Primary care providers feel conflicted about using costly follow-up tests for incidental imaging findings of limited clinical importance and may not act on unfamiliar incidental findings when no clear follow-up recommendations are provided in a radiology report.
Abstract
Purpose
To explore provider and patient characteristics that influence how primary care providers (PCPs) communicate and manage incidental imaging findings.
Materials and Methods
This HIPAA-compliant study was approved by the institutional review board. Through semistructured interviews, researchers explored concerns and perspectives of 30 PCPs on receiving and acting on incidental imaging findings. Open-ended questions were designed to elicit a range of responses rather than quantifiable data. Thematic codes were developed and explicitly defined. Three research assistants independently coded all 30 deidentified transcripts and resolved discrepancies (κ = 0.85). Codes pertaining to PCP and patient characteristics were organized into an explanatory model.
Results
Some PCPs felt compelled but frustrated to pursue costly follow-up for incidental imaging findings of limited clinical importance. Other PCPs did not act on findings that were unfamiliar or occurred in an unusual clinical context when follow-up recommendations were not given; the challenges of researching the clinical importance of these findings or seeking specialist consultation led to inaction. Some PCPs reported using a uniform approach to communicate and manage incidental findings, while others adapted their approach to the patient and the finding. Sometimes PCP characteristics such as follow-up style superseded patient characteristics. At other times patient characteristics such as health literacy superseded PCP characteristics.
Conclusion
PCPs cited a variety of objective and subjective factors that influence how they communicate and manage incidental imaging findings. These results suggest that some patients may receive inappropriate follow-up of incidental imaging findings and present an opportunity for radiologists to help PCPs and patients to best use the information conveyed in imaging reports.
© RSNA, 2016
Introduction
Incidental or unexpected actionable findings are commonly detected on imaging studies (1). Some of these findings require no further follow-up, while others require repeat imaging or tissue sampling to allow a definitive diagnosis to be made. Consensus statements and white papers have advocated for the use of specific follow-up algorithms for many incidental findings, including those for pulmonary and thyroid nodules, renal masses, and ovarian lesions (2–5). Yet up to two-thirds of patients whose radiology reports advise follow-up do not receive it (6,7), and the majority of repeat high-cost imaging examinations are initiated without a radiologist’s recommendation (8). These disparate scenarios reflect a host of factors other than imaging features that influence follow-up of radiologic findings. Our purpose was to conduct qualitative interviews with primary care physicians (PCPs) to explore how they communicate and manage incidental findings on imaging examinations; in this article we focus on characteristics of PCPs and patients that influence follow-up.
Study Overview
This study was approved by our institutional review board. The main 789-bed urban hospital in our health system employs 1871 physicians including 107 outpatient PCPs. We conducted open-ended, semistructured interviews with a convenience sample of 30 PCPs. PCPs were selected between August 2013 and January 2014 in order of response to recruitment e-mails and phone calls. Interviews were conducted between September 2013 and January 2014. The interview guide, which was developed through literature review and expert consultation, included a series of questions asking the PCPs to describe a patient in their practice with an incidental imaging finding. The interview was designed to uncover their concerns and perspectives about receiving and acting on these findings. Interview questions relevant to PCP and patient characteristics are provided in Appendix E1 (online) and the full guide is provided in Appendix E2 (online). Whereas quantitative studies use deductive reasoning to test a theory on the basis of predetermined domains, qualitative studies use inductive reasoning to generate theory on the basis of the experiences of the subjects interviewed. Accordingly, in this qualitative study, we sought to identify and understand a broad range of experiences with incidental findings, without enumerating or prioritizing providers’ responses.
Data Collection
Volunteers were recruited from the study site’s Departments of Family Medicine or Internal Medicine. Interviews were conducted by a research assistant with an MPH degree (nonauthor with more than 3 years of experience in qualitative research) and a qualitative research scientist with a PhD degree (R.F., with more than 13 years of experience); each had worked on more than 25 qualitative studies. PCPs were interviewed by phone or in person for approximately 20–30 minutes. All PCPs gave verbal consent, completed a short demographic questionnaire, and received a gift card for $50 at the completion of data collection. Audio recordings of every interview were transcribed verbatim and deidentified by an independent third party. Transcripts were checked for accuracy against the audio recordings by a member of the research team with an MPH degree and more than 3 years of qualitative research experience (nonauthor).
