Abstract
Background:
Effective breastfeeding is a function of the proper positioning of mother and baby and attachment of child to the mother's breast. Positioning of the baby's body is important for good attachment and successful breastfeeding. The study was planned to assess mother–infant pair latch on position and its impact on health status of the child.
Materials and Methods:
It was community-based cross-sectional study conducted among 1267 children between age group of 0–24 months in the urban and rural field practice areas of the Department of Community Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Ambala, Haryana. A self-designed semi-structured questionnaire along with the WHO criteria for assessment of correct latch on position was used in this study.
Results:
Out of 1267 mothers, only 29.9% mothers initiated breastfeeding within 1 h of delivery. Mothers who had high parity had better positioning scores as compared to mothers with low parity. About 83.7% mothers who had parity >2 had excellent scores as compared to those mothers having one child or two children. About 56.8% and 62.7% children who suffered from diarrhea and acute respiratory infection (ARI), respectively, had mothers with poor positioning and this difference was statistically significant (P < 0.001).
Conclusion:
It was concluded that mothers who had higher parity had better positioning and attachment scores and also mothers with excellent positioning scores, their children suffered less from diarrhea and ARI. Each mother should be observed for mother's and infant's positioning and attachment at the onset of breastfeeding and if needed given counseling on correct positioning and attachment.
Keywords: Breastfeeding, mothers, positioning
Introduction
Breast milk is the best gift that a mother can give to her newborn baby. It is a unique way with which a mother fulfils her role of a nurturer bestowed on her by God. It is a natural opportunity to communicate love at the very beginning of a child's life, providing hours of closeness, nurturing every day, laying the foundation for a caring, and trusting relationship between mother and the child.[1]
Breastfeeding is one of the oldest practices recommended in the ancient Hindu scriptures, Holy Quran, and Biblical records.[2] Breastfeeding is one of the most important determinants of child survival, birth spacing, and prevention of childhood infections.[3] Breast milk is the natural first food for babies. It is the safest, least allergic, and best infant feeding method. It embraces nutritional, immunological, behavioral and economic benefits as well as provides desirable mother-infant bonding.[4]
Human milk is the best food for the growing infant as it enhances growth and cognitive development also. It fulfills energy and nutritional needs of the baby in the first few months of life.[5] Studies conducted in developing countries have revealed that nonbreast-fed infants are 6–10 times more likely to die in the first few months of life as compared to breast-fed infants. Acute infections such as hemophilus influenza, meningitis, and urinary tract infections are less common and less severe in breast-fed infants.[2]
Early initiation of breastfeeding could reduce neonatal mortality by 22%, which would contribute to the achievement of Millennium Development Goals. Globally, over one million newborn infants could be saved each year by initiating breastfeeding within 1 h of life. In developing countries alone, early initiation of breastfeeding could save as many as 1.45 million lives each year by reducing deaths mainly due to diarrheal disorders and respiratory tract infections.[6]
Quality of infant feeding is decisive determinant of child survival. The link between poor infant feeding practices and malnutrition has been well established.[7] India is home to maximum number of under-five deaths and underweight children in the world. Results from National Family Health Survey-III (NFHS-III) show that at 6 months of age, 29.5% children are already underweight.[8] Prevalence of malnutrition under 3 years of age in India is 45%. Much of this is due to inappropriate feeding practices and also due to serious erosion of breastfeeding[9] apart from feeding practices position of the mother and correct latch on of the baby determine breastfeeding practices.
Effective breastfeeding is a function of the proper positioning of mother and baby and attachment of child to the mother's breast. Positioning of the baby's body is important for good attachment and successful breastfeeding. Most difficulties can be avoided altogether if good attachment and positioning are achieved at the first and early feeds. An effective sucking technique is considered important to establish breastfeeding, to ensure milk transfer, and to prevent breastfeeding problems. The baby's positioning and attachment to the breast during breastfeeding are fundamental toward the occurrence of different sorts of nipple trauma.[2] Therefore, the study was undertaken to assess mother–infant pair latch on position, and its impact on health status of the child.
Aim and objective
To assess mother–infant pair latch on position and its impact on health status of the child.
