Summary
Background
Chronic heart failure (HF) or coronary artery disease (CAD) confers risk for thromboembolism and secondary adverse cardiac events (ACEs) (e.g., mortality, myocardial infarction, and stroke). When HF and CAD occur concomitantly, ACE risk is reported to be elevated. We investigated ACEs, their epidemiology, and the resulting burden among patients with concomitant HF and CAD through a structured review of recent literature. Antithrombotic treatment for ACE prevention was assessed.
Methods
Pertinent databases (PubMed, other) were searched for relevant articles published from January 2004 to March 2015. Data collected included ACE incidence, healthcare resource use, costs, change in quality of life attributed to ACEs, and treatment practice for prevention of ACEs in patients with concomitant HF and CAD.
Results
Mortality rates for patients with both HF and CAD ranged from 4.9–12.3% at 30 days to 13.7–86% for periods between 9.9 months and 10 years. Incidence of ACEs among HF patients with CAD is, respectively, at least 82% and 15% higher than for patients without HF or without CAD, except for stroke investigated in two studies. All‐cause and HF‐related hospitalization is the main driver of the economic burden in patients with HF, the majority of whom had CAD origin. Despite high prevalence of ischemic complications, there is limited evidence to support the use of warfarin‐type antithrombotics among HF patients.
Conclusion
This study confirms that patients with concomitant HF and CAD are at elevated risk for ACEs and suggests the need for effective new antithrombotic treatments to further decrease ischemic complication rates in this population.
Keywords: Adverse cardiac events, Antithrombotics, Coronary artery disease, Heart failure
Introduction
Chronic heart failure (HF) is characterized by the inability of the heart to deliver oxygen appropriately for the needs of the body. With an incidence rate that approximates 10 per 1000 population over 65 years of age, HF affects nearly 5.8 million people in the United States, and more than 23 million people worldwide 1 translating to a prevalence of approximately 1–2% in developed countries 2. This prevalence rises to more than 10%1 among persons aged 85 years or older 2.
Of HF cases, at least half are systolic, referring to HF with reduced left ventricular ejection fraction (LVEF) indicative of systolic dysfunction; diastolic HF on the other hand refers to HF with diastolic dysfunction where LVEF is relatively preserved 4. The cause of approximately two‐thirds of systolic HF cases (i.e., with reduced LVEF) is coronary artery disease (CAD) 4, characterized by angina and reduced exercise tolerance due to atherosclerotic plaque formation 5.
Few studies have focused on HF patients with concomitant stable CAD. It is known that patients with cardiovascular (CV) disease in general are at risk of developing secondary adverse cardiac events (ACE), including all‐cause and CV death, nonfatal myocardial infarction (MI), nonfatal stroke, all‐cause and CV hospitalization 6. Further, several studies have reported outcomes in HF patients after an acute event (e.g., acute MI) 7, 8, 9, 10, 11, 12, 13. However, although there is some published evidence that concomitance of HF and CAD can increase the risk of death 14, there has been no synthesis to date of information on the range of secondary ACE in patients with concomitant HF and CAD. Furthermore, beyond their clinical burden, secondary ACE can have an important economic and humanistic impact in this large population of chronic HF patients with CAD, but again, this information has not been summarized in the literature 15.
Regarding treatment for HF, despite the current therapies available, patients with HF remain subject to high mortality rates and reduced quality of life 16. Further, patients with chronic HF are at increased risk of thromboembolism, even in the absence of atrial fibrillation (AF) 17. Heart failure is characterized by abnormalities in blood flow, vessel wall, and blood constituents, three prerequisites for thrombosis 17. However, the potential benefits of antithrombotic therapy to reduce incidence of secondary ACE in HF patients, and more specifically in HF patients with CAD, remain unclear.
The overall aim of this study was to investigate secondary ACE in populations of patients with concomitant chronic HF and stable CAD within the last decade. To do so, published information related to the incidence of secondary ACE, their economic and humanistic burden, and treatment practice with antithrombotic (anticoagulant/antiplatelet) therapy for prevention of such events in this patient population were reviewed.
Methods
Disease Definitions
In this study, HF was defined as chronic HF (HF for at least 3 months) with left ventricular dysfunction (LVEF ≤ 40%) in men and women aged 18 years and older.
Besides the term “coronary artery disease,” CAD was defined as: previous MI, history of coronary artery bypass graft (CABG), condition requiring coronary angiography and demonstrating at least 50% stenosis of one or more arteries, history of percutaneous coronary intervention (PCI), or in case of no documented history of MI, electrocardiogram (ECG) evidence (Q waves) with corresponding wall motion abnormality on echocardiogram.
Secondary ACE of interest include CV and all‐cause death, nonfatal MI, nonfatal stroke, CV and all‐cause hospitalization, and bleeding (major or minor).
