Abstract
A 25-year-old woman presented with fever of unknown origin, exhibiting malaise and low-grade fevers in evenings. These fevers exhibited a pattern of starting mid-menstrual cycle with resolution around the onset of menses, matching a pattern of “habitual hyperthermia” reported by H. Reimann in the 1930s. Extensive workup was unremarkable, and the fevers improved on oral synthetic estrogen and progesterone therapy.
Keywords: fever unknown origin, habitual hyperthermia
CASE REPORT
A 25-year-old woman had approximately 1 year of intermittent low-grade fevers (antipyretic unresponsive), with fatigue, malaise, proximal muscular aches, sweats, poor appetite, and 20 pounds weight loss. Her history was significant for birth by cesarean section at 38 weeks for fetal distress, unspecified upper airway surgery in infancy, intermittent fevers that spontaneously resolved in early childhood, mild childhood asthma, frequent otitis media requiring tympanostomy tubes into adulthood, environmental allergies with sinus congestion, eczema, and hives, and frequent viral upper respiratory infections and pharyngitis. In addition, she had self-limited “chronic lymphocytic thyroiditis,” irritable bowel syndrome, and pneumonia as a young adult, but she had no diabetes mellitus or known immunodeficiency. Her ethnicity was Arab and European for her paternal and maternal lineages, respectively, and her family history included a paternal aunt and uncle with unclear fevers in childhood that spontaneously resolved.
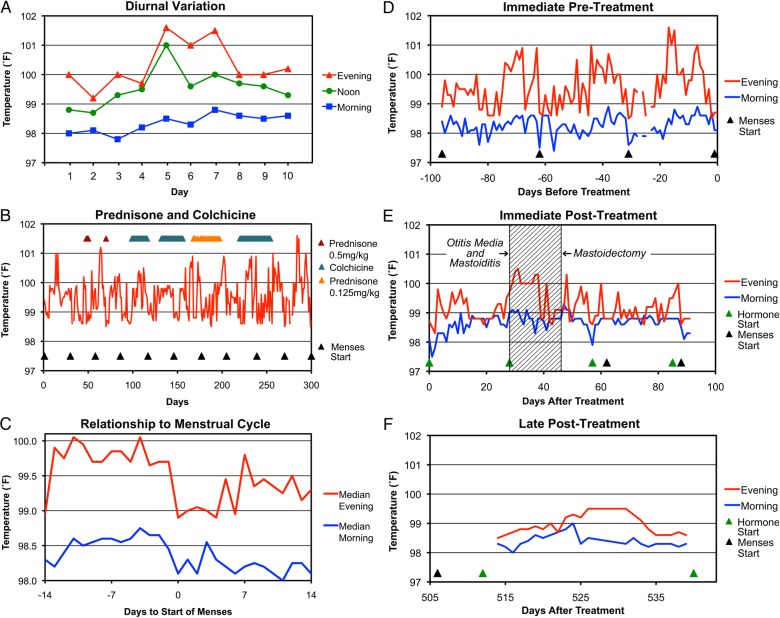
Physical examination, routine blood tests (including complete blood count [CBC]), and chest x-ray were unrevealing. A detailed body temperature log (digital oral readings 8:00 am, noon, and 8:00 pm) displayed exaggerated diurnal temperature variation, with relatively normal morning temperatures and intermittent evening elevations (Figure 1A).
Figure 1.
Pattern of fevers. (A) Ten days of representative body temperatures measured orally at approximately 8:00 am, noon, and 8:00 pm are plotted, showing changing amounts of diurnal variation over time. (B) The 8:00 pm temperatures over 300 days are plotted against trials of prednisone and colchicine, as well as onset of menstrual cycles. (C) The median temperatures across 10 menstrual cycles are plotted in relationship to start of menses. (D) The 8:00 am and 8:00 pm temperatures in the 3 months preceding treatment with oral levonorgestrel/ethinyl estradiol are plotted. (E) Temperatures in the 3 months after starting oral levonorgestrel/ethinyl estradiol are plotted. The shaded area indicates the timing of acute otitis media and mastoiditis culminating in mastoidectomy and tympanostomy tube placement. (F) Temperatures are plotted after several months receiving oral levonorgestrel/ethinyl estradiol.
Additional blood tests returned normal/negative: erythrocyte sedimentation rate (ESR), C-reactive protein, ferritin, complement, d-dimer, interleukin (IL)-1β and IL-6, serum protein electrophoresis, immunoglobulins, Mycobacterium tuberculosis, dihydrorhodamine 123 oxidation, human immunodeficiency virus, hepatitis B virus, hepatitis C virus, Coccidioides immitis, rheumatoid factors, Sjögren's syndrome (SS)A/SSB, Jo 1, and antinuclear antibodies (borderline at 1:40). Periodic fever syndrome genetic screening (Gene Dx) for ELANE (ELA2), LPIN2, MEFV, MVK, NLRP3 (CIAS1), PSTPIP1, and TNFRSF1A revealed only MEFV E148Q heterozygosity. Mitochondrial deoxyribonucleic acid genetic screening (Pro Genetic) for A3243G, T3271C, A8344G, G8363A, T8993C, T8993G, T9176C, G13513A, and T14709C was negative. Computed tomography scan of the sinuses was normal as were magnetic resonance imaging scans of the chest, abdomen, and pelvis.
