Abstract
Introduction:
National AIDS Control Organization (NACO) has expanded the reach of anti retroviral therapy (ART) to combat the epidemic of HIV/AIDS in India which has one of the largest populations of people living with HIV/AIDS (PLWHA) in the world. One of the major challenges related to ART is a lifelong commitment by patients to adhere diligently to daily medication dosing schedules and scheduled visits to the ART center. Hence, the current study is carried out to assess the drug adherence rate and loss to follow-up (LFU) among PLWHA attending ART centre of a tertiary care hospital in Western India.
Materials and Methods:
The current cross-sectional study was carried out using medical records of all patients registered at ART Center, Shree Sayaji General Hospital, Vadodara after taking Ethical Clearance from Local IRB. LFU was classified according to NACO guidelines. Data were collected using a standardized data extraction form as per NACO treatment card. Data entry and analysis were performed using Epi Info software.
Results:
Of 755 PLWHA registered at ART center, 534 (70.7%) subjects were alive on ART, 61 (8%) were transferred out, 68 (9%) died, and 92 (17%) were LFU. Nearly, 57% PLWHA have drug adherence rate of more than 95%. Education status of the participant showed independent and significant association with drug adherence.
Conclusion:
This study showed 57.3% were adherent to ART among PLWHA, whereas 17.22% were lost to follow-up. Hence, there is a need to emphasize on increasing drug adherence rate and on outreach activities to combat LFU.
Keywords: ART, drug adherence rate, loss to follow-up, people living with HIV/AIDS
Introduction
Large-scale programs to provide anti retroviral therapy (ART) have expanded to combat the epidemic of HIV/AIDS in India which is third among the populations of HIV-positive cases in the world.[1] However, the expansion ART programs have also brought challenges. One of the major challenges relates to retention of patients on ART. Successful implementation of an ART program hinges on a lifelong commitment by patients to adhere diligently to daily medication dosing schedules and scheduled visits to the ART center. A systematic review assessing the rates of follow-up in patients undergoing ART across sub-Saharan Africa reported approximately 25% of patients lost to follow-up 1 year after initiation of ART and the rate of lost to follow-up was 40% after 2 years.[2] Patients lost to follow-up (i.e. discontinuing treatment) are at high risk of more opportunistic infections, illness, and death. They also often reflect patients with advanced disease who, untreated, can further spread infection. However, despite the critical importance of lost to follow-up as a public health issue to combat the epidemic of HIV/AIDS, it is surprising that it has received very little attention.[3] There have been studies to determine the rates of follow-up and the reasons for lost to follow-up in lower income countries across the world which shows the seriousness of the issue.[3,4] Nevertheless, in case of India, reliable data on rates of lost to follow-up or the reasons for lost to follow-up is unavailable. Results across studies assessing the rate of follow-up in India are conflicting. The current study is carried out to study the rate of drug adherence and loss to follow-up (LFU) and factors affecting drug adherence among people living with HIV/AIDS (PLWHA) attending ART Centre of a Tertiary Care Government Hospital in Western India.
Materials and Methods
The study was carried out after taking permission from the Local Institutional Ethics Committee and Gujarat State AIDS Control Society. This cross-sectional study was carried out from August 2011 to November 2011. Shree Sayaji General Hospital (SSGH) is the largest Tertiary Care Government Hospital in Central Gujarat and third largest hospital in Western India. All PLWHA registered at ART Centre in this SSGH, from April 01, 2010, to March 31, 2011, were enrolled in the study. A retrospective chart review of all consecutive patients initiating ART at the primary ART Center in Vadodara was done. PLWHA was identified with a case or identification number only.