Data Sources and Searches
A comprehensive literature search was performed to identify studies on the burden of secondary ACE among patients with concomitant HF and CAD. Sources of information were the National Library of Medicine's PubMed, EMBASE, and Cochrane reviews. Searches were limited to English‐language articles published between January 1, 2004, and March 31, 2015. Search terms used included a combination of the following: [prevalence, incidence, epidemiol*, burden, cost, economic evaluation, cost of illness, budget impact, resource use, quality of life, MLHFQ, MLHF, KCCQ, EQ‐5D, EuroQoL, EuroQuol, SF‐12, SF‐36, chronic questionnaire, quality of life in severe questionnaire, patient reported outcomes, practice pattern, current practice, prescription, registry, observational, survey, secondary prevention, aspirin, clopidogrel, ticagrelor, prasugrel, factor Xa, antiplatelet, platelet aggregation inhibitor], [major ACE, major adverse CV events, death, mortality, MI, stroke, hospitalization, bleeding], and [HF, CAD, MI, CABG, PCI, coronary angiography, abnormal echocardiogram, ischemic, ischaemic].
Selection Criteria
Selected studies were limited to relevant patient populations. Study types included were as follows: observational, prospective, historical, cohort studies; randomized controlled studies; registry‐based, hospital, and claims database analyses; meta‐analyses; and systematic reviews. Bibliographies of the latter two were used as sources for individual studies not captured by the primary searches. Case reports, commentaries, letters, news, withdrawn articles, and historical reports were excluded. Studies reporting data in HF patients following an acute event (e.g., acute MI) or in HF patients with AF were also excluded.
Data Extraction and Analysis
Data on the prevalence, incidence, healthcare resource use, costs, and changes in patient's quality of life attributed to secondary ACE, as well as treatment practice patterns for prevention of secondary events in patients with HF and CAD were collected. We restricted treatment practice patterns to antiplatelets and anticoagulants in light of the potential importance of thromboembolism in patients with concomitant HF and CAD. Data on individual events and composite endpoints were extracted. Prevalence was defined as the proportion of patients who had experienced an adverse cardiac event in a given study population. Incidence was defined as the occurrence of an adverse cardiac event over a defined time period (follow‐up). Data on hospital admission (rate of hospitalization and length of stay) were used to report healthcare resource utilization among HF patients with CAD. All original costs were inflated to the year 2014, then converted to Euros (€) if necessary, using a currency calculator available on http://www.x-rates.com/.
Results
From a total of 224 full‐text articles assessed for eligibility, 20 studies were selected that reported information relevant to patients with concomitant HF and CAD that encompassed information on the incidence of ACE, their impact on healthcare resource utilization, costs, and quality of life, as well as on current practice patterns for secondary prevention of these events (Figure 1).
Figure 1.
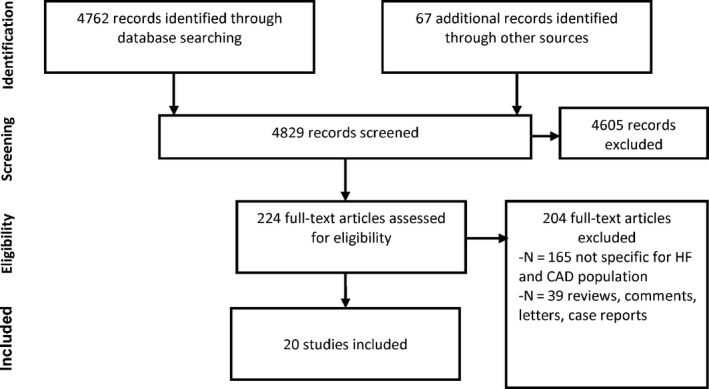
Search results – Prisma diagram.
Incidence of Adverse Cardiac Events in Patients with HF and CAD
Our study found country‐specific incidence data on ACE among patients with both HF and CAD in 11 studies, from countries including Australia 18, Canada 19, 20, Czech Republic 21, Denmark 22, France 23, Italy 24, Japan 25, the United States 26, 27 as well as three multinational studies 27, 28, 29. Nine studies reported incidence rates of ACE among patients with both HF and CAD (Table 1).
Table 1.
Incidence rates (%) of adverse cardiac events in patients with concomitant HF and CAD and patients with only HF or CAD
| Country/Study | Time frame | Patients | All‐cause mortality | CV mortality | MI | Stroke | Composite 1a | Composite 2a | Composite 3a |
|---|---|---|---|---|---|---|---|---|---|
| Australia/Lu et al., 2011 18 | 30 days | HF and CAD | 4.9b | NR | 4.4 | NR | 12.1b | NA | NA |
| No HF and CAD | 1.9 | 2.4 | 5.9 | ||||||
| 1 year | HF and CAD | 13.7b | 13.2b | 28.6b | |||||
| No HF and CAD | 3.5 | 4.3 | 12.6 | ||||||
| Canada/Ouzounian et al., 2009 20 | 5 years | HF, no CAD | 43–58 | NR | NR | NR | NA | 68–73 | NA |
| HF and CAD | 55–68c | 78–84c | |||||||
| Canada/Nagendran et al., 2014 19 | 30 days | HF (LVEF ≤ 0.35) and CAD | 6.78b | NR | NR | NR | NA | NA | NA |
| No HF (LVEF > 0.35) and CAD | 2.07 | ||||||||
| Denmark/Andersson et al., 2014 22 | 30 days | HF and CAD | 12.3b | 7–10b | 1.5–1.6b | 0.02–0.1 | NA | NA | 10.0b |
| No HF and CAD | 3.9 | 2 | 0.8–0.9 | 0.2 | 2.9 | ||||
| France/Rusinaru et al., 2014 23 | 1 year | HF, no CAD | 17 | NR | NR | NR | NA | NA | NA |
| HF and CAD | 38c | ||||||||
| 10 years | HF, no CAD | 67 | |||||||
| HF and CAD | 86c | ||||||||
