Abstract
Technical innovations in peritoneal dialysis (PD), now used widely for the long-term treatment of ESRD, have significantly reduced therapy-related complications, allowing patients to be maintained on PD for longer periods. Indeed, the survival rate for patients treated with PD is now equivalent to that with in-center hemodialysis. In parallel, changes in public policy have spurred an unprecedented expansion in the use of PD in many parts of the world. Meanwhile, our improved understanding of the molecular mechanisms involved in solute and water transport across the peritoneum and of the pathobiology of structural and functional changes in the peritoneum with long-term PD has provided new targets for improving efficiency and for intervention. As with hemodialysis, almost half of all deaths on PD occur because of cardiovascular events, and there is great interest in identifying modality-specific factors contributing to these events. Notably, tremendous progress has been made in developing interventions that substantially reduce the risk of PD-related peritonitis. Yet the gains have been unequal among individual centers, primarily because of unequal clinical application of knowledge gained from research. The work to date has further highlighted the areas in need of innovation as we continue to strive to improve the health and outcomes of patients treated with PD.
Keywords: peritoneal membrane, peritoneal dialysis, end-stage renal disease, cardiovascular disease, Life-threatening dialysis complications
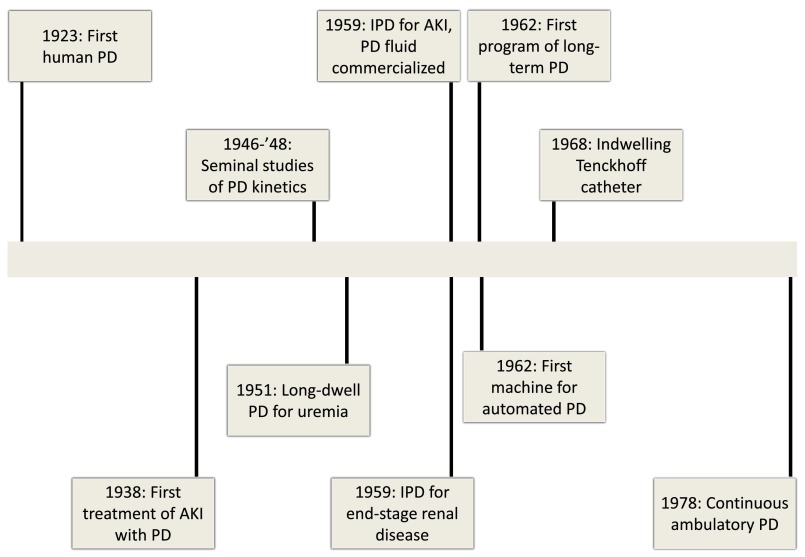
The first attempt to use the human peritoneum to dialyze uremic retention solutes was made almost 100 years ago.1 Over the next five decades, the therapy gradually evolved with an expansion in our understanding of solute and water kinetics that allowed for successful application of this mode of dialysis to AKI and ESRD.2–10 This, in addition to the development of the indwelling catheter that provided access to the peritoneal cavity at will and standardization of the composition of dextrose-based dialysate culminated in the introduction of continuous ambulatory peritoneal dialysis in 1976 (Figure 1).11–13 This was followed by changes in connectology to reduce the risk of infections, the introduction of volumetric cyclers, and several alternatives to conventional glucose-based peritoneal dialysis (PD) solutions.13–16 In this review, we highlight the major developments in the application of PD for the treatment of ESRD.
Figure 1.
Major landmarks in the development of PD as a treatment for ESRD (1923–1978).
Utilization and Outcomes with PD
The early experience with PD raised numerous concerns about whether the therapy was a viable alternative to in-center hemodialysis (HD) for the long-term treatment of ESRD. These included but were not limited to high risk of infections, inadequate clearance of small solutes, and deterioration of peritoneal health resulting in ultrafiltration failure, which together led to shorter time on therapy and higher risk for death compared with in-center HD.13,17–19 This led a leading nephrologist to retort in the 1980s that PD is a “second-class therapy for second-class patients by second-class doctors.” In part driven by these concerns, starting from the mid-1990s the proportion of patients with ESRD treated with PD progressively declined in many parts of the world.20,21
Yet, the greatest improvements in the clinical application of PD occurred at the same time as a progressively smaller proportion of patients were utilizing the therapy. In the decade starting from the mid-1990s, there was a significantly larger reduction in risk of death for patients starting with PD around the world than for those undergoing in-center HD (Table 1).22–29 As a result, virtually all studies indicate PD and in-center HD now provide similar short- (1- or 2-year) or long-term (up to 5 years) survival (Table 1).23–25,29–31 Furthermore, there has been a significant reduction in risk of patients treated with PD transferring to in-center HD in the United States, indicating a lower risk of therapy-related complications.32 These improvements have significant implications as they allow patients to receive treatment with an RRT best suited to their values, expectations, and lifestyles, and allow nations the flexibility to incentivize dialysis modalities that allow them to offer cost-effective treatment given increasing budgetary constraints.
Table 1.
Summary of studies from around the world demonstrating greater reductions in risk for death in patients treated with PD compared with in-center HD
| Author, Year | Country/Region | Periods | Mortality Trends by Modality | Trends in Comparative Survival |
|---|---|---|---|---|
| Mehrotra et al., 200722 | United States | 1996–1997 | Compared with 1998–1999, the adjusted hazards for patients starting PD to die or transfer to HD within 12 mo was 17% lower; no significant difference over time for patients starting HD | |
| 1998–1999 | ||||
| 2000–2001 | ||||
| 2002–2003 | ||||
| Mehrotra et al., 201123 | United States | 1996–1998 | The adjusted hazards ratio for death (PD, HD) were 1.07 (1.04, 1.11), 1.08 (1.06, 1.11), and 1.03 (0.99, 1.06), respectively | |
| 1999–2001 | ||||
| 2002–2004 | ||||
| Chang et al., 201224 | Taiwan | 1997–2001 | The adjusted hazards ratio for death (PD, HD) were 1.33 (1.21, 1.46), and 0.99 (0.87, 1.14), respectively | |
| 2002–2006 | ||||
| Yeates et al., 201225 | Canada | 1991–1995 | The adjusted hazards ratio for death (PD, HD) were 1.08 (1.02, 1.15), 1.13 (1.07, 1.20), and 0.99 (0.92, 1.06), respectively | |
| 1996–2000 | ||||
| 2001–2004 | ||||
| Heaf and Wehberg, 201426 | Denmark | 1990–1994 | Adjusted death risk for patients starting HD and PD in 2005–2010 was 30% (95% confidence interval, 13% to 37%) and 46% (95% confidence interval, 37% to 51%) lower compared with patients who started HD in 1990–1994 | The adjusted hazards ratio for death (PD, HD) were 0.95 (0.85, 1.06), 0.90 (0.82, 1.00), 0.84 (0.77, 0.92), and 0.80 (0.71, 0.89), respectively |
| 1995–1999 | ||||
| 2000–2004 | ||||
| 2005–2010 | ||||
| Marshall et al., 201527 | Australia and New Zealand | 1998–2002 | Compared with 1998–2002, adjusted death risk for patients starting HD in 2008–2012 was 21% lower (95% confidence interval, 15% to 26%); for patients starting PD, 27% lower (95% confidence interval, 11% to 23%) | |
| 2003–2007 | ||||
| 2008–2012 | ||||
| Ryu et al., 201528 | South Korea | Each year, from 2005 through 2008 | Compared with 2005, in 2008 adjusted death risk for patients starting HD was 15% lower (95% confidence interval, 9% to 20%) and starting PD 25% lower (95% confidence interval, 16% to 34%) | Among patients who started dialysis in 2008, no significant difference in risk for death for patients treated with HD, compared with those treated with PD (adjusted hazards ratio, 0.91 [0.82, 1.00]) |
| van de Luijtgaarden et al., 201529 | Europe (ERA-EDTA Registry) | 1993–1997 | Compared with 1993–1997, adjusted death risk for patients starting HD in 2003–2007 was 18% lower (95% confidence interval, 16% to 20%) and starting PD was 36% lower (95% confidence interval, 33% to 39%) | The adjusted hazards ratio for death (PD, HD) were 1.02 (0.98, 1.06), 1.00 (0.96, 1.03), and 0.91 (0.88, 0.95), respectively |
| 1998–2002 | ||||
| 2003–2007 |
ERA-EDTA, European Renal Association - European Dialysis and Transplant Association.
Public Policy Changes to Increase PD Utilization
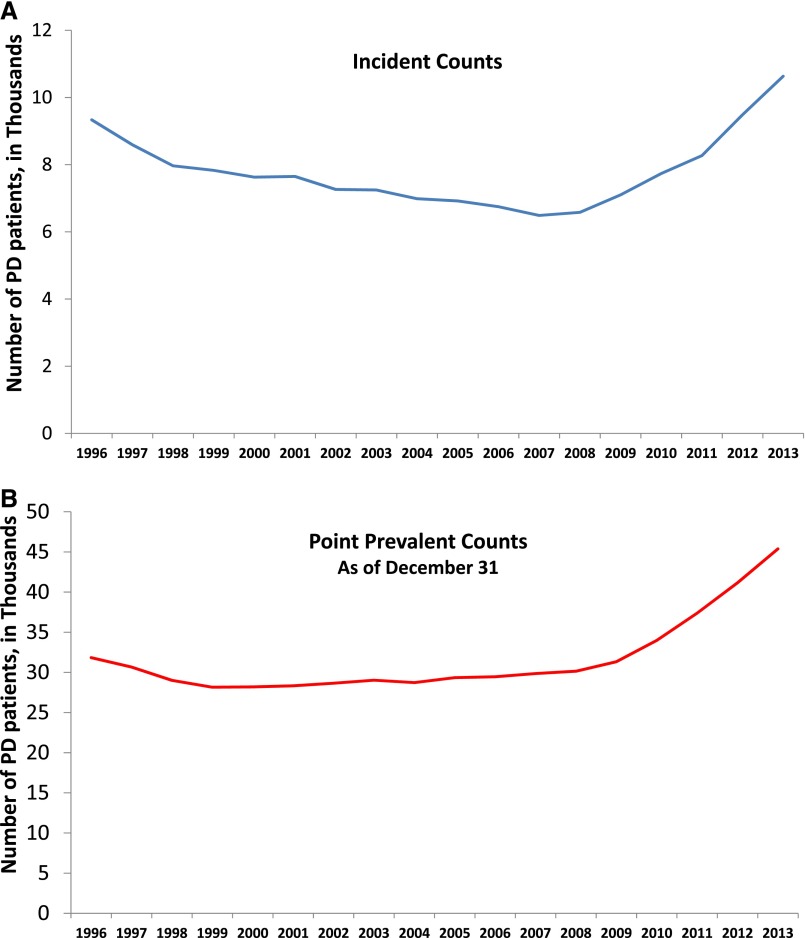
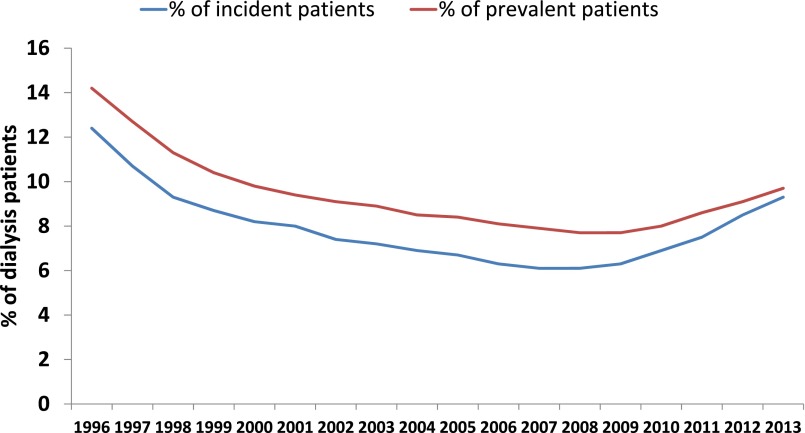
The relative costs of HD and PD vary around the world.33 In most developed countries and many developing countries societal costs with PD are lower providing impetus to these jurisdictions to enact public policy that promotes the use of a cheaper therapy.33 This is important as it has long been recognized that nonmedical factors, including reimbursement, are the primary determinants of the proportion of ESRD patients treated with PD in any region of the world.34,35 With a backdrop provided by recent studies that PD provides equivalent survival to in-center HD, several countries around the world have introduced changes to increase PD utilization to leverage its lower costs to the health system.36 In the United States, an expanded prospective payment system became effective in 2011, which includes the cost of parenteral dialysis-related medications in capitated payments made for each dialysis treatment.37,38 Because PD patients require a significantly lower dose of erythropoiesis stimulating agents to achieve any given hemoglobin level, this policy change offers a significant financial incentive to a greater use of PD.39 In Thailand, the government adopted a “PD-First” approach in 2008 as part of its universal health coverage scheme, as in Hong Kong, under the aegis of which dialysis services will be paid for only if the patient is treated with PD, given its lower cost.40 Finally, China has been rapidly expanding access to RRT for its population and has a policy that encourages the use of PD without mandating it.36 Each of these three countries has seen an unprecedented expansion in the use of PD. The growth in the United States has been so rapid (Figures 2, and 3) that the dominant manufacturer was not able to increase the supply of dialysate to meet the increasing demand leading to rationing of solutions in 2014.41 The shortage has abated but has not been completely eliminated. With increasing use of PD, it is likely that the patient census of individual facilities in such countries will become larger which in turn is associated with longer time for patients on PD because of reduced transfer to in-center HD.
