Abstract
Introduction:
Improving the quality of life in diabetic individuals is known to reduce morbidity and mortality. We aimed to investigate the quality of life and depression symptomatology situations and the related factors in patients with Type 2 diabetes mellitus (DM) in this study.
Materials and Methods:
In this study, 440 adult patients with Type 2 DM and under treatment admitted to Selcuk University Family Medicine Outpatient Diabetes Education Clinic were included in the study. A questionnaire containing sociodemographic characteristics of the participants, the Short Form 36 (SF-36) quality of life questionnaire was applied with Beck depression inventory face to face interviews.
Results:
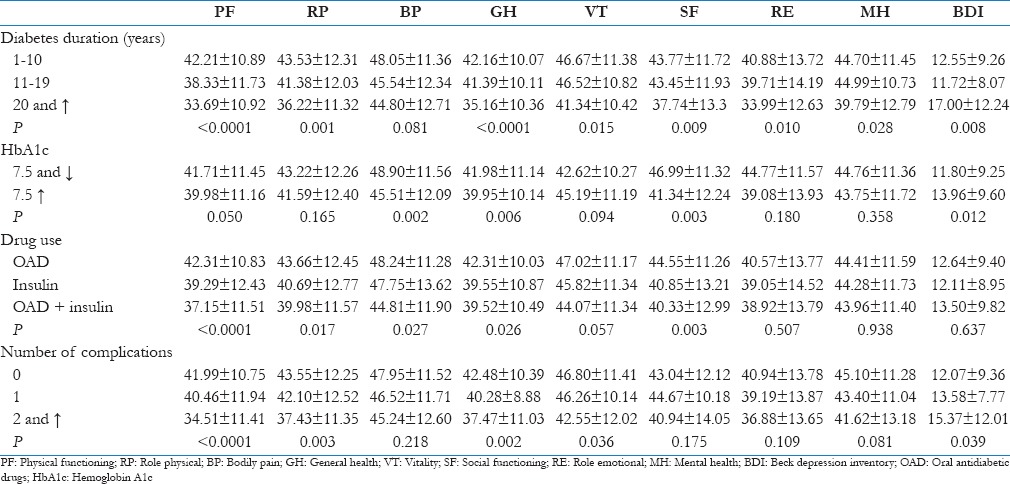
Mean scores of females in all SF-36 subscales were statistically significantly lower than those of male patients. Physical function, physical role limitations, general health, social function, emotional role limitations, and mental health mean scores of the patients with 1–10 years duration of diabetes were found statistically significantly higher than those with 20 years and over duration of diabetes. Physical function, physical role limitations, pain, general health, and social function mean scores in patients using oral antidiabetic drug (OAD) was statistically significantly higher compared to patients using insulin + OAD. The average physical function scores of the patients with no complications were statistically significantly higher than those with two and more complications.
Conclusion:
Quality of life and depression symptomatology are worse in females, the elderly, the overweight, people with lower level of education, in the widowed or divorced, homemakers, those with low incomes, those with longer duration of diabetes, patients using insulin, and those with two or more complications. There are many medical and sociodemographic factors affecting the quality of life and depressive symptomatology in the individuals with diabetes, so both health care workers and patients should pay the necessary attention to this issue.
