Abstract
Background and Objectives:
To study the role of ophthalmoscopy in pregnancy induced hypertension (PIH) in diagnosis, prognosis, differential diagnosis, line of treatment and effect of treatment.
Materials and Methods:
An observational study in which all the patients for the study are selected from antenatal clinic, antenatal wards and preeclampsia and eclampsia room in Department of Obstetrics and Gynecology, General Ophthalmic Out Patient Department (OPD) in case of ambulatory patients, during the period of Nov. 2003 to June 2006 randomly. In every case detail obstetric history, general examination and relevant pathological investigations were carried out. In every case, pupil was dilated with homatropine (2%) eye drops and detailed ophthalmic examination was carried out.
Results:
In our study out of 300 cases of PIH, there are 182 cases of mild preeclampsia and 76 cases of severe preeclampsia and 42 cases of eclampsia. Among these, 37 cases (20.33%) of mild preeclampsia and 75 cases (98.68%) of severe preeclampsia and 41 cases (97.62%) of eclampsia show positive fundus changes. The incidence of pre-term babies, intra uterine death, still birth and low birth weight infants is high in mothers having positive fundus changes, i.e. for pre-term infant (72.46%), still birth (62%) and low birth weight (45.56%) in our series The perinatal mortality is higher in patients having Grade II (33.85%), Grade III (54.29%), Grade IV (100%) hypertensive retinopathy.
Conclusion:
Retinal examination reveals important objective information in PIH, furthers their accurate diagnosis and refines their management.
Keywords: Fundus findings, pregnancy induced hypertension, hypertensive disorders of pregnancy, ophthalmoscopy, perinatal mortality
Introduction
Toxemia of pregnancy is a recognized entity for over 2000 years with its known complications and fatality.[1,2,3] Nowadays, a most accepted terminology for the following defined syndrome is “hypertensive disorders in pregnancy” given by American College of Obstetrics and Gynecology.[2,3] It is an important cause of maternal and fetal morbidity and mortality.[4,5,6] Pregnancy induced hypertension (PIH) was classified as gestational hypertension, preeclampsia, severe preeclampsia and eclampsia. PIH is a hypertensive disorder in pregnancy that occurs after 20 weeks of pregnancy in the absence of other causes of elevated blood pressure (BP) (BP >140/90 mmHg measured two times with at least of 4 hour interval) in combination with generalized edema and/or proteinuria (>300 mg per 24 hrs). When there is significant proteinuria it is termed as preeclampsia; seizure or coma as a consequence of PIH is termed as eclampsia.[2,3]
Preeclampsia was classified into mild and severe preeclampsia.
Mild eclampsia—BP >140/90 mmHg, proteinuria+, and/or mild edema of legs, Severe preeclampsia—BP >160/110 mmHg, proteinuria++ or ++++, headache, cerebral or visual disturbances, epigastric pain, impaired liver function tests and increase in serum creatinine.[2,3,7,4,5,6,7,8,9,10,11,12,13,26] Proteinuria was tested using dipstick method as +=0.3 gm/L, ++=1 gm/L, and +++=3 gm/L.[7,8,9,10] The pathological changes of this disease appear to be related to vascular endothelial dysfunction and its consequences (generalized vasospasm and capillary leak). Ocular involvement is common in PIH.[11,12,13] Common symptoms are blurring of vision, photpsia, scotomas and diplopia. Visual symptoms may be the precursor of seizures.[11,12,13,14,15,16,17] Progression of retinal changes correlates with progression of PIH and also with the fetal mortality due to similar vascular ischemic changes in placenta.[4,5,6] Vasospastic manifestations are reversible and the retinal vessels rapidly return to normal after delivery. Ophthalmoscope should be rated next to the sphygmomanometer as an instrument of diagnostic importance in cases of PIH. Ophthalmoscopy does not only helps in diagnosing the disease but repeated observations assist in assessing the severity, progress of disease, response to treatment if any and ultimate outcome or prognosis.[6,8,9,10,11,12,13,14,15,16,17,26].
Objective
To study the role of ophthalmoscopy in PIH in diagnosis, prognosis, differential diagnosis, line of treatment and effect of treatment.