Figure 2.
Secular trends in the number of patients treated with PD in the United States (1996–2013). (A) The number of patients treated with PD by 90 day of start of maintenance dialysis; (B) Point prevalent counts of the number of patients treated with PD as of December 31 of each calendar year.
Figure 3.
Secular trends in the proportion of patients undergoing maintenance dialysis treated with PD in the United States (1996–2013). The blue line represents the proportion of all patients undergoing maintenance dialysis treated with PD 90 days from the date of first dialysis and the red line represents the proportion of all patients undergoing maintenance dialysis on December 31 of any calendar year.
Rethinking Care Delivery to Increase Dialysis Treatment Options for Patients
An important barrier to a greater use of PD is that many patients with ESRD are unaware that dialysis can be done at home.42,43 Conversely, educating patients about treatment options is associated with a significantly higher use of PD even among patients who start dialysis without prior care with a nephrologist.44–46 Even when practices make comprehensive modality education programs available, many patients start RRT with little or no prior care by a nephrologist. These late-referred patients invariably start treatment with in-center HD with a central venous catheter.47,48 Even though “urgent-start” PD has been performed for decades, a growing number of centers around the world have now developed these programs both to increase the use of PD and reduce the proportion of patients that start dialysis with a central venous catheter.49–57 Successful implementation of urgent-start PD requires the ability to (1) educate late-referred patients on short notice about treatment options; (2) place PD catheters in a timely manner; and (3) offer intermittent PD in a hospital or dialysis facility up until the patient can be trained to perform treatments safely at home.58 A large number of case-series have reported successful implementation of urgent-start PD without an increase in incidence of leaks or other therapy-related mechanical complications.49–57
The elderly or the disabled is another group of patients that have significantly lower use of PD, even though many such patients would prefer treatment at home.59 Many programs have long used family members to help patients with PD.60 Several countries have extended this concept to include a visiting nurse to help patients with PD at home.59,61–64 Some of these patients require assistance only for a short period of time.63 Observational studies suggest that patients undergoing assisted PD have similar rates of bacterial peritonitis as with self-care PD and similar patient-reported outcomes and hospitalization as with in-center HD.61,64,65
Finally, racial/ethnic minorities in the United States have a significantly lower use of home-based dialysis therapies.66 It is imperative to further study this to ensure all patients have equal access to all dialysis modalities without regard to their race/ethnicity.
Improved Understanding of Peritoneal Physiology and Pathophysiology
The primary goal of dialysis is to remove water and uremic solutes, and the effectiveness of their removal is an important determinant of outcomes of patients treated with PD.67,68 Recent studies have expanded our understanding of solute and water transport processes across the peritoneum some of which could be leveraged for increasing the efficiency of PD.
Aquaporins in the Peritoneum
The water channel aquaporin-1 (AQP1) is constitutively expressed in endothelial cells lining peritoneal capillaries.69 It is a member of a highly conserved family of water channels that are organized as homotetramers, with each monomer containing a central pore that facilitates the movement of water across the lipidic membranes.70 The deletion of AQP1 in mice results in 50% decrease in net cumulative ultrafiltration, and abolition of sodium sieving.71,72 Indeed, glucose is effective as an osmotic agent because of the presence of the ultrasmall pore materialized by AQP1 in peritoneal endothelial cells.73 Investigators are currently examining AQP1 as a therapeutic target to increase ultrafiltration with PD. High-dose dexamethasone increases AQP1 expression in peritoneal capillaries of rodents resulting in enhanced free-water transport and ultrafiltration.74 Steroids may be efficacious in humans as illustrated by comparing ultrafiltration in patients before and after kidney transplantation.75 Another potential agent is an arylsulfonamide, AqF026, the first pharmacologic agonist of AQP1 that interacts with an intracellular loop involved in the gating of the channel.76 It enhances AQP1-mediated water transport and net ultrafiltration in rodents. These two examples give hope for the possibility of developing pharmacologic therapies targeting AQP1 to enhance ultrafiltration with PD.
Intraperitoneal Inflammation
There is increasing evidence that differences in chronic intraperitoneal inflammation, particularly IL-6 production by mesothelial and resident cells in the peritoneum, are primarily associated with differences in peritoneal solute transfer rate, which are in turn strongly associated with PD clinical outcomes.67,68,77–80 Consistent with this, genetic variants associated with higher IL-6 production are associated with higher peritoneal solute transfer rate.81,82
In addition to chronic inflammation, episodes of peritonitis are associated with acute increases in intraperitoneal inflammation resulting in higher peritoneal solute transfer rates and lower ultrafiltration.83 Studies in rodents suggest that locally released vasoactive substances, particularly nitric oxide, may mediate the increase in peritoneal solute transfer rate.84–86 Pharmacologic inhibition or genetic deletion of the endothelial nitric oxide synthase significantly attenuates intraperitoneal inflammation in animals with peritonitis and the associated change in peritoneal solute transfer rate and ultrafiltration.85
These findings point to potential therapeutic targets to be explored in the future to improve PD efficiency.
Structural and Functional Changes over Time
Prolonged treatment with PD is associated with structural (fibrosis, angiogenesis, hyalinizing vasculopathy) and functional (increased peritoneal solute transfer rate, ultrafiltration failure) changes.87 One of the most serious complications of long-term PD is encapsulating peritoneal sclerosis, a rare complication characterized by an exaggerated fibrogenic response of the peritoneum.88,89 Studies suggest that peritoneal ultrafiltration capacity decreases before the clinical manifestation of encapsulating peritoneal sclerosis and that the primary mechanism is reduction in osmotic conductance (ultrafiltration volume for a given osmotic gradient) that is related to the increased collagen fiber density in the interstitium.88,90,91
The mechanisms of peritoneal fibrosis remain debated. Progressive fibrosis is characterized by the release of growth factors such as TGF-β1, resulting in the accumulation of α-smooth muscle actin myofibroblasts in the peritoneum.87,92 Several in vitro and in vivo studies indicated that myofibroblasts are derived from mesothelial cells through epithelial-mesenchymal transition,93–96 in which epithelial cells lose their polarity and differentiation, gain migratory and invasive properties, and become pluripotent mesenchymal stem cells that differentiate into fibroblasts. Consistent with studies questioning the role of epithelial-mesenchymal transition in renal fibrosis,97–99 Chen et al.100 recently applied lineage-tracing technology in several models of peritoneal fibrosis and showed that submesothelial fibroblasts – and not mesothelial cells via epithelial-mesenchymal transition – are the major precursors of myofibroblasts.
These improvements in our understanding of the mechanisms involved in changes in the peritoneum with long-term PD hold hope that future therapies may allow us to ameliorate them. As an example, post hoc analysis of a recent randomized controlled trial suggests that patients treated with biocompatible PD solutions may not have the increase in peritoneal solute transfer rate after the first month of therapy, as seen with conventional PD solutions.101,102 Observational studies have also raised the possibility that inhibitors of the renin-angiotensin-aldosterone system may ameliorate change in peritoneal solute transfer capacity over time103; the beneficial effect of these drug classes, however, has not been tested in clinical trials.
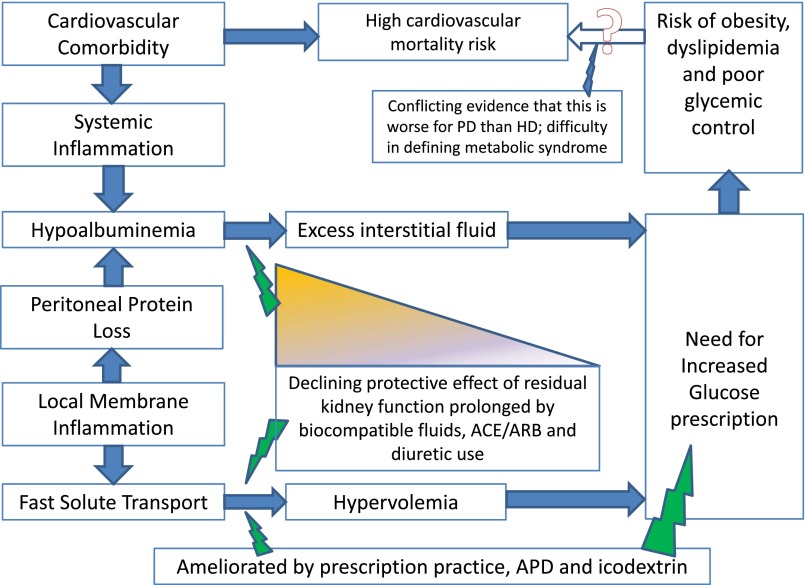
Cardiovascular Risk Modification in PD Patients
About 40%–60% of deaths in PD patients are associated with cardiovascular events104; even more can be considered indirectly related if the link between cardiovascular disease, inflammation and frailty leading to debilitation, transfer to HD, and treatment withdrawal are considered.79,105–107 Registry analyses suggest that PD patients may have a higher risk of myocardial infarction compared with HD.104,108 This section is focused on nonconventional cardiovascular risk factors, with emphasis on modification by treatment with PD (Figure 4). A more comprehensive evaluation of evidence of cardiovascular risk factors is included in recently published clinical practice guidelines.109,110
Figure 4.
Overview of interrelationships between modality-specific factors that may contribute to the cardiovascular risk of patients undergoing PD.
Importance of Metabolic Risk Factors and the Role of Glucose-Sparing Regimens
The most obvious risk factors exacerbated by PD are metabolic, related to systemic glucose absorption from the dialysate. They include worsening dyslipidemia, insulin resistance and metabolic syndrome, and weight gain.111–117 Yet, the evidence that they translate into significantly worse outcomes for PD patients is variable. For example, the greater weight gain with PD compared with HD is unclear. Patients gain weight after starting PD, and this is closely mirrored by an increase in total cholesterol and fat mass. However, in many circumstances this weight gain reflects catch-up of the predialysis loss.111,118 This also happens with HD and a large study found that the risk of significant weight gain is lower with PD.118 For patients undergoing maintenance dialysis, the greater nutritional risk is being underweight and in this context additional calories from the dialysate could be advantageous119,120; what is less clear is whether the lower death risk with larger body size consistently observed among patients undergoing HD is seen with PD.121 This may be influenced by other regional factors as the risk or benefit of being obese in PD varies between national registries, being harmful in Australasia and neutral or advantageous in the United States and Brazil.118,122–124
One potential shortcoming of the registry analyses is the use of body mass index as surrogate for obesity which may underestimate fat gain in PD patients; the preferred use of waist circumference in defining metabolic syndrome is also hard to validate in PD patients in whom abdominal girth measurements are influenced by intra-abdominal fluid. Equally, measuring insulin resistance in a patient who is never fasting because of continuous glucose absorption presents problems. This may explain the inconsistencies between studies linking metabolic syndrome in PD to worse outcomes.114,125,126 Again the role of treatment modality varies, as new-onset diabetes is less common in Chinese patients treated with PD than HD, and in either dialysis modality much less than for newly transplanted patients.127,128 What at first sight may be an obvious modality-specific risk factor for cardiovascular disease, i.e., systemic glucose absorption, turns out to be much less clear.