Keywords: Depression, diabetes, quality of life
Introduction
Diabetes mellitus (DM) is a chronic illness that requires continuing medical care and ongoing patient self-management education and support to prevent acute complications and to reduce the risk of long-term complications.[1,2,3] Diabetes causes morbidity and mortality with acute complications and affects adversely the quality of life with chronic complications. DM is an endocrine disease that can be seen at any age, is spreading rapidly in our country and around the world, costs too high treatment and causes so many problems due to its important complications.[1,2,3]
According to the international diabetes federation (IDF-2013), it was reported that 8.3% Of adults between 20 and 79 years old had diabetes in the world. The number of diabetic patients in the world in 2030 is estimated to reach 366 million. According to TURDEP I and II conducted on a large-scale on the prevalence of diabetes in our country; while the prevalence of diabetes across the country was 7.2% Between 1997 and 1998, it was found that it increased to 13.7% According to a TURDEP II study made 12 years later (2010). According to 2013 IDF, the prevalence in turkey was reported as 14.85%. Aging population and the increase of obesity are thought to be the major causes of diabetes epidemic.[3,4]
DM affects adversely quality of life of the patients, working life, interpersonal relationships, social activities, physical and mental states with its treatment protocols applied, and complications. Diabetes influences physical field with the impaired blood glucose regulation and complications developed, mental area with the problems and increased psychiatric distress emerged, and the social field with the troubles the experienced in social life. Improving the quality of life has been emphasized as a primary goal in the treatment of diabetes for many years. The quality of life in the course of disease in diabetic patients is considered as an important indicator, and it shows the patient's well-being. Therefore, evaluating the quality of life in diabetic individuals is important.[5,6] It is a reality, we daily face very often that patients do not know exactly their treatment, the names of the drugs they use, the effects and side effects of the drugs, and have enough information about the complications of diabetes. In this study, we aimed to evaluate and compare the quality of life, depression symptomatology status and related factors, their general level of knowledge about the diabetes treatment, and the level of knowledge about the disease-related complications and social aspects of the Type 2 diabetic patients admitted to hospital, taking the variables into account such as age, gender, marital status, education level, occupation, and economic status as.
Materials and Methods
Patients
In determining the sample size of our study, the formula prepared “to determine the number of individuals to be sampled whose universe is unknown sampling” was exploited. The formula is in the form of n = t2pq/d2.[7] (1.96)2 × 0.14 × 0.86/(0.05)2 = 185 Type 2 DM individuals have been estimated to be reached as a result of the calculation with 95% confidence level (α = 0.05) considering the incidence of Type 2 DM the Turkey is 13.7%. This study includes 440 patients at the age of 18 and over admitted to Selcuk University Family Medicine Diabetes Education Clinic between November 10, 2014, and March 31, 2015, and diagnosed with Type 2 DM according to the criteria stated in the American Diabetes Association guide (2015).
Exclusion criteria
The patients with a history of cerebrovascular events, those with infection, pregnant women, those with diagnosed liver failure, previously diagnosed malignancy, the patients who did not wish to participate in the study, those in lactation period, and those using anticonvulsant drugs were excluded from the study.
The sociodemographic questionnaire
A questionnaire consisting of 24 questions including the sociodemographic characteristics of the participants was administered with face to face interviews. To determine whether the DM complications exist, an eye exam annually, neurological examinations and glomerular filtration rate (GFR) was calculated with the modification of diet in renal disease formula in terms of nephrology, and complications were determined to scan the data from the patients files retrospectively for the last year. Duration of diabetes and the type of treatment, they patients employed were questioned.
The Short Form 36 quality of life scale
The Short Form 36 (SF-36) quality of life scale is self-rating scale; and it consists of 36 questions that allow the measurement of the eight dimensions of the quality of life including physical functioning, physical role limitations, emotional role limitations, bodily pain, social functionality, general mental health, energy/vitality, and general health. The subscale scores range from 0 to 100, higher scores on health mean a better state, while low scores indicate deterioration in health. It is not possible to calculate the total score of the scale.[6,8,9]
Beck depression inventory
Beck depression inventory (BDI) is a rating scale that can be used to determine the risk of depression and to measure the level and intensity change of depressive symptoms in the healthy and psychiatric patient groups. The scale includes a total of 21 questions. Each question is given 0–3 points, and the total score is obtained with their addition. The total score ranges from 0 to 63. The cut-off point of the scale is set as 17 in Turkish validity and reliability study.[10]
Ethics
This study approved by the decision of the Ethics Committee of Selcuk University Faculty of Medicine dated November 4, 2014, and number 2014/285 was conducted at Selcuk University Family Medicine Outpatient Diabetes Education Clinic between November 10, 2014, and March 31, 2015. An informed consent from in line with the World Medical Association's Declaration of Helsinki was obtained from each participant before the study.