Materials and Methods
Study area
The study was a community-based cross-sectional study conducted among 1267 children aged 0–24 months and their mothers in the urban and rural field practice areas of the Department of Community Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Ambala, Haryana, between January 1, 2013 and December 31, 2013. Mothers with infants and children up to 2 years of age were included in the study and mothers who could not breast-feed their children due to serious illness were excluded from the study.
Sample size was calculated assuming prevalence of 24.5%. As per the NFHS-III percentage of children who started breastfeeding within 1 h of birth (for all India) was 24.5%.[10] The sample size thus calculated was 1184. Assuming nonresponse rate to be 10%, the sample size was rounded off to 1300. One thousand three hundred mothers were approached and 33 could not be convinced to participate in the study. Therefore, responses from only 1267 mothers could be obtained.
Simple random sampling technique was used for sample collection. This was done by random number table method. The study was conducted by employing house-to-house survey technique. The data were collected by interviewing the mothers or the primary caregiver of the child after taking an informed and written consent. The objectives of the study were explained to all the mothers prior to the interview, and their consent was taken to examine their respective child.
The questions put forth were in the regional language. The data were collected using a self-designed and semi-structured questionnaire.
Study tools
Self-designed and semi-structured questionnaire for collecting the relevant information regarding the sociodemographic factors, knowledge, and level of awareness of mothers regarding infant feeding, trends of infant feeding, and assessment of impact of feeding practices adopted by mothers on child's health and nutritional status
Anthropometric assessment: Length (in centimeters) and weight in kilograms.
The following arbitrary scoring and grading system was developed and adopted to grade positioning (mother and infant) infant's mouth attachment and effective suckling during breastfeeding based on the WHO criteria. Each criterion was assigned 1 point.
The WHO recommended criteria for good positioning, attachment, and effective suckling during breastfeeding noted were following.
Mother relaxed and comfortable
Mother sit straight and well-supported back
Trunk facing forward and lap flat
Baby neck straight or bent slightly back and body straight
Baby's body turned toward mother
Baby's body close to mother's body and facing breast
Baby's whole body supported.
Criteria for grading correct position
One criteria from mother's position, one from infant's position or both from mother's position. Grade-Poor score 0–2
At least one criterion from mother's position and two or three criteria from infant's position. Grade-average score 3–4
At least two criteria from mother's position and three or four criteria from infant's position. Grade-good score 5–7.
Correctness of attachment
Chin touching breast
Mouth wide and open
Lower lip turned outward
More areola seen toward the baby's mouth.
Criteria for grading correctness of attachment
Any one of the four criteria. Grade-Poor score 1
Any two of the four criteria. Grade-Average score 2
Any three or all the four criteria. Grade-Good score 3–4.
Correctness of effective suckling
Slow sucks
Deep sucks
Sometimes pausing.
Criteria for grading effective suckling
Any one of the three criteria. Grade-Poor score 1
Any two or all the three criteria. Grade-Good score 2.
Statistical analysis
The data collected during the survey were entered in Microsoft excel and analyzed via SPSS (Statistical Package for Social Sciences) SPSS Version 20 (IBM, Chicago, USA). The child feeding practice, as well as socioeconomic and demographic factors and impact on nutritional status of children, was expressed as proportions in the form of percentages. Chi-square test of significance was applied to establish their association with breastfeeding and P < 0.05 was considered to be statistically significant.
Results
The study was conducted in three rural field practice areas and one urban area of Maharishi Markandeshwar Institute of Medical Sciences and Research. One thousand three hundred mothers were approached and 33 could not be convinced to participate in the study. Therefore, responses from only 1267 mothers could be obtained. The study conducted among 1267 mothers and their 0–24–month-old children revealed following findings.
Table 1 represents the distribution of mothers according to the age group and the area of residence. Among 1267 mothers with infants and children up to 2 years of age, 709 were from rural area and 558 from urban area. A large proportion of mothers (44.3%) belonged to the age group of 20–24 years, followed by 40.6% in the age group of 25–29 years while 3% belonged to the age group of <20 years and only 0.5% mothers belonged to the age group of 35–39 years. In rural area, majority of the mothers (60.1%) belonged to age group of 20–24 years whereas in urban area majority of the mothers, i.e., 57% belonged to the age group of 25–29 years.
Table 1.