Regardless of these inconsistencies, there are now several studies showing that these risk factors are modifiable, although none of the trials are sufficiently powered to address hard endpoints. Glucose sparing solutions have been developed, such as amino acid and icodextrin. In nonpatients with diabetes, the colloid agent icodextrin used in the long exchange prevents nonfluid (presumed fat) weight gain and improves insulin resistance.129–131 In patients with diabetes, including when in combination with amino acid solutions, icodextrin improves glycemic control and lipid profiles.132–134 Poor glycemic control is associated with worse outcomes in diabetic PD patients.135,136
Given the concern of increased risk of myocardial infarction in patients receiving PD the lack of evidence that statins can reduce this is disappointing.137 Interestingly, a prespecified subgroup analysis of the Study of Heart and Renal Protection study, the only trial to include PD patients, found a nonsignificant but potentially important risk reduction suggesting that these patients may be different and worthy of further investigation.138
Residual Kidney Function
Residual kidney function is strongly associated with better survival in studies of both PD and HD.139,140 In the Canada-USA study every 250 ml higher urine volume per day translated into a 36% lower 2-year mortality.139 Evidence suggests that PD is associated with better preservation of residual kidney function compared with HD, typical reported rates of loss in clearance per month being 0.25–0.28 and 0.30–0.40 ml/min per 1.73 m2, respectively141–146; the mechanism is still debated but is likely to be in part the avoidance of intravascular volume depletion which occurs more frequently with HD.147 Cohort studies and controlled trials find that in patients undergoing PD the rate of loss of kidney function could be slowed with avoidance of volume depletion, use of blockers of renin-angiotensin-aldosterone system, and the use of diuretics (urine volume and sodium loss).145,146,148,149
The most studied intervention to maintain residual kidney function is the use of biocompatible solutions. Biocompatible solutions avoid the need for sterilizing glucose at higher pH so limiting the formation of glucose degradation products and thus avoiding their associated toxicity. The Balance, Australia and New Zealand study demonstrated that these solutions delay the time to anuria, and slow the rate of loss of clearance from 0.28 to 0.22 ml/min per 1.73 m2 per month.150 Subsequent meta-analyses have confirmed this observation.143,151
Volume Management
As already alluded to, volume depletion puts residual kidney function at risk but equally volume excess is detrimental. Hypertension in patients healthy enough to be wait-listed for transplant is associated with worse survival and there is a growing body of evidence from bioimpedance data that over-hydration predicts worse survival.152,153 In anuric patients the ultrafiltration performance of the peritoneum becomes critical and daily net fluid removal of <750–1000 ml is associated with higher mortality.154,155 There is evidence that automated PD and icodextrin use can improve the risks associated with fast peritoneal solute transfer rate.68,156,157
The fluid status of PD patients is no worse on average than for HD patients predialysis, but that the distribution of fluid is likely different.147 Hypoalbuminaemia is more common with PD due to the additional peritoneal protein losses and is a reflection of their largely independent systemic and intraperitoneal inflammatory states.79,158 Intravascular plasma volume is typically normal in PD, even when excess fluid associated with hypoalbuminemia is present, indicating it being in the interstitial compartment.159 This means that normalizing fluid status runs the risk of plasma volume depletion, hypotension, and faster loss of residual kidney function. A recent trial using bioimpedance to support clinical decision making found that fluid status was very stable in PD patients with residual kidney function whereas the challenge in anuric patients was how to reduce volume status so that extracellular fluid was reduced in parallel with the loss in lean body tissue.160 The only intervention that achieved this was an increase in glucose prescription. As things stand, clinicians need to exercise caution and clinical judgment in setting target weights.
Peritonitis
Peritonitis continues to be a major cause of morbidity and mortality in PD patients globally.104,161,162 Depending on the underlying causative organism, PD-related peritonitis is complicated by relapse in 3%–20% (14% overall), catheter removal in 10%–88% (22% overall), permanent HD transfer in 9%–74% (18% overall), and death in 0.9%–8.6% (2%–6% overall) of cases.163–174 After a single episode of peritonitis, the risks of death due to infection, cardiovascular disease, and dialysis withdrawal are markedly increased in the first month and continue to remain significantly elevated for up to 6 months afterward.106 Severe and/or repeated peritonitis episodes may also culminate in sufficient damage that precludes successful PD and, rarely, encapsulating peritoneal sclerosis.175,176 The complication imposes a heavy financial burden on the health care system with one health economics analysis estimating the average cost of peritonitis-related hospitalization to be of the order of $3100.177 Finally, concern about the risk of PD peritonitis represents one of the most important patient-related barriers to the greater uptake of PD.178
Nevertheless, peritonitis is a preventable condition and there is abundant evidence that infection rates around the world have decreased considerably over time.179 Single center observational studies from different parts of the world, as well as multinational national registry studies have reported that the rates of PD-related infections have steadily decreased over the last 10–20 years.161,180–185 Although this reduction has been most apparent for Gram-positive infections, significant reductions have also been reported for Gram-negative peritonitis.161,180–185 These reductions have been variously attributed to the use of twin bag disconnection systems, implementation of mupirocin chemoprophylaxis protocols, topical exit site application of gentamicin, coprescription of nystatin or fluconazole with antibiotic therapy, improved training of PD patients and/or staff, and better identification and targeting of peritonitis risk factors.180,186–193 Within Australia, country-wide PD-related peritonitis rates fell significantly by 37% over a 5-year period from 0.62 episodes per patient-year in 2008 to 0.39 episodes per patient-year in 2013 after a concerted, multidisciplinary and multipronged national peritonitis reduction campaign involving quarterly audit and feedback of individual unit peritonitis rates, prioritization of peritonitis prevention trials by the Australasian Kidney Trials Network, updating national clinical practice guidelines on peritonitis, launching peritonitis guideline implementation projects, publishing of a call to action paper, establishment of a PD Academy to provide PD training to junior nephrologists and nursing staff, and development of a Home Dialysis Network to support home dialysis patients (http://homedialysis.org.au/).194–199
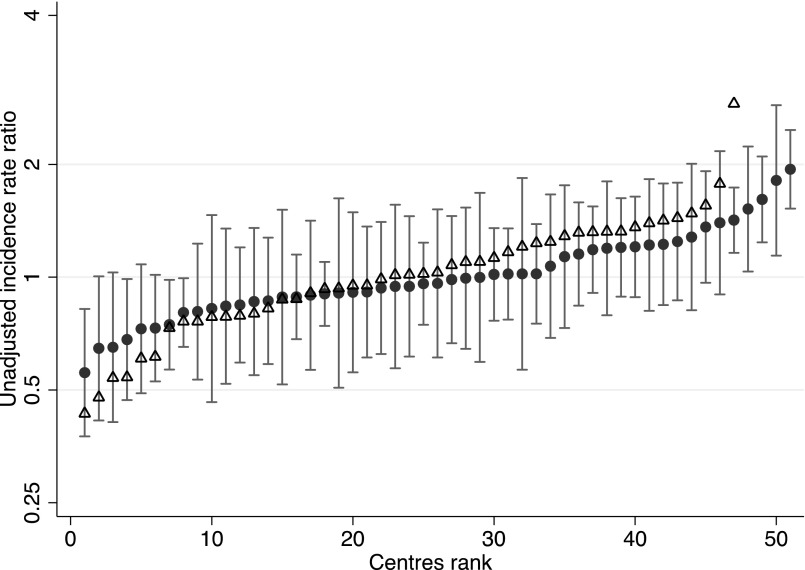
Despite these improvements, there remains a wide and unacceptable variation in reported rates from different countries, ranging from 0.06 episodes/year in Taiwan to 1.66 episodes/year in Israel.200 Furthermore, up to 20-fold variation in peritonitis rates has been reported between centers within individual countries, such as Australia (Figure 5),174,194 Austria,201 Scotland,202 and the United Kingdom.203 The sources of these variations have not been adequately investigated but may relate to center-related factors, such as unit size, topical antibiotic prophylaxis, or PD training practices.161,192,201,202,204,205 A previous national survey found highly variable and generally poor compliance of centers with clinical practice guidelines for prevention of peritonitis.206 More recently, an Australia and New Zealand Dialysis and Transplantation Registry analysis found that the wide variation in peritonitis rates across Australian dialysis centers was decreased by 16% after adjustment for patient characteristics (e.g., demographics, comorbidities), and was reduced by a further 34% after accounting for a limited number of center-level characteristics, such as unit size, proportion of dialysis patients treated with PD, use of antifungal chemoprophylaxis, icodextrin use, performance of peritoneal equilibration tests, cycler use, and propensity to admit patients with PD-related peritonitis to hospital.207 This observation suggests that center practices play a dominant role in mediating between-center variation in peritonitis rates. Similarly, unacceptable variations in the outcomes of peritonitis treatment have been significantly associated with observed deviations in practice from clinical practice guidelines.208
Figure 5.
Center-specific PD-related peritonitis rates (incidence rate ratios) in Australia during the periods 2004–2008 (open triangles) and 2009–2013 (solid circles).
The key message from these studies is that although peritonitis rates are generally improving globally over time, there have been marked and unacceptable variations in peritonitis rates and outcomes between centers in many countries. This variation is explained to a large extent by variation in center practices, with poorer results generally being observed in units that deviate from evidence-based best practice recommendations (and not infrequently from their own unit policies).195 Key strategies for correcting this ubiquitous problem in PD include benchmarking of PD center peritonitis rates and outcomes through the establishment of national PD peritonitis registries within each country, alignment of PD practice in each center with clinical practice guidelines, strengthening of clinical governance within each unit, and adoption of a whole-of-unit approach to continuous quality improvement, including root cause analysis of all cases of peritonitis within each center to identify areas for improvement.200,208
Future Directions
Despite tremendous progress on multiple fronts, patients with ESRD carry a heavy burden of disease and treatment. We owe to the patients to continue to reconfigure health care delivery to better match dialysis modality to patients’ desires, improve the efficiency of therapy without putting a greater burden on patients, reduce cardiovascular risk, and better apply lessons learnt from research in clinical practice (Table 2).
Table 2.
Important thematic areas in need of further research
| Thematic Areas | Details of Areas in Need of Further Research |
|---|---|
| Utilization and outcomes with PD | Approaches to modality education that optimize decision support and reduce decisional conflict |
| Clinical outcomes of late-referred patients starting treatment with PD (“urgent-start” PD) and in-center HD with central venous catheter | |
| Comparative effectiveness of home and in-center dialysis for end-of-life care for patients with ESRD | |
| Understanding reasons for the low utilization of PD by racial/ethnic minorities and tailored interventions to overcome barriers | |
| Adequately powered studies comparing a broad range of patient-reported outcomes with different dialysis modalities, including effect-modification by cultural differences | |
| Peritoneal physiology and pathobiology | Mechanisms of osmosis, choice of solutions, new osmotic agents, combination of different types of osmotic agents |
| Biomarkers of peritoneal solute and water transfer – at baseline and over time on PD: genetics, proteomics, metabolomics | |
| New indications for PD: intoxications (e.g., liposome-supported PD for intoxication and metabolic disorders) | |
| Reversibility of the structural changes in the peritoneal membrane: fibrosis, angiogenesis | |
| Cellular mechanisms of peritoneal fibrosis and EPS | |
| Identification of molecular counterparts of additional transport structures, e.g., the small pores | |
| Cardiovascular risk with PD | Validation of more practical approach to defining metabolic syndrome for PD patients |
| Better understanding of high risk cardiovascular risk phenotypes to include interactions with diabetes, gender, and ethnicity | |
| Adequately powered study to test the benefit of statins | |
| Trials to evaluate additional strategies for preserving residual kidney function | |
| Trials addressing the risk/benefit of preserving residual kidney function while optimizing volume status and BP management, including further evaluation of technologies to evaluate fluid status at the bedside | |
| Peritonitis | Determining which PD training methods, curricula, and structured assessment methods lead to better peritonitis rates |
| Determining whether structured periodic retraining after initial baseline training leads to a reduction in peritonitis rates | |
| Development and evaluation of rapid (within hours) organism identification methods in PD-related peritonitis | |
| Does use of continuous versus intermittent intraperitoneal antibiotics for peritonitis treatment lead to better peritonitis outcomes? | |
| Does temporary conversion of automated PD patients to CAPD during peritonitis treatment lead to better outcomes compared with leaving patients on automated PD? |
EPS, encapsulating peritoneal sclerosis; CAPD, continuous ambulatory peritoneal diaylsis.
Disclosures
S.J.D. has received research funding and speakers’ honoraria, and has participated in occasional advisory boards for Baxter Healthcare and Fresenius Medical Care. D.W.J. has previously received consultancy fees, research funds, speakers’ honoraria and travel sponsorships from Baxter Healthcare and Fresenius Medical Care.
