unhealthy diet adds significantly to the risks of obesity and diabetes among Canadian Aboriginals. As their lifestyle transition away from the physically demanding hunter-gatherer-harvester, modern day Aboriginals are more sedentary and reliant on motorized transport which drastically reduce their daily level of activities and caloric expenditure. According to the 2008 to 2009 Canadian Community Health Survey and the 2008–2010 First Nations Regional Health Survey, up to 74% of First Nations over the age of 18 reported physical inactivity during leisure time which is much higher than the 49% in non-Aboriginal cohort.[9] This translated to a much higher prevalence of obesity (25–40%) among Aboriginals than the non-Aboriginals (18%).[9]
Challenges of diabetes management among Aboriginals in Canada
It is an alarming fact that health disparities are predominant among Aboriginal population in Canada, which are well-illustrated by the higher prevalence and morbidity/mortality rate of conditions such as diabetes, obesity, and substance dependence. In the past 150 years, the dominance of imperialism and colonialism on Canadian Aboriginal soil had led to varying degree of racial discrimination and social oppression, leaving the roots for health and social inequities in terms of education, employment, housing and other access to social and health-care facilities.[18] Moreover, lack of trust and confidence in Canadian government still prevails among Aboriginal population which often leads to delayed efforts and unfruitful cooperation. An excellent example is the on-going stalemate of the Giant Mine between the Canadian Government and the First Nations in Northern Territories of Canada.[19,20]
Aboriginal Diabetes Initiatives
Background and history
In the face of the increasing epidemic of diabetes among Canadians and its toll on direct and indirect economic costs, the Government of Canada launched the Canadian Diabetes Strategy (CDS) in 1999, which was a 5-year program with C$115 million of funding. The Aboriginal Diabetes Initiative (ADI) was one of the four key components of CDS; the other three were: Prevention and Promotion of Diabetes, National Diabetes Surveillance System and National Coordination.[21] ADI was allocated C$58 million in the first 5 years (ADI Phase 1) with initial objectives mirroring that of CDS. Due to encouraging results, mainly in terms of coverage of up to 600 Aboriginal communities, ADI was funded with C$190 million for another 5 years (ADI Phase 2, from 2005 to 2010), to reinforce on-going activities and to expand four other key areas of services. In 2010, The Government of Canada injected another $275 million for a Phase 3 ADI with 4 new targeted areas of diabetes prevention and health promotion.[22]
Goals and objectives
In line with CDS, the overall objective of ADI was to improve the health of the Aboriginals in the context of diabetes, aiming to reduce the incidence and prevalence of the disease, minimize the contributing risks factors and mitigate the complications due to diabetes.
Developed pari passu with CDS, Phase 1 of ADI aimed to develop awareness and understanding of diabetes as the cornerstone to future health promotion and disease prevention programs in Aboriginal populations.
For Phase 2 of ADI, four main goals were laid out:
Disease prevention and health promotion: Community-based and culturally-sensitive activities such as berry picking, walking, dancing, picnic, and gardening. to increase physical activities; organizing community kitchens and cooking classes to promote adherence to traditional food instead of processed and fast food; removal of vending machines in schools that sell soft-drinks and snacks with high sugar and saturated fats
Diabetes screening and treatment: Better incentives to local health providers and mobile screening initiatives were launched in four provinces (Alberta, British Columbia, Manitoba, and Quebec) to enhance early detection of diabetes and screening for possible disease complications of the eyes, heart, kidneys, and limbs
Workforce training and capacity building: More than 330 community diabetes prevention workers were trained to work independently and also in partnership with other allied health professionals; continued education were also provided to other health-care providers who manage diabetes in Aboriginals
Research and disease surveillance: ADI established close liaison with relevant organizations bodies to maintain active research and also support studies to monitor and evaluate the various on-going programs and activities of ADI.
The current ADI Phase 3 focus on four areas:
Extending prevention initiatives to children, youth, parents, and families
Preventing pregestational and gestational diabetes
Enhance food security and improve access to more nutritious traditional food
Reinforce practice guidelines and disease management for health-care providers.