| Japan/Marui et al., 2014 25, d | 30 days | HF and CAD (PCI) | 1.3 | NR | 1.3 | 1.0 | NA | NA | NA |
| HF and CAD (CABG) | 2.0 | NR | 1.0 | 1.5 | |||||
| 3 years | HF and CAD (PCI) | 21c | 14c | 4 | 7 | ||||
| HF and CAD (CABG) | 16 | 9 | 3 | 6 | |||||
| Multinational/Mentz et al., 2013 27 (EVEREST) | 9.9 months (median) | HF, no CAD | 23.5 | 18.1 | 0.5 | 1.6 | NA | NA | NA |
| HF and CAD | 28.1c | 21.6c | 2.5c | 1.7 | |||||
| US and Canada/Gheorghiade et al., 2011 26 (BEST) | 26 months (median) | HF, no CAD | 24 | 20 | NR | NR | NA | NA | NA |
| HF and CAD | 37c | 32c | |||||||
| Multinational/Velazquez et al., 2011 29 (STICH) | 56 months (median) | HF and CAD (CABG) | 36 | 28 | NR | NR | NA | NA | NA |
BEST, Beta‐Blocker Evaluation of Survival Trial; CABG, coronary artery bypass graft; CAD, coronary artery disease; CV, cardiovascular; EVEREST, Efficacy of Vasopressin Antagonist in Heart Failure Outcome Study with tolvaptan; HF, heart failure; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NA, not applicable; NR, not reported; PCI, percutaneous coronary intervention; STICH, Surgical Treatment for Ischemic Heart Failure; US, United States.
Composite 1: death, MI, or target vessel revascularization; Composite 2: death, readmission for HF, admission for coronary events, or ischemic stroke; Composite 3: acute MI, ischemic stroke, or CV death.
Significant difference between CAD patients with and without HF.
Significant difference between HF patients with and without CAD.
Comparison between PCI and CABG, no controls without CAD or without HF.
All‐cause mortality among patients with HF and CAD, as shown in Table 1, indicated that 30‐day incidence ranged from 4.9% to 12.3%18, 19, 22 with one study reporting lower rates after PCI (1.3%) or CABG (2.0%) interventions 25. One‐, three‐, five‐, and 10‐year incidence of all‐cause mortality in patients with HF and CAD was also reported (13.7–38%18, 23, 16–21%25,55–68%20, and 86%23, respectively). Three randomized controlled studies reported all‐cause mortality rates of 28%27,36%29, and 37%26 after median follow‐up durations of 9.9, 56, and 26 months, respectively. Regarding incidence of CV death, one study reported that 7–10% of patients with HF and CAD died after 30 days 22, while figures of 21.6%27, 28%29, and 32%26 were reported over longer follow‐up periods in the aforementioned randomized controlled studies. Lower rates were reported at 3 years after PCI or CABG interventions (14% and 9%, respectively) 25.
The 30‐day incidence of MI among patients with concomitant HF and CAD ranged from 1.5 to 4.4%18, 22 with lower rates reported after PCI (1.3%) or CABG (1.0%) interventions in another study 25. Incidence of MI in patients with both HF and CAD was also reported at 9.9 months (2.5%)27 and at 1 year (13.2%)18, and after 3 years following PCI or CABG interventions (4% and 3%, respectively) 25.
For stroke in patients with both HF and CAD, very low (≤0.1%) 30‐day incidence rates were reported in a single study 22, but higher rates were reported for 30 days and 3 years after PCI (1% and 7%, respectively) or CABG (1.5% and 6%, respectively)25 and after 9.9 months (1.7%) in another study 27. Finally, incidence of different composites of the ACE described above was reported in three studies (Table 1).
Three studies in Table 1 reported incidence rates of various adverse cardiac events among HF patients with concomitant CAD compared with CAD patients without HF 18, 19, 22. Higher rates were observed in patients with HF and CAD except for MI and stroke at 30 days 18, 22. Incidence of adverse cardiac events is at least 82% greater in patients with both HF and CAD compared with CAD patients without HF.
Four studies in Table 1 reported incidence of various ACE among HF patients with concomitant CAD compared with HF patients without CAD 20, 23, 26, 27. Higher rates were observed in patients with both HF and CAD, except for stroke at 9.9 months in an individual study 27. Incidence of ACE is at least 15% greater in patients with HF and CAD than in HF patients without CAD.
Table 2 shows data from studies that reported the prognostic value of either HF in CAD patients or CAD in HF patients on the incidence of the ACE described above, expressed as hazard ratios after Cox regression analyses. Two studies reported a higher risk of all‐cause mortality in CAD patients with HF compared without HF although the effect was nonsignificant (P = .08) in the shorter time frame study (1 year). Compared with HF patients without CAD, patients with both HF and CAD are subject to a 1.5‐ to 3.8‐fold increased risk of subsequent ACE including all‐cause and CV death, MI, and a composite of all‐cause death or CV hospitalization; this was shown for all studies except the one with a follow‐up period of less than a year 27. It was noted that patients with severe HF (NYHA III‐IV and LVEF < 0.35) and CAD who also have renal impairment are at further risk of all‐cause mortality (data not shown) 30.