Materials and Methods
An observational study in which the patients for the study are selected from antenatal clinic, antenatal ward and “preeclampsia and eclampsia room” in Department of Obstetrics and Gynecology and general ophthalmic OPD in case of ambulatory patients during the period of November 2003 to June 2006 randomly.[9,10,18]
In every case, detail obstetric history including a detail antenatal history was taken. General examination and relevant pathological investigations like routine blood count, HIV, HBsAg, renal function tests, TORCH complex etc., were carried out. In every case, pupil was dilated with homatropine (2%) eye drops. Then detailed ophthalmic examination was carried out with special emphasis on direct ophthalmoscopy apart from visual acuity of both eyes and anterior segment examination.
Fundus findings were noted in detail, changes in the color of the disc, disc margin, physiological cup, changes in retinal blood vessels especially caliber of vessels, arterio-venous (AV) ratio, changes in vessel wall, blood column, appearance of vascular light reflex, changes at AV crossings, changes in macular area and changes in background, overall appearance, presence of hemorrhages, exudates or any pathology were recorded.[8,11,12,13,14,15,16,17,18] Fundus changes were graded as per modified Keith, Wagner and Barker classification.[19] Assessment of prognosis as regards to vision and life (mortality) was made.
Statistical analysis
Data was entered in MS Excel spreadsheet and presentation of data was done in the form of percentages.
Results
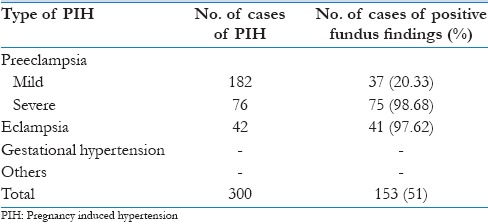
In our study, out of 300 cases of PIH, there are 182 cases of mild preeclampsia and 76 cases of severe preeclampsia and 42 cases of eclampsia. Among these, 37 cases (20.33%) of mild preeclampsia and 75 cases (98.68%) of severe preeclampsia and 41 cases (97.62%) of eclampsia showed positive fundus changes [Table 1].
Table 1.
The relation of positive fundus changes with number of cases of pregnancy induced hypertension
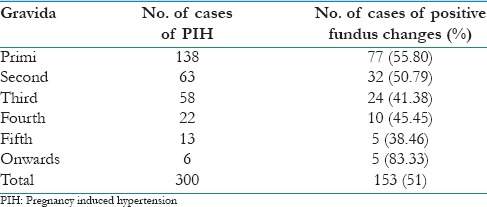
As shown in Table 2, the incidence of positive fundus findings is most common in primi gravida (55.80%) and second gravida (50.79%), than multi gravida, i.e. third gravida (41.38%), fourth gravida (45.45%), and fifth gravida (38.46%).[8,14,15,16,17] The second high peak was seen in patients having multiple pregnancies, i.e. sixth gravida onward (83.33%).
Table 2.
The relation of number of cases of PIH and positive fundus findings with number of gravida
As shown in Table 3, the young patients are very prone to PIH and positive fundus findings are frequently present in 18 to 25 years of age.[8,14,15,16,17] Out of 66 patients under 20 years of age, 36 had positive findings (54.55%) and out of 119 patients in age group 21-25 years, 61 had positive fundus findings (51.26%).
Table 3.
Relationship between total number of cases of PIH and fundus changes according to age
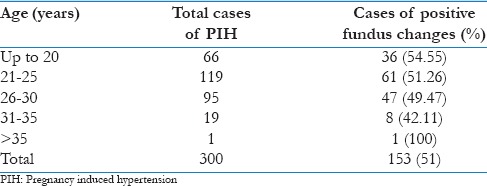
Table 4 shows that hypertension was found in maximum patients in 6-7 months of amenorrhea, i.e. 71.43% and 7-8 months of amenorrhea, i.e. 75%. All cases of post partum eclampsia showed positive fundus changes.[8,14,15,16,17]
Table 4.
Relationship between number of cases of PIH and fundus changes according to duration of pregnancy
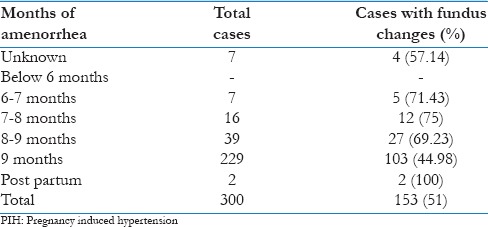
Table 5 depicts the relation of number of cases of PIH and the fundus findings with systolic blood pressure. It shows maximum percentages of positive cases were seen in 181-200 Hg of systolic blood pressure, i.e. 93.10% and 100%.[8,14,15,16,17]
Table 5.