Statistical analysis
All the data collected were evaluated by SPSS 16.0 statistics package program (SPSS Inc., Chicago, IL, USA). Numbers, percentages, means, and standard deviation were used in the evaluation of the data. P < 0.05 was considered significant. Chi-square test, ANOVA test, and Student's t-test were conducted between the groups by handing out the frequency distribution of categorical data. Pearson correlation analyses were used to determine the relation between the numerical variables. Correlation coefficient (r); from 0.000 to 0.249 was considered weak; from 0.250 to 0.499 moderate; from 0.500 to 0.749 strong; and between 0.750 and 1.000 was considered a very strong relationship.
Results
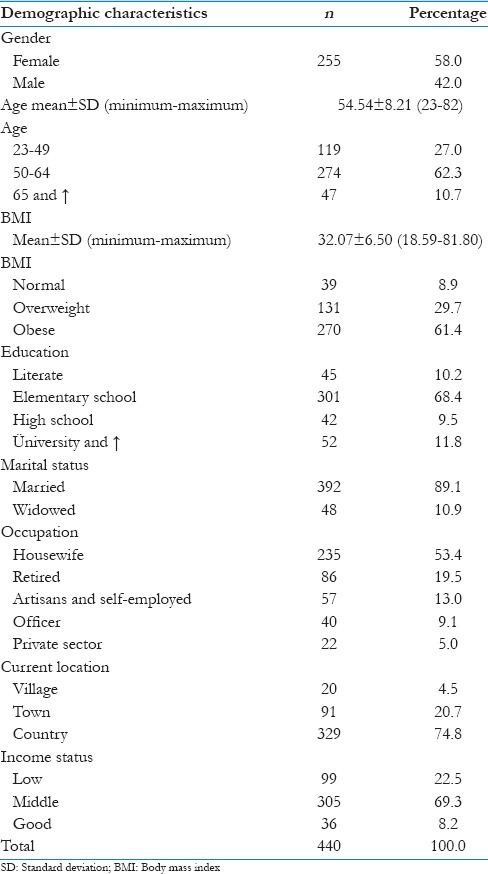
Demographic characteristics of the studied population are shown in Table 1.
Table 1.
Demographic characteristics of the studied population
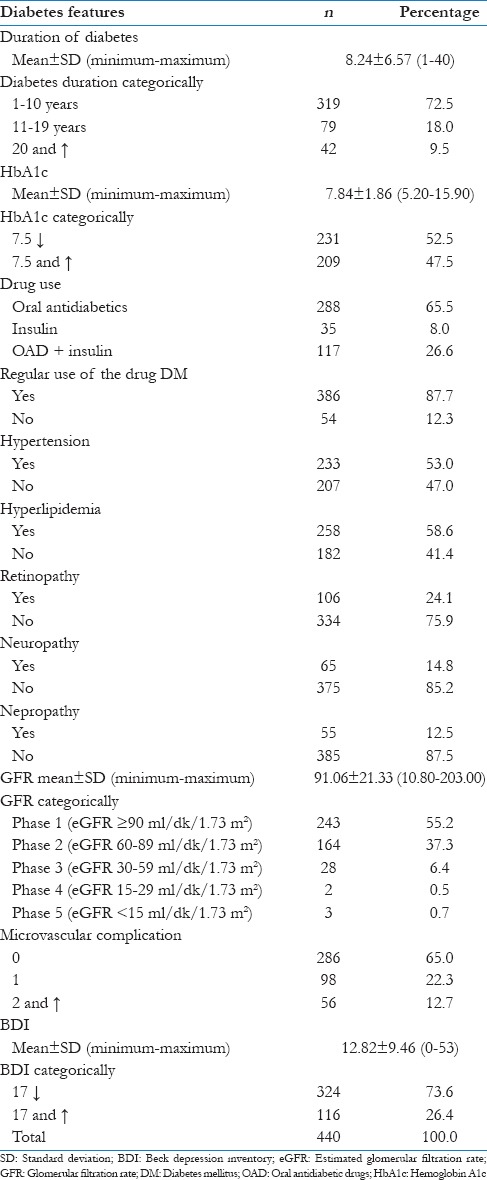
Diabetes and characteristics of patients in the study are shown in Table 2.
