Abstract
Background
Understanding the economic value of health interventions is essential for policy makers to make informed resource allocation decisions. The objective of this systematic review was to summarize available information on the economic impact of children’s surgical care in low- and middle-income countries (LMICs).
Methods
We searched MEDLINE (Pubmed), Embase, and Web of Science for relevant articles published between Jan. 1996 and Jan. 2015. We summarized reported cost information for individual interventions by country, including all costs, disability weights, health outcome measurements (most commonly disability-adjusted life years [DALYs] averted) and cost-effectiveness ratios (CERs). We calculated median CER as well as societal economic benefits (using a human capital approach) by procedure group across all studies. The methodological quality of each article was assessed using the Drummond checklist and the overall quality of evidence was summarized using a scale adapted from the Agency for Healthcare Research and Quality.
Findings
We identified 86 articles that met inclusion criteria, spanning 36 groups of surgical interventions. The procedure group with the lowest median CER was inguinal hernia repair ($15/DALY). The procedure group with the highest median societal economic benefit was neurosurgical procedures ($58,977). We found a wide range of study quality, with only 35% of studies having a Drummond score ≥ 7.
Interpretation
Our findings show that many areas of children’s surgical care are extremely cost-effective in LMICs, provide substantial societal benefits, and are an appropriate target for enhanced investment. Several areas, including inguinal hernia repair, trichiasis surgery, cleft lip and palate repair, circumcision, congenital heart surgery and orthopedic procedures, should be considered “Essential Pediatric Surgical Procedures” as they offer considerable economic value. However, there are major gaps in existing research quality and methodology which limit our current understanding of the economic value of surgical care.
Introduction
Surgically treatable conditions constitute a large portion of the global burden of disease.[1] The consequences of inadequate surgical care in low and middle-income countries (LMICs) are especially dire among children, where many conditions result in lifelong disabilities or premature deaths.[2, 3] In recent years there has been a growing interest in surgery as a global health priority and recognition of its role in a functioning health care system in the World Bank’s Disease Control Priorities in Developing Countries and the Lancet Commission on Global Surgery.[4, 5]
Understanding the economic value of health interventions is essential for policy makers to make resource allocation decisions. Common types of economic evaluation includes cost analysis, which reports the monetary costs per procedure; cost-effectiveness analysis, which relates costs to a standardized health outcome such as infections averted or a quantifiable health metric; cost-benefit analysis, which describes patients’ willingness to pay for a treatment; and societal economic benefit, which quantifies the economic losses that will be reduced for an individual and society as a result of successful treatment of a condition. Cost-effectiveness analyses necessitates the use of health outcome metrics such as the Disability-Adjusted Life Year (DALY), which is a composite measure of years of life lost due to premature mortality and years lived with disability. DALY estimates require several assumptions, most importantly a disability weight (DW), which reflects the severity of a health state and ranges from 0 (perfect health) to 1 (equivalent to death). DALY and DW estimates have been thoroughly summarized in the Global Burden of Disease (GBD) studies and other reports,[6–9] although estimates for surgical care remain problematic for many reasons, such as the large number of diagnoses and procedures, complexity of surgical interventions, and limited number of DWs for conditions requiring surgical intervention[10]
Several recent studies have demonstrated that many areas of surgical care are cost-effective compared with other common health interventions, although these studies do not focus on care of children.[11–13] In this report, we performed a systematic review to describe the economic impact of children’s surgical care in LMICs with three goals: 1) to summarize published research on cost and cost-effectiveness of children’s surgical procedures, 2) to construct a reference table of reported disability weights for conditions requiring surgical procedures, and 3) to describe the societal economic benefit of surgical care for children.
Methods
Selection Criteria
For our systematic review, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines[14] (see S1 Checklist) and registered the study with PROSPERO (registration number: CRD42015016059). Our search encompassed all English-language indexed articles published from January 1996-January 2015 that fulfilled each of the following criteria:
Surgery: studies analyzed surgical procedures, surgical facilities, or missions;
Pediatric population: recipients included children less than 18 years of age;
Economic analysis: studies reported care costs, DALYs averted, life years saved (LYS), quality-adjusted life years (QALYs) saved, health-adjusted life years (HALYs) gained, or societal economic benefit;
LMIC: care performed in a LMIC as defined by the World Bank as of February, 2015;[15]
Data Sources
We conducted a search for eligible studies in MEDLINE (PubMed), Embase, and Web of Science on February 1, 2015. Database-specific indexing terms were used, with the full search listed in S1 Table. We collected additional articles outside the search by consulting experts and reviewing bibliographies of identified studies. We excluded systematic reviews or other non-primary data sources.
Article Selection and Data Extraction
Two researchers (ATS and HER) screened abstracts of identified articles, and considered each full text for inclusion with disagreements settled by discussion. For each included report, we collected intervention type, population, cost, health outcomes, average cost-effectiveness ratio (CER), incremental cost-effectiveness ratio (ICER), and societal economic benefit. If a study did not report costs or health outcomes on a “per procedure” basis, we translated results to this format by dividing total amounts by reported procedure count. Interventions were organized into 36 procedure groups under 8 areas (cardiac surgery, otolaryngology/ear, nose, and throat surgery [ENT], general surgery, neurosurgery, ophthalmology, orthopedics, plastic and reconstructive surgery, and urology). We converted outcomes to 2015 United States dollars (USD) by using PPP conversion factors from the World Bank[16] and the Consumer Price Index Inflation calculator.[17] For studies spanning multiple years, we used the last year reported for conversion.
Article Grading
To assess the quality of each report, we used the 10-point checklist of Drummond.[18] Two observers independently graded each article with disagreements resolved by discussion. To translate individual Drummond scores into a metric that captures overall evidence quality for each of the 36 procedure groups, we adapted a grading scale from the Agency for Healthcare Research and Quality (AHRQ)[19] to reflect overall evidence quality, quantity, and consistency by the following criteria:
High: high level of assurance that research findings are valid; no important disagreement exists across studies; includes at least one study with a Drummond score of 9–10 per procedure type.
Moderate: moderate level of assurance that findings are valid; little disagreement exists across studies; includes at least two studies with a score of 7–8.5 or one study with a score of 9–10 per procedure type.
Low: low level of assurance that findings are valid; category includes studies with conflicting results; less than two studies have scores that exceed 6.5 per procedure type.
Disability Weight Reference Table
A reference table of disability weights for pediatric health conditions commonly requiring surgical procedures was created by compiling values from the GBD studies, with preference given to values reported by GBD 2013,[8] then GBD 2004,[7] and finally Poenaru et al.[20] There were no disability weights identified for cystic echinococcosis, inguinal hernia, or Ponseti clubfoot management in the aforementioned sources, so we reported disability weights published from articles in our review. For circumcision in Sub-Saharan Africa, we calculated a disability weight of 0.028 based on the assumption that a circumcision reduces HIV prevalence from 12% to 6%[21] with an average of 15.5 DALYs/case of HIV averted.[22]
Cost-Effectiveness Assessment
We followed WHO-CHOICE guidelines [23] to assign each intervention into a cost-effectiveness category. Interventions with a maximum CER of less than that country’s gross domestic product (GDP) per capita as defined by the World Bank [24] were considered very cost-effective, interventions with a CER of less than three times the GDP per capita were cost-effective, and all others were not cost-effective. Using the upper and lower bounds of extracted CER (both average and incremental), we summarized the CER values reported from each article in the different procedure groups (using only those articles that used DALY as the health outcome). We also calculated median CERs for each procedure group using minimum and maximum values extracted from all articles that used DALYs as the base health metric. All statistical analyses were performed with STATA v14.1 (StataCorp LP).