Analysis
Thematic codes were developed in two ways: a priori (informed by the literature and interview guide) and through line-by-line reading of a subsample of interview transcripts. Each code was given an explicit definition to ensure coding accuracy and to improve intercoder reliability (9). Codes relevant to PCP and patient characteristics are provided in Appendix E3 (online) and the full code book is provided in Appendix E4 (online). Three research assistants who had coded 3–25 qualitative studies (nonauthor with an MPH degree and more than 3 years of qualitative research experience and author E.K.B. and a nonauthor, each with a BS degree and more than 2 years of qualitative research experience) independently coded all 30 deidentified transcripts by using a software program for qualitative data coding and analysis (Nvivo 10; QSR International, Doncaster, Australia). Coding was supervised by a qualitative research scientist (R.F., with more than 13 years of experience). Discrepancies in coding were resolved in consensus and review with clinical members of the research team. A constant comparison approach was used, whereby completed interviews were coded before later interviews were conducted. On the basis of this information, a sample size of 30 was considered sufficient to achieve saturation, meaning later interviews did not generate new codes (10). Codes pertaining to PCP and patient characteristics were organized into an explanatory model.
Results
A total of 15 family medicine and 15 internal medicine providers participated in this study. Mean age, years in practice, and sex and race distribution were similar between specialties. Compared with all outpatient PCPs at our main hospital, a slightly higher proportion of male PCPs participated in the study (Table). Intercoder reliability was calculated with Nvivo 10 software by using the κ coefficient. The software compares agreement and disagreement between coders in the assignment of specific codes to segments of the interview transcript. Complete agreement in coding correlates with a mean κ of 1; near perfect agreement, a mean κ of 0.81–0.99; substantial agreement, a mean κ of 0.61–0.80; and moderate agreement, a mean κ of 0.41–0.60. Analysis of intercoder reliability for this study revealed substantial to almost perfect agreement (mean κ = 0.85; range, 0.60–1.00). This result was supported by percentage of agreement analysis, which yielded a mean of 95% (range, 82%–100%) agreement of all codes examined in this study (11).
Characteristics of Study PCPs Compared with All Outpatient PCPs at Our Main Hospital
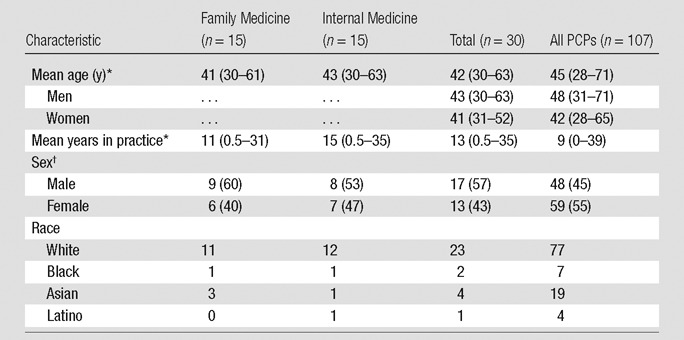
Note.—Unless otherwise indicated, data are number of patients.
*Data are mean number of years, with the range in parentheses.
†Data are number of patients, with percentage in parentheses.
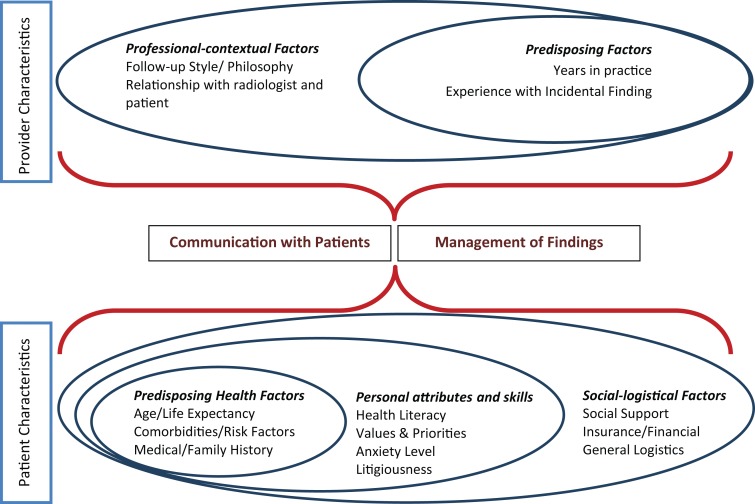
Coding of interview transcripts revealed that both subjective and objective characteristics influenced PCP and patient decisions about communication and management of incidental findings. Provider characteristics that influenced decision making included predisposing and professional contextual factors; patient characteristics included predisposing health factors, personal attributes and skills, and social-logistical factors (Figure). Summative statements for key themes were supported by PCP quotations.