Table 2.
Features related to diabetes patients
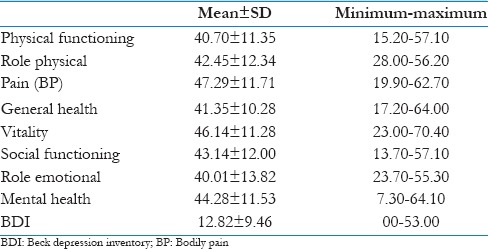
The average of the quality of life and the Beck depression ratings of the patients enrolled in the study are shown in Table 3.
Table 3.
The quality of life of patients and the average of Beck depression inventory
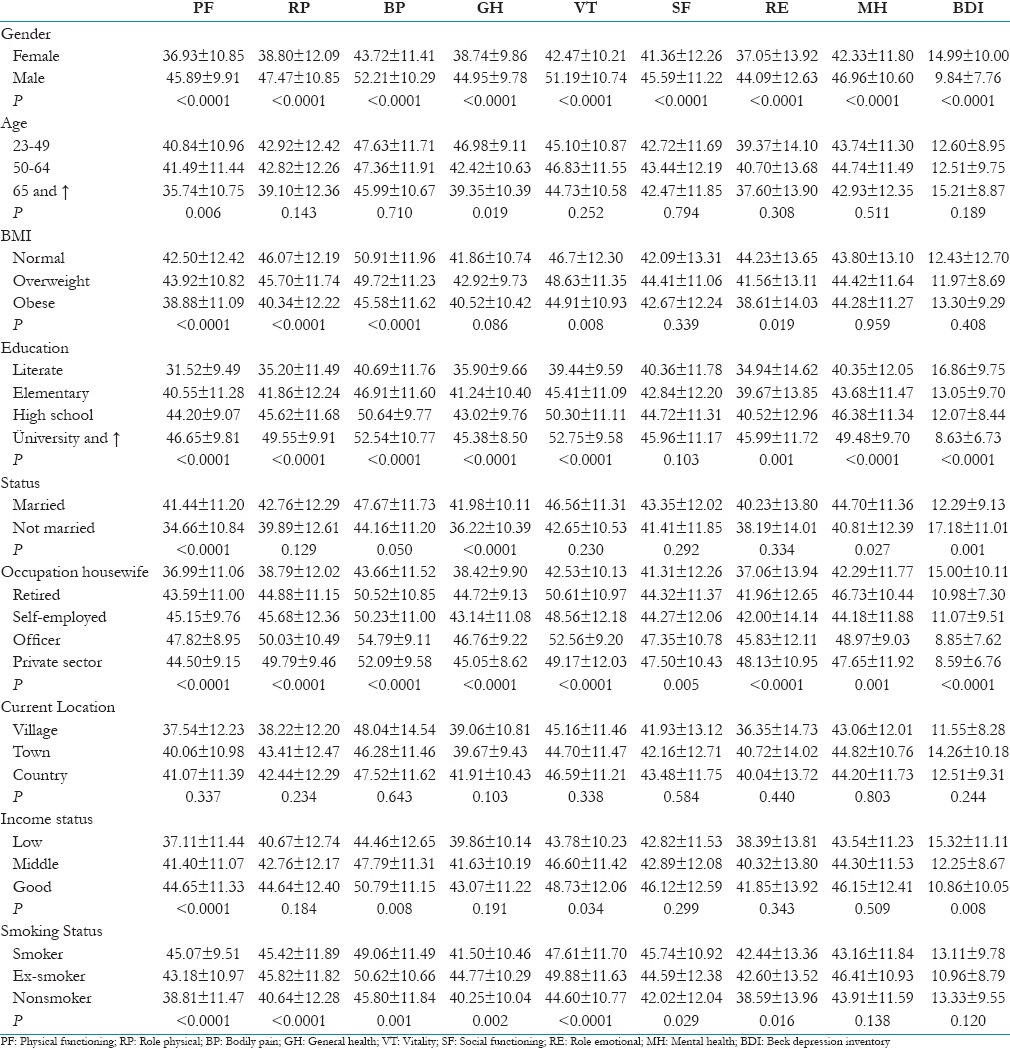
Comparison of the sociodemographic characteristics of the patients enrolled in the study with SF-36 and BDI parameters are shown in Table 4.