DISCUSSION
Empiric diagnostic and therapeutic trials of prednisone and colchicine had no discernable effects (Figure 1B). Follow-up revealed a consistent pattern of rising evening temperatures after menses, abruptly dropping just before onset (Figure 1C). To evaluate hormonal involvement, oral combination levonorgestrel/ethinyl estradiol (Jolessa) was initiated. The cyclical pattern of fever (and associated fatigue, malaise, anorexia, sweats, and muscle aches) immediately dampened, although incidentally she developed acute otitis media, mastoiditis, and consistent fevers, which improved after mastoidectomy and tympanostomy tube placement (Figure 1E). Interruption of levonorgestrel/ethinyl estradiol after 3 months was accompanied by recurrent symptoms that were unresponsive to anakinra. Restarting hormonal treatment yielded a long-term response (Figure 1F), although the patient continues to have fevers during frequent episodes of seasonal upper respiratory infections.
“Habitual hyperthermia” is poorly defined, apparently first coined in 1917 as persistently elevated basal body temperature up to 38.0°C without pathology [1]. In 1932 and 1935, Dr. H. A. Reimann [2, 3] described a more specific syndrome in women as exaggeration of diurnal temperature variation in the latter half of the menstrual cycle that was unresponsive to antipyretics. White blood cell count with differential, ESR, and “metabolic tests” were normal. He offered no diagnostic criteria, stating that such observations are “helpful in establishing a diagnosis … but the picture must be regarded as a whole” [2], and no further definitions followed after 1935.
However, habitual hyperthermia has been diagnosed in multiple case series of fever of unknown origin (FUO), assigned to 5 of 199 patients (2.5%) by Knockaert et al [4] in 1992, 11 of 290 patients (3.8%) by Vanderschueren et al [5] in 2003, and 8 of 144 patients (5.5%) by Zenone [6] in 2006, yet these reports lack diagnostic criteria (eg, gender) and/or citations defining the syndrome. Moreover, Vanderschueren et al [5] stated that the standard Petersdorf [7] FUO criteria exclude habitual hyperthermia despite offering it as an etiology for 3.8% of their cohort.
Our case closely matches Reimann's: a woman with exaggerated diurnal temperature variation temporally related to the menstrual cycle, normal CBC, and ESR, and lack of response to antipyretics, although she had associated symptoms and a history of childhood fevers that he did not describe in his cases. It is unclear why she had symptoms associated with her fevers that are more consistent with an inflammatory cause, reflecting either a variant of the syndrome or a superimposed process. Blood IL-1β and IL-6 were normal and anakinra had no effect, supporting his hypothesis of central dysregulation. Although our patient also had superimposed frequent upper respiratory tract infections, the underlying pattern of temperatures absent these infections closely mirrors his reports. Responsiveness to levonorgestrel/ethinyl estradiol additionally suggests a menstrual-related hormonal effect that is responsive to suppression by synthetic estrogen/progesterone. Although variation related to the menstrual cycle has been known since 1868 [8] or earlier, the mechanism of hormonal effects remains unclear [9].
CONCLUSIONS
To our knowledge, this is the first detailed report of habitual hyperthermia since 1935, and it is the only successful therapeutic intervention. How long to treat and the natural history of this syndrome are unclear. When Reimann [10] re-evaluated his first case from 1932 in 1946 after “six pregnancies …, an attack of typhus, several bouts of malaria,” the temperature pattern remained, and he concluded “it will be of interest to see what effect the menopause will have,” although that outcome for this patient and the others he described in the second report appears to be lost to the annals of medical history.
Acknowledgments
We thank the patient for her diligent temperature record-keeping and generous willingness to share her case. We also thank and Dr. Paul Krogstad for manuscript review.
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Moro E. [Habituelle Hyperthermie]. Sonderdruck aus: Monatsschrift für Kinderheilkunde XIV Bd 1917; 4:S. 214–23. [Google Scholar]
- 2.Reimann HA. Habitual hyperthermia. J Am Med Assoc 1932; 99:1860–2. [DOI] [PubMed] [Google Scholar]
- 3.Reimann HA. Habitual hyperthermia: a clinical study of four cases with long continued low grade fever. Arch Intern Med 1935; 55:792–808. [Google Scholar]
- 4.Knockaert DC, Vanneste LJ, Vanneste SB, Bobbaers HJ. Fever of unknown origin in the 1980s. An update of the diagnostic spectrum. Arch Intern Med 1992; 152:51–5. [PubMed] [Google Scholar]
- 5.Vanderschueren S, Knockaert D, Adriaenssens T et al. From prolonged febrile illness to fever of unknown origin: the challenge continues. Arch Intern Med 2003; 163:1033–41. [DOI] [PubMed] [Google Scholar]
- 6.Zenone T. Fever of unknown origin in adults: evaluation of 144 cases in a non-university hospital. Scand J Infect Dis 2006; 38:632–8. [DOI] [PubMed] [Google Scholar]
- 7.Petersdorf RG, Beeson PB. Fever of unexplained origin: report on 100 cases. Medicine 1961; 40:1–30. [DOI] [PubMed] [Google Scholar]
- 8.Squire W. Puerperal temperatures. Trans Obstet Soc Lond 1868; 9:129–44. [Google Scholar]
- 9.Forman RG, Chapman MC, Steptoe PC. The effect of endogenous progesterone on basal body temperature in stimulated ovarian cycles. Human Reprod 1987; 2:631–4. [DOI] [PubMed] [Google Scholar]
- 10.Reimann HA. Habitual hyperthermia; premenstrual fever. J Am Med Assoc 1946; 132:144. [DOI] [PubMed] [Google Scholar]