Illustration shows modified ecologic model of PCP and patient characteristics, organized into spheres of influence, considered by PCPs in the communication and management of incidental findings (12).
Provider Characteristics: Predisposing Factors
Experience with incidental findings.—PCPs felt uncomfortable managing incidental imaging findings outside their scope of practice. They indicated the value of clear descriptions and explicit radiologist recommendations for follow-up of incidental findings in two situations: (a) when they had no personal experience with a particular finding or (b) when a finding occurred in an unusual clinical context (eg, hemangiomas during pregnancy). In the absence of such recommendations, PCPs had to invest more work to determine how to proceed; one provider stated that this additional work led to “inertia” in acting on the finding. Others relied on their own professional experiences to develop a follow-up algorithm for the management of common incidental findings.
In my own knowledge and experience…there are incidental findings that I am completely oblivious to. “What in the world is that?” “What they are talking about?” “I’ve got to look that up.” And my lack of understanding about what they are saying creates a certain inertia with regards to my discussion with patients about plans. Sometimes that inertia is “look, you know, we should be doing something but I’m not going to recommend it because I just don’t know better,” or “I’ve already set out on a plan and I need to alter the course but I’m not because I don’t know any better.”
Years in practice.—Self-described “junior” PCPs reported that they were likely to order more tests or seek consultation when they received a report containing an incidental finding.
I called the radiologist and asked him to describe them (pulmonary nodules)…better to me…I don’t think it’s cancer, it’s very unlikely to be, but I needed more help to sort that out. I think perhaps being a younger doc I kind of proceeded on a little more (information).
Conversely, senior clinicians reported that they frequently relied on their own ability to review images, citing error rates among radiologists in imaging interpretation.
Provider Characteristics: Professional-Contextual Factors
Follow-up style and philosophy.—PCPs spoke about a follow-up style or approach that determined how they routinely communicated and managed incidental findings, regardless of the clinical need for follow-up. Others reported having no set approach; instead, these individuals tailored follow-up to the clinical need of the individual patient, to their level of confidence regarding the finding, and to the provided differential diagnosis. These PCPs did not feel bound by recommendations in the report.
I always take radiology reports within the context of the system that I work in and understanding that there’s a certain error rate and that a recommendation is a recommendation is a recommendation and that’s that. I’ve also then gotten on the phone with radiologists who say “you have got to do this (follow-up).” And I hear those recommendations within the context of my practice, the context of the relationship I have with the patient, and often the unspoken response, which is “yeah, and one day you should be a primary care doctor and try and understand what these discussions are about.”
Regardless of follow-up style, many PCPs expressed a strong sense of frustration stemming from the “quagmire” of follow-up for incidental findings producing a large financial burden on the health care system. Although these providers believed that the majority of incidental findings were of limited clinical importance, they felt compelled to perform follow-up for a variety of reasons, including low tolerance for ambiguity, lingering uncertainty, institutional or national culture, and fear prompted by outlier reports of malignancy in young patients.
I admit that most times, I think almost all the times, I will then get the follow-up study. Although I sometimes wonder how much we are chasing a ghost that is expensive, but not necessarily going to lead to better outcomes.
Relationship with patient.—PCPs’ individual relationships with patients often informed how and when they disclosed incidental findings to patients or family members as well as their choice of management. Many providers spoke about the role of patient expectations and the importance of knowing how much information their patients wanted or needed. Not surprisingly, the longer their relationship with individual patients, the better PCPs felt they could gauge expectations.
There are patients I would say “this is what we (found) and it’s not clear but sounds like its nothing that important. Do you want additional radiation to just get at the bottom of the problem or should we just follow you clinically?” And then, especially for patients who have a great relationship with you, they really value your (input), and I don’t necessarily often need to order another test…But then when you have people who are doctor shopping…and you don’t have a ton of time with them to build rapport and you’re in a rush. Then the easiest thing is maybe just to order another thing.