Table 4.
The comparison of the sociodemographic characteristics of diabetic patients with the Short Form 36 and Beck depression inventory parameters
Comparison of the diabetes characteristics of the patients enrolled in the study with the SF-36 and BDS parameters are shown in Table 5.
Table 5.
Comparison of the diabetes characteristics of the patients with Short Form 36 and Beck depression inventory parameters
The Hb values of the patients included in our study had a positive relation at moderate level (r = 0.337, P = 0.000) with the mean physical function score, positive at weak levels (r = 0.179, P = 0.000) with the mean role limitations score, positive at weak levels (r = 0.216, P = 0.000) with mean pain score, positive at weak level (r = 0.238, P = 0.000) with the mean general health status scores, positive at weak levels (r = 0.194, P = 0.000) with the average of social function score, positive at weak levels (r = 0.113, P = 0.018) with the mean mental health scores and had negative correlation at weak levels (r = −0.208, P = 0.000) with the average BDI score. The GFR values of the patients included in our study had positive relation at weak level (r = 0.163, P = 0.001) with the mean physical function score, positive at weak level (r = 0.153, P = 0.001) with the mean role limitations score, positive at weak levels (r = 0.103, P = 0.030) with mean pain score, and had negative correlation at weak levels (r = 0.161, P = 0.001) with the average BDI scores.
Discussion
The quality of life is important in many aspects for diabetes and diabetes care providers. Diabetes leads to a decrease in self-care worsening at glycemic control and increased risk of complications in diabetic individuals. Since these conditions can be powerful indicators of the ability of the diabetic subjects to cope with diabetes, and the attacks that may occur in the short- and long-term, the quality of life in diabetic people is very important. Quality of life is also an important datum reflecting the results of treatment applied to diabetic people. Quality of life is a concept that encompasses a wide range of field, and it is affected complicatedly with the way of relation to the physical health of the individual, psychological state, personal beliefs, social relations, and the surrounding events.[11]
When the patients in our study were compared according to their genders with the SF-36 sub-parameters, physical function, physical role limitations, pain, general health, energy, social function, emotional role limitations, and mental health mean scores of the female patients were statistically significantly lower than those of the male patients. In the literature, gender is reported to have an effect on the quality of life. The quality of life in diabetic women have been found to be lower than in men in the studies conducted.[12,13,14,15] It is also reported that the quality of life in women is worse than in men in the general population.[15] In a study conducted by Saraç et al., women received lower scores than men in all dimensions of SF-36 except physical function.[15] As stated in this and many other studies, the lower quality of life than men in both diabetic women and the women in general public can be explained by social roles and limitations belonging to the male and female gender, and it can also be attributed to physiological structures and hormonal differences of women.
