Globally, nearly half of all under‐five deaths annually (3 million deaths) are attributable to undernutrition, as malnutrition is associated with increased risk of morbidity and infections, which leads to mortality (Liu et al. 2015). In 2011, at least 165 million children worldwide were stunted, and 52 million were wasted, with higher prevalence in south Asia and sub‐Saharan Africa. Malnutrition is not confined to children but is also rampant among women of reproductive age. This maternal malnutrition contributes to fetal growth restriction, which leads to low birthweight and increases risk of childhood infections and mortality. Children exposed to these risks early in life have a higher risk of growth faltering and stunting, which can cause long‐term irreversible and detrimental cognitive, motor and health impairments (Black et al. 2013). Most of the irreversible damage due to malnutrition occurs during gestation and in the first 24 months of life, hence underscores the importance of intervening in this period.
Malnutrition is widespread in Pakistan among all ages, and the progress has not been encouraging over the last decade. One‐third of children in Pakistan are underweight, 44% are stunted, 15% are wasted, half of them are anemic, and almost one‐third of the children have iron deficiency anemia (Table 1) (Government of Pakistan 2011). There is prominent inequity between the nutritional indicators of urban and rural populations, and children from the poorest wealth quintile are faring the worst. Among women, 14% of women of reproductive age are thin or undernourished (BMI less than 18.5 kg/m2), and this prevalence is highest among the poorest, uneducated and rural‐dwelling women. Micronutrient deficiencies are also prevalent among women with half of the women anaemic and high rates of vitamin A, zinc and iron deficiencies (Government of Pakistan 2011). Figure 1 shows that stunting prevalence varies greatly within Pakistan's districts, ranging between 22% and 76%. The lowest figures for wasting and underweight were both less than 2.5% and the highest were 42% for wasting and 54% for underweight (Di Cesare et al. 2015).
Table 1.
Malnutrition status of children in Pakistan
| Characteristics | Stunted (%) | Normal | ||
|---|---|---|---|---|
| Severe | Moderate | Mild | ||
| Age | ||||
| 0‐23 months | 18.3 | 18.3 | 23.3 | 40 |
| 24‐59 months | 24.9 | 24.1 | 23.6 | 27.4 |
| Characteristics | Wasted (%) | Normal | ||
| Severe | Moderate | Mild | ||
| Age | ||||
| 0‐23 months | 8.8 | 11.7 | 20.8 | 58.7 |
| 24‐59 months | 5.2 | 8.2 | 21.6 | 65.1 |
| Characteristics | Underweight (%) | Normal | ||
| Severe | Moderate | Mild | ||
| Age | ||||
| 0‐23 months | 13.1 | 18.6 | 27.6 | 40.7 |
| 24‐59 months | 11.4 | 19.4 | 28.8 | 40.4 |
Figure 1.
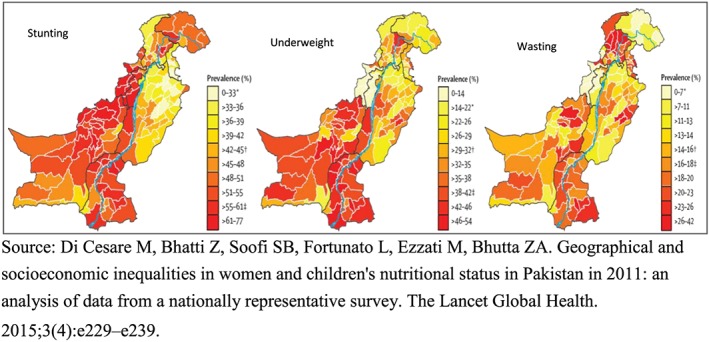
District comparisons of undernutrition in Pakistan.
Current recommendations for improved infant and young child nutrition (IYCN) include initiation of breastfeeding within 1 h of birth, exclusive breastfeeding of infants until 6 months of age, introduction of safe and nutritionally rich foods in addition to breastfeeding at about 6 months of age and continued breastfeeding with complementary feeding until 2 years of age or older. All IYCN indicators in Pakistan are ‘undesirably low’ even when compared with other countries in the South Asian region. Pakistan is conspicuous for having the lowest rates for early initiation of breastfeeding, exclusive breastfeeding rates and timely initiati on of complementary feeding (Table 2); and the highest rate in the region for bottle feeding. Latest data suggest that immediate breastfeeding is initiated in 18% of all births, whereas exclusive breastfeeding is carried out in only 38% of infants younger than 6 months in 2011. In Pakistan, 20% of children aged 2 months and 46% aged 9 to 11 months were reported using bottles with nipples and 19% of children aged 4–5 months were being fed solid to semi‐solid food. In addition, complementary feeding practices are far from optimal as 15% of the children meet the minimum acceptable diet and 22% observe minimum dietary diversity (Government of Pakistan 2011; Pakistan Demographic and Health Survey 2013).