Distribution of study participants according to age and area of residence
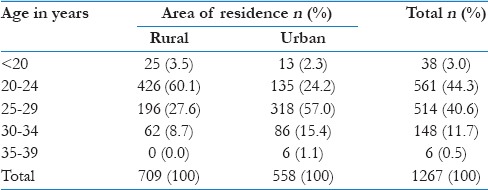
Table 2 represents the educational status of the mothers according to their area of residence. Nearly 22.2% of all mothers were illiterate and majority, i.e. 26.3% mothers were educated up to primary level followed by graduation (i.e., 18.1%). In rural area, majority of the mothers, i.e., 34.7% were illiterate, 30.9% mothers had received education up to primary level, 15.4% received education up to high school, and 11.5% were educated up to secondary school level. In urban area, a large proportion of the respondents (34.2%) were graduates and 20.4% were educated up to primary school level. About 18.6% and 14.2% attended high school and secondary school, respectively. Only 2.1% mothers were educated up to postgraduate level in rural area as compared to 6.3% mothers in urban area. The study revealed a statistically significant difference (P < 0.001) between education status of the mothers residing in rural and urban area.
Table 2.
Distribution of mothers according to their educational status and area of residence
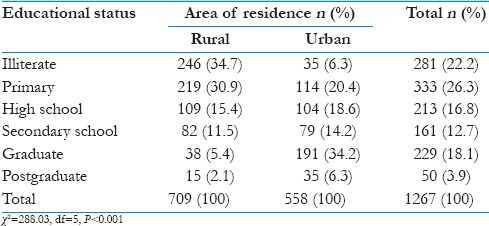
Table 3 depicts the time of initiation of breastfeeding among mothers according to area of residence. Out of 1267 mothers, only 29.9% mothers initiated breastfeeding within 1 h of delivery. More number of mothers (33.6%) in rural area initiated breastfeeding within 1 h of delivery, whereas only (25.3%) mothers in urban area could initiate breastfeeding within 1 h. Maximum number of the mothers (40.9%) in urban area initiated breastfeeding within first 24 h and same trend was seen in rural area (34.1%). The difference in the time of initiation of breastfeeding between urban and rural mothers was statistically significant (P < 0.001).
Table 3.
Distribution of mothers according to time of initiation of breastfeeding
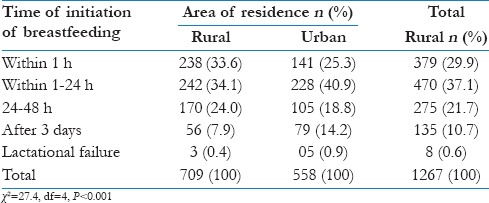
Table 4 shows the comparison of criteria for good positioning, attachment, and effective suckling between mothers of urban and rural area. It is clear from this table that positioning was significantly (P < 0.001) better among urban mothers as 57.9% had excellent scoring whereas this percentage was low 37.9% in rural mothers. Similarly, attachment was also significantly (P < 0.001) better among urban mothers. Fifty-nine percent of urban mothers exhibited excellent attachment compared to only 40.1% rural mothers who had good scores. Criteria for effective suckling were also better among mothers living in urban area, i.e., 59% compared to 37.7% mothers of rural area showing a significant difference (P < 0.001).
Table 4.
Distribution of mothers according to criteria of good positioning, attachment, effective suckling
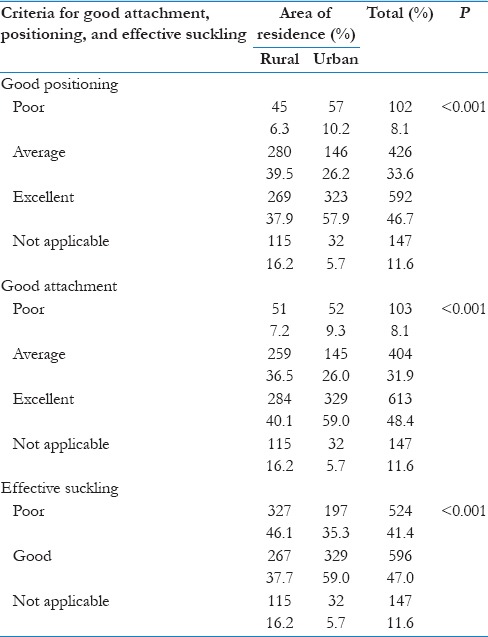
Table 5 shows the relationship of parity with positioning of the mother. Mothers who had high parity had better positioning scores as compared to mothers with low parity. About 83.7% mothers who had parity >2 had excellent scores as compared to those mothers having one child or two children. Mothers with one child mostly had average scores. There was a significant association between parity and positioning of the mother (P < 0.001).