The relation of number of cases of PIH and fundus findings with systolic blood pressure
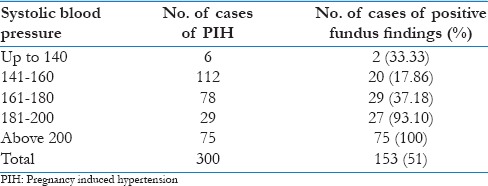
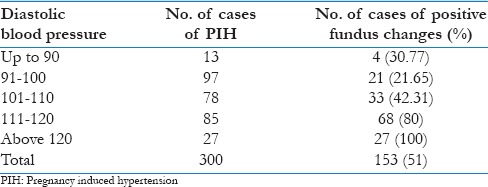
As shown in Tables 5 and 6, the incidence of fundus changes do not increase with increase of systolic blood pressure; while they increase with rise of diastolic blood pressure.[14,15,16,17,20] There is highest incidence of positive fundus findings when diastolic blood pressure is greater than 110 mm of Hg i.e. 68 out of 85 patients (80%) [Table 6].
Table 6.
The relation of number of cases of PIH and fundus findings with diastolic blood presure
As per Table 7, there is incidence of normal fundus in 147 (49%) cases, arterial attenuation in 49 cases (16.33%); arterio venous crossing changes along with retinal edema in 65 cases (21.67%), and hemorrhages and exudates in 35 cases (11.67%) and there was one case of papilledema (0.33%) and 3 cases of retinal detachment (1%).[8,14,15,16,17,20,21,22,23,24,25,26]
Table 7.
The relation of number of cases of PIH according to fundus changes (according to modified Keith, Wagner and Barker classification)
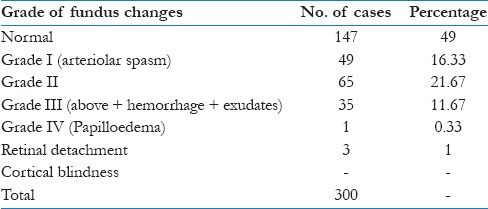
In our study, most of cases 49 (16.33%) were of arterial attenuation; arterial attenuation was transient and disappeared after 7 to 10 days of control of PIH or delivery, either spontaneous or induced.[8,9,10,17] In half of the cases, arterial attenuation was limited to nasal arterioles. The spasm of retinal vessels was irregular, intermittent and spasmodic.[6,11,12,13,14,15,16,17,20]
In the present study, arterio venous crossing changes were found in 65 (21.67%). Arterio venous crossing changes were more closely related to generalized edema and proteinuria.[7,8] These changes regressed post partum [Table 7].
In the present study, 31 cases had superficial flame-shaped hemorrhages, 1 case of dot and blot hemorrhage and 1 case of pre-retinal hemorrhage. Nineteen cases had cotton wool spots and one case had hard exudates [Table 8].
Table 8.
The relation of individual fundus findings with no. of cases of PIH
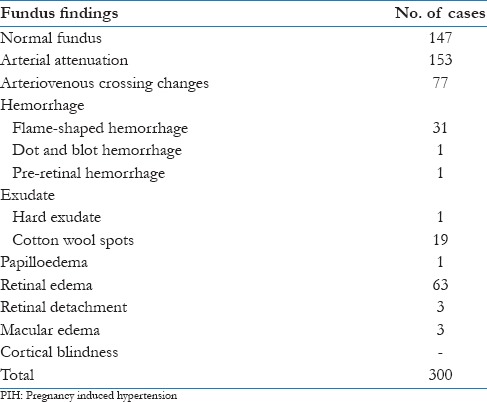
Superficial hemorrhages disappeared after 10 to 40 days and exudates disappeared after 40 to 60 days of delivery.
Exudative retinal detachment regressed within 2 days post partum. Retinal as well as macular edema took one and half months to regress. Pre-retinal hemorrhage took 6 months to regress.