Table 2.
Prognostic impact of HF or CAD on incidence of adverse cardiac events in patients with HF and CAD
| Country/Study | Time frame | Population | Hazard ratio (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| All‐cause death | CV death | MI | Stroke | Compositea | |||
| Australia/Lu et al., 2011 18 | 1 year | Patients undergoing PCI with HF versus without | 1.7 (0.93–3.1) | NR | NR | NR | NA |
| Canada/Nagendran et al., 2014 19 | 8 years | Patients undergoing CABG with HF versus without | 2.43 (1.78–3.32) | NR | NR | NR | NA |
| Czech Republic/Rosolova et al., 2005 21 | 4 years | HF with a history of MI versus without | 2.386 (1.59–3.59) | NR | NR | NR | NA |
| France/Rusinaru et al., 2014 23 | 10 years | HF with reduced EF (<50%; mean at 35%) and CAD versus no CAD | 1.60 (1.19–2.15) | 2.01 (1.38–2.92) | 3.84 (1.16–12.7) | NR | NA |
| Italy/Fumagalli et al., 2014 24 | 27 months | HF with severe LVSD and ICD placement with CAD versus without | 1.67 (1.43–1.97) | NR | NR | NR | NA |
| Multinational/Mentz et al., 2013 27 (EVEREST) | 9.9 months (median) | Systolic CHF (EF ≤ 40%) with CAD versus without | 1.12 (0.97–1.30) | 1.15 (0.97–1.35) | NR | NR | NA |
| US and Canada/Gheorghiade et al., 2011 26 (BEST) | 26 months (median) | Systolic CHF (EF ≤ 35%) with CAD versus without | 1.69 (1.47–1.95) | 1.77 (1.51–2.07) | NR | NR | NA |
| Multinational/Manzano et al., 2011 28 (SENIORS) | 21 months | HF (EF ≤ 35%) with prior MI versus without | 1.743 (1.374–2.464) | NR | NR | NR | 1.545 (1.264–1.905) |
BEST, Beta‐Blocker Evaluation of Survival Trial; CABG, coronary artery bypass graft; CAD, coronary artery disease; CHF, chronic heart failure; CI, confidence interval; CV, cardiovascular; EF, ejection fraction; EVEREST, Efficacy of Vasopressin Antagonist in Heart Failure Outcome Study with tolvaptan; HF, heart failure; ICD, implantable cardioverter defibrillator; LVSD, left ventricular systolic dysfunction; MI, myocardial infarction; NA, not applicable; NR, not reported; PCI, percutaneous coronary intervention; SENIORS, Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisation in Seniors with Heart Failure; US, United States.
All data are from multivariate analyses.
Composite: all‐cause mortality or cardiovascular hospital admission.
Resource Use and Costs Associated with Adverse Cardiac Events in Patients with HF and CAD
Data on resource use associated with ACE in patients with HF (of whom the majority were of CAD origin) were found in two studies covering Canada, the UK, and the United States from the Warfarin and Antiplatelet Therapy in Chronic Heart Failure (WATCH) trial 31 and the multinational cohort in Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM)‐Added 32 trial (Table 3). These trials enrolled HF patients of whom 72% and 62% were of CAD origin, respectively. Annual rates ranging from 38 to 89% and from 8 to 32% were reported for all‐cause and HF‐related hospitalizations, respectively. Lower incidence rates were reported for other causes of hospitalization such as MI and stroke in the CHARM‐Added trial (<4%).
Table 3.
Adverse cardiac event‐related resource use (annual hospitalization rates) in WATCH and CHARM‐Added trials
| Trial‐Country | Population/follow‐up | All‐cause | HF‐related | Other causes | |
|---|---|---|---|---|---|
| MI | Stroke | ||||
| WATCH 31, a | HF, 72% CAD/1.9 years (mean) | ||||
| Canada | 0.38–0.50 | 0.11–0.22 | NR | NR | |
| UK | 0.43–0.47 | 0.08–0.14 | NR | NR | |
| US (Veterans Administration) | 0.60–0.89 | 0.09–0.32 | NR | NR | |
| US (Non‐Veterans Administration) | 0.64–0.83 | 0.19–0.29 | NR | NR | |
| CHARM‐Added 32, b | HF, 62% CAD/41 months (median) | ||||
| International (26 countries) | 0.668–0.675 | 0.253–0.300 | 0.028–0.039 | 0.027–0.027 | |
CAD, coronary artery disease; HF, heart failure; MI, myocardial infarction; NR, not reported; US, United States.
Lowest and highest rates of aspirin, clopidogrel, and warfarin trial.
Rates for candesartan and placebo arms, respectively.
Costs associated with ACE and medications were also found in the WATCH and CHARM‐Added trial reports. Specifically, annual total medical costs per patient for Canada, the UK, and the United States were reported in the first trial 31, and both hospital and total medical daily costs per patient for France, Germany, Italy, and the UK were reported in the second trial (Table 4) 32, 33. In the WATCH trial, inpatient (hospitalization) costs accounted for about 87% of total medical costs 31. Total medical costs including hospitalizations, emergency department visits, outpatient medical procedures, and medications were higher in the United States versus Canada and were lowest in the UK. In the CHARM‐Added trial, hospital costs accounted for 64–69%, 47–54%, 50–55%, and 69–73% of total medical costs (including in addition CV procedures and medications) in the candesartan and placebo arms in France, Germany, Italy, and the UK, respectively. Both hospital and total medical costs were higher for the UK, followed by France, Italy, and Germany (Table 4).