Partnership and collaborative framework
The historical dominance of British imperialism and colonialism on Canadian Aboriginal soil in the last 150 years significantly impacted the Aboriginal culture. In view of this, ADI adopted a collaborative network approach which embraced multiple partners from federal departments, provincial governments to the Aboriginal organizations and communities. The philosophy is simple - to work for and to work with the Aboriginals. For the current Phase 3, to ensure delivery of services to First Nations, Inuit and Métis that live outside their traditional communities, partnerships had been established with four representative organizations: Assembly of First Nations, Inuit Tapirit Kanatami, Congress of Aboriginal Peoples and the Métis National Council. To oversee the efficient running and maintain standards of diabetic programs and services, ADI maintain strong and continued linkages with organizations like the First Nations Diabetes Working Group, the Canadian Diabetes Association, the Inuit Diabetes Network, the National Aboriginal Diabetes Association and the CDS. To ensure comprehensive coverage of services and activities, ADI established a First Nations and Inuit Health region in every Province/Territory in Canada: Pacific, Saskatchewan, Ontario, Alberta, Manitoba, Quebec, Atlantic, and Northern Territory. Aboriginal communities and organizations are invited to submit plans or proposals to apply for funding from ADI to enable community-based programs and activities that are in line with the current ADI initiatives. The proposals also need to define the target populations and address the needs; involve the community members from design, development, planning to implementation and finally, reinforce partnerships between various stakeholders and beneficiaries.[22]
Impact of Aboriginal Diabetes Initiative on Health of Population
During the three phases of ADI, multiple programs had been launched in various Aboriginal communities of difference provinces in Canada. Suffice to say, so far the impact of these ADI activities has been predominantly positive and encouraging.
Regarding disease screening
In terms of screening of diabetes and its complications, the Screening for Limb, Eye, Cardiovascular and Kidney Project (SLICK) for Aboriginals with T2DM in Alberta is an excellent example. With ADI funding, two mobile units (SLICK Vans) were equipped with necessary laboratory and ophthalmological equipment. From December 2001 to July 2003, trained medical personnel traveled in these two vans to 44 First Nations communities in the province of Alberta and screened 1151 patients with T2DM for diabetic complications. At the same time, Clinical Practice Guidelines were implemented as per the Canadian Diabetes Association. There were modest improvements in the first follow-up at 6–12 months.[23] This SLICK project continued longitudinally and by its 6th year, 2102 patients were registered, and there were statistically significant improvement in most of the outcome measures, notably body mass index, HBA1c, waist circumference, total cholesterol, blood pressure, foot, and kidney complications.[24]
Regarding healthy eating and cooking
In terms of programs for promoting healthy diet, the Food Skills for Families Program (FSFP) provides a very successful role model. It was administered by the Canadian Diabetic Association and funded by the British Columbia Ministry of Health via the ADI (Pacific Region). This FSFP is an on-going program which was initially launched in September 2008. It trained community facilitators who deliver a 6 weeks’ program with talks and demonstrations to schools and communities regarding knowledge of healthy food and cooking.[25] There are three main goals in this program: (i) To impart nutritional knowledge and cooking skills to Aboriginal population at risks of diabetes; (ii) to build up capacity within the target communities by training community facilitators who reach out to deliver the program; (iii) to enrich existing food security and children nutritional programs both in community and schools settings.[26] By June 2013, there are 328 community facilitators who had delivered 660 programs which had benefited up to 16,000 Aboriginal adults and children in total. To ensure sustainability, there is the Train-the-Trainer program which involved master trainers who are dietitians. To provide ease of reference of core knowledge, an on-line curriculum was developed with supply of DVD version on request.[26] The FSFP was periodically evaluated basing on pre- and post-questionnaires to the program participants, combined with feedback from community facilitators, master trainers, program administrators, partners, collaborators, and other stakeholders.[25,26,27,28] In the evaluation reports published in March 2010[27] and October 2012,[26] ADI concluded that in all three Phases of the FSFP, significant changes have been observed among the program participants both personally and socially. At the personal level, participants reported an increased tendency to eat 5–7 servings of fruits and vegetables a day, as they had increased their knowledge to do so [Figure 3]. At the same time, they reported more intake of whole grain food and lesser consumption of sugar, salt, and fat in general.[26,27] Building on more knowledge of healthy diet, participants also incorporate more healthy recipes with lower fat [Figures 4 and 5]. Moreover, participants also feel significantly more confident in reading food labels, cooking new foods, carrying out basic food safety procedures, and keeping their diet healthy [Figure 6].