In the present series, retinal edema was present in 63 cases. Edema was more marked in central fundus. Edema subsided one and half month post partum. Retinal edema is suggestive of severity of PIH.
In the present series, three cases of retinal detachment were found. Termination of pregnancy was advised. There was regression of retinal detachment post partum with restoration of vision.[9,10,22,23,24,25,26]
In our series, there was one case of papilloedema along with flame-shaped hemorrhages and cotton wool spots.[21] Antenatal care was not taken. Termination of pregnancy was advised.
There was pre-term vaginal delivery with a still born child.
Papilloedema regressed after one and half month. Positive fundus changes in severe preeclampsia cannot be ignored as they can be indicator of impending eclampsia.[8,9,10,18,26]
In our series, eclampsia developed in 42 cases out of 300. Only 1 case had normal fundii (2.38%), 1 case had Grade I hypertensive retinopathy (2.38%), 21 patients had Grade II hypertensive retinopathy (50%), 17 cases had Grade III hypertensive retinopathy (40.48%), and there were 2 cases of retinal detachment (4.76%). Thus, 41 cases (97.62%) had positive fundus findings. Visual disturbances of varying degree were recorded in patients having positive fundus changes. It was markedly reduced in patients having Gr-III and Gr. IV retinopathy.
The reason for this deterioration was macular edema or exudative retinal detachment and disc edema. The recovery of vision is better in patients with Gr. I and Gr. II retinopathy. No case of loss of vision due to cortical lesion was reported in our series.
Anterior segment examination was normal in most cases, except for subconjunctival hemorrhage due to Valsalva's maneuver and reduced sensitivity to corneal sensations.[27,28]
The corelation of fundus changes and fetal outcome is depicted in Table 9.
Table 9.
Distribution of PIH cases on fetal outcome
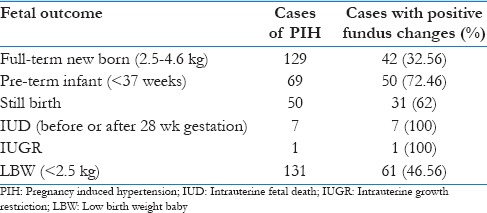
Out of 69 cases of preterm infants, 50 cases, i.e. 72.46% had positive fundus findings. Out of 50 still births, 31 (62%) had positive fundus findings. Out of 131 cases of low birth weight infants, 61 (46.56%) had positive fundus findings.[4,5,6] All seven cases of intra uterine death and one case of intra uterine growth restriction had positive fundus changes.[4,5,6]
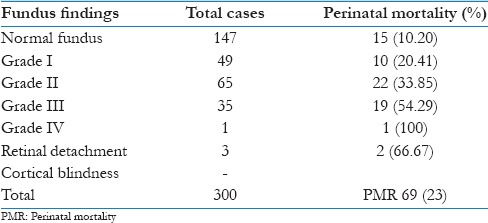
Table 10 shows perinatal mortality increases at par with increasing grade of hypertensive retinopathy as per modified Keith Wagener Barker classification.[4,5,6,19] The perinatal mortality is higher in patients having Grade II, Grade III, and Grade IV hypertensive retinopathy, i.e. 33.85%, 54.29%, and 100%, respectively as compared with normal fundii, i.e. 10.20% and with that with Grade I hypertensive retinopathy, i.e. 20.41%. The overall perinatal mortality was 23%, i.e. 69 out of 300 cases.[4,5,6,7,8,9,10]
Table 10.
The relation of fundus changes with perinatal mortality
Discussions
The fundii of 300 patients with PIH from Nov. 2003 to Jan. 2006 were studied and the findings tabulated.
The incidence of PIH is more common in primipara and second gravida than multigravida because the young retinal arterioles are more sensitive to high blood pressure. The multigravida women are aware of complications of pregnancy and so they attend antenatal clinic regularly. The second high peak was seen in patients having multiple pregnancies.
The incidence of PIH as well as positive fundus findings is more common in age group of 18 to 25 years.
The probable reason for higher incidence in younger age group could be non-compensatory hypertension.
The arteriolar sclerosis of retinal arterioles in elderly patients prevents to develop fundus changes in PIH.