Societal Economic Benefit
To determine the societal economic benefit gained from surgical care, we used a human capital approach. This method equates the value of a human life to the discounted market value of the economic output produced by an individual over an expected lifetime, and is frequently used by WHO for cost analyses.[25] For articles that reported economic benefits, we converted results to a “per procedure” basis and reported the minimum and maximum values. For articles without information on societal economic benefit, we calculated this benefit by multiplying reported minimum and maximum DALYs averted, QALYs gained, HALYs gained, or LYS by purchasing power parity (PPP) estimates of gross national income (GNI)/capita from the World Bank.[24] For articles that used DALYs as the health outcome, we summarized the societal economic benefit for each procedure group by presenting the values for each individual intervention within that group, and also reported median values of each procedure.
Results
Literature Search
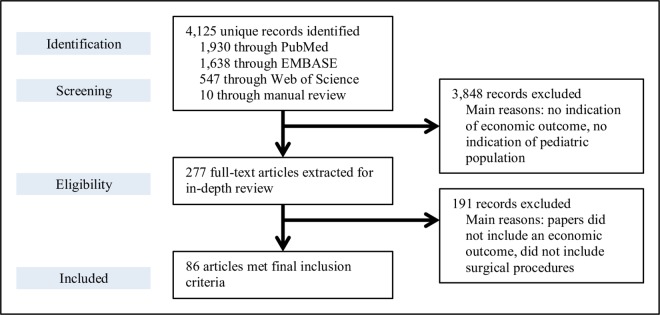
We identified 4,125 articles through our initial search. Altogether, 86 studies met inclusion criteria (Fig 1),[26–111] with articles summarized into 36 different procedure groups.
Fig 1. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram of the literature reviewing process on the economics of pediatric surgery in low- and middle-income countries.
4,125 articles were identified through our initial search, and altogether 86 studies met the full inclusion criteria to be included in our review.
Article Grading and Disability Weights
The studies had a wide range of quality, with 65% of studies (n = 56) with Drummond scores 0–6.5, 19% (n = 16) with scores 7–8.5, and 16% (n = 14) with scores 9–10 (Table 1, individual scores in S2 Table). When summarized by procedure group, six had a high strength of evidence: inguinal hernia repair, trichiasis surgery, circumcision, cleft lip and palate repair, congenital heart defects, and orthopedic procedures. All other interventions had a moderate or low strength of evidence. Disability weights for pediatric surgical conditions identified from the GBD studies [7, 8] and others [20, 38, 72, 97] ranged from 0.005 for finger amputation, to 0.850 for posterior sagittal anorectoplasty (Table 2).
Table 1. Summary of scores using Drummond 10-point checklist and overall strength of evidence for 36 surgical interventions.
| Number of articles in Drummond score rangea: | Strength of Evidenceb | ||||
|---|---|---|---|---|---|
| Intervention category | 0–6.5 | 7–8.5 | 9–10 | Total articles | |
| Cardiac surgery: congenital heart defects [85–94] | 5 | 4 | 1 | 10 | High |
| General Surgery: inguinal hernia repair [29, 35–39] | 2 | 1 | 3 | 6 | High |
| Ophthalmology: trichiasis surgery [54–56] | - | - | 3 | 3 | High |
| Orthopedics: various procedures [44,67–73] | 5 | 2 | 1 | 8 | High |
| PRS: cleft lip & palate [58–65] | 3 | 2 | 1 | 6 | High |
| Urology: circumcision [45–49] | 2 | - | 3 | 5 | High |
| Ophthalmology: cataract repair [56,80–83] | 4 | - | 1 | 5 | Moderate |
| Neurosurgery: hydrocephalus [66] | - | - | 1 | 1 | Moderate |
| Cardiac surgery: mediastinitis treatment [104] | - | 1 | - | 1 | Low |
| ENT: middle ear reconstruction [99] | 1 | - | - | 1 | Low |
| ENT: cochlear implantation [111] | 1 | - | - | 1 | Low |
| ENT: various procedures [44] | 1 | - | - | 1 | Low |
| General Surgery: anorectal reconstruction [28] | 1 | - | - | 1 | Low |
| General Surgery: appendectomy [29–32] | 3 | 1 | - | 4 | Low |
| General Surgery: Buruli ulcer [98] | 1 | - | - | 1 | Low |
| General Surgery: choledochal cyst excision [105] | 1 | - | - | 1 | Low |
| General Surgery: cystic echinococcosis [95–97] | 2 | 1 | - | 3 | Low |
| General Surgery: Hirschsprung’s repair [27] | 1 | - | - | 1 | Low |
| General Surgery: iliopsoas abscess [40] | 1 | - | - | 1 | Low |
| General Surgery: kidney transplantation [106] | 1 | - | - | 1 | Low |
| General Surgery: removal of ureteral stents [110] | 1 | - | - | 1 | Low |
| General Surgery: splenectomy [107, 108] | 1 | 1 | - | 2 | Low |
| General Surgery: various procedures [26,44,50] | 2 | 1 | - | 3 | Low |
| Neurosurgery: epilepsy procedures [78,79] | 2 | - | - | 2 | Low |
| Neurosurgery: frontoethmoidal meningoencephalocoele [51–53] | 3 | - | - | 3 | Low |
| Neurosurgery: various procedures [44,57] | 2 | - | - | 2 | Low |
| Ophthalmology: corneal ulcers [84] | 1 | - | - | 1 | Low |
| Ophthalmology: ocular trauma [42] | 1 | - | - | 1 | Low |
| Ophthalmology: retinopathy of prematurity [109] | - | 1 | - | 1 | Low |
| Orthopedics: amputation [103] | 1 | - | - | 1 | Low |
| Orthopedics: clubfoot treatment [33,34] | 2 | - | - | 2 | Low |
| Orthopedics: leg fractures [74–77] | 3 | 1 | - | 4 | Low |
| PRS: burn treatment [100–103] | 4 | - | - | 4 | Low |
| PRS: various procedures [43,44] | 2 | - | - | 2 | Low |
| Urology: genital reconstruction [41] | 1 | - | - | 1 | Low |
| Urology: various procedures [44] | 1 | - | - | 1 | Low |
Abbreviations include: PRS plastic & reconstructive surgery; ENT ear, nose & throat.
a Articles graded using the Drummond 10-point checklist to assess methodological quality of economic assessments.[18]
b Strength of evidence determined by adapting the Evidence-Based Practice Centers of the Agency for Healthcare Research and Quality grading scale.[19] Ratings were assigned based on the quality, quantity, and consistency of the evidence in the literature.