Figure 3.
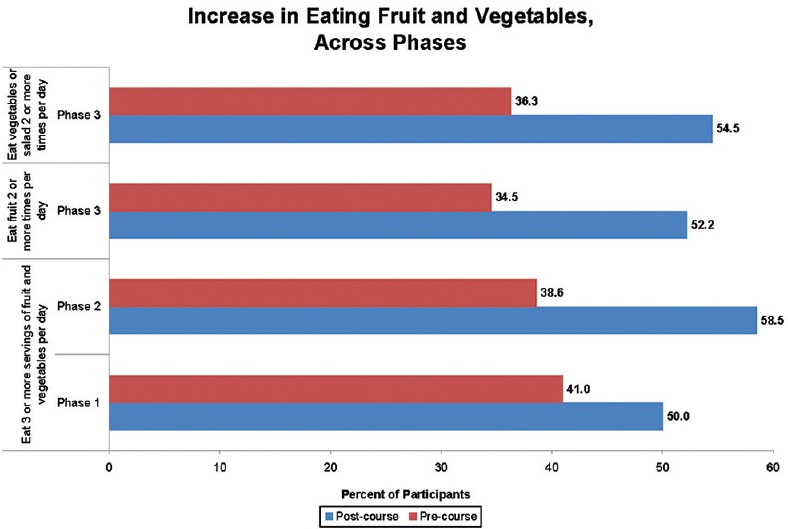
Impact of all 3 Phases of the Food Skills for Families Program in increasing fruit and vegetables intake among participants. Source: Canadian Diabetes Association
Figure 4.
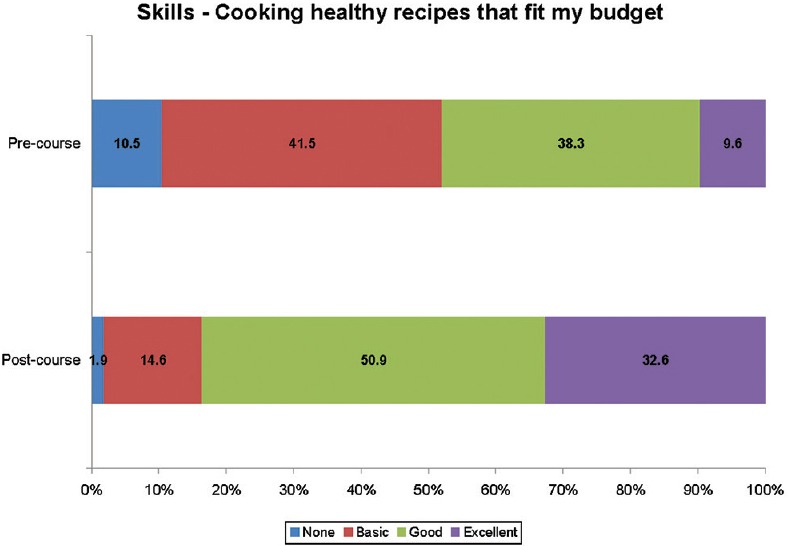
Incorporation of more healthy recipes after attending the Food Skills for Families Program. Source: Canadian Diabetes Association
Figure 5.