It is known that the prevalence of diabetes increases with age in older people and many studies have investigated the relationship between diabetes and quality of life in older people.[14] When the patients were classified into three groups according to age in our study (young adult, adult, and elderly) and assessed, all sub-parameters except physical functioning and general health parameters of SF-36 did not differ significantly between the three groups. Although there are studies in the literature indicating that the quality of life is related to age, and the quality of life in young people is better, there are also studies indicating that there is not relationship between quality of life and age.[16,17] Papadopoulos et al. have found significant differences between the age groups only in the physical functioning parameters among the subscales of the SF-36 but no significant difference in the other parameters.[14] Although there was no statistically significant difference in the average of BDI scores between the groups, the elderly received the highest score. In our study, depression scores were found to increase with advanced age. Advanced age may be a risk factor for depression. It can be considered that economic difficulties, hard living conditions, low levels of education in our country, lack of knowledge of the disease, and concern for the future may affect diabetes and psychosocial health at later ages.
Of the sub-parameters of SF-36, physical functions, physical role limitations, pain, energy vitality, and emotional role distress scores in obese patients included in our study were statistically significantly lower compared to those with overweight and normal weight. In his study, Saraç et al. have reported that the quality of life is lower, especially in physical and social respect in the nondiabetic obese, and the degradation rate of the quality of life in both sexes is reported to be significantly higher in the obese than in the patients with normal weight.[15] Huang et al. have found in their study conducted in Taiwan investigating the relation of the quality of life with overweight using SF-36 in the individuals of the general population that overweight occurs in combination with deterioration in the physical quality of life, but the mental quality of life is not affected.[18] In our study, mental health and BDS scores were founded changed with body mass index too. Therefore, we believe that this situation may result from the normal acceptance of being overweight in the region where the patients live and causing no negativity.
When the relationship between the marital status and quality of life of the patients included in our study were compared, married patients received higher scores than patients who were not married in all sub-titles of the SF-36 quality of life scale and this situation in physical function, general health, and mental health parameters were found to be statistically significant. Those who are married have been reported to receive higher scores than the divorced and widows in all dimensions of SF-36 in studies on the quality of life. In the study of Papadopoulos et al., the quality of life scores of the married subjects were found higher than the single or widowed in all sizes.[14] In a study conducted by the Akinci et al. the quality of life of the married was found higher than the unmarried similar to our findings.[19] Jacobson et al. have reported that since being divorced or widowed negatively affects the quality of life in diabetic patients, their quality of life is lower than the married subjects.[20] It suggests that this result may be caused by the point of the view of society toward widowed individuals, lack of social support, living alone, and increase in responsibilities.
When the quality of life scores according to the occupation of the patients enrolled in our study are examined; the quality of life of homemakers has been found to be significantly lower in all sizes compared to other professional groups. The lowest scores homemakers receive are consistent with the fact that quality of life scores of women are lower than those of men. In our study, officer occupational groups have received the highest scores of SF-36 in all parameters. We believe that this may arise from regular working hours and income of civil servants, having a job guarantee and having higher level of education than the other groups in our study. In our study, we have determined that there is a significant correlation between the mean BDI scores and professional status. The highest average of BDI scores belongs to the homemakers. This case may be a result of women's being prone to depression. In addition, lack of any occupation, restricted life with home and low level of education