Table 2. Disability weights for common pediatric surgical conditions.
| Intervention | Disability weighta | Intervention | Disability weighta |
|---|---|---|---|
| Cardiac Surgery | Ophthalmology | ||
| Arterial switch operation [7] | 0.323 | Cataract repair [8] | 0.031 |
| Atrial septal defect [7] | 0.323 | Corneal ulcers [8] | 0.031 |
| Atrioventricular septal defect [7] | 0.323 | Laser treatment for retinopathy of prematurity [8] | |
| Blalock-Taussig shunt [7] | 0.323 | 0.184 | |
| Coarctation of aorta [7] | 0.323 | Ocular trauma [7] | 0.354 |
| Fontan procedure [7] | 0.323 | Trachoma: Blindness [7] | 0.570 |
| Mediastinitis treatment [7] | 0.323 | Trachoma: Low vision [7] | 0.170 |
| Patent ductus arteriosus [7] | 0.323 | Orthopedics | |
| Tetralogy of Fallot [7] | 0.323 | Amputation: arm [8] | 0.079 |
| Totally anomalous pulmonary venous connection [7] | Amputation: thumb [8] | 0.011 | |
| 0.323 | Amputation: finger [8] | 0.005 | |
| Ventricular septal defect [7] | 0.323 | Femoral shaft fractures [8] | 0.042 |
| ENT | Musculoskeletal injuries [8] | 0.079 | |
| Chronic suppurative otitis media: middle ear reconstruction [8] | Open tibial injuries [8] | 0.055 | |
| 0.158 | Pediatric trauma: major surgical treatment [7] | ||
| Cochlear implantation [8] | 0.204 | 0.208 | |
| General Surgery | Pediatric trauma: minor procedures [8] | 0.014 | |
| Appendectomy [7] | 0.463 | Ponseti clubfoot management [72] | 0.231 |
| Buruli ulcer [8] | 0.051 | Various orthopedic injury procedures [8] | |
| Choledochal cyst excision [8] | 0.114 | 0.042 | |
| Cystic echinococcosis [97] | 0.239 | Plastic and Reconstructive Surgery | |
| Drainage of iliopsoas abscess [8] | 0.114 | Burns: superficial [8] | 0.016 |
| Hirschsprung’s repair: transanal endorectal pull-through [20] | Burns: partial thickness [8] | 0.314 | |
| 0.720 | Burns: full thickness [8] | 0.314 | |
| Inguinal hernia repair [38] | 0.300 | Cleft lip [7] | 0.082 |
| Kidney transplantation [8] | 0.547 | Cleft palate [7] | 0.216 |
| Liver transplantation [7] | 0.330 | Neurosurgery | |
| Posterior sagittal anorectoplasty [7] | 0.850 | Epilepsy: anterior temporal lobe lobectomy [8] | |
| Removal of ureteral stents [7] | 0.067 | 0.552 | |
| Splenectomy [8] | 0.114 | Epilepsy: corpus callosotomy [8] | 0.552 |
| Urology | Frontoethmoidal meningoencephalocoele [8] | ||
| Circumcision | 0.028 b | 0.405 | |
| Genital reconstruction [8] | 0.114 | Hydrocephalus [20] | 0.740 |
Abbreviations include: DALY disability-adjusted life years; DW disability weight
GBD Global Burden of Disease study; HIV human immunodeficiency virus.
a Estimated DW values were assigned based on published values, with preference given to long-term over short-term values, and subtracting treated weights from untreated weights whenever both were listed. For conditions with multiple published DWs, preference was first given to the values from GBD 2013 study,[8] followed by the GBD 2004 update,[7] and then Poenaru et al.[20] For conditions without a DW from those sources, values published from other sources were used.
Economic Outcomes
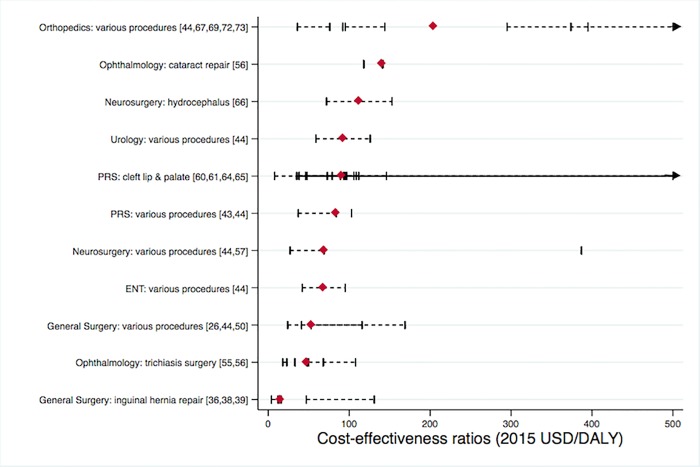
Of the 86 studies in our search, 84 reported cost data (detailed in S3 Table), 24 reported CER, and 2 reported societal economic benefit. In total, 53 procedural CERs were extracted (Table 3). There were 45 of the 53 CERs that reported DALY as the basis of health outcome (of which 36 used average costs and 9 used incremental costs for ICER), 3 reported QALY (2 average, 1 incremental), 3 used life-years saved or gained (2 average, 1 incremental), and 2 reported HALY (1 average, 1 incremental). The procedure with the lowest minimum CER was $4-14/DALY for inguinal hernia repair in Uganda.[39] All interventions were very cost-effective at each country’s GDP level by WHO standards. When summarized by procedure group, there were 12 procedures with CER information using DALYs as the health outcome. Eight of these had a median CER below $100, and 11 had a median CER below $1,000 (Fig 2). Inguinal hernia repair had the lowest median CER ($15), followed by trichiasis surgery ($48). Not shown in Fig 2 was cystic echinococcosis treatment, which had only one observation with a CER of $1,628/DALY.
Table 3. Cost-Effectiveness Ratios of Pediatric Surgical Procedures.