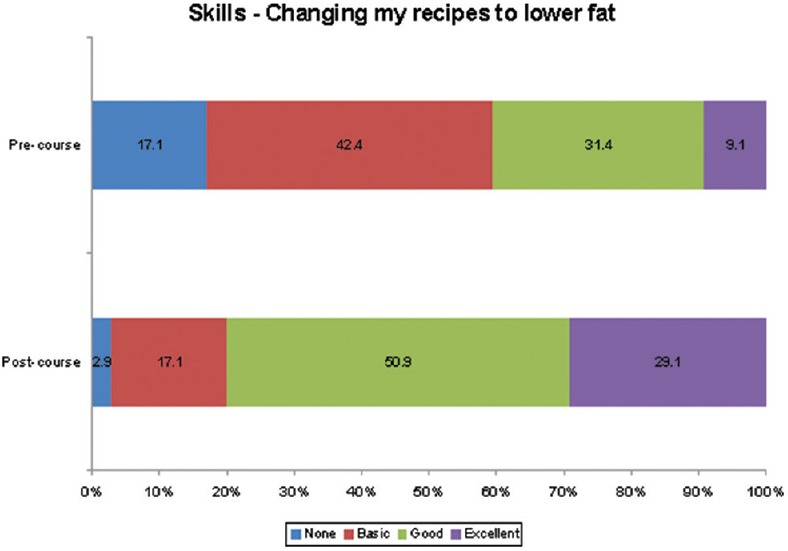
Participants’ change to low-fat recipes after attending the Program. Source: Canadian Diabetes Association
Figure 6.
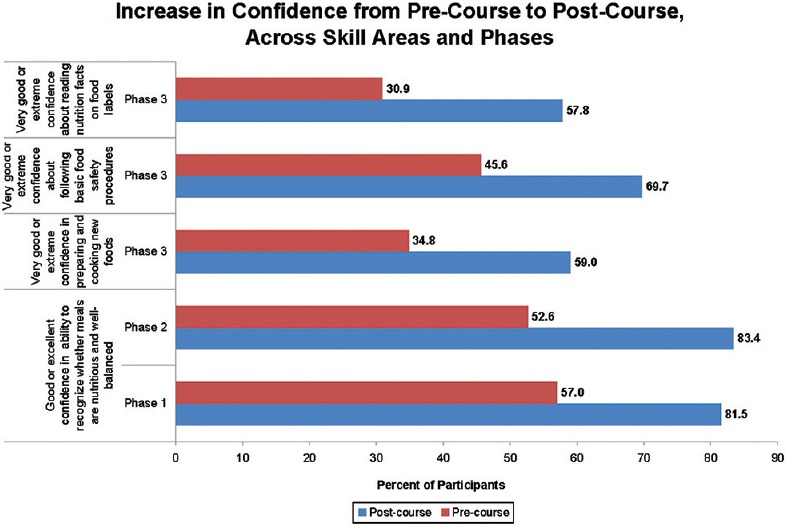
Significant increase in confidence regarding reading food labels, cooking new foods, following food safety procedures and keeping healthier diets. Source: Canadian Diabetes Association
Impact of Aboriginal Diabetes Initiative on Health Care Inequities
Improving access to health care and education
By providing both hardware and software (qualified personnel) in mobile units to administer screening and medical advice on the site, the SLICK program directly eliminate health-care inequities due to geographic and accessibility barrier for Aboriginal patients with diabetes. In sending community facilitators to target Aboriginal communities and schools, the FSFP overcame health education inequities due to access and networking barriers. Before attending the FSFP, Aboriginal participants reported the leading four common barriers to healthy eating as (i) lack of healthy recipes; (ii) healthy food too costly; (iii) lack of knowledge regarding healthy cooking methods; (iv) lack of knowledge regarding healthy food. After attending the program, the percentage of participants reporting the same four barriers drop drastically except (ii) healthy food too costly.
Improving social networking, community participation, and family cohesion
The mobile unit from SLICK acts as a shuttle to reduce social and cultural gaps between Aboriginal communities and the government health-care providers. This helped eliminate the social inequities due to community segregation and cultural isolation which can lead to general distrust and alienation. In the review report of FSFP, there was a consensus that the program drastically enhanced social connections and interactions between different communities and parties, allowing participants to make new friends, exchange telephone numbers, and invite other participants to their homes to cook.[27] Moreover, participants reported being more motivated in promoting healthier lifestyles to their children and family members with engagement in more physical exercises and healthy cooking. This helps to reinforce the core values of families and reduce social inequities due to poor family dynamics.