Table 2.
Breastfeeding and complementary feeding rates in Pakistan
| NNS 2011 | DHS 2013 | |||
|---|---|---|---|---|
| N | % | N | % | |
| Exclusive under 6 months | 2174 | 13 | 1164 | 37.7 |
| Continued breastfeeding 12‐15 months | 1616 | 77.3 | 864 | 80.6 |
| Continued breastfeeding at 2 years | 753 | 54.3 | 837 | 56 |
| Age‐appropriate breastfeeding children (0‐23 months) | 9083 | 63.6 | 4262 | 56 |
| Introduction of semi‐solid (6‐8 months) | 1591 | 51.3 | 466 | 66 |
| Minimum dietary diversity (6‐23 months) | 6909 | 3 | 2855 | 22.2 |
| Minimum meal frequency (6‐23 months) | 6909 | 56.4 | 2855 | 62.7 |
| Minimum acceptable diet (6‐23 months) | 6909 | 7.3 | 2855 | 14.8 |
Underlying determinants and interventions
Several factors account for these failures in improving child‐feeding practices and hence nutrition. There is a general lack of awareness among the population regarding optimal feeding practices and other social taboos and misconceptions (such as the concept of ‘hot and cold foods’ or inappropriateness of foods for children) that further affect practices. The promotion and marketing of infant formulas is a recognized barrier for exclusive and predominant breastfeeding practices. To improve child nutrition and reduce stunting, it is imperative to focus on other parallel factors including improving maternal nutrition and antenatal care and especially nutrition of adolescent girls and young mothers. Low literacy rates among women, their lack of empowerment and involvement in decision‐making, early marriages, high fertility rates with lack of birth spacing, and poor access to health care facilities are all important determinants of child and maternal malnutrition. To this must be added measures to prevent common childhood illnesses such as diarrhea and acute respiratory infections and improve access to timely and quality care. Other factors affecting nutrition include poverty, food insecurity, unsafe water, poor sanitation and environmental hygiene. Recent data in Pakistan suggest that about 58 million people (36%) either defecate in the open or have access to shared toilets, in rural areas, 45% of the population still practice open defecation. Around 50% of the population has access to piped water, while other measures indicate that the majority of households (90%) do not treat their drinking water, and only 8% of households use an appropriate water treatment method (Government of Pakistan 2011).
In addition to the lack of progress, there are also widespread disparities in health care accessibility and quality that need to be bridged. Bringing the health services closer to women and children would make the difference. Pakistan has an extensive existing lady health workers programme, which with improvements can pave the way to reduce these inequalities. Social safety nets are another recognized medium, which can be implemented. There is a need to ensure regular data on nutrition indicators with more discrete regional‐level or district‐level data. There is need for integrating various different sectors and programmes to achieve the desired results effectively and efficiently as many of the determinants and influencing factors are outside the health sector. A behavioral change communication activity should be designed and implemented at national level to impart the IYCN messages, and these messages (behavioral change communication) should be tailored to the local needs and should be very specific and clear, and it should be given at the same level so that mother should associate with it. Promotion of practices that promote healthy lifestyle, food availabi‐lity, diversity, access, proper storage, preparation and utilization among economically disadvantaged segment of population should be ensured. Religious leaders in Pakistan can play a vital role in this advocacy as the Holy Quran has advised breastfeeding for 2 years, this must be used as a motivating agent in all advocacy campaigns, and religious leaders must be given detailed trainings on the code. The skills of health care providers should be enhanced to ensure optimum nutrition during pregnancy and early infancy and this should include lactation support.