Table 5.
Relationship of parity with positioning of the mother
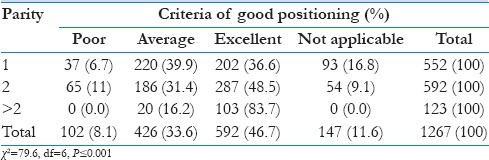
Table 6 depicts that 56.8% children whose mothers had poor positioning suffered from diarrhea compared to 34.1% children whose mothers had excellent positioning scores, and this difference is statistically significant (P = 0.001).
Table 6.
Relationship of positioning of the baby with diarrhea
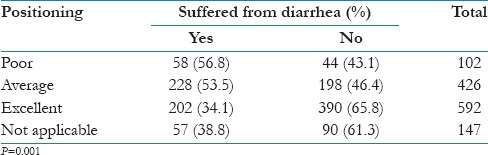
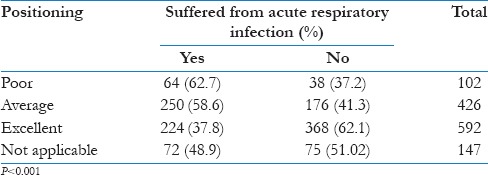
Table 7 represents that majority of the children (62.7%) with mothers having poor positioning suffered more from acute respiratory infection (ARI) as compared to 37.8% children whose mothers had excellent positioning and this difference is statistically significant (P< 0.001)
Table 7.
Relationship of positioning of the baby with acute respiratory infection
Discussion
Breastfeeding is critical for sustaining newborn and infant health and well-being. It is estimated that 10.9 million children worldwide under the age of 5 years die every year, of which 2.4 million deaths occur in India alone. In keeping with the Millennium Development Goals, countries in the developing world have committed to reduce the under-five mortality rate by two-thirds between 1990 and 2015. Appropriate feeding practices remain only feasible intervention in addressing this goal.
Trends of breastfeeding
Although breastfeeding practices are universal in India, significant erosion of breastfeeding practices has occurred due to modernization. The current study revealed that a total of 29.9% mothers had initiated breastfeeding within 1 h of delivery. In rural area, 33.6% mothers initiated breastfeeding within one hour, whereas in urban area, only 25.3% could start breastfeeding within 1 h of birth. Figures observed in total and in urban area of Ambala, Haryana, are consistent with figures reported by NFHS-III, which found that initiation of breastfeeding within an hour of birth was 24.5%.[10] DLHS-3 collected data of 534 districts and reported similar figure, i.e., 40%.[11] which is in agreement with findings of rural area of Ambala, Haryana.
Positioning and attachment in relation to parity and its impact on child's health
The present study revealed that 46.7% infants were held in excellent position and excellent attachment was seen in 48.4% mothers, 83.7% mothers who had parity more than 2 had excellent positioning and attachment. Gandhavi et al. and Chaudhary et al. reported that 40% mother–infant pair had excellent attachment.[12,13] In contrast to this, Tamiru et al. in Ethiopia found that 64.08% mothers had poor positioning and 51.15% had poor attachment.[14] This can be attributed to the fact that majority of the mothers in this study, i.e. 56.3% were illiterate.
Synonymous to the findings of the current study, Goyal et al. concluded that 74.0% of multiparous mothers had good positioning and attachment.[2]
In the past, several parameters related to breastfeeding have been correlated with increase in the incidence of respiratory infections which include proper positioning of the baby at the breast, length/duration of each feed, spacing between feeds and practice of mixed feeding. The current study focuses to establish correlation if any between infant latching, positioning, attachment overall effectiveness of suckling on the incidence of diarrhea and respiratory infections using the WHO criteria.
Although each child is unique in his/her own way, the technique of breastfeeding is universally the same and if modified by maternal or health-care provider services may lead to undesirable results. We had definite parameters to assess three functions, viz., attachment, parity, and suckling efficacy which could be objectively scored. Hence, we were able to come to striking conclusions, which have so far not been well documented.