Data from the medical chart of the patients were collected using a standardized data extraction form based on the National AIDS Control Organization (NACO) treatment card which broadly includes patient demographics, previous and current medical history, 1st day of treatment, and date of the last visit for collection of medications. As per NACO treatment card entry point has been recorded as the mechanism by which client was referred to ART center whether the client was referred from Integrated Counselling and Testing Center, Revised National Tuberculosis Control Programme/Tuberculosis, Outpatient Department of the Hospital, PPTCT, STI Clinic, outreach workers, nongovernmental organization, or by private practitioner. Data were entered and analyzed using Epi Info Software version 6.0 (Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia (USA).).[5]
According to the current treatment scheme patients undergoing ART, visit the ART center once every month to collect their medication for the month. Patients not showing up at the clinic to collect their medications for three consecutive months were classified as lost to follow-up. Drug adherence among PLWHA is divided into three categories. Category A: ≥95% drug adherence missed 3 pills a month. Category B: 80–95% drug adherence where 3–11 pills missed a month and Category C: <80% drug adherence where more than 11 pills missed in a month.[6] Factors affecting drug adherence among PLWHA were studied by putting the variables in multiple logistic regression model in which P < 0.05 is considered to be statistically significant.
Results
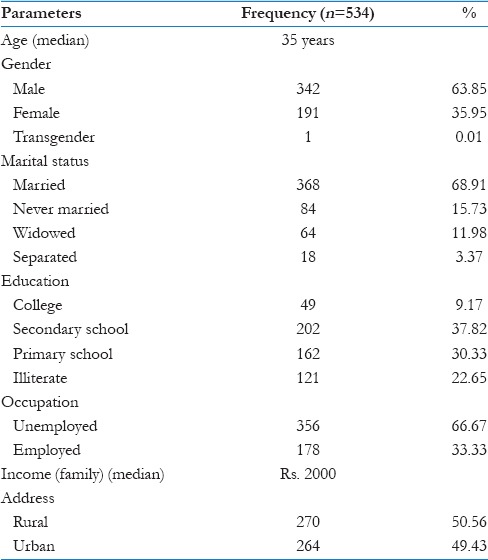
Out of 755 PLWHA registered at ART center, 534 (70.7%) subjects were actively undergoing ART, 61 (8%) were transferred out, 68 (9%) died, and 92 (17%) were LFU. The average duration of LFU patients on ART was 2 months before they became LFU. The sociodemographic profile of 534 PLWHA actively undergoing ART is as shown in Table 1. The median age of PLWHA was 35 years, and nearly 64% were males. Nearly, 69% were married and 23% were illiterate. Majority (67%) of them were unemployed with median family income of Rs. 2000/month. Half of the PLWHA were from rural areas and a half from the urban areas.
Table 1.
Sociodemographic profile of people living with HIV/AIDS attending antiretroviral treatment center
As shown in Figure 1, the drug adherence rate among PLWHA was 306 (57.3%) PLWHA were in Category A followed by 158 (29.6%) PLWHA were in Category B while 70 (13.1%) PLWHA were in Category C.
Figure 1.
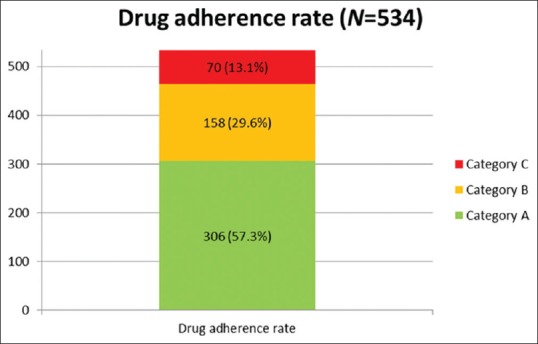
Drug adherence rate among people living with HIV/AIDS attending ART center
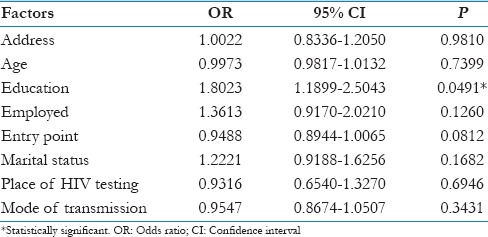
Table 2 shows the multivariate analysis related to factors affecting drug adherence rate among PLWHA using logistic regression model, in which address, age, employment status, entry point, marital status, place of HIV testing, and mode of transmission were not found to be associated with drug adherence. However, education status of the participant showed independent and significant association with drug adherence. Those who were literate were 1.8 times (odds ratio = 1.8, 95% confidence interval: 1.8–2.50, P < 0.05) adherent to ART as compared to illiterate.