Our study correlates with the study of Neutra et al., who reported that women under 20 years were six to seven times more susceptible than those in age 25-29 years.[18]
PIH as well as positive fundus findings are more common in those patients not attending antenatal clinics.[8,9,10,14,15,16,17,18]
The incidence of fundus findings in PIH was highest in 6-7 months of amenorrhea and 7-8 months of amenorrhea. The cause of lower incidence of fundus changes in 8th and 9th month of amenorrhea may be due to good control of hypertension during the initial months of pregnancy.[8,9,10,14,15,16,17,18]
Burnier et al. recorded in their study of PIH that fundus changes were present in 21% cases before 6 months, 38% between 6 and 7 months, 56.01% between 7 and 8 months of amenorrhea, and in 33% between 8 and 9 months.[7,8]
We have correlated systolic blood pressure with fundus changes [Table 5]. The cause of increased number of fundus changes with systolic blood pressure greater than 180 mmHg may be that the above that level of systolic blood pressure can cause changes in the vessel wall like hypertonus, acute cellular necrosis, disruption of inner as well as outer blood retinal barrier and subsequent circulatory breakdown because of increased permeability.[19,20,21]
The fundus findings run more parallel with diastolic blood pressure than systolic blood pressure, edema or proteinuria.[7,19,20,21] Increase in diastolic blood pressure causes proportionate rise in number of cases with positive fundus changes as compared to systolic blood pressure. There is highest incidence of positive fundus findings when diastolic blood pressure is greater than 110 mmHg, i.e. 68 out of 85 patients (80%). The reason for the vascular changes may be that young vessels do not show fibrotic changes, which are seen in elderly vessels. These young vessels easily break more frequently and earlier when diastolic blood pressure rises more than 110 mmHg. Diastolic blood pressure greater than 110 mmHg is considered a reliable indicator of severity of PIH. Diastolic blood pressure above 120 mmHg is dangerous because most of cases, i.e. 100%, show positive fundus changes [Table 6].[20]
According to Agarwal et al., severity of fundus changes increases at par with rising diastolic blood pressure.[29]
In our study, the incidence of normal fundus in 147 (49%) cases, arterial attenuation in 49 cases (16.33%), arterio venous crossing changes along with retinal edema in 65 cases (21.67%) and hemorrhages and exudates in 35 cases (11.67%) and there was 1 case of papilloedema (0.33%) and 3 cases of retinal detachment (1%)[8,11,12,13,14,15,16,17,22,23,24,25,26] [Table 7].
Schultz et al. and O'Briem et al. in their study of 47 patients found normal retina in 9 (19.1%), arteriolar spasm in 13 (27.5%), retinopathy in 12 (25.5%) while small central retinal detachment in 3 patients.[16]
Kicinski et al., in a study of 139 cases, found 87 (62.5%) with constricted arterioles and 22 cases (15.8%) with organic retinal change including cotton wool exudates, hemorrhages and papilloedema.[8,26]
In our study, the overall incidence of fundus changes was lower than that reported by Kicinski et al., in 1964.[8,26]
Our study shows similarities with the study by Prachakvej et al.,[15] which studied 17 cases of toxemia of pregnancy comprising of 2 cases of mild preeclampsia, 8 cases of severe preeclampsia and 7 cases of eclampsia. He found fundus changes in later two groups.
The cause of less cases of positive fundus changes may be because of present awareness regarding antenatal care than the previous era.[9,10]
Hypertensive changes of fundus are evident by spasm of retinal arterioles which is an early sign of PIH.[11,12,13,14,15,16,17,19,20,21] Arterio venous crossing changes were more closely related to generalized edema and proteinuria. The retinal edema is suggestive of severity of PIH. In the present study, retinal edema is a bad prognostic sign and associated with spontaneous pre-mature delivery and still birth.
In the present series, three cases of retinal detachment were found. Termination of pregnancy was advised. There regression of retinal detachment post partum with restoration of vision.[22,23,24,25,26]
Fry et al.[23] showed that retinal detachment occurs in 1.2% cases of late toxemias and 10.4% cases of eclampsia.
Bosco et al.[24] had reported 10 cases of retinal detachment (RD). Out of 10 patients, 7 patients had no prenatal care. In seven patients, RD was bilateral. Oliver et al.[25] and Uchenik et al.[25] reported a case of retinal detachment in patients having 28 wks amenorrhea. RD was decreased after 12 hrs of lower section caesarean section and completely disappear after 36 hours except at post pole as a local edematous area.