Table 4.
Adverse cardiac event‐related hospital costs and total medical costs in WATCH and CHARM‐Added trials
| Trial/Country | ||
|---|---|---|
| WATCH 31 | Hospital annual cost/patient | Total medical annual cost/patient (€2014)a |
| Canada | NR | 3643–4053 |
| UK | NR | 1997–2380 |
| US (Veterans Administration) | NR | 6994–8553 |
| US (Non‐Veterans Administration) | NR | 5366–6925 |
| CHARM‐Added 32, 33 | Hospital daily cost/patient (€2014)b | Total medical daily cost/patient (€2014)b |
|---|---|---|
| France | 14.04–16.03 | 22.04–23.21 |
| Germany | 6.76–7.71 | 14.25–14.25 |
| Italy | 9.46–10.95 | 19.10–20.00 |
| UK | 18.48–21.06 | 26.83–28.75 |
NR, not reported; UK, United Kingdom; US, United States.
Lowest and highest cost of aspirin, clopidogrel, and warfarin trial.
cost for candesartan and placebo arms, respectively.
Association Between Quality of Life and Adverse Cardiac Events in Patients with HF and CAD
No studies addressing the direct effect of ACE on quality of life of patients with HF and CAD were found. However, evidence of an association between quality of life and adverse events in a group of HF patients of whom the majority had CAD was found in two studies from the UK 34, 35. Using the Minnesota Living with Heart Failure Questionnaire (MLHFQ), one study showed that poor quality of life at baseline was associated with increased risk of mortality and hospital admissions in patients with HF (62% of CAD origin) 35. In the other study, in which 77% of HF patients had CAD, better quality of life was associated with improved survival based on MLHFQ and EuroQoL measures. The same study showed that treatment with loop diuretics and angiotensin‐converting enzyme inhibitors improved quality of life over baseline among surviving patients (MLHFQ physical scores 18.8 ± 11.8 vs. 21.7 ± 11.2 at baseline; P = 0.016) 34.
Antiplatelet and Anticoagulant Practice Patterns in Patients with HF and CAD
Given the evidence above indicating that patients with HF and CAD are subject to greater incidence of secondary ACE compared with patients with HF alone, treatment practices in this population were investigated. For reference, clinical practice guidelines from both the ESC in Europe and the ACCF/AHA in the United States state that there is no evidence supporting the use of antiplatelets or anticoagulants other than aspirin to prevent ACE in patients with HF, except for patients those who suffer from AF or have experienced a prior thromboembolic event 4, 36. Prevalence of AF in patients with HF varies from 4% in NYHA class I to 40% in NYHA class IV patients 36. For patients with stable CAD, aspirin (or clopidogrel when aspirin is contraindicated) is also recommended 5, 37.
We selected observational and clinical studies reporting antiplatelet and anticoagulant use in patients with HF and CAD; these are summarized in Table 5. It should be noted that data are from populations with different comorbidities, and the percentage of patients with AF was not reported in any of these studies. The antiplatelet aspirin was used by 73–84% of patients, while clopidogrel was used by 13–16% of patients in a clinical study 29 and by 55% of HF patients after MI in an observational study 38. This higher percentage in the latter study may reflect recommendations to prescribe dual antiplatelet therapy among patients with MI 5, 37. Use of any thienopyridine and a nonaspirin antiplatelet was estimated at 25% and 6.1%, respectively, in two other studies 39, 40. The anticoagulant warfarin was used by 13–29% of patients with HF and CAD in these studies (Table 5). Because AF is a common comorbidity especially among patients with severe chronic HF, these results should be interpreted with caution.
Table 5.
Practice patterns of antiplatelets and anticoagulants among patients with concomitant HF and CAD
| Country/Study | Study design | Population | Observation period | Antiplatelet use, % patients | Anticoagulant use, % patients | ||
|---|---|---|---|---|---|---|---|
| Aspirin | Clopidogrel | Other | Warfarin | ||||
| Australia/Krum et al., 2006 38 | Multicentre | 116 patients with MI and HF | 2004–2005 | 84 | 55 | NR | 13 |
| Canada/Ezekowitz et al., 2004 39 | Prospective cohort | 6427 patients with HF and angiographically proven CAD | NR | 73 | NR | 25a | 29 |
| US/Newby et al., 2006 40 | Retrospective registry (database) | 8914 patients with CAD and HF | 1995–2002 | 75.3 | NR | 6.1b | 13 |
| International‐STICH trial (22 countries)/Velazquez et al., 201129 | Multicenter, nonblinded, randomized | 1212 patients with CAD suitable for revascularization and LVEF ≤ 0.35 | July 2002‐May 2007 | 84 | 13–16 | NR | 20–21 |
CAD, coronary artery disease; HF, heart failure; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NR, not reported; STICH, Surgical Treatment for Ischemic Heart Failure; US, United States.
Any thienopyridine.
Nonaspirin antiplatelet.