Table 2.
Multivariate analysis for factors affecting drug adherence among people living with HIV/AIDS
Discussion
Based on HIV Sentinel Surveillance 2008–2009, it is estimated that India has an adult HIV prevalence of 0.31% (0.25% among women and 0.36% among men).[7] In Gujarat, estimated HIV prevalence is 0.37% in total while 0.30% among females and 0.44% among males.[8] India's National ART Programme was launched on April 01, 2004 under the NACO, as an initiative of the Ministry of Health and Family Welfare of the Government of India and the introduction of antiretroviral therapy (ART) at free of cost at all ART centers has also been initiated. However, now, the question arises of lifelong commitment by PLWHA to adhere diligently to daily medication dosing schedules and scheduled visits to the ART center.
A total of 755 patients were registered during a period of 1 year, out of which 70% were actively undergoing ART, 17% were LFU, 8% died, and 9% transferred out. Similar baseline characteristics were also observed by Sharma et al. in a Tertiary Care ART Centre in North India.[9] While a systematic review assessing the rates of follow-up in patients undergoing ART across sub-Saharan Africa also reported approximately 25% LFU within 1 year of initiation of ART.[10]
In the current study, the drug adherence rate (Category A) among PLWHA attending the ART Centre of Tertiary Care Hospital in Gujarat was found to be 57.3%. Whereas Peltzer et al. in South Africa and Bijal et al. in private clinics of Mumbai found as high as 70.8% and 73% drug adherence rate, respectively.[4,11] However, in many studies cost has been well-documented barrier to drug adherence because of high cost of ART in private sectors giving a load to the out of pocket expenditure to PLWHA.[12,13,14]
In India, few studies have identified factors associated with adherence to ART. In this study, we have tried to find out the sociodemographic factors associated with drug adherence. Literacy status of the patient was found to be significantly associated with drug adherence with AOR of 1.8, which is comparable to studies conducted by Kleeberger et al. and Wasti et al.[15,16] Contradictory to this, Sarna et al. in Pune and New Delhi; and Achappa et al. in South India found literacy significantly associated with drug adherence in bivariate analysis but not in multivariate analysis.[17,18]
Being a cross-sectional study, this research has its own limitations. Since, it was not our main objective, so we have tried to find relation only between drug adherence and sociodemographic characteristics, but there are many other factors associated with drug adherence which needs to be explored.