Acknowledgments
Studies mentioned in this review were supported in part by the National Institutes of Health (R01DK99165), Fondation Saint-Luc at Universtie Catholique de Louvain, Baxter Extramural Grants, and the Fonds National de la Recherche Scientifique.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Ganter G: Uber die Beseitigung giftiger Stoffe aus dem Blute durch Dialyse. Munch Med Wochenschr 70: 1478–1480, 1923 [Google Scholar]
- 2.Wear JB, Sisk IR, Trinkle AJ: Peritoneal lavage in the treatment of uremia: an experimental and clinical study. J Urol 39: 53–62, 1938 [Google Scholar]
- 3.Frank HA, Seligman AM, Fine J: Treatment of uremia after acute renal failure by peritoneal irrigation. J Am Med Assoc 130: 703–705, 1946 [DOI] [PubMed] [Google Scholar]
- 4.Seligman AM, Frank HA, Fine J: Treatment of Experimental Uremia by Means of Peritoneal Irrigation. J Clin Invest 25: 211–219, 1946 [PubMed] [Google Scholar]
- 5.Frank HA, Seligman AM, Fine J: Further experiences with peritoneal irrigation for acuter renal failure including a description of modifications in method. Ann Surg 128: 561–608, 1948 [PubMed] [Google Scholar]
- 6.Odel HM, Ferris DO, Power MH: Peritoneal lavage as an effective means of extrarenal excretion; a clinical appraisal. Am J Med 9: 63–77, 1950 [DOI] [PubMed] [Google Scholar]
- 7.Grollman A, Turner LB, McLEAN JA: Intermittent peritoneal lavage in nephrectomized dogs and its application to the human being. AMA Arch Intern Med 87: 379–390, 1951 [DOI] [PubMed] [Google Scholar]
- 8.Doolan PD, Murphy WP Jr, Wiggins RA, Carter NW, Cooper WC, Watten RH, Alpen EL: An evaluation of intermittent peritoneal lavage. Am J Med 26: 831–844, 1959 [DOI] [PubMed] [Google Scholar]
- 9.Maxwell MH, Rockney RE, Kleeman CR, Twiss MR: Peritoneal dialysis. 1. Technique and applications. J Am Med Assoc 170: 917–924, 1959 [DOI] [PubMed] [Google Scholar]
- 10.Boen ST, Mulinari AS, Dillard DH, Scribner BH: Periodic peritoneal dialysis in the management of chronic uremia. Trans Am Soc Artif Intern Organs 8: 256–262, 1962 [Google Scholar]
- 11.Tenckhoff H, Schechter H: A bacteriologically safe peritoneal access device. Trans Am Soc Artif Intern Organs 14: 181–187, 1968 [PubMed] [Google Scholar]
- 12.Popovich RP, Moncrief JW, Decherd JB, Bomar JB, Pyle WK: The definition of a novel portable/wearable equilibrium peritoneal dialysis technique. Trans Am Soc Artif Intern Organs 5: 484–489, 1976 [Google Scholar]
- 13.Oreopoulos DG, Robson M, Izatt S, Clayton S, deVeber GA: A simple and safe technique for continuous ambulatory peritoneal dialysis (CAPD). Trans Am Soc Artif Intern Organs 24: 484–489, 1978 [PubMed] [Google Scholar]
- 14.Maiorca R, Cantaluppi A, Cancarini GC, Scalamogna A, Broccoli R, Graziani G, Brasa S, Ponticelli C: Prospective controlled trial of a Y-connector and disinfectant to prevent peritonitis in continuous ambulatory peritoneal dialysis. Lancet 2: 642–644, 1983 [DOI] [PubMed] [Google Scholar]
- 15.Buoncristiani U: Birth and evolution of the “Y” set. ASAIO J 42: 8–11, 1996 [PubMed] [Google Scholar]
- 16.Diaz-Buxo JA, Farmer CD, Walker PJ, Chandler JT, Holt KL: Continuous cyclic peritoneal dialysis: a preliminary report. Artif Organs 5: 157–161, 1981 [DOI] [PubMed] [Google Scholar]
- 17.Ahmad S, Gallagher N, Shen F: Intermittent peritoneal dialysis: status reassessed. Trans Am Soc Artif Intern Organs 25: 86–89, 1979 [PubMed] [Google Scholar]
- 18.Heimbürger O, Waniewski J, Werynski A, Tranaeus A, Lindholm B: Peritoneal transport in CAPD patients with permanent loss of ultrafiltration capacity. Kidney Int 38: 495–506, 1990 [DOI] [PubMed] [Google Scholar]
- 19.Bloembergen WE, Port FK, Mauger EA, Wolfe RA: A comparison of mortality between patients treated with hemodialysis and peritoneal dialysis. J Am Soc Nephrol 6: 177–183, 1995 [DOI] [PubMed] [Google Scholar]
- 20.Mehrotra R: Peritoneal dialysis penetration in the United States: march toward the fringes? Perit Dial Int 26: 419–422, 2006 [PubMed] [Google Scholar]
- 21.Jain AK, Blake P, Cordy P, Garg AX: Global trends in rates of peritoneal dialysis. J Am Soc Nephrol 23: 533–544, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehrotra R, Kermah D, Fried L, Kalantar-Zadeh K, Khawar O, Norris K, Nissenson A: Chronic peritoneal dialysis in the United States: declining utilization despite improving outcomes. J Am Soc Nephrol 18: 2781–2788, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Mehrotra R, Chiu YW, Kalantar-Zadeh K, Bargman J, Vonesh E: Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch Intern Med 171: 110–118, 2011 [DOI] [PubMed] [Google Scholar]
- 24.Chang YK, Hsu CC, Hwang SJ, Chen PC, Huang CC, Li TC, Sung FC: A comparative assessment of survival between propensity score-matched patients with peritoneal dialysis and hemodialysis in Taiwan. Medicine (Baltimore) 91: 144–151, 2012 [DOI] [PubMed] [Google Scholar]
- 25.Yeates K, Zhu N, Vonesh E, Trpeski L, Blake P, Fenton S: Hemodialysis and peritoneal dialysis are associated with similar outcomes for end-stage renal disease treatment in Canada. Nephrol Dial Transplant 27: 3568–3575, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Heaf JG, Wehberg S: Relative survival of peritoneal dialysis and haemodialysis patients: effect of cohort and mode of dialysis initiation. PLoS One 9: e90119, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marshall MR, Polkinghorne KR, Kerr PG, Agar JW, Hawley CM, McDonald SP: Temporal Changes in Mortality Risk by Dialysis Modality in the Australian and New Zealand Dialysis Population. Am J Kidney Dis 66: 489–498, 2015 [DOI] [PubMed] [Google Scholar]
- 28.Ryu JH, Kim H, Kim KH, Hann HJ, Ahn HS, Lee S, Kim SJ, Kang DH, Choi KB, Ryu DR: Improving survival rate of Korean patients initiating dialysis. Yonsei Med J 56: 666–675, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van de Luijtgaarden MW, Jager KJ, Segelmark M, Pascual J, Collart F, Hemke AC, Remon C, Metcalfe W, Miguel A, Kramar R, Aasarod K, Abu Hanna A, Krediet RT, Schon S, Ravani P, Caskey FJ, Couchoud C, Palsson R, Wanner C, Finne P, Noordzij M: Trends in dialysis modality choice and related patient survival in the ERA-EDTA Registry over a 20-year period. Nephrol Dial Transplant 31: 120–128, 2016 [DOI] [PubMed] [Google Scholar]
- 30.Quinn RR, Hux JE, Oliver MJ, Austin PC, Tonelli M, Laupacis A: Selection bias explains apparent differential mortality between dialysis modalities. J Am Soc Nephrol 22: 1534–1542, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weinhandl ED, Foley RN, Gilbertson DT, Arneson TJ, Snyder JJ, Collins AJ: Propensity-matched mortality comparison of incident hemodialysis and peritoneal dialysis patients. J Am Soc Nephrol 21: 499–506, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehrotra R, Chiu YW, Kalantar-Zadeh K, Vonesh E: The outcomes of continuous ambulatory and automated peritoneal dialysis are similar. Kidney Int 76: 97–107, 2009 [DOI] [PubMed] [Google Scholar]
- 33.Karopadi AN, Mason G, Rettore E, Ronco C: Cost of peritoneal dialysis and haemodialysis across the world. Nephrol Dial Transplant 28: 2553–2569, 2013 [DOI] [PubMed] [Google Scholar]
- 34.Nissenson AR, Prichard SS, Cheng IK, Gokal R, Kubota M, Maiorca R, Riella MC, Rottembourg J, Stewart JH: Non-medical factors that impact on ESRD modality selection. Kidney Int Suppl 40: S120–S127, 1993 [PubMed] [Google Scholar]
- 35.Lameire N, Van Biesen W: Epidemiology of peritoneal dialysis: a story of believers and nonbelievers. Nat Rev Nephrol 6: 75–82, 2010 [DOI] [PubMed] [Google Scholar]
- 36.Liu FX, Gao X, Inglese G, Chuengsaman P, Pecoits-Filho R, Yu A: A Global Overview of the Impact of Peritoneal Dialysis First or Favored Policies: An Opinion. Perit Dial Int 35: 406–420, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sedor JR, Watnick S, Patel UD, Cheung A, Harmon W, Himmelfarb J, Hostetter TH, Inrig JK, Mehrotra R, Robinson E, Smedberg PC, Shaffer RN; American Society of Nephrology ESRD Task Force : ASN End-Stage Renal Disease Task Force: perspective on prospective payments for renal dialysis facilities. J Am Soc Nephrol 21: 1235–1237, 2010 [DOI] [PubMed] [Google Scholar]
- 38.Watnick S, Weiner DE, Shaffer R, Inrig J, Moe S, Mehrotra R; Dialysis Advisory Group of the American Society of Nephrology : Comparing mandated health care reforms: the Affordable Care Act, accountable care organizations, and the Medicare ESRD program. Clin J Am Soc Nephrol 7: 1535–1543, 2012 [DOI] [PubMed] [Google Scholar]
- 39.Duong U, Kalantar-Zadeh K, Molnar MZ, Zaritsky JJ, Teitelbaum I, Kovesdy CP, Mehrotra R: Mortality associated with dose response of erythropoiesis-stimulating agents in hemodialysis versus peritoneal dialysis patients. Am J Nephrol 35: 198–208, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tantivess S, Werayingyong P, Chuengsaman P, Teerawattananon Y: Universal coverage of renal dialysis in Thailand: promise, progress, and prospects. BMJ 346: f462, 2013 [DOI] [PubMed] [Google Scholar]
- 41.Blake PG, Golper TA, Saxena AB: A critical shortage of solution threatens unprecedented growth in peritoneal dialysis. Nephrol News Issues 28: 14–16, 2014 [PubMed] [Google Scholar]
- 42.Mehrotra R, Marsh D, Vonesh E, Peters V, Nissenson A: Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int 68: 378–390, 2005 [DOI] [PubMed] [Google Scholar]
- 43.Kutner NG, Zhang R, Huang Y, Wasse H: Patient awareness and initiation of peritoneal dialysis. Arch Intern Med 171: 119–124, 2011 [DOI] [PubMed] [Google Scholar]
- 44.Manns BJ, Taub K, Vanderstraeten C, Jones H, Mills C, Visser M, McLaughlin K: The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: a randomized trial. Kidney Int 68: 1777–1783, 2005 [DOI] [PubMed] [Google Scholar]
- 45.Lacson E Jr, Wang W, DeVries C, Leste K, Hakim RM, Lazarus M, Pulliam J: Effects of a nationwide predialysis educational program on modality choice, vascular access, and patient outcomes. Am J Kidney Dis 58: 235–242, 2011 [DOI] [PubMed] [Google Scholar]
- 46.Rioux JP, Cheema H, Bargman JM, Watson D, Chan CT: Effect of an in-hospital chronic kidney disease education program among patients with unplanned urgent-start dialysis. Clin J Am Soc Nephrol 6: 799–804, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmidt RJ, Domico JR, Sorkin MI, Hobbs G: Early referral and its impact on emergent first dialyses, health care costs, and outcome. Am J Kidney Dis 32: 278–283, 1998 [DOI] [PubMed] [Google Scholar]
- 48.Lameire N, Van Biesen W: The pattern of referral of patients with end-stage renal disease to the nephrologist--a European survey. Nephrol Dial Transplant 14[Suppl 6]: 16–23, 1999 [DOI] [PubMed] [Google Scholar]