Positive fundus changes in severe preeclampsia cannot be ignored as they can be indicator of impending eclampsia.[8,9,10,14,15,16,17,18]
Fundus findings in severe preeclampsia if neglected can lead to eclampsia with devastating consequences.[4,8,9,10,18]
Eclampsia developed in 42 cases out of 300. Forty-one cases (97.62%) had positive fundus findings.
In eclampsia, the finding of normal fundii indicates excellent prognosis for both the mother and the infant.
There is an increase incidence of pre-term babies, still births, intra uterine death, intra uterine growth restriction and low birth weight babies in patients with positive fundus changes. This high incidence is probably due to placental insufficiency; short gestation period; socio-economic status; nutritional and intrauterine environment; chronic hypertension; birth trauma, infections, increased parity; chronic maternal disease and genetic influence are responsible for increased perinatal mortality.[4,5,6,8,9,10,14,15,16,17,26]
All seven cases of intra uterine death and one case of intra uterine growth restriction had positive fundus changes.
The perinatal mortality was higher in patients having Grade II, Grade III, Grade IV hypertensive retinopathy, i.e. 33.85%, 54.29%, 100%, respectively, as compared to those with normal fundii, i.e. 10.20% and with that with Grade I hypertensive retinopathy, i.e. 20.41%. The overall perinatal mortality was 23%, i.e. 69 out of 300 cases. The high incidence of perinatal mortality is due to pre-term deliveries; intra-uterine death, still birth; the causes of which have been enumerated above [Table 10].
Fundii showing Grade II changes with retinal edema or having Grade III changes, i.e. hemorrhages and exudates, suggest severity of PIH and pregnancy should be terminated; but it can be allowed to continue for 3 to 4 weeks in favor of maturity of fetus.
In severe preeclampsia, Grade III retinopathy termination should be performed at the earliest possible time irrespective of estimated weight of the fetus.
The presence of retinal hemorrhage, transudate or papilledema associated with hypertension, requires prompt interruption of pregnancy regardless of duration of gestation.[8,9,10]
Retinal detachment and papilloedma are indication for termination of pregnancy.
In conclusion, retinal examination reveals important objective information concerning PIH, furthers their accurate diagnosis and refines their management.
The services of an ophthalmologist must be considered essential in proper conduct of obstetrics Department.
Acknowledgement
I would like to acknowledge faculty and staff of M & J Western Regional Institute of Ophthalmology, B. J. Medical College and allied Civil Hospital (Obstetrics-Pediatrics Department). Ahmedabad.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Dieckmann WJ. The toxaemias of pregnancy. 2nd edition. St. Louis: CV Mosby; 1952. pp. 240–9. [Google Scholar]
- 2.Hughes EC, editor. Obstetric-Gynaecology Terminology. Philadelphia: FA Davis; 1972. pp. 422–3. [Google Scholar]
- 3.Davey DA, MacGillivray I. The classification and definition of the hypertensive disorders of pregnancy. Am J Obstet Gynecol. 1988;158:892–8. doi: 10.1016/0002-9378(88)90090-7. [DOI] [PubMed] [Google Scholar]
- 4.Perinatal mortality and morbidity associated with eclampsia. J Obstet Gynaecol India. 1983;33:37–41. [Google Scholar]
- 5.Perinatal mortality. J Obstet Gynaecol India. 1986;36:432–5. [Google Scholar]
- 6.Sandowsky A, Serr DM, Landau J. Retinal changes and foetal prognosis in toxaemia of pregnancy. Obstet Gynecol. 1956;8:426–31. [PubMed] [Google Scholar]
- 7.Burnier R. Albuminurie gravidique et troubles oculaires [dissertation], par le Dr Rene'Burnier, Vigot fre'res. 1911 [Google Scholar]