Conclusion
This study observed 57.3% drug adherence rate and 17.22% LFU among PLWHA attending ART Centre in Tertiary Care Government Hospital in Western India. As government programs in India expand access to free ART for PLWHA, the development of validated low-cost interventions that optimize adherence is quite essential now.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rassool GH. Current issues and forthcoming events: HIV infection rates decrease in several countries, but global number of people living with HIV continues to rise. J Adv Nurs. 2006;54:132. doi: 10.1111/j.1365-2648.2006.03827.x. [DOI] [PubMed] [Google Scholar]
- 2.Brinkhof MW, Dabis F, Myer L, Bangsberg DR, Boulle A, Nash D, et al. Early loss of HIV-infected patients on potent antiretroviral therapy programmes in lower-income countries. Bull World Health Organ. 2008;86:559–67. doi: 10.2471/BLT.07.044248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brinkhof MW, Pujades-Rodriguez M, Egger M. Mortality of patients lost to follow-up in antiretroviral treatment programmes in resource-limited settings: Systematic review and meta-analysis. PLoS One. 2009;4:e5790. doi: 10.1371/journal.pone.0005790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peltzer K, Friend-du Preez N, Ramlagan S, Anderson J. Antiretroviral treatment adherence among HIV patients in KwaZulu-Natal, South Africa. BMC Public Health. 2010;10:111. doi: 10.1186/1471-2458-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atlanta (GA): Centers for Disease Control and Prevention; 2001. Epi Info [A Word Processing Database and Statistical computer Programme for Public Health]. Version 6.04. [Google Scholar]
- 6.National AIDS Control Organization (NACO). Antiretroviral Therapy Guidelines for HIV-Infected Adults and Adolescents Including Post-Exposure Prophylaxis. New Delhi: National AIDS Control Organization (NACO); 2007. [Google Scholar]
- 7.National AIDS Control Organization (NACO). HIV Sentinel Surveillance and HIV Estimation in India 2008-2009: A Technical Brief. New Delhi: National AIDS Control Organization (NACO); 2010. [Google Scholar]
- 8.National AIDS Control Organisation (NACO). NACP Phase III Fact Sheets: State Wise Estimated Prevalence of HIV in India. New Delhi: National AIDS Control Organization (NACO); 2011. [Google Scholar]
- 9.Sharma SK, Dhooria S, Prasad KT, George N, Ranjan S, Gupta D, et al. Outcomes of antiretroviral therapy in a northern Indian urban clinic. Bull World Health Organ. 2010;88:222–6. doi: 10.2471/BLT.09.068759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in sub-Saharan Africa: A systematic review. PLoS Med. 2007;4:e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah B, Walshe L, Saple DG, Mehta SH, Ramnani JP, Kharkar RD, et al. Adherence to antiretroviral therapy and virologic suppression among HIV-infected persons receiving care in private clinics in Mumbai, India. Clin Infect Dis. 2007;44:1235–44. doi: 10.1086/513429. [DOI] [PubMed] [Google Scholar]
- 12.Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: Overview of published literature. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S123–7. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- 13.Byakika-Tusiime J, Oyugi JH, Tumwikirize WA, Katabira ET, Mugyenyi PN, Bangsberg DR. Adherence to HIV antiretroviral therapy in HIV+Ugandan patients purchasing therapy. Int J STD AIDS. 2005;16:38–41. doi: 10.1258/0956462052932548. [DOI] [PubMed] [Google Scholar]
- 14.Safren SA, Kumarasamy N, James R, Raminani S, Solomon S, Mayer KH. ART adherence, demographic variables and CD4 outcome among HIV-positive patients on antiretroviral therapy in Chennai, India. AIDS Care. 2005;17:853–62. doi: 10.1080/09540120500038439. [DOI] [PubMed] [Google Scholar]
- 15.Kleeberger CA, Phair JP, Strathdee SA, Detels R, Kingsley L, Jacobson LP. Determinants of heterogeneous adherence to HIV-antiretroviral therapies in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 2001;26:82–92. doi: 10.1097/00126334-200101010-00012. [DOI] [PubMed] [Google Scholar]
- 16.Wasti SP, Simkhada P, Randall J, Freeman JV, van Teijlingen E. Factors influencing adherence to antiretroviral treatment in Nepal: A mixed-methods study. PLoS One. 2012;7:e35547. doi: 10.1371/journal.pone.0035547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarna A, Pujari S, Sengar AK, Garg R, Gupta I, Dam JV. Adherence to antiretroviral therapy and its determinants amongst HIV patients in India. Indian J Med Res. 2008;127:28–36. [PubMed] [Google Scholar]
- 18.Achappa B, Madi D, Bhaskaran U, Ramapuram JT, Rao S, Mahalingam S. Adherence to Antiretroviral Therapy Among People Living with HIV. N Am J Med Sci. 2013;5:220–3. doi: 10.4103/1947-2714.109196. [DOI] [PMC free article] [PubMed] [Google Scholar]