- 49.Song JH, Kim GA, Lee SW, Kim MJ: Clinical outcomes of immediate full-volume exchange one year after peritoneal catheter implantation for CAPD. Perit Dial Int 20: 194–199, 2000 [PubMed] [Google Scholar]
- 50.Banli O, Altun H, Oztemel A: Early start of CAPD with the Seldinger technique. Perit Dial Int 25: 556–559, 2005 [PubMed] [Google Scholar]
- 51.Povlsen JV, Ivarsen P: How to start the late referred ESRD patient urgently on chronic APD. Nephrol Dial Transplant 21[Suppl 2]: ii56–ii59, 2006 [DOI] [PubMed] [Google Scholar]
- 52.Jo YI, Shin SK, Lee JH, Song JO, Park JH: Immediate initiation of CAPD following percutaneous catheter placement without break-in procedure. Perit Dial Int 27: 179–183, 2007 [PubMed] [Google Scholar]
- 53.Lobbedez T, Lecouf A, Ficheux M, Henri P, Hurault de Ligny B, Ryckelynck JP: Is rapid initiation of peritoneal dialysis feasible in unplanned dialysis patients? A single-centre experience. Nephrol Dial Transplant 23: 3290–3294, 2008 [DOI] [PubMed] [Google Scholar]
- 54.Yang YF, Wang HJ, Yeh CC, Lin HH, Huang CC: Early initiation of continuous ambulatory peritoneal dialysis in patients undergoing surgical implantation of Tenckhoff catheters. Perit Dial Int 31: 551–557, 2011 [DOI] [PubMed] [Google Scholar]
- 55.Ghaffari A: Urgent-start peritoneal dialysis: a quality improvement report. Am J Kidney Dis 59: 400–408, 2012 [DOI] [PubMed] [Google Scholar]
- 56.Koch M, Kohnle M, Trapp R, Haastert B, Rump LC, Aker S: Comparable outcome of acute unplanned peritoneal dialysis and haemodialysis. Nephrol Dial Transplant 27: 375–380, 2012 [DOI] [PubMed] [Google Scholar]
- 57.Alkatheeri AM, Blake PG, Gray D, Jain AK: Success of Urgent-Start Peritoneal Dialysis in a Large Canadian Renal Program. Perit Dial Int 36: 171–176, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mehrotra R: Expanding access to peritoneal dialysis for incident dialysis patients. Am J Kidney Dis 59: 330–332, 2012 [DOI] [PubMed] [Google Scholar]
- 59.Oliver MJ, Garg AX, Blake PG, Johnson JF, Verrelli M, Zacharias JM, Pandeya S, Quinn RR: Impact of contraindications, barriers to self-care and support on incident peritoneal dialysis utilization. Nephrol Dial Transplant 25: 2737–2744, 2010 [DOI] [PubMed] [Google Scholar]
- 60.Cheng CH, Shu KH, Chuang YW, Huang ST, Chou MC, Chang HR: Clinical outcome of elderly peritoneal dialysis patients with assisted care in a single medical centre: a 25 year experience. Nephrology (Carlton) 18: 468–473, 2013 [DOI] [PubMed] [Google Scholar]
- 61.Lobbedez T, Verger C, Ryckelynck JP, Fabre E, Evans D: Is assisted peritoneal dialysis associated with technique survival when competing events are considered? Clin J Am Soc Nephrol 7: 612–618, 2012 [DOI] [PubMed] [Google Scholar]
- 62.Béchade C, Lobbedez T, Ivarsen P, Povlsen JV: Assisted Peritoneal Dialysis for Older People with End-Stage Renal Disease: The French and Danish Experience. Perit Dial Int 35: 663–666, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oliver MJ, Quinn RR, Richardson EP, Kiss AJ, Lamping DL, Manns BJ: Home care assistance and the utilization of peritoneal dialysis. Kidney Int 71: 673–678, 2007 [DOI] [PubMed] [Google Scholar]
- 64.Verger C, Duman M, Durand PY, Veniez G, Fabre E, Ryckelynck JP: Influence of autonomy and type of home assistance on the prevention of peritonitis in assisted automated peritoneal dialysis patients. An analysis of data from the French Language Peritoneal Dialysis Registry. Nephrol Dial Transplant 22: 1218–1223, 2007 [DOI] [PubMed] [Google Scholar]
- 65.Iyasere OU, Brown EA, Johansson L, Huson L, Smee J, Maxwell AP, Farrington K, Davenport A: Quality of Life and Physical Function in Older Patients on Dialysis: A Comparison of Assisted Peritoneal Dialysis with Hemodialysis. Clin J Am Soc Nephrol 11: 423–430, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mehrotra R, Soohoo M, Rivara MB, Himmelfarb J, Cheung AK, Arah OA, Nissenson AR, Ravel V, Streja E, Kuttykrishnan S, Katz R, Molnar MZ, Kalantar-Zadeh K: Racial and Ethnic Disparities in Use of and Outcomes with Home Dialysis in the United States [published online ahead of print December 10, 2015]. J Am Soc Nephrol doi:10.1681/ASN.2015050472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brimble KS, Walker M, Margetts PJ, Kundhal KK, Rabbat CG: Meta-analysis: peritoneal membrane transport, mortality, and technique failure in peritoneal dialysis. J Am Soc Nephrol 17: 2591–2598, 2006 [DOI] [PubMed] [Google Scholar]
- 68.Mehrotra R, Ravel V, Streja E, Kuttykrishnan S, Adams SV, Katz R, Molnar MZ, Kalantar-Zadeh K: Peritoneal Equilibration Test and Patient Outcomes. Clin J Am Soc Nephrol 10: 1990–2001, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Devuyst O, Nielsen S, Cosyns JP, Smith BL, Agre P, Squifflet JP, Pouthier D, Goffin E: Aquaporin-1 and endothelial nitric oxide synthase expression in capillary endothelia of human peritoneum. Am J Physiol 275: H234–H242, 1998 [DOI] [PubMed] [Google Scholar]
- 70.Agre P: Aquaporin water channels (Nobel Lecture). Angew Chem Int Ed Engl 43: 4278–4290, 2004 [DOI] [PubMed] [Google Scholar]
- 71.Morelle J, Sow A, Vertommen D, Jamar F, Rippe B, Devuyst O: Quantification of osmotic water transport in vivo using fluorescent albumin. Am J Physiol Renal Physiol 307: F981–F989, 2014 [DOI] [PubMed] [Google Scholar]
- 72.Ni J, Verbavatz JM, Rippe A, Boisdé I, Moulin P, Rippe B, Verkman AS, Devuyst O: Aquaporin-1 plays an essential role in water permeability and ultrafiltration during peritoneal dialysis. Kidney Int 69: 1518–1525, 2006 [DOI] [PubMed] [Google Scholar]
- 73.Rippe B, Stelin G, Haraldsson B: Computer simulations of peritoneal fluid transport in CAPD. Kidney Int 40: 315–325, 1991 [DOI] [PubMed] [Google Scholar]
- 74.Stoenoiu MS, Ni J, Verkaeren C, Debaix H, Jonas JC, Lameire N, Verbavatz JM, Devuyst O: Corticosteroids induce expression of aquaporin-1 and increase transcellular water transport in rat peritoneum. J Am Soc Nephrol 14: 555–565, 2003 [DOI] [PubMed] [Google Scholar]
- 75.de Arteaga J, Ledesma F, Garay G, Chiurchiu C, de la Fuente J, Douthat W, Massari P, Terryn S, Devuyst O: High-dose steroid treatment increases free water transport in peritoneal dialysis patients. Nephrol Dial Transplant 26: 4142–4145, 2011 [DOI] [PubMed] [Google Scholar]
- 76.Yool AJ, Morelle J, Cnops Y, Verbavatz JM, Campbell EM, Beckett EA, Booker GW, Flynn G, Devuyst O: AqF026 is a pharmacologic agonist of the water channel aquaporin-1. J Am Soc Nephrol 24: 1045–1052, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Oh KH, Jung JY, Yoon MO, Song A, Lee H, Ro H, Hwang YH, Kim DK, Margetts P, Ahn C: Intra-peritoneal interleukin-6 system is a potent determinant of the baseline peritoneal solute transport in incident peritoneal dialysis patients. Nephrol Dial Transplant 25: 1639–1646, 2010 [DOI] [PubMed] [Google Scholar]
- 78.Pecoits-Filho R, Araújo MR, Lindholm B, Stenvinkel P, Abensur H, Romão JE Jr, Marcondes M, De Oliveira AH, Noronha IL: Plasma and dialysate IL-6 and VEGF concentrations are associated with high peritoneal solute transport rate. Nephrol Dial Transplant 17: 1480–1486, 2002 [DOI] [PubMed] [Google Scholar]
- 79.Lambie M, Chess J, Donovan KL, Kim YL, Do JY, Lee HB, Noh H, Williams PF, Williams AJ, Davison S, Dorval M, Summers A, Williams JD, Bankart J, Davies SJ, Topley N; Global Fluid Study Investigators : Independent effects of systemic and peritoneal inflammation on peritoneal dialysis survival. J Am Soc Nephrol 24: 2071–2080, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rumpsfeld M, McDonald SP, Johnson DW: Higher peritoneal transport status is associated with higher mortality and technique failure in the Australian and New Zealand peritoneal dialysis patient populations. J Am Soc Nephrol 17: 271–278, 2006 [DOI] [PubMed] [Google Scholar]
- 81.Gillerot G, Goffin E, Michel C, Evenepoel P, Biesen WV, Tintillier M, Stenvinkel P, Heimbürger O, Lindholm B, Nordfors L, Robert A, Devuyst O: Genetic and clinical factors influence the baseline permeability of the peritoneal membrane. Kidney Int 67: 2477–2487, 2005 [DOI] [PubMed] [Google Scholar]
- 82.Hwang YH, Son MJ, Yang J, Kim K, Chung W, Joo KW, Kim Y, Ahn C, Oh KH: Effects of interleukin-6 T15A single nucleotide polymorphism on baseline peritoneal solute transport rate in incident peritoneal dialysis patients. Perit Dial Int 29: 81–88, 2009 [PubMed] [Google Scholar]
- 83.Combet S, Van Landschoot M, Moulin P, Piech A, Verbavatz JM, Goffin E, Balligand JL, Lameire N, Devuyst O: Regulation of aquaporin-1 and nitric oxide synthase isoforms in a rat model of acute peritonitis. J Am Soc Nephrol 10: 2185–2196, 1999 [DOI] [PubMed] [Google Scholar]
- 84.Ferrier ML, Combet S, van Landschoot M, Stoenoiu MS, Cnops Y, Lameire N, Devuyst O: Inhibition of nitric oxide synthase reverses changes in peritoneal permeability in a rat model of acute peritonitis. Kidney Int 60: 2343–2350, 2001 [DOI] [PubMed] [Google Scholar]
- 85.Ni J, Moulin P, Gianello P, Feron O, Balligand JL, Devuyst O: Mice that lack endothelial nitric oxide synthase are protected against functional and structural modifications induced by acute peritonitis. J Am Soc Nephrol 14: 3205–3216, 2003 [DOI] [PubMed] [Google Scholar]
- 86.Ni J, McLoughlin RM, Brodovitch A, Moulin P, Brouckaert P, Casadei B, Feron O, Topley N, Balligand JL, Devuyst O: Nitric oxide synthase isoforms play distinct roles during acute peritonitis. Nephrol Dial Transplant 25: 86–96, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Devuyst O, Margetts PJ, Topley N: The pathophysiology of the peritoneal membrane. J Am Soc Nephrol 21: 1077–1085, 2010 [DOI] [PubMed] [Google Scholar]
- 88.Morelle J, Sow A, Hautem N, Bouzin C, Crott R, Devuyst O, Goffin E: Interstitial Fibrosis Restricts Osmotic Water Transport in Encapsulating Peritoneal Sclerosis. J Am Soc Nephrol 26: 2521–2533, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Korte MR, Sampimon DE, Betjes MG, Krediet RT: Encapsulating peritoneal sclerosis: the state of affairs. Nat Rev Nephrol 7: 528–538, 2011 [DOI] [PubMed] [Google Scholar]
- 90.Lambie ML, John B, Mushahar L, Huckvale C, Davies SJ: The peritoneal osmotic conductance is low well before the diagnosis of encapsulating peritoneal sclerosis is made. Kidney Int 78: 611–618, 2010 [DOI] [PubMed] [Google Scholar]
- 91.Sampimon DE, Barreto DL, Coester AM, Struijk DG, Krediet RT: The value of osmotic conductance and free water transport in the prediction of encapsulating peritoneal sclerosis. Adv Perit Dial 30: 21–26, 2014 [PubMed] [Google Scholar]
- 92.Williams JD, Craig KJ, Topley N, Von Ruhland C, Fallon M, Newman GR, Mackenzie RK, Williams GT; Peritoneal Biopsy Study Group : Morphologic changes in the peritoneal membrane of patients with renal disease. J Am Soc Nephrol 13: 470–479, 2002 [DOI] [PubMed] [Google Scholar]