- 8.Kicinski J, Krawczyk Z, Skwierczynska J. Analysis of labour complicated by late pregnancy toxaemias with refrence to changes in the fundus oculi. Ginekol Pol. 1962;33:217–28. [PubMed] [Google Scholar]
- 9.Dekker G, Sibai B. Primary, secondary and tertiary prevention of pre-eclampsia. Lancet. 2001;357:209–15. doi: 10.1016/S0140-6736(00)03599-6. [DOI] [PubMed] [Google Scholar]
- 10.Walker JJ. Care of the patient with severe pregnancy induced hypertension. Eur J Obstet Gynecol Reprod Biol. 1996;65:127–35. doi: 10.1016/0028-2243(95)02318-m. [DOI] [PubMed] [Google Scholar]
- 11.Ballatyn AJ, Michaelson IC. The fundus of the eye. Baltimore: Williams and Wilkins; 1970. pp. 182–3. [Google Scholar]
- 12.Hallum AV. Eye changes in hypertensive toxaemia of pregnancy. A study of 300 cases. JAMA. 1936;106:1649–51. [Google Scholar]
- 13.Jaffe G, Schatz H. Ocular manifestations of pre-eclampsia. Am J Ophthalmol. 1987;103:309–15. [PubMed] [Google Scholar]
- 14.Gibson GG. The clinical significance of retinal changes in hypertensive toxaemia of pregnancy. Am J Ophthalmol. 1938;21:22. [Google Scholar]
- 15.Prachakvej P. Retinal changes in toxaemia of pregnancy. J Med Assoc Thai. 1971;54:552–8. [PubMed] [Google Scholar]
- 16.Schultz JF, O'Brien CS. Retinal changes in hypertensive toxaemia of pregnancy. A report of 47 cases. Am J Ophthalmol. 1938;21:767–74. [Google Scholar]
- 17.Wagner HP. Arterioles of retina in toxaemia of pregnancy. JAMA. 1933;101:1380–4. [Google Scholar]
- 18.Neutra RR. A case-control study for estimating the risk of eclampsia in California, Colombia. Am J Obstet Gynecol. 1973;117:894. doi: 10.1016/0002-9378(73)90058-6. [DOI] [PubMed] [Google Scholar]
- 19.Norman MK, Wagener HP, Barker NW. Some different types of essential hypertension: Their course and prognosis. Am J Med Sci. 1939;197:332–43. doi: 10.1097/00000441-197412000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Wagener HP, Keith NM. Diffuse arteriolar disease with hypertension and associated retinal lesion. Medicine. 1939;18:317. [Google Scholar]
- 21.Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension. Ophthalmology. 1986;93:1383–400. doi: 10.1016/s0161-6420(86)33554-1. [DOI] [PubMed] [Google Scholar]
- 22.Clapp CA. Detachment of retina in eclampsia and toxaemia of pregnancy. Am J Ophthalmol. 1919;2:473–85. [Google Scholar]
- 23.Fry WE. Extensive bilateral retinal detachment in eclampsia with complete reattachment. Report of two cases. Arch Ophthalmol. 1929;1:609–14. [Google Scholar]
- 24.Bosco JA. Spontaneous nontraumatic retinal detachment in pregnancy. Am J Obstet Gynecol. 1961;82:208–12. [Google Scholar]
- 25.Oliver M, Uchenik D. Bilateral exudative retinal detachment in eclampsia without hypertensive retinopathy. Am J Ophthalmol. 1980;90:792–6. doi: 10.1016/s0002-9394(14)75194-3. [DOI] [PubMed] [Google Scholar]
- 26.Kicinski J. Some problems of pregnancy, labour and puerperium in women with pulmonary tuberculosis. Prace. L'odzkie Towarzystwo Naukowe: Wydzial IV, Nauk Lekarskich; 1964. pp. 54–1. [PubMed] [Google Scholar]
- 27.Landesman R, Douglas RG, Holze E. The bulbar conjunctival vascular bed in toxaemia of pregnancy. Am J Obstet Gynaecol. 1954;68:170–83. doi: 10.1016/0002-9378(54)90476-7. [DOI] [PubMed] [Google Scholar]
- 28.Sharpey-Schafer EP. Effects of valsalva's manoeuvre on the normal and failing circulation. Br Med J. 1955;1:693–5. doi: 10.1136/bmj.1.4915.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agarwal LP, Chawla SR, Saxena RF. Ophthalmodynamometry in toxaemia of pregnancy. Am J Obstet Gynecol. 1957;74:521–5. doi: 10.1016/0002-9378(57)90503-3. [DOI] [PubMed] [Google Scholar]