| Intervention | Location | Cost-effectiveness ratio, as reporteda | Unit of outcome | Cost-effectiveness ratio, 2015 USDb | ||
|---|---|---|---|---|---|---|
| Cardiac Surgery | ||||||
| Costa et al (2014) [94] | Atrial septal defects: percutaneous | Brazil | R$976 | QALY, average | $553 | |
| R$230,641 | QALY, incremental | $123,550 | ||||
| Atrial septal defects: surgical | R$631 | QALY, average | $357 | |||
| Ear, Nose & Throat | ||||||
| Wu et al (2013) [44] | Various ENT procedures | Kenya | $42–95 | DALY, average | $44–100 | |
| General Surgery | ||||||
| Jha et al (1998) [29] | Appendectomye | Guinea | $36 | LYS, average | $58 | |
| Inguinal hernia repaire | $74 | LYS, average | $119 | |||
| Gosselin et al (2006) [26] | Various general surgery | Sierra Leone | $33 | DALY, average | $41 | |
| Shillcutt et al (2010) [36] | Inguinal hernia repair | Ghana | $11–15 | DALY, incremental | $12–16 | |
| Wang et al (2012) [97] | Cystic echinococcosis | China | $1,469 | DALY, average | $1,628 | |
| Ilbawi et al (2013) [50] | Various general surgery | Cameroon | $21–147 | DALY, average | $24–169 | |
| Shillcutt et al (2013) [38] | Inguinal hernia repair | Ecuador | $44–123 | DALY, incremental | $47–131 | |
| Wu et al (2013) [44] | Various general surgery | Kenya | $50–110 | DALY, average | $53–116 | |
| Eeson et al (2015) [39] | Inguinal hernia repair | Uganda | $3–12 | DALY, incremental | $4–14 | |
| Neurosurgery | ||||||
| Warf et al (2011) [66] | Hydrocephalus | Uganda | $59–126 | DALY, average | $72–153 | |
| Wu et al (2013) [44] | Various neurological operations | Kenya | $26–65 | DALY, average | $27–69 | |
| Davis et al (2014) [57] | Various neurological operations | Guatemala | $385 | DALY, average | $387 | |
| Ophthalmology | ||||||
| Evans et al (1996) [54] | Trichiasis surgery | Burma | $59 | HALY, average | $107 | |
| $10 | HALY, incremental | $18 | ||||
| Baltussen et al (2005) [55] | Trichiasis surgery | Africa | $13–17 | DALY, average | $18–23 | |
| Americas | $49 | DALY, average | $68 | |||
| Mediterranean | $36–78 | DALY, average | $50–108 | |||
| Southeast Asia | $24 | DALY, average | $33 | |||
| Western Pacific | $35 | DALY, average | $48 | |||
| Baltussen et al (2012) [56] | Trichiasis surgery | Sub-Saharan Africa | $71–189 | DALY, incremental | $86–230 | |
| Trichiasis surgery | $71–90 | DALY, average | $86–110 | |||
| Cataract repair | $116–117 | DALY, incremental | $141–142 | |||
| Cataract repair | $116 | DALY, average | $141 | |||
| Trichiasis surgery | Southeast Asia | $285–849 | DALY, incremental | $347–1,034 | ||
| Trichiasis surgery | $285–374 | DALY, average | $347–455 | |||
| Cataract repair | $97 | DALY, incremental | $118 | |||
| Cataract repair | $97 | DALY, average | $118 | |||
| Orthopedics | ||||||
| Grimes et al (2014) [67] | Various orthopedic procedures | Malawi | $92–139 | DALY, average | $95–144 | |
| Gosselin et al (2008) [69] | Various orthopedic procedures | Cambodia | $77 | DALY, average | $92 | |
| Gosselin et al (2011) [72] | Various orthopedic procedures | Nicaragua | $362 | DALY, average | $395 | |
| Dominican Repub. | $362 | DALY, average | $395 | |||
| Haiti | $343 | DALY, average | $374 | |||
| Chen et al (2012) [73] | Various orthopedic procedures | Nicaragua | $270–719 | DALY, incremental | $295–787 | |
| Wu et al (2013) [44] | Various orthopedic procedures | Kenya | $34–72 | DALY, average | $36–76 | |
| Plastic and Reconstructive Surgery | ||||||
| Corlew (2010) [60] | Cleft lip & palate | Nepal | $29–73 | DALY, average | $35–89 | |
| Magee Jr. et al (2010) [61] | Cleft lip & palate | Vietnam | $7–850 | DALY, average | $8–939 | |
| Nicaragua | $66–1,828 | DALY, average | $73–2,019 | |||
| Kenya | $96–1,193 | DALY, average | $106–1,318 | |||
| Moon et al (2012) [64] | Cleft lip & palate | Vietnam | $43–97 | DALY, average | $47–106 | |
| Poenaru (2013) [65] | Cleft lip & palate | Africa | $72–134 | DALY, average | $79–146 | |
| Americas | $35–85 | DALY, average | $38–93 | |||
| Europe | $35–89 | DALY, average | $38–97 | |||
| Middle East | $42–100 | DALY, average | $46–109 | |||
| Southeast Asia | $44–102 | DALY, average | $48–112 | |||
| Western Pacific | $35–87 | DALY, average | $38–95 | |||
| Rattray et al (2013) [43] | Various reconstructive procedures | Cambodia | $99 | DALY, average | $103 | |
| Wu et al (2013) [44] | Various reconstructive procedures | Kenya | $35–79 | DALY, average | $37–84 | |
| Urology | ||||||
| Binagwaho et al (2010) [45] | Circumcision | Rwanda | $334 | LYG, incremental | $370 | |
| Wu et al (2013) [44] | Various urologic operations | Kenya | $56–119 | DALY, average | $59–126 | |
Abbreviations include: DALY disability-adjusted life-year; LYS life-year saved; LYG life-years gained; HALY health-adjusted life-year; QALY quality-adjusted life-year; USD United States dollar; Int. $ International dollars (a hypothetical currency unit with the same purchasing power parity that the U.S. dollar has in the United States at a given time).
a All values presented on a per-procedure basis.
Fig 2. Cost-effectiveness (2015 USD/DALY) of 11 pediatric surgical intervention categories.
Individual article references shown in brackets. Red diamonds represent median costs, black lines represent the range of values from each article. Abbreviations include: ENT ear, nose and throat; PRS plastic and reconstructive surgery; DALY disability-adjusted life year; USD United States dollar.
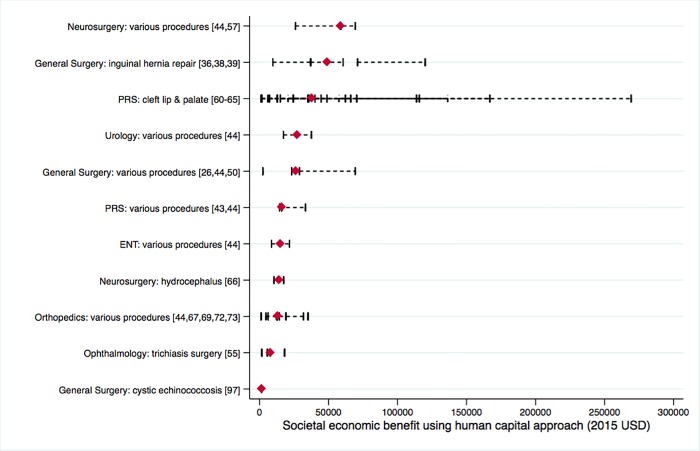
Many procedures were clinically effective as measured by averted DALYs, and most showed a substantial societal economic benefit (detailed in S4 Table). The intervention with the highest societal economic benefit was atrial septal defect repair in Brazil ($313,866). When summarized by procedure group, we were able to extract or calculate societal economic impact for 11 types of procedures based on articles that used DALYs as the health outcome. There were 9 out of those 11 procedure groups that had a median benefit greater than $10,000/procedure (Fig 3). Various neurosurgical procedures had the highest median economic benefit ($58,977), followed by inguinal hernia repair ($48,864).
Fig 3. Societal economic benefit of 11 pediatric surgical intervention categories, measured using a human capital approach.