Relationship with reporting radiologist.—PCPs’ individual relationships with reporting radiologists also colored their approach to incidental findings. Providers described greater trust in the interpretation of an incidental finding reported by a radiologist they knew. They also claimed to be more likely to reach out to a radiologist they knew personally to discuss the finding.
I’m still relatively new to this institution…In my previous institution (I knew the) radiologists and I was more likely to either call them up directly or curbside them about a report. If I had some level of trust developed I could say “oh yeah I know that radiologist … I trust their reading.”
Some PCPs expressed skepticism regarding follow-up recommendations issued by private practice groups, where there was a perceived financial conflict of interest to perform further imaging.
Patient Characteristics
Predisposing health factors.—PCP communication of incidental findings to patients was often informed by the patient’s clinical context. When a patient was of advanced age, with other comorbid conditions, and had no symptoms referable to the incidental finding, some providers stated that they opted not to disclose the finding due to low pretest probability. Others explained that they routinely shared incidental findings with their patients regardless of patient characteristics, even when they hoped that the patient or family would not opt for further follow-up.
Well, I think the one that immediately comes to mind that I typically will use as a triaging factor will be either the age of the patient, but more importantly, their estimated life expectancy. And so if someone has many chronic illnesses and this is an incidental finding that does not seem to be causing major problems, then, in general, I will discuss it with the patient and hopefully make a decision not to pursue unless it’s causing problems or symptoms.
In contrast, PCPs indicated that they were more likely to pursue follow-up for patients with one or more risk factors for cancer, including personal or family history of cancer, smoking, diabetes, and obesity.
Personal attributes and skills.—Personal patient traits, such as health literacy level, anxiety level, and perceived litigiousness also affected how PCPs communicated incidental findings. For example, providers claimed they were less likely to explain incidental findings to patients with low health literacy than those with high health literacy who were better able to discern the likelihood of false-positive findings. Similarly, providers were more likely to direct treatment decisions for patients with low health literacy and more likely to engage in shared decision making with patients with high health literacy.
And I think that’s a tendency for most patients. If you tell them there’s an abnormality that has a small risk of being cancer, I do not know many patients who would opt not for the additional imaging study….If this patient...was a radiologist, I could see him being able to kind of discern the immense false positivity of the incidental finding. But I don’t think the average patient (understands that likelihood), even when you explain to them that it’s almost assuredly nothing. I think it takes a lot of trust in their doctor to believe that when the radiology specialist is concerned about (the finding).
In addition to patient and family values, higher patient anxiety levels led some PCPs to pursue follow-up for incidental findings and other providers to couch the discovery of incidental findings in benign language.
Even if the radiologist has guidelines and even if the doctor…understand how to manage the incidental finding, there are patients that...feel anxious about an incidental finding and maybe drive your behavior to do something that you normally wouldn’t do.
PCPs were more likely to disclose everything regarding incidental findings of limited clinical importance to patients whom they considered litigious even if they believed the patient could not fully understand the finding.
Social and logistical factors.—PCPs perception of patients’ social and logistical support influenced the disclosure and management of incidental findings. PCPs preferred to have friends or family members in the room as “a second set of ears” when communicating findings and determining follow-up to gauge logistical issues such as transportation. Providers cited insurance coverage, copayments, and related financial issues as important barriers to follow-up for some patients.
Often people with bad social support have bad transportation issues (and) have difficulties with getting a lot of diagnostic tests done. I think that involving as many people as possible with their care is important.
Discussion
In December 2013, the Presidential Commission for the Study of Bioethical Issues outlined the need for research on recipient and practitioner preferences about the discovery, disclosure, and management of incidental and secondary findings (13). The current qualitative analysis describes a breadth of objective and subjective factors influencing PCPs’ communication and management of incidental imaging findings. Some PCPs felt compelled but frustrated to pursue costly testing for imaging findings of limited clinical importance; others said they did not act on imaging findings that were unfamiliar or occurred in an unusual clinical context if no radiologist recommendation was given. A variety of approaches were described by PCPs to communicate and manage incidental findings; some reported a one-size-fits-all style, while others claimed to adapt their approach to the specific patient and finding. These findings suggest that some patients may receive inappropriate follow-up of incidental findings and present an opportunity for radiologists to help PCPs and patients act on the information conveyed in imaging reports.