- 93.Yang AH, Chen JY, Lin JK: Myofibroblastic conversion of mesothelial cells. Kidney Int 63: 1530–1539, 2003 [DOI] [PubMed] [Google Scholar]
- 94.Yáñez-Mó M, Lara-Pezzi E, Selgas R, Ramírez-Huesca M, Domínguez-Jiménez C, Jiménez-Heffernan JA, Aguilera A, Sánchez-Tomero JA, Bajo MA, Alvarez V, Castro MA, del Peso G, Cirujeda A, Gamallo C, Sánchez-Madrid F, López-Cabrera M: Peritoneal dialysis and epithelial-to-mesenchymal transition of mesothelial cells. N Engl J Med 348: 403–413, 2003 [DOI] [PubMed] [Google Scholar]
- 95.Margetts PJ, Bonniaud P, Liu L, Hoff CM, Holmes CJ, West-Mays JA, Kelly MM: Transient overexpression of TGF-beta1 induces epithelial mesenchymal transition in the rodent peritoneum. J Am Soc Nephrol 16: 425–436, 2005 [DOI] [PubMed] [Google Scholar]
- 96.Aroeira LS, Aguilera A, Selgas R, Ramírez-Huesca M, Pérez-Lozano ML, Cirugeda A, Bajo MA, del Peso G, Sánchez-Tomero JA, Jiménez-Heffernan JA, López-Cabrera M: Mesenchymal conversion of mesothelial cells as a mechanism responsible for high solute transport rate in peritoneal dialysis: role of vascular endothelial growth factor. Am J Kidney Dis 46: 938–948, 2005 [DOI] [PubMed] [Google Scholar]
- 97.Humphreys BD, Lin SL, Kobayashi A, Hudson TE, Nowlin BT, Bonventre JV, Valerius MT, McMahon AP, Duffield JS: Fate tracing reveals the pericyte and not epithelial origin of myofibroblasts in kidney fibrosis. Am J Pathol 176: 85–97, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kriz W, Kaissling B, Le Hir M: Epithelial-mesenchymal transition (EMT) in kidney fibrosis: fact or fantasy? J Clin Invest 121: 468–474, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Quaggin SE, Kapus A: Scar wars: mapping the fate of epithelial-mesenchymal-myofibroblast transition. Kidney Int 80: 41–50, 2011 [DOI] [PubMed] [Google Scholar]
- 100.Chen YT, Chang YT, Pan SY, Chou YH, Chang FC, Yeh PY, Liu YH, Chiang WC, Chen YM, Wu KD, Tsai TJ, Duffield JS, Lin SL: Lineage tracing reveals distinctive fates for mesothelial cells and submesothelial fibroblasts during peritoneal injury. J Am Soc Nephrol 25: 2847–2858, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.García-López E, Lindholm B, Davies S: An update on peritoneal dialysis solutions. Nat Rev Nephrol 8: 224–233, 2012 [DOI] [PubMed] [Google Scholar]
- 102.Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, Foo MW, Jones B, Kulkarni H, Langham R, Ranganathan D, Schollum J, Suranyi MG, Tan SH, Voss D; balANZ Trial Investigators : The effect of low glucose degradation product, neutral pH versus standard peritoneal dialysis solutions on peritoneal membrane function: the balANZ trial. Nephrol Dial Transplant 27: 4445–4453, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kolesnyk I, Noordzij M, Dekker FW, Boeschoten EW, Krediet RT: A positive effect of AII inhibitors on peritoneal membrane function in long-term PD patients. Nephrol Dial Transplant 24: 272–277, 2009 [DOI] [PubMed] [Google Scholar]
- 104.Johnson DW, Dent H, Hawley CM, McDonald SP, Rosman JB, Brown FG, Bannister K, Wiggins KJ: Association of dialysis modality and cardiovascular mortality in incident dialysis patients. Clin J Am Soc Nephrol 4: 1620–1628, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Isoyama N, Machowska A, Qureshi AR, Yamamoto T, Anderstam B, Heimburger O, Barany P, Stenvinkel P, Lindholm B: Elevated Circulating S100a12 Associates with Vascular Disease and Worse Clinical Outcome in Peritoneal Dialysis Patients. Perit Dial Int 36: 269–276, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Boudville N, Kemp A, Clayton P, Lim W, Badve SV, Hawley CM, McDonald SP, Wiggins KJ, Bannister KM, Brown FG, Johnson DW: Recent peritonitis associates with mortality among patients treated with peritoneal dialysis. J Am Soc Nephrol 23: 1398–1405, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Davies SJ, Phillips L, Griffiths AM, Russell LH, Naish PF, Russell GI: What really happens to people on long-term peritoneal dialysis? Kidney Int 54: 2207–2217, 1998 [DOI] [PubMed] [Google Scholar]
- 108.Kim H, Kim KH, Ahn SV, Kang SW, Yoo TH, Ahn HS, Hann HJ, Lee S, Ryu JH, Yu M, Kim SJ, Kang DH, Choi KB, Ryu DR: Risk of major cardiovascular events among incident dialysis patients: A Korean national population-based study. Int J Cardiol 198: 95–101, 2015 [DOI] [PubMed] [Google Scholar]
- 109.Wang AY, Brimble KS, Brunier G, Holt SG, Jha V, Johnson DW, Kang SW, Kooman JP, Lambie M, McIntyre C, Mehrotra R, Pecoits-Filho R: ISPD Cardiovascular and Metabolic Guidelines in Adult Peritoneal Dialysis Patients Part I - Assessment and Management of Various Cardiovascular Risk Factors. Perit Dial Int 35: 379–387, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wang AY, Brimble KS, Brunier G, Holt SG, Jha V, Johnson DW, Kang SW, Kooman JP, Lambie M, McIntyre C, Mehrotra R, Pecoits-Filho R: ISPD Cardiovascular and Metabolic Guidelines in Adult Peritoneal Dialysis Patients Part II - Management of Various Cardiovascular Complications. Perit Dial Int 35: 388–396, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Little J, Phillips L, Russell L, Griffiths A, Russell GI, Davies SJ: Longitudinal lipid profiles on CAPD: their relationship to weight gain, comorbidity, and dialysis factors. J Am Soc Nephrol 9: 1931–1939, 1998 [DOI] [PubMed] [Google Scholar]
- 112.Attman PO, Samuelsson OG, Moberly J, Johansson AC, Ljungman S, Weiss LG, Knight-Gibson C, Alaupovic P: Apolipoprotein B-containing lipoproteins in renal failure: the relation to mode of dialysis. Kidney Int 55: 1536–1542, 1999 [DOI] [PubMed] [Google Scholar]
- 113.de Moraes TP, Fortes PC, Ribeiro SC, Riella MC, Pecoits-Filho R: Comparative analysis of lipid and glucose metabolism biomarkers in non-diabetic hemodialysis and peritoneal dialysis patients. J Bras Nefrol 33: 173–179, 2011. [DOI] [PubMed]
- 114.Johnson DW, Armstrong K, Campbell SB, Mudge DW, Hawley CM, Coombes JS, Prins JB, Isbel NM: Metabolic syndrome in severe chronic kidney disease: Prevalence, predictors, prognostic significance and effects of risk factor modification. Nephrology (Carlton) 12: 391–398, 2007 [DOI] [PubMed] [Google Scholar]
- 115.Jiang N, Qian J, Lin A, Lindholm B, Axelsson J, Yao Q: Initiation of glucose-based peritoneal dialysis is associated with increased prevalence of metabolic syndrome in non-diabetic patients with end-stage renal disease. Blood Purif 26: 423–428, 2008 [DOI] [PubMed] [Google Scholar]
- 116.Szeto CC, Chow KM, Kwan BC, Chung KY, Leung CB, Li PK: New-onset hyperglycemia in nondiabetic chinese patients started on peritoneal dialysis. Am J Kidney Dis 49: 524–532, 2007 [DOI] [PubMed] [Google Scholar]
- 117.Choi SJ, Kim NR, Hong SA, Lee WB, Park MY, Kim JK, Hwang SD, Lee HK: Changes in body fat mass in patients after starting peritoneal dialysis. Perit Dial Int 31: 67–73, 2011 [DOI] [PubMed] [Google Scholar]
- 118.Lievense H, Kalantar-Zadeh K, Lukowsky LR, Molnar MZ, Duong U, Nissenson A, Krishnan M, Krediet R, Mehrotra R: Relationship of body size and initial dialysis modality on subsequent transplantation, mortality and weight gain of ESRD patients. Nephrol Dial Transplant 27: 3631–3638, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ahmadi SF, Zahmatkesh G, Streja E, Mehrotra R, Rhee CM, Kovesdy CP, Gillen DL, Ahmadi E, Fonarow GC, Kalantar-Zadeh K: Association of Body Mass Index with Mortality in Peritoneal Dialysis Patients: A Systematic Review and Meta-Analysis. Perit Dial Int 36: 315–325, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bergström J, Fürst P, Alvestrand A, Lindholm B: Protein and energy intake, nitrogen balance and nitrogen losses in patients treated with continuous ambulatory peritoneal dialysis. Kidney Int 44: 1048–1057, 1993 [DOI] [PubMed] [Google Scholar]
- 121.Park J, Ahmadi SF, Streja E, Molnar MZ, Flegal KM, Gillen D, Kovesdy CP, Kalantar-Zadeh K: Obesity paradox in end-stage kidney disease patients. Prog Cardiovasc Dis 56: 415–425, 2014. [DOI] [PMC free article] [PubMed]
- 122.McDonald SP, Collins JF, Johnson DW: Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand patient populations. J Am Soc Nephrol 14: 2894–2901, 2003 [DOI] [PubMed] [Google Scholar]
- 123.Fernandes NM, Bastos MG, Franco MR, Chaoubah A, Lima MG, Divino-Filho JC, Qureshi AR; Brazilian Peritoneal Dialysis Multicenter Study (BRAZPD) Group : Body size and longitudinal body weight changes do not increase mortality in incident peritoneal dialysis patients of the Brazilian peritoneal dialysis multicenter study. Clinics (Sao Paulo) 68: 51–58, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Badve SV, Paul SK, Klein K, Clayton PA, Hawley CM, Brown FG, Boudville N, Polkinghorne KR, McDonald SP, Johnson DW: The association between body mass index and mortality in incident dialysis patients. PLoS One 9: e114897, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liao CT, Kao TW, Chou YH, Wu MS, Chen YM, Chuang HF, Hung KY, Chu TS, Wu KD, Tsai TJ: Associations of metabolic syndrome and its components with cardiovascular outcomes among non-diabetic patients undergoing maintenance peritoneal dialysis. Nephrol Dial Transplant 26: 4047–4054, 2011 [DOI] [PubMed] [Google Scholar]
- 126.Szeto CC, Kwan BC, Chow KM, Leung CB, Cheng MS, Law MC, Li PK: Metabolic syndrome in peritoneal dialysis patients: choice of diagnostic criteria and prognostic implications. Clin J Am Soc Nephrol 9: 779–787, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chou CY, Liang CC, Kuo HL, Chang CT, Liu JH, Lin HH, Wang IK, Yang YF, Huang CC: Comparing risk of new onset diabetes mellitus in chronic kidney disease patients receiving peritoneal dialysis and hemodialysis using propensity score matching. PLoS One 9: e87891, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Woodward RS, Schnitzler MA, Baty J, Lowell JA, Lopez-Rocafort L, Haider S, Woodworth TG, Brennan DC: Incidence and cost of new onset diabetes mellitus among U.S. wait-listed and transplanted renal allograft recipients. Am J Transplant 3: 590–598, 2003 [DOI] [PubMed] [Google Scholar]
- 129.Davies SJ, Woodrow G, Donovan K, Plum J, Williams P, Johansson AC, Bosselmann HP, Heimbürger O, Simonsen O, Davenport A, Tranaeus A, Divino Filho JC: Icodextrin improves the fluid status of peritoneal dialysis patients: results of a double-blind randomized controlled trial. J Am Soc Nephrol 14: 2338–2344, 2003 [DOI] [PubMed] [Google Scholar]
- 130.Wolfson M, Piraino B, Hamburger RJ, Morton AR; Icodextrin Study Group : A randomized controlled trial to evaluate the efficacy and safety of icodextrin in peritoneal dialysis. Am J Kidney Dis 40: 1055–1065, 2002 [DOI] [PubMed] [Google Scholar]