Individual article references shown in brackets. Red diamonds represent median values, black bars represent the range of values from each article. Abbreviations include: ENT ear, nose and throat; PRS plastic and reconstructive surgery; USD United States dollars.
Discussion
Our review demonstrates that many areas of children’s surgical care in LMICs provide considerable economic value. These findings confirm the work of the Lancet Commission on Global Surgery and others, and suggest that surgical care is a valuable investment and should be incorporated as an essential component of a functioning health care system. Although we have reviewed the largest set of existing reports of children’s surgical care in LMICs, the limited range of economic analyses suggests that we have just examined the “tip of the iceberg” of pediatric surgical conditions.
As health care for children grows as a global health priority, this information should assist policy-makers for the development of funding priorities. However, as Baltussen et al. note, economic analyses should be used collectively with other criteria such as poverty reduction and severity of disease for a comprehensive approach to health care priority setting.[112] Use of a rights-based approach will ensure that a procedure that does not have a favorable cost-effectiveness or one that lacks adequate economic analysis is not excluded in provision of basic children’s health care services. Children’s surgical care should be thought of as an essential component of a “package of care,” as surgical care is an essential modality for the overall health care of children. Economic information should be taken into context by all local stakeholders, as local experts best understand the economic constraints within individual countries and the optimal methods to affect health care change.
Several particular areas of surgical care for children offer great economic value and are supported by high quality evidence. These should be considered as “Essential Children’s Surgical Procedures,” and include inguinal hernia repair, trichiasis surgery, cleft lip and palate repair, circumcision, congenital heart surgery, and orthopedic procedures. Our recommendations align with those of Mock et al.,[113] which prioritize surgical care based on health burden, success of a surgical intervention, and cost-effectiveness. We strongly advocate for increased investment in these “Essential Children’s Surgical Procedures” to improve health for children and gain economic benefit for a society. Many other procedures may potentially be quite cost-effective, although the quality of economic analysis is not as well developed, such as for Hirschsprung’s disease, anorectal reconstruction, appendectomy, clubfoot, abscess, meningoencephalocoele, trauma, hydrocephalus, epilepsy, and cataracts. Although our study strived to incorporate all available economic data on children’s surgical care, many areas still lack adequate economic analysis to make clear recommendations. For instance, we did not identify any economic studies for care of undescended testicles, typhoid perforation or intussusception. Although issues surrounding capacity and delivery of children’s surgical care are not addressed in our review, some procedures may be more appropriate for care and offer maximal economic benefits within different levels of a health system (i.e. district hospital, tertiary center).[114] Furthermore, innovative solutions such as task-sharing of surgical tasks to non-physician healthcare workers may be vital to maximize the economic value of surgical care for children.[115]
Moving forward, we encourage improvements in research methods to define the costs and value of surgical care. First, we advocate for refinement of the use of the DALY, DWs, and other output metrics for economic analysis of surgical treatments. Although a complete discussion of the limitations of the DALY and DW metrics for surgical care is beyond the scope of this review, they remains problematic for many reasons, such as the complexity of surgical care and procedures, identification of surgical component of care for health states requiring multidisciplinary care, or impact of surgical complications on health state outcomes.[10] Second, we support consistent use of WHO guidelines that define appropriate costs for economic analyses, which should reflect all customary costs for care in a public hospital setting, including infrastructure (capital costs, maintenance and utility costs, management overhead) and staff salaries, as well as indirect costs such as for travel or lost wages.[23] Third, we encourage the use of national datasets as they become available for economic analyses, such that variation between hospitals or researchers is minimized.
Existing disability weights incorporated into DALY estimates have been widely criticized for producing seemingly unrealistic values and have garnered concern regarding universal valuation for people from different geographic, cultural, or socioeconomic backgrounds.[116] Alternative measures of characterizing health states and the burden of conditions amenable to surgery include the epidemiological modeling strategy of Higashi et al.[117] Their model utilized inputs from GBD data to characterize the DALYs from congenital anomalies that could be potentially addressable from surgical intervention in LMIC, thereby estimating the excessive morbidity and mortality associated with these conditions. Coupling novel modeling strategies to enhance DALY estimations with comprehensive cost data will markedly improve economic analyses and facilitate scale-up modeling to help guide policy to improve surgical infrastructure.
Our study has several limitations inherent to economic analyses, including dependence on a wide range of assumptions as well as limited granularity of input data. Many articles report evidence from surgical missions and non-governmental organizations, which tend to underestimate or omit critical costs such as use of the facility, equipment depreciation, and overhead.[13] Also, the cost-effectiveness of an operation will vary by location and type of facility.[13] For example, costs associated with a surgical mission may be very different from a second-level hospital. Although all costs and CERs were converted and inflated to 2015 USD for consistency, our review included a wide timeframe stretching back to 1998, and some of the procedures described here may be outdated and no longer considered standard of care. Furthermore, many of the studies use different methods for age-weighting and discounting, which can impact the cost-effectiveness of a procedure. Some have argued that these practices are not appropriate,[118] and they have been subsequently omitted from the GBD 2010 study. Finally, we recognize limitations in assessment of the quality of surgical studies using the Drummond checklist, which is increasingly used for comparison of economic analyses across different health settings. Several items of the Drummond checklist are difficult to apply towards surgical care as noted by Marseille and Morshed,[119] such as reliance on the equal weighting of all criteria elements. However, the final score does allow for general comparison between studies. By translating quality assessments into “high, medium, or low” categories using AHRQ guidelines, we sought to translate these findings into commonly used categories.
Many of the CERs presented here from LMICs were based on average cost-effectiveness, which is most appropriate for scenarios where performing the intervention and doing nothing are the only options. This metric does not reflect the availability of alternate options with intermediate cost and effectiveness, and are problematic when comparing different treatments.[120] Analyses using ICERs would be needed to compare interventions that are mutually exclusive. In our analyses, all but one study used standard of usual care as the comparator for ICER calculations. However, ICERs are often not generalizable across different settings, because the “next best alternative” might vary by location. Thus, the results presented here are not intended to be used as an absolute standard for comparison between procedures, but rather to define a pattern from existing data to describe the economic benefits of pediatric surgical interventions in LMICs.
In summary, we found that many areas of surgical care for children are quite cost-effective and result in substantial economic benefits for LMICs. However, there are major gaps in existing research methodology which limit our understanding of the actual value of pediatric surgical care. Despite these limitations, it is clear that improved investment in surgical care in many setting is an extremely cost-effective approach to support health care for children, and should be considered as a key component of “packages of care” for children.