Discussion
Coronary artery disease is the major cause of chronic systolic HF, with a prevalence of more than 60% in patients with reduced systolic function;4 however, whether it constitutes a real thrombotic concern in patients with chronic HF is largely unknown. In the present study, we report the incidence and burden of ACE and antithrombotic practice patterns in chronic HF patients with CAD through a structured review of the recent literature. Incidence data specific to this population showed that these patients are exposed to an increased risk of subsequent ACE compared with HF patients without CAD or CAD patients without HF. Hospitalization, mainly due to HF, occurred in 38–89% of patients and accounted for 47–87% of total medical costs; it was the main driver of the economic burden in patients with chronic HF and CAD. Finally, anticoagulant treatment was found to be used by an appreciable proportion (13–29%) of HF patients with CAD and different comorbidities.
We observed heterogeneity in incidence rates across studies within each adverse event category. Besides being due to different follow‐up times, this may be explained by the heterogeneity within the CAD populations for which data were reported. Coronary artery disease defines a heterogeneous patient population, including patients with previous MI, stable or recurrent angina, patients necessitating vascular interventions such as PCI and CABG, and others (described under Methods) 5. Heterogeneity can also exist among patients with HF due to varying severity of left ventricular systolic dysfunction. Furthermore, heterogeneity in the nature of events included in the composite endpoints makes comparison difficult between studies.
Although published information on chronic HF and CAD as separate disease states is abundant in the literature, much less information is available specifically for patients with concomitant HF and CAD, and several gaps were identified by the present study. Data on stroke, MI, and CV death are scarce in this population, and data on bleeding—one adverse cardiac event consequent to the use of antithrombotic treatment—were lacking for this HF and CAD patient population. Risk of bleeding is not necessarily a factor in patients with HF but could markedly increase in a subgroup of patients with CAD treated with antiplatelets or anticoagulants. Further, epidemiological and economic data were found for a small number of countries. Information on the impact of individual events on health‐related quality of life, resource use, and medical costs was also inadequate. However, despite these limitations, this study identified an important clinical and economic burden associated with occurrence of ACE in patients with chronic HF and CAD.
As with any study that relies on literature search methodology, there are inherent limitations. Studies chosen for inclusion may be subject to selection bias; to circumvent this, two of the authors screened and reviewed the relevant articles. Further, because we restricted the time frame of the search, this may have contributed to a fewer number of published studies retrieved for specific topics, as described above. However, because we were interested in recent rather than historical information, the data retrieved, although from a smaller number of studies, are likely more meaningful to present‐day scenarios.
Regarding anticoagulation treatment, whether it could be useful in HF patients with CAD remains an open question. Currently, warfarin is recommended only for HF patients with AF or at increased risk of thromboembolism. Warfarin is associated with an increased risk of hemorrhage, and among a sample of patients with HF but without AF, it was associated with a reduction of stroke but no impact on survival compared with standard antiplatelet treatment 41, 42, 43.In current practice, the present study showed that an appreciable number of HF patients with CAD and different comorbidities used anticoagulation treatment (warfarin). Whether HF patients with comorbidities such as CAD can benefit from anticoagulation treatments other than warfarin is an interesting avenue for future clinical trials. New oral anticoagulants, such as dabigatran, rivaroxaban and apixaban, have been shown to reduce the risk of stroke in patients with AF, and with or without HF 17, but their potential benefits in HF patients without AF have not been explored. Furthermore, the demonstration in the ATLAS ACS 2 TIMI 51 study that subjects with recent acute coronary syndrome (ACS) and HF showed decreased risk of primary efficacy endpoint events (composite of CV death, MI, and stroke) with the use of rivaroxaban compared with placebo 44 provides rationale for the exploration of rivaroxaban effects in similar patients with chronic HF and CAD but without a recent ACS event.
In conclusion, this study highlights the burden of ACE in patients with HF and CAD and identifies several gaps in the published literature for this specific population. The limited information available pertaining to ACE in patients with concomitant HF and CAD calls for the need to conduct large observational studies and analyses of registry‐based data, especially for reporting the impact of events on resource use and costs, on patient quality of life, and regarding current practice of antiplatelet and anticoagulant treatments in this population.
Conflict of Interest Statement
Louis Lavoie, Hanane Khoury, and Sharon Welner received consultancy fees from Bayer Pharma AG to conduct the study. Jean‐Baptiste Briere is an employee of Bayer Pharma AG.
Author Contributions
LL contributed to concept/design, data analysis/interpretation, drafting of the article, critical revision of the article, and data collection; HK and JBB contributed to concept/design, data analysis/interpretation, and critical revision of the article; SW contributed to concept/design, data analysis/interpretation, drafting of the article, and critical revision of the article.
Financial Support
This study was funded by Bayer HealthCare Pharmaceuticals.
Note
As a point of comparison, the global prevalence of diabetes mellitus was estimated at 8.3% in 2013 3.