One of the major findings was much higher incidence of diarrhea among children with poor attachment or positioning in turn leading to ineffective suckling and this was found significantly higher compared to those children who had good attachment, positioning, and suckling. Possible reasons were explored, and it was found that abnormal positioning and latchment lead to dispersion of milk in various directions inside the oral cavity and the lying down position could have led to spread of milk in eustachian tube, thereby causing increased incidence of ARI. Since milk is a good culture for growth of bacteria, the same infected milk along with baby's saliva could easily move down the gullet in upper intestines thereby leading into diarrheal disease. Although we could not vouch for this hypothesis owing to paucity of similar studies on the impact of latch on mother–child pair on child's health, the mechanism seems very plausible and explains the above phenomenon.
Effective breast feeding is not only possible by mere theoretical knowledge, but a lot depends on prior experience and demonstration of feeding methodology by elderly and health care providers. This study confirmed this belief that correct positioning and attachment was significantly better amongst the multiparas compared to primiparas. Also effective ''latch on'’ had a direct effect on morbidities like diarrhea and ARI, in our study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.UNICEF. Breastfeeding: Foundation for a Healthy Future. 2000. [Last accessed on 2014 Sep 19]. Available from: http://www.unicef.org/publications/files/pub_brochure_en.pdf .
- 2.Goyal RC, Banginwar AS, Ziyo F, Toweir AA. Breastfeeding practices: Positioning, attachment (latch-on) and effective suckling – A hospital-based study in Libya. J Family Community Med. 2011;18:74–9. doi: 10.4103/2230-8229.83372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahmood SE, Srivastava A, Shrotriya VP, Mishra P. Infant feeding practices in the rural population of north India. J Family Community Med. 2012;19:130–5. doi: 10.4103/2230-8229.98305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaili V, Sharma P, Kandpal SD, Semwal J, Srivastava A, Nautiyal V. A community based study on breastfeeding practices in a rural area of Uttarakhand. Natl J Community Med. 2012;3:283–6. [Google Scholar]
- 5.WHO. Exclusive Breastfeeding. 2014. [Last accessed on 2014 Sep 19]. Available from: http://www.who.int/nutrition/topics/exclusive_breastfeeding/en/
- 6.Nigam R, Sinha U. Assessment of knowledge and attitude of antenatal mothers towards breastfeeding. Natl J Community Med. 2012;3:381–4. [Google Scholar]
- 7.Ministry of Women and Child Development. National Guidelines on Infant and Young Child Feeding. 2006. [Last accessed on 2014 Sep 19]. Available from: http://www.wcd.nic.in/publication/infantandyoungchildfeed.pdf .
- 8.Dadhich JP, Agarwal RK. Mainstreaming early and exclusive breastfeeding for improving child survival. Indian Pediatr. 2009;46:11–7. [PubMed] [Google Scholar]
- 9.Bhardwaj SL, Rathore MS, Paliwal A. A study of breast feeding and neonatal care practices in some ethnic communities in periurban slums at Jaipur Rajasthan. Int J Contemp Appl Stud Man. 2012;14:459–65. [Google Scholar]
- 10.Ministry of Health and Family Welfare Government of India. National Family Health Survey (NFHS-3), 2005-2006. [Last accessed on 2014 Sep 19]. Available from: http://www.pdf.usaid.gov/pdf_docs/PNADK385.pdf .
- 11.Breastfeeding Promotion Network of India on World Breastfeeding Week. 2012. [Last accessed on 2014 Sep 19]. Available from: http://www.bpni.org/WBW/2012/Trends-3indicators-of-Breastfeeding.pdf .
- 12.Gandhavi RN, Vidhani M, Patel F, Patel A, Mehta S, Chavan LB. Are today's mother aware enough about breast feeding.: A knowledge, attitude and practice study on urban mothers? Natl J Med Res. 2013;3:396–8. [Google Scholar]
- 13.Chaudhary RN, Shah T, Raja S. Knowledge and practice of mothers regarding breast feeding: A hospital based study. Health Renaissance. 2011;9:194–200. [Google Scholar]
- 14.Tamiru D, Bogale B, Merdikios B. Breast-feeding patterns and factors with exposure to suboptimal breast-feeding practices in rural communities of Arba Minch Zuria, Ethiopia. Glob Health Perspect. 2013;1:105–12. [Google Scholar]