may also have influenced this situation. When the quality of life scores of the patients in our study were evaluated according to the duration of diabetes, quality of life in all subscales except for the pain subscale of the SF-36 subscales in those with diabetes duration over 20 years was significantly lower than those with diabetes duration <20 years. In our study, it has been observed that the longer life spent with diabetes gets, the lower the scores fall in all sub-headings of the quality of life, that is, the quality of life decreases when the time spent with the disease extends. Some studies have shown that longer disease duration increases the risk of chronic complications and complications reduces the quality of life of patients by restricting their participation in everyday life.[21,22,23]
Hemoglobin A1c (HbA1c) is a safe indicator of glycemic control in the long-term, and it is considered as the best-glycemic control parameter. Target HbA1c values should be determined according to the risk of each patient's diabetes complications, the presence of other diseases accompanied by diabetes, the life expectancy, and the patient's preferences.[22] When quality of life scores were assessed according to the patients’ HbA1c values obtained in our study, the mean scores of physical function, pain, general health, social function of those with the target HbA1c values (<7.5) was significantly higher than those without target HbA1c values (≥7.5 and ↑), and their mean BDI scores were significantly lower. The presence of depression has been shown to affect adversely keeping the blood sugar under control and the therapy compliance. It has been reported that diabetic patients with depression develop insulin resistance, and compliance to the treatment is impaired.[21,22,23]
When the quality of life scores of patients in our study were considered according to the use of drug form; the mean scores of physical function, physical role limitations, pain, general health, social function were statistically significantly higher in cases using oral antidiabetic drugs (OAD) than in the cases using insulin + OAD. In the literature, there are studies indicating that the form of treatment affects the quality of life of diabetic people. The quality of life is worse, especially in the cases receiving insulin therapy.[9,24] In a study conducted by Gönen et al. it has been found that the quality of life of diabetic patients using insulin in all sizes of SF-36 is lower than those not using insulin; the difference in all dimensions except for physical functioning dimension is significant.[9] Family physicians can affect the quality of life of patients with OAD therapy before initiating insulin therapy by following-up closely and targeting the HbA1c values. With the development of complications in patients with DM, the quality of life of patients is deteriorated particularly with increased the physical constraints. When the presence of diabetes-related complications was compared with the quality of life in our study; the mean scores of the physical functions, physical role limitations, general health, and vitality-energy subscales of SF-36 in patients with two or more complications were statistically significantly lower than those of the patients with one or no complications. Similarly, in the literature major depressive disorder rate in patients with diabetic complications were found higher than in patients without diabetic complications.[5,23,25,26]
Approaching the diabetes patients as holistic requires the diagnosis and treatment of the accompanying diseases such as organic, mental, spiritual, psychophysiological, and psychosocial tables beside physical therapy. Priorities should be identified for improving the quality of life in the treatment and management of the disease. There are many medical and sociodemographic factors affecting the quality of life and depression symptomatology in people with diabetes, so health professionals, patients and as well as relatives of patients should pay the necessary attention this issue.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.6th ed. Brussels, Belgium: International Diabetes Federation; 2013. [Last accessed on 2015 Jul 25]. International Diabetes Federation. IDF Diabetes Atlas. Available from: https://www.idf.org/sites/default/files/EN_6E_Atlas_Full_0.pdf . [Google Scholar]
- 2.Saeed AA. Association of tobacco products use and diabetes mellitus-results of a national survey among adults in Saudi Arabia. Balkan Med J. 2012;29:247–51. doi: 10.5152/balkanmedj.2012.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 4.Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28:169–80. doi: 10.1007/s10654-013-9771-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eren I, Erdi Ö, Çivi I. The quality of life in the patients with type II diabetes mellitus and effects of complications on the quality of life. Clin Psychiatri. 2004;7:85–94. [Google Scholar]