References
- 1. Liu L, Eisen HJ. Epidemiology of heart failure and scope of the problem. Cardiol Clin 2014;32:1–8. vii. [DOI] [PubMed] [Google Scholar]
- 2. Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart 2007;93:1137–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. International Diabetes Federation . IDF diabetes atlas, 6th edition. Brussels, Belgium: 2013. http://www.idf.org/diabetesatlas/download-book. (Accessed 6 Jan 2014). [Google Scholar]
- 4. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33:1787–1847. [DOI] [PubMed] [Google Scholar]
- 5. Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949–3003. [DOI] [PubMed] [Google Scholar]
- 6. Hicks KA, Hung HMJ, Mahaffey KW, Mehran R. Standardized definitions for end point events in cardiovascular trials. 2010. http://www.clinpage.com/images/uploads/endpoint-defs_11-16-2010.pdf. (Accessed 21 Jun 2013).
- 7. Abildstrom SZ, Ottesen MM, Rask‐Madsen C, Andersen PK, Rosthoj S, Torp‐Pedersen C, Kober L. Sudden cardiovascular death following myocardial infarction: the importance of left ventricular systolic dysfunction and congestive heart failure. Int J Cardiol 2005;104:184–189. [DOI] [PubMed] [Google Scholar]
- 8. Bertomeu‐Gonzalez V, Nunez J, Nunez E, et al. Prognostic effect of renal dysfunction after ST‐segment elevation myocardial infarction with and without heart failure. Int J Cardiol 2006;112:159–165. [DOI] [PubMed] [Google Scholar]
- 9. Bonde L, Sorensen R, Fosbol EL, et al. Increased mortality associated with low use of clopidogrel in patients with heart failure and acute myocardial infarction not undergoing percutaneous coronary intervention: A nationwide study. J Am Coll Cardiol 2010;55:1300–1307. [DOI] [PubMed] [Google Scholar]
- 10. Hung J, Teng TH, Finn J, et al. Trends from 1996 to 2007 in incidence and mortality outcomes of heart failure after acute myocardial infarction: A population‐based study of 20,812 patients with first acute myocardial infarction in Western Australia. J Am Heart Assoc 2013;2:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Juilliere Y, Cambou JP, Bataille V, et al. Heart failure in acute myocardial infarction: A comparison between patients with or without heart failure criteria from the FAST‐MI registry. Rev Esp Cardiol (Engl Ed) 2012;65:326–333. [DOI] [PubMed] [Google Scholar]
- 12. Lewinter C, Bland JM, Crouch S, et al. Impact of aspirin and statins on long‐term survival in patients hospitalized with acute myocardial infarction complicated by heart failure: An analysis of 1706 patients. Eur J Heart Fail 2014;16:95–102. [DOI] [PubMed] [Google Scholar]
- 13. Velazquez EJ, Francis GS, Armstrong PW, et al. An international perspective on heart failure and left ventricular systolic dysfunction complicating myocardial infarction: The VALIANT registry. Eur Heart J 2004;25:1911–1919. [DOI] [PubMed] [Google Scholar]
- 14. Smith SC Jr, Blair SN, Bonow RO, et al. AHA/ACC Scientific Statement: AHA/ACC guidelines for preventing heart attack and death in patients with atherosclerotic cardiovascular disease: 2001 update: A statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation 2001;104:1577–1579. [DOI] [PubMed] [Google Scholar]
- 15. Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: Lessons learned from hospitalized heart failure registries. J Am Coll Cardiol 2014;63:1123–1133. [DOI] [PubMed] [Google Scholar]
- 16. McMurray JJV, Stewart S. The burden of heart failure. Eur Heart J Suppl 2002;4(Suppl. D):D50–D58. [Google Scholar]
- 17. Gheorghiade M, Vaduganathan M, Fonarow GC, et al. Anticoagulation in heart failure: Current status and future direction. Heart Fail Rev 2013;18:797–813. [DOI] [PubMed] [Google Scholar]
- 18. Lu KJ, Yan BP, Ajani AE, et al. Impact of concomitant heart failure on outcomes in patients undergoing percutaneous coronary interventions: Analysis of the Melbourne Interventional Group registry. Eur J Heart Fail 2011;13:416–422. [DOI] [PubMed] [Google Scholar]
- 19. Nagendran J, Norris CM, Appoo JJ, Ross DB, Nagendran J. Left ventricular end‐diastolic pressure predicts survival in coronary artery bypass graft surgery patients. Ann Thorac Surg 2014;97:1343–1347. [DOI] [PubMed] [Google Scholar]
- 20. Ouzounian M, Tu JV, Austin PC, Chong A, Liu PP, Lee DS. Statin therapy and clinical outcomes in heart failure: A propensity‐matched analysis. J Card Fail 2009;15:241–248. [DOI] [PubMed] [Google Scholar]
- 21. Rosolova H, Cech J, Simon J, et al. Short to long term mortality of patients hospitalised with heart failure in the Czech Republic–a report from the EuroHeart Failure Survey. Eur J Heart Fail 2005;7:780–783. [DOI] [PubMed] [Google Scholar]
- 22. Andersson C, Merie C, Jorgensen M, et al. Association of beta‐blocker therapy with risks of adverse cardiovascular events and deaths in patients with ischemic heart disease undergoing noncardiac surgery: A Danish nationwide cohort study. JAMA Intern Med 2014;174:336–344. [DOI] [PubMed] [Google Scholar]