- 131.de Moraes TP, Andreoli MC, Canziani ME, da Silva DR, Caramori JC, Ponce D, Cassi HV, de Andrade Bastos K, Rio DR, Pinto SW, Filho SR, de Campos LG, Olandoski M, Divino-Filho JC, Pecoits-Filho R: Icodextrin reduces insulin resistance in non-diabetic patients undergoing automated peritoneal dialysis: results of a randomized controlled trial (STARCH). Nephrol Dial Transplant 30: 1905–1911, 2015 [DOI] [PubMed] [Google Scholar]
- 132.Paniagua R, Ventura MD, Avila-Díaz M, Cisneros A, Vicenté-Martínez M, Furlong MD, García-González Z, Villanueva D, Orihuela O, Prado-Uribe MD, Alcántara G, Amato D: Icodextrin improves metabolic and fluid management in high and high-average transport diabetic patients. Perit Dial Int 29: 422–432, 2009 [PubMed] [Google Scholar]
- 133.Li PK, Culleton BF, Ariza A, Do JY, Johnson DW, Sanabria M, Shockley TR, Story K, Vatazin A, Verrelli M, Yu AW, Bargman JM; IMPENDIA and EDEN Study Groups : Randomized, controlled trial of glucose-sparing peritoneal dialysis in diabetic patients. J Am Soc Nephrol 24: 1889–1900, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sniderman AD, Sloand JA, Li PK, Story K, Bargman JM: Influence of low-glucose peritoneal dialysis on serum lipids and apolipoproteins in the IMPENDIA/EDEN trials. J Clin Lipidol 8: 441–447, 2014 [DOI] [PubMed] [Google Scholar]
- 135.Duong U, Mehrotra R, Molnar MZ, Noori N, Kovesdy CP, Nissenson AR, Kalantar-Zadeh K: Glycemic control and survival in peritoneal dialysis patients with diabetes mellitus. Clin J Am Soc Nephrol 6: 1041–1048, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yoo DE, Park JT, Oh HJ, Kim SJ, Lee MJ, Shin DH, Han SH, Yoo TH, Choi KH, Kang SW: Good glycemic control is associated with better survival in diabetic patients on peritoneal dialysis: a prospective observational study. PLoS One 7: e30072, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Palmer SC, Navaneethan SD, Craig JC, Johnson DW, Perkovic V, Nigwekar SU, Hegbrant J, Strippoli GF: HMG CoA reductase inhibitors (statins) for dialysis patients. Cochrane Database Syst Rev 9: CD004289, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, Wanner C, Krane V, Cass A, Craig J, Neal B, Jiang L, Hooi LS, Levin A, Agodoa L, Gaziano M, Kasiske B, Walker R, Massy ZA, Feldt-Rasmussen B, Krairittichai U, Ophascharoensuk V, Fellström B, Holdaas H, Tesar V, Wiecek A, Grobbee D, de Zeeuw D, Grönhagen-Riska C, Dasgupta T, Lewis D, Herrington W, Mafham M, Majoni W, Wallendszus K, Grimm R, Pedersen T, Tobert J, Armitage J, Baxter A, Bray C, Chen Y, Chen Z, Hill M, Knott C, Parish S, Simpson D, Sleight P, Young A, Collins R; SHARP Investigators : The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet 377: 2181–2192, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bargman JM, Thorpe KE, Churchill DN; CANUSA Peritoneal Dialysis Study Group : Relative contribution of residual renal function and peritoneal clearance to adequacy of dialysis: a reanalysis of the CANUSA study. J Am Soc Nephrol 12: 2158–2162, 2001 [DOI] [PubMed] [Google Scholar]
- 140.Termorshuizen F, Dekker FW, van Manen JG, Korevaar JC, Boeschoten EW, Krediet RT; NECOSAD Study Group : Relative contribution of residual renal function and different measures of adequacy to survival in hemodialysis patients: an analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD)-2. J Am Soc Nephrol 15: 1061–1070, 2004 [DOI] [PubMed] [Google Scholar]
- 141.Fernández-Lucas M, Teruel-Briones JL, Gomis-Couto A, Villacorta-Pérez J, Quereda-Rodríguez-Navarro C: Maintaining residual renal function in patients on haemodialysis: 5-year experience using a progressively increasing dialysis regimen. Nefrologia 32: 767–776, 2012 [DOI] [PubMed] [Google Scholar]
- 142.Lin YF, Huang JW, Wu MS, Chu TS, Lin SL, Chen YM, Tsai TJ, Wu KD: Comparison of residual renal function in patients undergoing twice-weekly versus three-times-weekly haemodialysis. Nephrology (Carlton) 14: 59–64, 2009 [DOI] [PubMed] [Google Scholar]
- 143.Seo EY, An SH, Cho JH, Suh HS, Park SH, Gwak H, Kim YL, Ha H: Effect of biocompatible peritoneal dialysis solution on residual renal function: a systematic review of randomized controlled trials. Perit Dial Int 34: 724–731, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kjaergaard KD, Peters CD, Jespersen B, Tietze IN, Madsen JK, Pedersen BB, Novosel MK, Laursen KS, Bibby BM, Strandhave C, Jensen JD: Angiotensin blockade and progressive loss of kidney function in hemodialysis patients: a randomized controlled trial. Am J Kidney Dis 64: 892–901, 2014 [DOI] [PubMed] [Google Scholar]
- 145.Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, Krediet RT; NECOSAD Study Group : Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int 62: 1046–1053, 2002 [DOI] [PubMed] [Google Scholar]
- 146.Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, Wolfe RA, Hulbert-Shearon T, Jones CA, Bloembergen WE: Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol 11: 556–564, 2000 [DOI] [PubMed] [Google Scholar]
- 147.van Biesen W, Claes K, Covic A, Fan S, Lichodziejewska-Niemierko M, Schoder V, Verger C, Wabel P: A multicentric, international matched pair analysis of body composition in peritoneal dialysis versus haemodialysis patients. Nephrol Dial Transplant 28: 2620–2628, 2013 [DOI] [PubMed] [Google Scholar]
- 148.Ha IS, Yap HK, Munarriz RL, Zambrano PH, Flynn JT, Bilge I, Szczepanska M, Lai WM, Antonio ZL, Gulati A, Hooman N, van Hoeck K, Higuita LM, Verrina E, Klaus G, Fischbach M, Riyami MA, Sahpazova E, Sander A, Warady BA, Schaefer F; International Pediatric Peritoneal Dialysis Network Registry : Risk factors for loss of residual renal function in children treated with chronic peritoneal dialysis. Kidney Int 88: 605–613, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Medcalf JF, Harris KP, Walls J: Role of diuretics in the preservation of residual renal function in patients on continuous ambulatory peritoneal dialysis. Kidney Int 59: 1128–1133, 2001 [DOI] [PubMed] [Google Scholar]
- 150.Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, Foo MW, Jones B, Kulkarni H, Langham R, Ranganathan D, Schollum J, Suranyi M, Tan SH, Voss D; balANZ Trial Investigators : Effects of biocompatible versus standard fluid on peritoneal dialysis outcomes. J Am Soc Nephrol 23: 1097–1107, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cho Y, Johnson DW, Craig JC, Strippoli GF, Badve SV, Wiggins KJ: Biocompatible dialysis fluids for peritoneal dialysis. Cochrane Database Syst Rev 3: CD007554, 2014 [DOI] [PubMed] [Google Scholar]
- 152.Udayaraj UP, Steenkamp R, Caskey FJ, Rogers C, Nitsch D, Ansell D, Tomson CR: Blood pressure and mortality risk on peritoneal dialysis. Am J Kidney Dis 53: 70–78, 2009 [DOI] [PubMed] [Google Scholar]
- 153.Davies SJ, Davenport A: The role of bioimpedance and biomarkers in helping to aid clinical decision-making of volume assessments in dialysis patients. Kidney Int 86: 489–496, 2014 [DOI] [PubMed] [Google Scholar]
- 154.Brown EA, Davies SJ, Rutherford P, Meeus F, Borras M, Riegel W, Divino Filho JC, Vonesh E, van Bree M; EAPOS Group : Survival of functionally anuric patients on automated peritoneal dialysis: the European APD Outcome Study. J Am Soc Nephrol 14: 2948–2957, 2003 [DOI] [PubMed] [Google Scholar]
- 155.Jansen MA, Termorshuizen F, Korevaar JC, Dekker FW, Boeschoten E, Krediet RT; NECOSAD Study Group : Predictors of survival in anuric peritoneal dialysis patients. Kidney Int 68: 1199–1205, 2005 [DOI] [PubMed] [Google Scholar]
- 156.Johnson DW, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Badve SV: Superior survival of high transporters treated with automated versus continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant 25: 1973–1979, 2010 [DOI] [PubMed] [Google Scholar]
- 157.Cho Y, Johnson DW, Badve S, Craig JC, Strippoli GF, Wiggins KJ: Impact of icodextrin on clinical outcomes in peritoneal dialysis: a systematic review of randomized controlled trials. Nephrol Dial Transplant 28: 1899–1907, 2013 [DOI] [PubMed] [Google Scholar]
- 158.Mehrotra R, Duong U, Jiwakanon S, Kovesdy CP, Moran J, Kopple JD, Kalantar-Zadeh K: Serum albumin as a predictor of mortality in peritoneal dialysis: comparisons with hemodialysis. Am J Kidney Dis 58: 418–428, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.John B, Tan BK, Dainty S, Spanel P, Smith D, Davies SJ: Plasma volume, albumin, and fluid status in peritoneal dialysis patients. Clin J Am Soc Nephrol 5: 1463–1470, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Tan BK, Yu Z, Fang W, Lin A, Ni Z, Qian J, Woodrow G, Jenkins SB, Wilkie ME, Davies SJ: Longitudinal bioimpedance vector plots add little value to fluid management of peritoneal dialysis patients. Kidney Int 89: 487–497, 2016 [DOI] [PubMed] [Google Scholar]
- 161.Cho Y, Johnson DW: Peritoneal dialysis-related peritonitis: towards improving evidence, practices, and outcomes. Am J Kidney Dis 64: 278–289, 2014 [DOI] [PubMed] [Google Scholar]
- 162.Johnson DW, Dent H, Hawley CM, McDonald SP, Rosman JB, Brown FG, Bannister KM, Wiggins KJ: Associations of dialysis modality and infectious mortality in incident dialysis patients in Australia and New Zealand. Am J Kidney Dis 53: 290–297, 2009 [DOI] [PubMed] [Google Scholar]
- 163.Szeto CC, Wong TY, Chow KM, Leung CB, Li PK: The clinical course of culture-negative peritonitis complicating peritoneal dialysis. Am J Kidney Dis 42: 567–574, 2003 [DOI] [PubMed] [Google Scholar]
- 164.Szeto CC, Chow KM, Kwan BC, Law MC, Chung KY, Yu S, Leung CB, Li PK: Staphylococcus aureus peritonitis complicates peritoneal dialysis: review of 245 consecutive cases. Clin J Am Soc Nephrol 2: 245–251, 2007 [DOI] [PubMed] [Google Scholar]
- 165.Szeto CC, Kwan BC, Chow KM, Lau MF, Law MC, Chung KY, Leung CB, Li PK: Coagulase negative staphylococcal peritonitis in peritoneal dialysis patients: review of 232 consecutive cases. Clin J Am Soc Nephrol 3: 91–97, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Barraclough K, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Corynebacterium peritonitis in Australian peritoneal dialysis patients: predictors, treatment and outcomes in 82 cases. Nephrol Dial Transplant 24: 3834–3839, 2009 [DOI] [PubMed] [Google Scholar]
- 167.Fahim M, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Culture-negative peritonitis in peritoneal dialysis patients in Australia: predictors, treatment, and outcomes in 435 cases. Am J Kidney Dis 55: 690–697, 2010 [DOI] [PubMed] [Google Scholar]
- 168.Miles R, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Predictors and outcomes of fungal peritonitis in peritoneal dialysis patients. Kidney Int 76: 622–628, 2009 [DOI] [PubMed] [Google Scholar]
- 169.Barraclough K, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Polymicrobial peritonitis in peritoneal dialysis patients in Australia: predictors, treatment, and outcomes. Am J Kidney Dis 55: 121–131, 2010 [DOI] [PubMed] [Google Scholar]