Conclusion
In Canada, the incidence and prevalence for diabetes mellitus continue to rise with a higher preponderance among the Aboriginal population. Due to various genetic and biological factors, Aboriginals with diabetes are also more predisposed to suffer from complications of diabetes. This is compounded by social disparities as a result of political oppression and discrimination from the historical government which led to significant inequities in health-care access. To ameliorate the situation, Government of Canada launched the ADI to enhance earlier detection and prevention of diabetes, better management of disease, and higher vigilance in complications screening. Since its inception in 1999, ADI had achieved the major objectives for diabetic patients in Aboriginal communities through the many programs and activities over all provinces of Canada. At the time of writing, ADI is now in its 3rd round of operation with an annual funding of C$50 million till 2015. From a public health perspective, ADI also made a significant impact in ameliorating health inequities among Aboriginals, as illustrated by the SLICK and FSFP Programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stanyon R, Sazzini M, Luiselli D. Timing the first human migration into Eastern Asia. J Biol. 2009;8:18. doi: 10.1186/jbiol115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amos W, Hoffman JI. Evidence that two main bottleneck events shaped modern human genetic diversity. Proc Biol Sci. 2010;277:131–7. doi: 10.1098/rspb.2009.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Constituion Act. 1982. [Last assessed: 2016 Jun 30]. Available from: http://www.uottawa.ca/constitutional-law/ca1982.html .
- 4.Ottawa: 2013. [Last accessed on 2014 Jan 01]. Statistics Canada. Canada (Code 01) (Table). National Household Survey (NHS) Aboriginal Population Profile. 2011 National Household Survey. Statistics Canada Catalogue No. 99-011-X2011007. Available from: http://www12.statcan.gc.ca/nhs-enm/2011/dp-pd/aprof/index.cfm?Lang = E . [Google Scholar]
- 5.Canada: Statistics Canada; 2013. [Last assessed on 2016 Jun 30]. 2011 National Household Survey. Aboriginal Peoples in Canada: First Nations People, Métis and Inuit. Available from: http://www.statcan.gc.ca/daily-quotidien/130508/dq130508a-eng.htm?HPA . [Google Scholar]
- 6.Chase LA. The trend of diabetes in Saskatchewan, 1905 to 1934. Can Med Assoc J. 1937;36:366–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Young TK, Reading J, Elias B, O’Neil JD. Type 2 diabetes mellitus in Canada's first nations: Status of an epidemic in progress. CMAJ. 2000;163:561–6. [PMC free article] [PubMed] [Google Scholar]
- 8.Haddad PS, Musallam L, Martineau LC, Harris C, Lavoie L, Arnason JT, et al. Comprehensive evidence-based assessment and prioritization of potential antidiabetic medicinal plants: A case study from canadian Eastern james bay cree traditional medicine. Evid Based Complement Alternat Med 2012. 2012:893426. doi: 10.1155/2012/893426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canada: 2011. [Last accessed on 2016 Jul 17]. PHAC. Diabetes in Canada: Facts and Figures from a Public Health Perspective. Available from: http://www.phac-aspc.gc.ca/cd-mc/publications/diabetesdiabete/facts-figures-faits-chiffres-2011/highlightssaillants-eng.php#chp6 . [Google Scholar]
- 10.Oster RT, Johnson JA, Balko SU, Svenson LW, Toth EL. Increasing rates of diabetes amongst status Aboriginal youth in Alberta, Canada. Int J Circumpolar Health. 2012;71:1–7. doi: 10.3402/ijch.v71i0.18501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neel JV. Diabetes mellitus: A “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet. 1962;14:353–62. [PMC free article] [PubMed] [Google Scholar]
- 12.Hales CN, Barker DJ. Type 2 (non-insulin-dependent) diabetes mellitus: The thrifty phenotype hypothesis. Diabetologia. 1992;35:595–601. doi: 10.1007/BF00400248. [DOI] [PubMed] [Google Scholar]
- 13.Hegele RA, Cao H, Harris SB, Hanley AJ, Zinman B. The hepatic nuclear factor-1alpha G319S variant is associated with early-onset type 2 diabetes in Canadian Oji-Cree. J Clin Endocrinol Metab. 1999;84:1077–82. doi: 10.1210/jcem.84.3.5528. [DOI] [PubMed] [Google Scholar]