Supporting Information
(DOC)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
Research support was provided to ATS by Megan Von Isenburg, Duke University Medical Center Library.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Shrime MG, Bickler SW, Alkire BC, Mock C. Global burden of surgical disease: an estimation from the provider perspective. Lancet Glob Health. 2015;3 (Suppl. 2):S8–9. Epub 2015/05/01. 10.1016/s2214-109x(14)70384-5 . [DOI] [PubMed] [Google Scholar]
- 2.Bickler SW, Rode H. Surgical services for children in developing countries. Bull World Health Organ. 2002;80(10):829–35. Epub 2002/12/10. ; PubMed Central PMCID: PMCPmc2567648. [PMC free article] [PubMed] [Google Scholar]
- 3.Belli PC, Bustreo F, Preker A. Investing in children's health: what are the economic benefits? Bull World Health Organ. 2005;83(10):777–84. Epub 2005/11/12. ; PubMed Central PMCID: PMCPmc2626422. doi: /S0042-96862005001000015 [PMC free article] [PubMed] [Google Scholar]
- 4.Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN. Essential Surgery Disease Control Priorities, third edition, volume 1 Washington, DC: The World Bank; 2015. [PubMed] [Google Scholar]
- 5.Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015. Epub 2015/05/01. 10.1016/s0140-6736(15)60160-x . [DOI] [PubMed] [Google Scholar]
- 6.Murray C, Lopez A. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020 Harvard University Press; 1996. [Google Scholar]
- 7.World Health Organization. The global burden of disease: 2004 update. Available: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/. Accessed 11 August 2015.
- 8.Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 2015;3(11):e712–23. Epub 2015/10/18. 10.1016/s2214-109x(15)00069-8 . [DOI] [PubMed] [Google Scholar]
- 9.Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2129–43. Epub 2012/12/19. 10.1016/s0140-6736(12)61680-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bickler S, Ozgediz D, Gosselin R, Weiser T, Spiegel D, Hsia R, et al. Key concepts for estimating the burden of surgical conditions and the unmet need for surgical care. World J Surg. 2010;34(3):374–80. Epub 2009/10/29. 10.1007/s00268-009-0261-6 ; PubMed Central PMCID: PMCPmc2816802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grimes CE, Henry JA, Maraka J, Mkandawire NC, Cotton M. Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg. 2014;38(1):252–63. Epub 2013/10/09. 10.1007/s00268-013-2243-y . [DOI] [PubMed] [Google Scholar]
- 12.Chao TE, Sharma K, Mandigo M, Hagander L, Resch SC, Weiser TG, et al. Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health. 2014;2(6):e334–45. Epub 2014/08/12. 10.1016/s2214-109x(14)70213-x . [DOI] [PubMed] [Google Scholar]
- 13.Prinja S, Nandi A, Horton S, Levin C, Laxminarayan R. Costs, effectiveness, and cost-effectiveness of selected surgical procedures and platforms In Essential Surgery. Disease Control Priorities, third edition, volume 1 Washington, D.C.: The World Bank; 2015. pp. 317–38. [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. Epub 2010/02/23. 10.1016/j.ijsu.2010.02.007 . [DOI] [PubMed] [Google Scholar]
- 15.The World Bank. Country and Lending Groups 2015. Available: http://data.worldbank.org/about/country-and-lending-groups. Available 1 February 2015.
- 16.The World Bank. PPP conversion factor, GDP (LCU per international $) 2016. Available: http://data.worldbank.org/indicator/PA.NUS.PPP. Accessed 30 January 2016.
- 17.United States Department of Labor. CPI Inflation Calculator 2015 [Jul 7, 2015)]. Available: http://www.bls.gov/data/inflation_calculator.htm. Accessed 7 July 2015.
- 18.Drummond M. Methods for the economic evaluation of health care programmes 3rd edn. Oxford medical publications. Oxford; New York: Oxford University Press; 2005. [Google Scholar]
- 19.Owens DK, Lohr KN, Atkins D, Treadwell JR, Reston JT, Bass EB, et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—agency for healthcare research and quality and the effective health-care program. J Clin Epidemiol. 2010;63(5):513–23. Epub 2009/07/15. 10.1016/j.jclinepi.2009.03.009 . [DOI] [PubMed] [Google Scholar]
- 20.Poenaru D, Pemberton J, Frankfurter C, Cameron BH. Quantifying the disability from congenital anomalies averted through pediatric surgery: a cross-sectional comparison of a pediatric surgical unit in Kenya and Canada. World J Surg. 2015;39(9):2198–206. Epub 2015/06/04. 10.1007/s00268-015-3103-8 . [DOI] [PubMed] [Google Scholar]
- 21.Londish GJ, Murray JM. Significant reduction in HIV prevalence according to male circumcision intervention in sub-Saharan Africa. Int J Epidemiol. 2008;37(6):1246–53. Epub 2008/03/05. 10.1093/ije/dyn038 . [DOI] [PubMed] [Google Scholar]
- 22.Uthman OA, Popoola TA, Yahaya I, Uthman MM, Aremu O. The cost-utility analysis of adult male circumcision for prevention of heterosexual acquisition of HIV in men in sub-Saharan Africa: a probabilistic decision model. Value Health. 2011;14(1):70–9. Epub 2011/01/08. 10.1016/j.jval.2010.10.011 . [DOI] [PubMed] [Google Scholar]
- 23.Edejer TT-T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, et al. WHO guide to cost-effectiveness analysis Geneva: World Health Organization; 2003. [Google Scholar]
- 24.The World Bank. World Bank Development Indicators. Available: http://databank.worldbank.org/data/reports.aspx?source=world-development-indicators. Accessed 12 August 2015.