The way forward
Improving maternal and child nutrition and reducing stunting require concerted efforts across a broad range of measures, legislation and policies, which can be universally implemented. There has been a singular lack of emphasis on nutrition promotion in the public sector primary health care initiatives. A set of measures that can impact stunting in Pakistan must include multisectoral initiatives. All the provinces in Pakistan have recognized that improving nutritional status of the population would require a multipronged approach with both nutrition‐sensitive and nutrition‐specific approaches. Although these ‘multisectoral nutrition strategies’ have been approved, implementation remains variable. There is clear need for implementation plans and commensurate political will and leadership to bring about change at the grassroots. This would need a nutrition lens for defining, implementing and measuring nutrition‐sensitive interventions, especially in sectors including agriculture, water and sanitation, education, poverty alleviation and social protection. Some of these measures include
Attention to developing and deploying human resources for nutrition at district level. A critical mass of people is required at all levels from policymakers, implementers, supervisors, health care professionals and community workers. These workers should have expertise and training in nutrition and work full time on nutrition activities in both nutrition sensitive and specific sectors.
Improving nutrition will require food safety and social protection. Pakistan has cash transfer programmes and Bait‐ul‐Maal funds, and these transfers can be conditionally linked to health and nutrition services, with upward revision in cash transfer amounts to adjust for food inflation and linkage of beneficiaries with livestock and agriculture schemes.
There are significant nutritional needs for women of reproductive age in Pakistan, and some of the associations with maternal height reflect intergenerational problems, and others reflect more acute exposures during pregnancy. Addressing fetal growth retardation and small for gestational age births, estimated to account for over a quarter of all births, may also reduce the burden of stunting in young infants and improve developmental outcomes. Targeting women nutrition way before pregnancy and during adolescence and preconception care provides a window of opportunity, which can bear enduring results for generations to come.
Pakistan must do better to improve rates of exclusive breastfeeding. This requires mass education and stringent implementation of the ‘International Code of Marketing of Breast‐milk Substitutes’. Additionally, support structures for working mothers to continue breastfeeding must be provided including paid maternity leave beyond the current limitations, availability of child care centers and designated area for breastfeeding at work place as well as support for women working in the non‐formal sectors.
Beyond breastfeeding, Pakistan has never had a concerted programme to improve complementary feeding, which is a major determinant of linear growth deviation after 6 months of age. The current focus and guidelines on complementary feeding are particularly poor. Interventions are needed to optimize the timing of introduction of complementary foods, with appropriate low‐cost fortified foods or in food secure households, appropriate home available diets. In high‐risk food insecure households, consideration should be given to the provision of low‐cost commodities for complementary feeding.
Amidst the water scarcity crisis in Pakistan, public‐sector investments are essential in providing secure and safe water to the population. Similarly, a massive national campaign must be launched to improve environmental and living conditions, promote the use of toilets and reduce the risks of fecal contamination.
The situation in Pakistan is ripe for change with a greater current emphasis on nutrition and formulation of various national and provincial nutrition focused strategies; policy makers and planners need to recognize the importance of improved child health and nutrition for national development and look at nutrition strategies as a net investment in the nation's future.
Conflict of interest
The authors declare that they have no conflicts of interest.
Contributions
All authors contributed to the writing.
Das, J. K. , Achakzai, A. B. K. , and Bhutta, Z. A. (2016) Stop stunting: Pakistan perspective on how this could be realized. Maternal & Child Nutrition, 12: 253–256. doi: 10.1111/mcn.12285.
This perspective paper was commissioned by the guest editors of this special supplement of Maternal and Child Nutrition to bring country‐specific perspectives to the issue of stunting in South Asia. It has not been peer reviewed. The views in this paper are the authors' views and do not necessarily reflect the views or policies of their organizations
References
- Black R.E., Victora C.G., Walker S.P., Bhutta Z.A., Christian P., de Onis M., et al. (2013) Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet 382 (9890), 427–51. [DOI] [PubMed] [Google Scholar]
- Di Cesare M., Bhatti Z., Soofi S.B., Fortunato L., Ezzati M. & Bhutta Z.A. (2015) Geographical and socioeconomic inequalities in women and children's nutritional status in Pakistan in 2011: an analysis of data from a nationally representative survey. The Lancet Global Health 3 (4), e229–e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Pakistan (2011) National Nutrition Survey. Planning Commission, Planning and Development Division. [Google Scholar]
- Liu L., Oza S., Hogan D., Perin J., Rudan I., Lawn J.E. et al. (2015) Global, regional, and national causes of child mortality in 2000–13, with projections to inform post–2015 priorities: an updated systematic analysis. Lancet 385 (9966): 430–440. [DOI] [PubMed] [Google Scholar]
- Pakistan Demographic and Health Survey . 2013. National Institute of Population Studies; 2012‐13.