- 14.Hegele RA, Zinman B, Hanley AJ, Harris SB, Barrett PH, Cao H. Genes, environment and Oji-Cree type 2 diabetes. Clin Biochem. 2003;36:163–70. doi: 10.1016/s0009-9120(03)00004-3. [DOI] [PubMed] [Google Scholar]
- 15.Millar K, Dean HJ. Developmental origins of type 2 diabetes in aboriginal youth in Canada: It is more than diet and exercise. J Nutr Metab 2012. 2012:127452. doi: 10.1155/2012/127452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuhnlein HV, Receveur O, Soueida R, Egeland GM. Arctic indigenous peoples experience the nutrition transition with changing dietary patterns and obesity. J Nutr. 2004;134:1447–53. doi: 10.1093/jn/134.6.1447. [DOI] [PubMed] [Google Scholar]
- 17.Egeland GM, Johnson-Down L, Cao ZR, Sheikh N, Weiler H. Food insecurity and nutrition transition combine to affect nutrient intakes in Canadian arctic communities. J Nutr. 2011;141:1746–53. doi: 10.3945/jn.111.139006. [DOI] [PubMed] [Google Scholar]
- 18.Frohlich KL, Ross N, Richmond C. Health disparities in Canada today: Some evidence and a theoretical framework. Health Policy. 2006;79:132–43. doi: 10.1016/j.healthpol.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Jardine CG, Banfield L, Driedger SM, Furgal CM. Risk communication and trust in decision-maker action: A case study of the Giant Mine Remediation Plan. Int J Circumpolar Health. 2013;72 doi: 10.3402/ijch.v72i0.21184. doi: 10.3402/ijch.v72i0.21184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Banfield L, Jardine CG. Consultation and remediation in the North: Meeting international commitments to safeguard health and well-being. Int J Circumpolar Health. 2013;72 doi: 10.3402/ijch.v72i0.21231. doi: 10.3402/ijch.v72i0.21184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stewart P. Building a National Diabetes Strategy: A Strategic Framework. Canada: Ministry of Health of Canada; 2005. [Last assessed on 2016 Jun 30]. Available from: http://www.publications.gc.ca/collections/collection_2008/phac-aspc/HP5-5-2-2005E.pdf . [Google Scholar]
- 22.Health Canada. Aboriginal Diabetes Initiatives Program Framework; 2010-2015. [Last accessed on 2014 Jan 03]. Available from: http://www.hc-sc.gc.ca/fniah-spnia/pubs/diseases-maladies/_diabete/2010-2015-frame-cadre/index-eng.php .
- 23.Virani S, Strong D, Tennant M, Greve M, Young H, Shade S, et al. Rationale and implementation of the SLICK project: Screening for Limb, I-Eye, Cardiovascular and Kidney (SLICK) complications in individuals with type 2 diabetes in Alberta's First Nations communities. Can J Public Health. 2006;97:241–7. doi: 10.1007/BF03405595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oster RT, Shade S, Strong D, Toth EL. Improvements in indicators of diabetes-related health status among first nations individuals enrolled in a community-driven diabetes complications mobile screening program in Alberta, Canada. Can J Public Health. 2010;101:410–4. doi: 10.1007/BF03404863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canadian Diabetes Association. Food Skills for Families. Evaluation Report Phase Four to Seven. 2011. [Last assessed on 2016 Jun 30]. Available from: http://www.foodskillsforfamilies.ca/Food_Skills_for_Families_Evaluation_Report_March_2011.pdf .
- 26.Canadian Diabetes Association. Food Skills for Families. ADI Evaluation Report, 2011-2012. 2012. [Last assessed on 2016 Jun 30]. Available from: http://www.foodskillsforfamilies.ca/wp-content/uploads/2011/03/Food-Skills-for-Families-ADI-Evaluation-Report_October-2012.pdf .
- 27.Canadian Diabetes Association. Food Skills for families. Final Evaluation Report Mar 2010. [Last assessed on 2016 Jun 30]. Available from: http://www.foodskillsforfamilies.ca/wp-content/uploads/2011/07/Food-Skills-for-Families_Final-Evaluation-Report_Low-Res.pdf .
- 28.Canadian Diabetes Association. Food Skills for families. Evaluation Report July 2012-June 2013. [Last assessed on 2016 Jun 30]. Available from: http://www.foodskillsforfamilies.ca/wp-content/uploads/2013/11/Food-Skills-for-Families_WEB.pdf .