- 25.Sachs JD. Macroeconomics and health: investing in health for economic development Report of the Commission on Macroeconomics and Health. Geneva: World Health Organization; 2001. [Google Scholar]
- 26.Gosselin RA, Thind A, Bellardinelli A. Cost/DALY averted in a small hospital in Sierra Leone: what is the relative contribution of different services? World J Surg. 2006;30(4):505–11. Epub 2006/03/11. 10.1007/s00268-005-0609-5 . [DOI] [PubMed] [Google Scholar]
- 27.Pratap A, Chandra Shakya V, Kumar Biswas B, Sinha A, Tiwari A, Shekhar Agrawal C, et al. Single-stage transanal endorectal pull-through for Hirschsprung's disease: perspective from a developing country. J Pediatr Surg. 2007;42(3):532–5. 10.1016/j.jpedsurg.2006.10.049 [DOI] [PubMed] [Google Scholar]
- 28.Gangopadhyay AN, Chooramani Gopal S, Sharma S, Gupta DK, Sharma SP, Vittal Mohan T. Management of anorectal malformations in Varanasi, India: A long-term review of single and three stage procedures. Pediatr Surg Int. 2006;22(2):169–72. 10.1007/s00383-005-1567-6 [DOI] [PubMed] [Google Scholar]
- 29.Jha P, Bangoura O, Ranson K. The cost-effectiveness of forty health interventions in Guinea. Health Policy Plan. 1998;13(3):249–62. Epub 1998/08/05. . [DOI] [PubMed] [Google Scholar]
- 30.Paudel RK, Jain BK, Rani S, Gupta SK, Niraula SR. Acute appendicitis: a quality assurance study. Trop Gastroenterol. 2003;24(2):83–6. Epub 2003/11/08. . [PubMed] [Google Scholar]
- 31.Utpal D. Laparoscopic versus open appendectomy in West Bengal, India. Chin J Dig Dis. 2005;6(4):165–9. Epub 2005/10/26. 10.1111/j.1443-9573.2005.00225.x . [DOI] [PubMed] [Google Scholar]
- 32.Wu K, Yang L, Wu A, Wang J, Xu S, Zhao H, et al. Single-site laparoscopic appendectomy in children using conventional instruments: a prospective, randomized, control trial. Pediatr Surg Int. 2014. [DOI] [PubMed] [Google Scholar]
- 33.Adegbehingbe OO, Oginni LM, Ogundele OJ, Ariyibi AL, Abiola PO, Ojo OD. Ponseti clubfoot management: changing surgical trends in Nigeria. Iowa Orthop J. 2010;30:7–14. Epub 2010/11/04. ; PubMed Central PMCID: PMCPmc2958264. [PMC free article] [PubMed] [Google Scholar]
- 34.Perveen R, Evans AM, Ford-Powell V, Dietz FR, Barker S, Wade PW, et al. The Bangladesh clubfoot project: Audit of 2-year outcomes of ponseti treatment in 400 children. Journal of Pediatric Orthopaedics. 2014. [DOI] [PubMed] [Google Scholar]
- 35.Osuigwe A, Ekwunife CN, Ihekowba CH. Use of prophylactic antibiotics in a paediatric day-case surgery at NAUTH, Nnewi, Nigeria: A randomized double-blinded study. Trop Doct. 2006;36(1):42–4. 10.1258/004947506775598833 . [DOI] [PubMed] [Google Scholar]
- 36.Shillcutt SD, Clarke MG, Kingsnorth AN. Cost-effectiveness of groin hernia surgery in the Western Region of Ghana. Arch Surg. 2010;145(10):954–61. Epub 2010/10/20. 10.1001/archsurg.2010.208 . [DOI] [PubMed] [Google Scholar]
- 37.Banu T, Chowdhury TK, Kabir M, Talukder R, Lakhoo K. Bringing surgery to rural children: Chittagong, Bangladesh experience. World J Surg. 2013;37(4):730–6. Epub 2013/02/06. 10.1007/s00268-013-1916-x . [DOI] [PubMed] [Google Scholar]
- 38.Shillcutt SD, Sanders DL, Teresa Butron-Vila M, Kingsnorth AN. Cost-effectiveness of inguinal hernia surgery in northwestern Ecuador. World J Surg. 2013;37(1):32–41. Epub 2012/10/18. 10.1007/s00268-012-1808-5 . [DOI] [PubMed] [Google Scholar]
- 39.Eeson G, Birabwa-Male D, Pennington M, Blair GK. Costs and cost-effectiveness of pediatric inguinal hernia repair in Uganda. World J Surg. 2015;39(2):343–9. Epub 2014/10/02. 10.1007/s00268-014-2818-2 . [DOI] [PubMed] [Google Scholar]
- 40.Afaq A, Jain BK, Dargan P, Bhattacharya SK, Rauniyar RK, Kukreti R. Surgical drainage of primary iliopsoas abscess—Safe and cost-effective treatment. Trop Doct. 2002;32(3):133–5. [DOI] [PubMed] [Google Scholar]
- 41.Ekenze SO, Ezegwui HU, Adiri CO. Genital lesions complicating female genital cutting in infancy: a hospital-based study in south-east Nigeria. Ann Trop Paediatr. 2007;27(4):285–90. Epub 2007/12/07. 10.1179/146532807x245670 . [DOI] [PubMed] [Google Scholar]
- 42.Murithi I, Gichuhi S, Njuguna MW. Ocular injuries in children. East Afr Med J. 2008;85(1):39–45. Epub 2008/06/12. . [DOI] [PubMed] [Google Scholar]
- 43.Rattray KW, Harrop TC, Aird J, Tam T, Beveridge M, Gollogly JG. The cost effectiveness of reconstructive surgery Cambodia. Asian Biomedicine. 2013;7(3):319–24. 10.5372/1905-7415.0703.182 . [DOI] [Google Scholar]
- 44.Wu VK, Poenaru D. Burden of surgically correctable disabilities among children in the Dadaab Refugee Camp. World J Surg. 2013;37(7):1536–43. Epub 2013/01/04. 10.1007/s00268-012-1899-z . [DOI] [PubMed] [Google Scholar]
- 45.Binagwaho A, Pegurri E, Muita J, Bertozzi S. Male circumcision at different ages in Rwanda: a cost-effectiveness study. PLoS Med. 2010;7(1):e1000211 Epub 2010/01/26. 10.1371/journal.pmed.1000211 ; PubMed Central PMCID: PMCPmc2808207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manji KP. Circumcision of the young infant in a developing country using the Plastibell(TM). Ann Trop Paediatr. 2000;20(2):101–4. [DOI] [PubMed] [Google Scholar]
- 47.Gray RH, Li X, Kigozi G, Serwadda D, Nalugoda F, Watya S, et al. The impact of male circumcision on HIV incidence and cost per infection prevented: a stochastic simulation model from Rakai, Uganda. AIDS. 2007;21(7):845–50. Epub 2007/04/07. 10.1097/QAD.0b013e3280187544 . [DOI] [PubMed] [Google Scholar]
- 48.Njeuhmeli E, Forsythe S, Reed J, Opuni M, Bollinger L, Heard N, et al. Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS Med. 2011;8(11):e1001132 Epub 2011/12/06. 10.1371/journal.pmed.1001132 ; PubMed Central PMCID: PMCPmc3226464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tumwesigyea NM, Wabwire-Mangena F, Bagendaa D, Ssengoobab F, Opioc A, Nalwaddab CK, et al. Modelling the potential impact and cost of scaling-up male circumcision in resource poor settings: A case of Uganda. African Journal of AIDS Research. 2013;12(1):61–9. 10.2989/16085906.2013.815416 [DOI] [PubMed] [Google Scholar]
- 50.Ilbawi AM, Einterz EM, Nkusu D. Obstacles to surgical services in a rural Cameroonian district hospital. World J Surg. 2013;37(6):1208–15. Epub 2013/03/07. 10.1007/s00268-013-1977-x . [DOI] [PubMed] [Google Scholar]