- 23. Rusinaru D, Houpe D, Szymanski C, Levy F, Marechaux S, Tribouilloy C. Coronary artery disease and 10‐year outcome after hospital admission for heart failure with preserved and with reduced ejection fraction. Eur J Heart Fail 2014;16:967–976. [DOI] [PubMed] [Google Scholar]
- 24. Fumagalli S, Gasparini M, Landolina M, et al. Determinants of all‐cause mortality in different age groups in patients with severe systolic left ventricular dysfunction receiving an implantable cardioverter defibrillator (from the Italian ClinicalService Multicenter Observational Project). Am J Cardiol 2014;113:1691–1696. [DOI] [PubMed] [Google Scholar]
- 25. Marui A, Kimura T, Nishiwaki N, et al. Three‐year outcomes after percutaneous coronary intervention and coronary artery bypass grafting in patients with heart failure: From the CREDO‐Kyoto percutaneous coronary intervention/coronary artery bypass graft registry cohort‐2. Eur J Cardiothorac Surg 2015;47:316–321. [DOI] [PubMed] [Google Scholar]
- 26. Gheorghiade M, Flaherty JD, Fonarow GC, et al. Coronary artery disease, coronary revascularization, and outcomes in chronic advanced systolic heart failure. Int J Cardiol 2011;151:69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mentz RJ, Allen BD, Kwasny MJ, et al. Influence of documented history of coronary artery disease on outcomes in patients admitted for worsening heart failure with reduced ejection fraction in the EVEREST trial. Eur J Heart Fail 2013;15:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Manzano L, Babalis D, Roughton M, et al. Predictors of clinical outcomes in elderly patients with heart failure. Eur J Heart Fail 2011;13:528–536. [DOI] [PubMed] [Google Scholar]
- 29. Velazquez EJ, Lee KL, Deja MA, et al. Coronary‐artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med 2011;364:1607–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Smilde TD, Hillege HL, Navis G, Boomsma F, de ZD, van Veldhuisen DJ. Impaired renal function in patients with ischemic and nonischemic chronic heart failure: Association with neurohormonal activation and survival. Am Heart J 2004;148:165–172. [DOI] [PubMed] [Google Scholar]
- 31. Patterson ME, Grant WC, Glickman SW, et al. Resource use and costs of treatment with anticoagulation and antiplatelet agents: Results of the WATCH trial economic evaluation. J Card Fail 2009;15:819–827. [DOI] [PubMed] [Google Scholar]
- 32. McMurray JJ, Andersson FL, Stewart S, et al. Resource utilization and costs in the Candesartan in Heart failure: assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J 2006;27:1447–1458. [DOI] [PubMed] [Google Scholar]
- 33. Colombo GL, Caruggi M, Ottolini C, Maggioni AP. Candesartan in heart failure: Assessment of reduction in mortality and morbidity (CHARM) and resource utilization and costs in Italy. Vasc Health Risk Manag 2008;4:223–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Austin J, Williams WR, Hutchison S. Multidisciplinary management of elderly patients with chronic heart failure: Five year outcome measures in death and survivor groups. Eur J Cardiovasc Nurs 2009;8:34–39. [DOI] [PubMed] [Google Scholar]
- 35. Iqbal J, Francis L, Reid J, Murray S, Denvir M. Quality of life in patients with chronic heart failure and their carers: A 3‐year follow‐up study assessing hospitalization and mortality. Eur J Heart Fail 2010;12:1002–1008. [DOI] [PubMed] [Google Scholar]
- 36. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62:e147–e239. [DOI] [PubMed] [Google Scholar]
- 37. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2012;126:e354–e471. [DOI] [PubMed] [Google Scholar]
- 38. Krum H, Meehan A, Varigos J, Loane PR, Billah B. Does the presence of heart failure alter prescribing of drug therapy after myocardial infarction? A multicentre study. Med J Aust. 2006;185:191–194. [DOI] [PubMed] [Google Scholar]
- 39. Ezekowitz J, McAlister FA, Humphries KH, Norris CM, Tonelli M, Ghali WA, Knudtson ML. The association among renal insufficiency, pharmacotherapy, and outcomes in 6427 patients with heart failure and coronary artery disease. J Am Coll Cardiol 2004;44:1587–1592. [DOI] [PubMed] [Google Scholar]
- 40. Newby LK, LaPointe NM, Chen AY, et al. Long‐term adherence to evidence‐based secondary prevention therapies in coronary artery disease. Circulation 2006;113:203–212. [DOI] [PubMed] [Google Scholar]
- 41. Cokkinos DV, Haralabopoulos GC, Kostis JB, Toutouzas PK. Efficacy of antithrombotic therapy in chronic heart failure: The HELAS study. Eur J Heart Fail 2006;8:428–432. [DOI] [PubMed] [Google Scholar]
- 42. Homma S, Thompson JL, Pullicino PM, et al. Warfarin and aspirin in patients with heart failure and sinus rhythm. N Engl J Med 2012;366:1859–1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Massie BM, Collins JF, Ammon SE, et al. Randomized trial of warfarin, aspirin, and clopidogrel in patients with chronic heart failure: The Warfarin and Antiplatelet Therapy in Chronic Heart Failure (WATCH) trial. Circulation 2009;119:1616–1624. [DOI] [PubMed] [Google Scholar]
- 44. Mega JL, Braunwald E, Wiviott SD, et al. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med 2012;366:9–19. [DOI] [PubMed] [Google Scholar]