PCPs who felt compelled to follow up on incidental findings of limited clinical importance cited inexperience, low tolerance for ambiguity, lingering uncertainty, institutional or national culture, patient anxiety, or fear prompted by outlier reports of malignancy in young patients. These factors are known triggers of the cascade effect of medical technology, whereby a domino-like chain of testing is initiated because of one abnormal test result (14,15). Several PCPs discussed the importance of understanding the likelihood of false-positive imaging findings. No PCPs touched on a quantifiable threshold of ambiguity above which follow-up would be pursued; does it make a difference if an incidental imaging finding has a 1%, 10%, or 15% chance of requiring further treatment before follow-up is ordered? The answer will likely vary according to the patient and the PCP and plausibly influences both communication and management of incidental findings.
PCPs said they did not follow up on findings that were unfamiliar or findings that occurred in an unusual clinical context if a radiologist recommendation was not given; the challenges of researching the clinical importance of these findings or seeking specialist consultation led to inaction. Accurate and consistent inclusion of evidence-based recommendations in radiology reports can make follow-up care more consistent with guidelines (16). Evidence-based rather than opinion-based recommendations may help educate providers, patients, and even radiologists on the natural history of incidental findings and the likelihood of false-positive test results. In the appropriate setting, recommendations could state the likelihood of malignancy based on imaging features or when follow-up is not indicated (17). For example, simple renal cysts and indeterminate adnexal masses are frequently detected at unenhanced CT but almost never correspond to malignancy in the asymptomatic population (18,19). Conversely, newly detected renal masses at unenhanced CT have a one in five chance of malignancy (20). The American College of Radiology white papers on the management of incidental imaging findings offer clear algorithms for follow-up based on imaging features, size of the finding, and clinical context of the patient (4,21–24); yet they do not represent evidence-based guidelines. At the same time, there are a number of barriers to achieving the full potential effect of evidence-based imaging recommendations: (a) Data on patient outcomes associated with evidence-based guidelines are scarce, (b) guidelines are not available for all incidental findings, and (c) patient-related factors such as high anxiety levels can supersede guidelines. Research is needed on the optimal wording for follow-up recommendations that alleviate rather than amplify patient and PCP distress. This issue is particularly important given increasing patient access to radiology reports through electronic portals (25,26).
The inconsistent approach described by PCPs to the follow-up of incidental findings is not unique to radiology (7,27,28). PCP characteristics such as follow-up style may sometimes supersede patient characteristics. At other times, patient characteristics such as perceived health literacy may supersede PCP characteristics. Radiologists typically are not aware of each patient’s full clinical context and the unique provider-patient dynamic. However, radiologists could compensate for this lack of information by providing a range of evidence-based treatment options, when available. For example, alternative recommendations could be given for patients with limited and extended life expectancy or for those with low, average, and high disease risk factors (2,4). In addition, the use of qualifying language in recommendations such as “if clinically indicated” may reduce PCPs’ feelings of medicolegal obligation associated with radiologist recommendations (29). It remains to be seen whether such innovations can increase adherence to evidence-based treatment algorithms.
PCPs described greater trust in reports issued by a radiologist they knew personally and were more likely to ask questions of such radiologists. These findings support the value of increased radiologist interaction outside of the Radiology Department. This can be accomplished by placing radiology reading rooms in clinical areas and increasing radiologists’ participation in multidisciplinary conferences. These efforts come at the cost of time, resulting in lower study interpretation volume, and increased likelihood of interruption from referring providers. Justifying these costs may be easier, however, as payment models evolve to reward appropriate health care use rather than simply high volume.
We explored the range of PCP experiences with incidental imaging findings by using a systematic qualitative approach, which limited our sample size because of time and cost. Although we achieved saturation (ie, later interviews did not elicit new information relative to earlier interviews) these data were not quantifiable. There were several limitations to the study. First, direct patient interviews might have revealed other factors relating to patients’ decisions to pursue or not pursue follow-up. Second, this study was conducted at a single academic medical center, which may limit the generalizability of these results.