- 6.Lau CY, Qureshi AK, Scott SG. Association between glycaemic control and quality of life in diabetes mellitus. J Postgrad Med. 2004;50:189–93. [PubMed] [Google Scholar]
- 7.Sümbüloğlu K, Sümbüloğlu V. Biostatistics. 7th ed. Ankara: Şahin Printing House; 1997. [Google Scholar]
- 8.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 9.Gönen MS, Güngör K, Çilli AS, Kamıs U, Akpınar Z, Kısakol G, et al. Comprehensive analysis of health related quality of life in patients with diabetes: A study from Konya Turkey. Turk J Endocrinol Metab. 2007;11:81–8. [Google Scholar]
- 10.Hisli N. Use of the beck depression ınventory with Turkish üniversity students: Reliability, validity, and factor analysis. Turk J Psychol. 1989;7:3–13. [Google Scholar]
- 11.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2015;31:55–60. [Google Scholar]
- 12.Jonsson PM, Nyström L, Sterky G, Wall S. Sociodemographic predictors of self-rated health in patients with diabetes of short duration. Scand J Public Health. 2001;29:263–70. [PubMed] [Google Scholar]
- 13.Edelman D, Olsen MK, Dudley TK, Harris AC, Oddone EZ. Impact of diabetes screening on quality of life. Diabetes Care. 2002;25:1022–6. doi: 10.2337/diacare.25.6.1022. [DOI] [PubMed] [Google Scholar]
- 14.Papadopoulos AA, Kontodimopoulos N, Frydas A, Ikonomakis E, Niakas D. Predictors of health-related quality of life in type II diabetic patients in Greece. BMC Public Health. 2007;7:186. doi: 10.1186/1471-2458-7-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saraç ZF, Tütüncüoğlu P, Parıldar S, Saygılı F, Yılmaz C, Tüzün M. Quality of life in Turkish diabetic patients. Turk J Endocrinol Metab. 2007;11:48–53. [Google Scholar]
- 16.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–18. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 17.Glasgow RE, Ruggiero L, Eakin EG, Saygılı F, Yılmaz C, Tüzün M. Quality of life in non-insulin-dependent diabetes and a comparison with insulin-dependent diabetes. Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care. 1997;20:562–7. doi: 10.2337/diacare.20.4.562. [DOI] [PubMed] [Google Scholar]
- 18.Huang IC, Frangakis C, Wu AW. The relationship of excess body weight and health-related quality of life: Evidence from a population study in Taiwan. Int J Obes (Lond) 2006;30:1250–9. doi: 10.1038/sj.ijo.0803250. [DOI] [PubMed] [Google Scholar]
- 19.Akinci F, Yildirim A, Gözü H, Sargin H, Orbay E, Sargin M. Assessment of health-related quality of life (HRQoL) of patients with type 2 diabetes in Turkey. Diabetes Res Clin Pract. 2008;79:117–23. doi: 10.1016/j.diabres.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Jacobson AM, de Groot M, Samson JA. The evaluation of two measures of quality of life in patients with type I and type II diabetes. Diabetes Care. 1994;17:267–74. doi: 10.2337/diacare.17.4.267. [DOI] [PubMed] [Google Scholar]
- 21.Özder A. The well-being and depression status of diabetic patients in primary health care. Acta Med Mediterr. 2015;31:23. [Google Scholar]
- 22.Qaseem A, Vijan S, Snow V, Cross JT, Weiss KB, Owens DK. Clinical Efficacy Assessment Subcommittee of the American College of Physicians. Glycemic control and type 2 diabetes mellitus: The optimal hemoglobin A1c targets. A guidance statement from the American College of Physicians. Ann Intern Med. 2007;147:417–22. doi: 10.7326/0003-4819-147-6-200709180-00012. [DOI] [PubMed] [Google Scholar]
- 23.Zhang W, Xu H, Zhao S, Yin S, Wang X, Guo J, et al. Prevalence and influencing factors of co-morbid depression in patients with type 2 diabetes mellitus: A General Hospital based study. Diabetol Metab Syndr. 2015;7:60. doi: 10.1186/s13098-015-0053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pala T, Eser E, Özmen B, Aydemir Ö, Boyvoda S. The determinants of quality of life including treatment satisfaction in patients with type two diabetes mellitus: Are different generic Qol instruments sensitive to the same determinants? Turk J Endocrinol Metab. 2004;3:91–9. [Google Scholar]
- 25.Zenteno JFT, Cardiel MH. Risk factors associated with depression in patients with Type 2 diabetes mellitus. Arch Med Res. 2002;33:53–60. doi: 10.1016/s0188-4409(01)00349-6. [DOI] [PubMed] [Google Scholar]
- 26.Dzida G, Karnieli E, Svendsen AL, Solje KS, Hermanns N on behalf of the SOLVE Study Group. Depressive symptoms prior to and following insulin initiation in patients with type 2 diabetes mellitus: Prevalence, risk factors and effect on physician resource utilisation. Prim Care Diabetes. 2015;30 doi: 10.1016/j.pcd.2015.01.002. pii: S1751-9918(15)00003-0. [DOI] [PubMed] [Google Scholar]