- 170.Edey M, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Enterococcal peritonitis in Australian peritoneal dialysis patients: predictors, treatment and outcomes in 116 cases. Nephrol Dial Transplant 25: 1272–1278, 2010 [DOI] [PubMed] [Google Scholar]
- 171.Fahim M, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Coagulase-negative staphylococcal peritonitis in Australian peritoneal dialysis patients: predictors, treatment and outcomes in 936 cases. Nephrol Dial Transplant 25: 3386–3392, 2010 [DOI] [PubMed] [Google Scholar]
- 172.Govindarajulu S, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Staphylococcus aureus peritonitis in Australian peritoneal dialysis patients: predictors, treatment, and outcomes in 503 cases. Perit Dial Int 30: 311–319, 2010 [DOI] [PubMed] [Google Scholar]
- 173.Jarvis EM, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Predictors, treatment, and outcomes of non-Pseudomonas Gram-negative peritonitis. Kidney Int 78: 408–414, 2010 [DOI] [PubMed] [Google Scholar]
- 174.Ghali JR, Bannister KM, Brown FG, Rosman JB, Wiggins KJ, Johnson DW, McDonald SP: Microbiology and outcomes of peritonitis in Australian peritoneal dialysis patients. Perit Dial Int 31: 651–662, 2011 [DOI] [PubMed] [Google Scholar]
- 175.Brown MC, Simpson K, Kerssens JJ, Mactier RA; Scottish Renal Registry : Encapsulating peritoneal sclerosis in the new millennium: a national cohort study. Clin J Am Soc Nephrol 4: 1222–1229, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Johnson DW, Cho Y, Livingston BE, Hawley CM, McDonald SP, Brown FG, Rosman JB, Bannister KM, Wiggins KJ: Encapsulating peritoneal sclerosis: incidence, predictors, and outcomes. Kidney Int 77: 904–912, 2010 [DOI] [PubMed] [Google Scholar]
- 177.Howard K, Hayes A, Cho Y, Cass A, Clarke M, Johnson DW: Economic evaluation of neutral-pH, low-glucose degradation product peritoneal dialysis solutions compared with standard solutions: a secondary analysis of the balANZ Trial. Am J Kidney Dis 65: 773–779, 2015 [DOI] [PubMed] [Google Scholar]
- 178.Morton RL, Snelling P, Webster AC, Rose J, Masterson R, Johnson DW, Howard K: Dialysis modality preference of patients with CKD and family caregivers: a discrete-choice study. Am J Kidney Dis 60: 102–111, 2012 [DOI] [PubMed] [Google Scholar]
- 179.Campbell DJ, Johnson DW, Mudge DW, Gallagher MP, Craig JC: Prevention of peritoneal dialysis-related infections. Nephrol Dial Transplant 30: 1461–1472, 2015 [DOI] [PubMed] [Google Scholar]
- 180.Huang JW, Hung KY, Yen CJ, Wu KD, Tsai TJ: Comparison of infectious complications in peritoneal dialysis patients using either a twin-bag system or automated peritoneal dialysis. Nephrol Dial Transplant 16: 604–607, 2001 [DOI] [PubMed] [Google Scholar]
- 181.Han SH, Lee SC, Ahn SV, Lee JE, Choi HY, Kim BS, Kang SW, Choi KH, Han DS, Lee HY: Improving outcome of CAPD: twenty-five years’ experience in a single Korean center. Perit Dial Int 27: 432–440, 2007 [PubMed] [Google Scholar]
- 182.Moraes TP, Pecoits-Filho R, Ribeiro SC, Rigo M, Silva MM, Teixeira PS, Pasqual DD, Fuerbringer R, Riella MC: Peritoneal dialysis in Brazil: twenty-five years of experience in a single center. Perit Dial Int 29: 492–498, 2009 [PubMed] [Google Scholar]
- 183.Huang ST, Chuang YW, Cheng CH, Wu MJ, Chen CH, Yu TM, Shu KH: Evolution of microbiological trends and treatment outcomes in peritoneal dialysis-related peritonitis. Clin Nephrol 75: 416–425, 2011 [DOI] [PubMed] [Google Scholar]
- 184.Rocha A, Rodrigues A, Teixeira L, Carvalho MJ, Mendonça D, Cabrita A: Temporal trends in peritonitis rates, microbiology and outcomes: the major clinical complication of peritoneal dialysis. Blood Purif 33: 284–291, 2012 [DOI] [PubMed] [Google Scholar]
- 185.Ozisik L, Ozdemir FN, Tanriover MD: The changing trends of peritoneal dialysis related peritonitis and novel risk factors. Ren Fail 37: 1027–1032, 2015 [DOI] [PubMed] [Google Scholar]
- 186.Kiernan L, Kliger A, Gorban-Brennan N, Juergensen P, Tesin D, Vonesh E, Finkelstein F: Comparison of continuous ambulatory peritoneal dialysis-related infections with different “Y-tubing” exchange systems. J Am Soc Nephrol 5: 1835–1838, 1995 [DOI] [PubMed] [Google Scholar]
- 187.Lo WK, Chan CY, Cheng SW, Poon JF, Chan DT, Cheng IK: A prospective randomized control study of oral nystatin prophylaxis for Candida peritonitis complicating continuous ambulatory peritoneal dialysis. Am J Kidney Dis 28: 549–552, 1996 [DOI] [PubMed] [Google Scholar]
- 188.Thodis E, Bhaskaran S, Pasadakis P, Bargman JM, Vas SI, Oreopoulos DG: Decrease in Staphylococcus aureus exit-site infections and peritonitis in CAPD patients by local application of mupirocin ointment at the catheter exit site. Perit Dial Int 18: 261–270, 1998 [PubMed] [Google Scholar]
- 189.Bernardini J, Bender F, Florio T, Sloand J, Palmmontalbano L, Fried L, Piraino B: Randomized, double-blind trial of antibiotic exit site cream for prevention of exit site infection in peritoneal dialysis patients. J Am Soc Nephrol 16: 539–545, 2005 [DOI] [PubMed] [Google Scholar]
- 190.Troidle L, Finkelstein F: Treatment and outcome of CPD-associated peritonitis. Ann Clin Microbiol Antimicrob 5: 6, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Gadola L, Poggi C, Poggio M, Sáez L, Ferrari A, Romero J, Fumero S, Ghelfi G, Chifflet L, Borges PL: Using a multidisciplinary training program to reduce peritonitis in peritoneal dialysis patients. Perit Dial Int 33: 38–45, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Zhang L, Hawley CM, Johnson DW: Focus on peritoneal dialysis training: working to decrease peritonitis rates. Nephrol Dial Transplant 31: 214–222, 2016 [DOI] [PubMed] [Google Scholar]
- 193.Schaepe C, Bergjan M: Educational interventions in peritoneal dialysis: a narrative review of the literature. Int J Nurs Stud 52: 882–898, 2015 [DOI] [PubMed] [Google Scholar]
- 194.Registry ANZDATA: 37th Report, Chapter 5, Adelaide, Australia, Peritoneal Dialysis, Australia and New Zealand Dialysis and Transplant Registry, 2015 [Google Scholar]
- 195.Jose MD, Johnson DW, Mudge DW, Tranaeus A, Voss D, Walker R, Bannister KM: Peritoneal dialysis practice in Australia and New Zealand: a call to action. Nephrology (Carlton) 16: 19–29, 2011 [DOI] [PubMed] [Google Scholar]
- 196.Johnson DW, Badve SV, Pascoe EM, Beller E, Cass A, Clark C, de Zoysa J, Isbel NM, McTaggart S, Morrish AT, Playford EG, Scaria A, Snelling P, Vergara LA, Hawley CM; HONEYPOT Study Collaborative Group : Antibacterial honey for the prevention of peritoneal-dialysis-related infections (HONEYPOT): a randomised trial. Lancet Infect Dis 14: 23–30, 2014 [DOI] [PubMed] [Google Scholar]
- 197.Campbell DJ, Brown FG, Craig JC, Gallagher MP, Johnson DW, Kirkland GS, Kumar SK, Lim WH, Ranganathan D, Saweirs W, Sud K, Toussaint ND, Walker RG, Williams LA, Yehia M, Mudge DW: Assessment of current practice and barriers to antimicrobial prophylaxis in peritoneal dialysis patients. Nephrol Dial Transplant 31: 619–627, 2016 [DOI] [PubMed] [Google Scholar]
- 198.Walker A, Bannister K, George C, Mudge D, Yehia M, Lonergan M, Chow J: KHA-CARI Guideline: peritonitis treatment and prophylaxis. Nephrology (Carlton) 19: 69–71, 2014 [DOI] [PubMed] [Google Scholar]
- 199.Zhang L, Badve SV, Pascoe EM, Beller E, Cass A, Clark C, De Zoysa J, Isbel NM, McTaggart S, Morrish AT, Playford EG, Scaria A, Snelling P, Vergara LA, Hawley CM, Johnson DW, Honeypot Study Collaborative : Microbiological results of the HONEYPOT study - secondary analysis of a randomised, controlled trial of exit site application of medihoney for the prevention of catheter-associated infections in PD patients. Nephrology (Carlton) 19: 30, 2014 [Google Scholar]
- 200.Piraino B, Bernardini J, Brown E, Figueiredo A, Johnson DW, Lye WC, Price V, Ramalakshmi S, Szeto CC: ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int 31: 614–630, 2011 [DOI] [PubMed] [Google Scholar]
- 201.Kopriva-Altfahrt G, König P, Mündle M, Prischl F, Roob JM, Wiesholzer M, Vychytil A, Arneitz K, Karner A, Artes R, Wolf E, Auinger M, Pawlak A, Fraberger J, Hofbauer S, Galvan G, Salmhofer H, Pichler B, Wazel M, Gruber M, Thonhofer A, Hager A, Malajner S, Heiss S, Braunsteiner T, Zweiffler M, König P, Rudnicki M, Kogler R, Kohlhauser D, Wiesinger T, Kopriva-Altfahrt G, Moser E, Kotanko P, Loibner H, Nitz H, Miska HJ, Wenzel R, Wölfer M, Mündle M, Breuss H, Hölzl B, Prischi F, Schmekal B, Riener EM, Roob JM, Wonisch W, Vikydal R, Vychytil A, Frank B, Wieser C, Wiesholzer M, Pokorny K; Austrian Study Group for Prevention of Peritoneal Catheter-Associated Infections : Exit-site care in Austrian peritoneal dialysis centers -- a nationwide survey. Perit Dial Int 29: 330–339, 2009 [PubMed] [Google Scholar]
- 202.Kavanagh D, Prescott GJ, Mactier RA: Peritoneal dialysis-associated peritonitis in Scotland (1999-2002). Nephrol Dial Transplant 19: 2584–2591, 2004 [DOI] [PubMed] [Google Scholar]
- 203.Davenport A: Peritonitis remains the major clinical complication of peritoneal dialysis: the London, UK, peritonitis audit 2002-2003. Perit Dial Int 29: 297–302, 2009 [PubMed] [Google Scholar]
- 204.Martin LC, Caramori JC, Fernandes N, Divino-Filho JC, Pecoits-Filho R, Barretti P; Brazilian Peritoneal Dialysis Multicenter Study BRAZPD Group : Geographic and educational factors and risk of the first peritonitis episode in Brazilian Peritoneal Dialysis study (BRAZPD) patients. Clin J Am Soc Nephrol 6: 1944–1951, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Figueiredo AE, Moraes TP, Bernardini J, Poli-de-Figueiredo CE, Barretti P, Olandoski M, Pecoits-Filho R; BRAZPD Investigators : Impact of patient training patterns on peritonitis rates in a large national cohort study. Nephrol Dial Transplant 30: 137–142, 2015 [DOI] [PubMed] [Google Scholar]
- 206.Badve SV, Smith A, Hawley CM, Johnson DW: Adherence to guideline recommendations for infection prophylaxis in peritoneal dialysis patients. NDT Plus 2: 508, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Nadeau-Fredette AC, Johnson DW, Hawley CM, Pascoe E, Cho Y, Clayton PA, Borlace M, Badve SV, Sud K, Boudville N, McDonald SP: Centre-specific factors associated with peritonitis risk - a multi-center registry analysis [published online ahead of print, January 13, 2016. Perit Dial Int doi:10.3747/pdi.2015.00146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Li PK, Szeto CC, Piraino B, Bernardini J, Figueiredo AE, Gupta A, Johnson DW, Kuijper EJ, Lye WC, Salzer W, Schaefer F, Struijk DG; International Society for Peritoneal Dialysis : Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int 30: 393–423, 2010 [DOI] [PubMed] [Google Scholar]