In conclusion, the communication and management of incidental imaging findings has gained increasing attention among physicians and policy makers because of the frequency with which these findings are detected during routine clinical testing. PCPs feel conflicted about using costly testing for incidental imaging findings of limited clinical importance and may not act on unfamiliar incidental findings when no clear follow-up recommendations are given. A variety of approaches are described by PCPs to communicate and manage incidental findings. Some PCPs report a uniform approach and others claim to adapt their approach to the patient and the finding. Our results suggest that some patients may receive inappropriate follow-up of incidental findings. Further research is needed to determine whether specific changes in radiology reports, such as including evidence-based treatment recommendations for incidental imaging findings, can alleviate patient and PCP distress, enhance communication, increase appropriate imaging use, and improve patient outcomes.
Advances in Knowledge
■ Some primary care providers (PCPs) feel compelled to follow up on incidental imaging findings of limited clinical importance because of inexperience, low tolerance for ambiguity, lingering uncertainty, institutional or national culture, patient anxiety, or fear prompted by outlier reports of malignancy in young patients.
■ PCPs may not follow up incidental imaging findings that are unfamiliar or findings that occur in an unusual clinical context if an explicit recommendation is not provided by the radiologist; the challenges of understanding these findings or seeking specialist consultation may lead to inaction.
■ PCPs describe a variety of approaches to communicating and managing incidental imaging findings; some report a uniform approach and others claim to adapt their approach to the patient and the finding.
■ PCPs state that they are more likely to trust a report issued by and ask questions of a radiologist they know personally.
Implications for Patient Care
■ PCPs value explicit recommendations by radiologists for the follow-up of incidental imaging findings.
■ Some patients may receive inappropriate follow-up of incidental findings in the absence of radiologist recommendations.
■ Radiologist recommendations cannot address all of the factors that influence how PCPs communicate and manage incidental imaging findings.
APPENDIX
Received October 9, 2015; revision requested November 13; revision received February 2, 2016; accepted February 22; final version accepted March 9.
Supported by the National Institutes of Health (1-KM-CA156715-01).
See also the editorial by Thorwarth in this issue.
Disclosures of Conflicts of Interest: H.M.Z. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: grants from the Penn Medicine Center for Innovation and Evidence-based Practice Center-Agency for Healthcare Research and Quality, the Abraham Cancer Center, the Emergency Care Research Institute, and the American College of Radiology. Other relationships: disclosed no relevant relationships. E.K.B. disclosed no relevant relationships. C.P.L. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: board membership, travel reimbursement, and founder’s shares and stock options from Montage Healthcare; medical advisory board membership, travel reimbursement, and honorarium from Elsevier; and medical/technical advisory board membership and stock options from Activate Networks. Other relationships: disclosed no relevant relationships. R.F. disclosed no relevant relationships.
Abbreviation:
- PCP
- primary care provider
References
- 1.Lumbreras B, Donat L, Hernández-Aguado I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol 2010;83(988):276–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005;237(2):395–400. [DOI] [PubMed] [Google Scholar]
- 3.Frates MC, Benson CB, Charboneau JW, et al. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 2005;237(3):794–800. [DOI] [PubMed] [Google Scholar]
- 4.Berland LL, Silverman SG, Gore RM, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 2010;7(10):754–773. [DOI] [PubMed] [Google Scholar]
- 5.Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology 2010;256(3):943–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blagev DP, Lloyd JF, Conner K, et al. Follow-up of incidental pulmonary nodules and the radiology report. J Am Coll Radiol 2014;11(4):378–383. [DOI] [PubMed] [Google Scholar]
- 7.Cho JS, Fulgham P, Clark A, Kavoussi L. Followup imaging after urological imaging studies: comparison of radiologist recommendation and urologist practice. J Urol 2010;184(1):254–257. [DOI] [PubMed] [Google Scholar]
- 8.Lee SI, Saokar A, Dreyer KJ, Weilburg JB, Thrall JH, Hahn PF. Does radiologist recommendation for follow-up with the same imaging modality contribute substantially to high-cost imaging volume? Radiology 2007;242(3):857–864. [DOI] [PubMed] [Google Scholar]
- 9.Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Observations. Chicago, Ill: Aldine, 1967. [Google Scholar]
- 10.Crabtree BF, Miller WL. Doing qualitative research. Research methods for primary care. Newbury Park, Calif: Sage, 1992. [Google Scholar]
- 11.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37(5):360–363. [PubMed] [Google Scholar]
- 12.Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. 4th ed. San Francisco, Calif: Jossey-Bass, 2008. [Google Scholar]
- 13.Presidential Commission for the Study of Bioethical Issues . Anticipate and Communicate: Ethical Management of Incidental and Secondary Findings in the Clinical, Research, and Direct-to-Consumer Contexts. http://bioethics.gov/sites/default/files/FINALAnticipateCommunicate_PCSBI_0.pdf. Published 2013. Accessed May 2, 2016. [DOI] [PubMed]
- 14.Casarella WJ. A patient’s viewpoint on a current controversy. Radiology 2002;224(3):927. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA. Cascade effects of medical technology. Annu Rev Public Health 2002;23:23–44. [DOI] [PubMed] [Google Scholar]
- 16.Elias RM, Knudsen J, Sykes AM, Morgenthaler TI. Impact of a standardized recommendation and electronic prompts on follow-up of indeterminate pulmonary nodules found on computed tomography [abstr]. Am J Respir Crit Care Med 2011;183:A6420. [Google Scholar]
- 17.Berlin L. Pitfalls of the vague radiology report. AJR Am J Roentgenol 2000;174(6):1511–1518. [DOI] [PubMed] [Google Scholar]
- 18.O’Connor SD, Silverman SG, Ip IK, Maehara CK, Khorasani R. Simple cyst-appearing renal masses at unenhanced CT: can they be presumed to be benign? Radiology 2013;269(3):793–800. [DOI] [PubMed] [Google Scholar]
- 19.Pickhardt PJ, Hanson ME. Incidental adnexal masses detected at low-dose unenhanced CT in asymptomatic women age 50 and older: implications for clinical management and ovarian cancer screening. Radiology 2010;257(1):144–150. [DOI] [PubMed] [Google Scholar]
- 20.Wernli KJ, Rutter CM, Dachman AH, Zafar HM. Suspected extracolonic neoplasms detected on CT colonography: literature review and possible outcomes. Acad Radiol 2013;20(6):667–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel MD, Ascher SM, Paspulati RM, et al. Managing incidental findings on abdominal and pelvic CT and MRI, part 1: white paper of the ACR Incidental Findings Committee II on adnexal findings. J Am Coll Radiol 2013;10(9):675–681. [DOI] [PubMed] [Google Scholar]
- 22.Khosa F, Krinsky G, Macari M, Yucel EK, Berland LL. Managing incidental findings on abdominal and pelvic CT and MRI, Part 2: white paper of the ACR Incidental Findings Committee II on vascular findings. J Am Coll Radiol 2013;10(10):789–794. [DOI] [PubMed] [Google Scholar]
- 23.Heller MT, Harisinghani M, Neitlich JD, Yeghiayan P, Berland LL. Managing incidental findings on abdominal and pelvic CT and MRI, part 3: white paper of the ACR Incidental Findings Committee II on splenic and nodal findings. J Am Coll Radiol 2013;10(11):833–839. [DOI] [PubMed] [Google Scholar]
- 24.Sebastian S, Araujo C, Neitlich JD, Berland LL. Managing incidental findings on abdominal and pelvic CT and MRI, Part 4: white paper of the ACR Incidental Findings Committee II on gallbladder and biliary findings. J Am Coll Radiol 2013;10(12):953–956. [DOI] [PubMed] [Google Scholar]
- 25.Joosten EA, DeFuentes-Merillas L, de Weert GH, Sensky T, van der Staak CP, de Jong CA. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom 2008;77(4):219–226. [DOI] [PubMed] [Google Scholar]
- 26.Pickles T, Ruether JD, Weir L, Carlson L, Jakulj F; SCRN Communication Team . Psychosocial barriers to active surveillance for the management of early prostate cancer and a strategy for increased acceptance. BJU Int 2007;100(3):544–551. [DOI] [PubMed] [Google Scholar]
- 27.Baicker K, Buckles KS, Chandra A. Geographic variation in the appropriate use of cesarean delivery. Health Aff (Millwood) 2006;25(5):w355–w367. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, Baicker K, Newhouse JP. Geographic variation in Medicare drug spending. N Engl J Med 2010;363(5):405–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gunn AJ, Sahani DV, Bennett SE, Choy G. Recent measures to improve radiology reporting: perspectives from primary care physicians. J Am Coll Radiol 2013;10(2):122–127. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.