- 51.Roux FE, Lauwers F, Oucheng N, Say B, Joly B, Gollogly J. Treatment of frontoethmoidal meningoencephalocele in Cambodia: a low-cost procedure for developing countries. J Neurosurg. 2007;107(1 Suppl):11–21. Epub 2007/07/25. 10.3171/ped-07/07/011 . [DOI] [PubMed] [Google Scholar]
- 52.Gollogly J, Oucheng N, Lauer G, Pinzer T, Lauwers F, Roux FE, et al. Frontoethmoidal meningoencephalocoele repair in Cambodia: outcomes and cost comparisons. Trop Doct. 2008;38(3):167–70. Epub 2008/07/17. 10.1258/td.2007.070124 . [DOI] [PubMed] [Google Scholar]
- 53.Oucheng N, Lauwers F, Gollogly J, Draper L, Joly B, Roux FE. Frontoethmoidal meningoencephalocele: appraisal of 200 operated cases. J Neurosurg Pediatr. 2010;6(6):541–9. Epub 2010/12/03. 10.3171/2010.9.peds1043 . [DOI] [PubMed] [Google Scholar]
- 54.Evans TG, Ranson MK, Kyaw TA, Ko CK. Cost effectiveness and cost utility of preventing trachomatous visual impairment: lessons from 30 years of trachoma control in Burma. Br J Ophthalmol. 1996;80(10):880–9. Epub 1996/10/01. ; PubMed Central PMCID: PMCPmc505642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baltussen R, Sylla M, Frick KD, Mariotti SR. Cost-effectiveness of trachoma control in seven world regions. Ophthalmic Epidemiol. 2005;12(2):91–101. 10.1080/09286580490932761 . [DOI] [PubMed] [Google Scholar]
- 56.Baltussen R, Smith A. Cost effectiveness of strategies to combat vision and hearing loss in sub-Saharan Africa and South East Asia: mathematical modelling study. Br Med J. 2012;344 10.1136/bmj.e615 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davis MC, Than KD, Garton HJ. Cost effectiveness of a short-term pediatric neurosurgical brigade to guatemala. World Neurosurg. 2014;82(6):974–9. Epub 2014/08/26. 10.1016/j.wneu.2014.08.038 . [DOI] [PubMed] [Google Scholar]
- 58.Hodges AM, Hodges SC. A rural cleft project in Uganda. Br J Plast Surg. 2000;53(1):7–11. Epub 2000/02/05. 10.1054/bjps.1999.3238 . [DOI] [PubMed] [Google Scholar]
- 59.Tollefson TT, Wong JK, Sykes JM, Larrabee WF Jr. Cleft lip-palate deformities in western China: Epidemiology, surgical reconstruction, and cost. Arch Facial Plast Surg. 2006;8(4):234–9. 10.1001/archfaci.8.4.234 [DOI] [PubMed] [Google Scholar]
- 60.Corlew DS. Estimation of impact of surgical disease through economic modeling of cleft lip and palate care. World J Surg. 2010;34(3):391–6. Epub 2009/08/25. 10.1007/s00268-009-0198-9 . [DOI] [PubMed] [Google Scholar]
- 61.Magee WP Jr., Vander Burg R, Hatcher KW. Cleft lip and palate as a cost-effective health care treatment in the developing world. World J Surg. 2010;34(3):420–7. Epub 2010/01/12. 10.1007/s00268-009-0333-7 . [DOI] [PubMed] [Google Scholar]
- 62.Alkire B, Hughes CD, Nash K, Vincent JR, Meara JG. Potential economic benefit of cleft lip and palate repair in sub-Saharan Africa. World J Surg. 2011;35(6):1194–201. Epub 2011/03/25. 10.1007/s00268-011-1055-1 . [DOI] [PubMed] [Google Scholar]
- 63.Hughes CD, Babigian A, McCormack S, Alkire BC, Wong A, Pap SA, et al. The clinical and economic impact of a sustained program in global plastic surgery: valuing cleft care in resource-poor settings. Plast Reconstr Surg. 2012;130(1):87e–94e. Epub 2012/06/30. 10.1097/PRS.0b013e318254b2a2 . [DOI] [PubMed] [Google Scholar]
- 64.Moon W, Perry H, Baek RM. Is international volunteer surgery for cleft lip and cleft palate a cost-effective and justifiable intervention? A case study from East Asia. World J Surg. 2012;36(12):2819–30. Epub 2012/09/19. 10.1007/s00268-012-1761-3 . [DOI] [PubMed] [Google Scholar]
- 65.Poenaru D. Getting the job done: analysis of the impact and effectiveness of the SmileTrain program in alleviating the global burden of cleft disease. World J Surg. 2013;37(7):1562–70. Epub 2012/12/13. 10.1007/s00268-012-1876-6 . [DOI] [PubMed] [Google Scholar]
- 66.Warf BC, Alkire BC, Bhai S, Hughes C, Schiff SJ, Vincent JR, et al. Costs and benefits of neurosurgical intervention for infant hydrocephalus in sub-Saharan Africa: Clinical article. J Neurosurg Pediatr. 2011;8(5):509–21. 10.3171/2011.8.PEDS11163 [DOI] [PubMed] [Google Scholar]
- 67.Grimes CE, Mkandawire NC, Billingsley ML, Ngulube C, Cobey JC. The cost-effectiveness of orthopaedic clinical officers in Malawi. Trop Doct. 2014;44(3):128–34. 10.1177/0049475514535575 [DOI] [PubMed] [Google Scholar]
- 68.Gurses D, Sarioglu-Buke A, Baskan M, Kilic I. Cost factors in pediatric trauma. Can J Surg. 2003;46(6):441–5. Epub 2003/12/19. ; PubMed Central PMCID: PMCPmc3211766. [PMC free article] [PubMed] [Google Scholar]
- 69.Gosselin RA, Heitto M. Cost-effectiveness of a district trauma hospital in Battambang, Cambodia. World J Surg. 2008;32(11):2450–3. Epub 2008/08/22. 10.1007/s00268-008-9708-4 . [DOI] [PubMed] [Google Scholar]
- 70.Dada A, Giwa SO, Yinusa W, Ugbeye M, Gbadegesin S. Complications of treatment of musculoskeletal injuries by bone setters. West Afr J Med. 2009;28(1):43–7. Epub 2009/08/11. . [DOI] [PubMed] [Google Scholar]
- 71.Reddy GM, Negandhi H, Singh D, Singh AJ. Extent and determinants of cost of road traffic injuries in an Indian city. Indian J Med Sci. 2009;63(12):549–56. Epub 2010/02/18. 10.4103/0019-5359.59988 . [DOI] [PubMed] [Google Scholar]
- 72.Gosselin RA, Gialamas G, Atkin DM. Comparing the cost-effectiveness of short orthopedic missions in elective and relief situations in developing countries. World J Surg. 2011;35(5):951–5. Epub 2011/02/26. 10.1007/s00268-010-0947-9 ; PubMed Central PMCID: PMCPmc3071471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen AT, Pedtke A, Kobs JK, Edwards GS Jr., Coughlin RR, Gosselin RA. Volunteer orthopedic surgical trips in Nicaragua: a cost-effectiveness evaluation. World J Surg. 2012;36(12):2802–8. Epub 2012/07/11. 10.1007/s00268-012-1702-1 . [DOI] [PubMed] [Google Scholar]
- 74.Padhi NR, Padhi P. Use of external fixators for open tibial injuries in the rural third world: panacea of the poor? Injury. 2007;38(2):150–9. Epub 2006/12/05. 10.1016/j.injury.2006.08.053 . [DOI] [PubMed] [Google Scholar]
- 75.Gosselin RA, Heitto M, Zirkle L. Cost-effectiveness of replacing skeletal traction by interlocked intramedullary nailing for femoral shaft fractures in a provincial trauma hospital in Cambodia. Int Orthop. 2009;33(5):1445–8. Epub 2009/05/14. 10.1007/s00264-009-0798-x ; PubMed Central PMCID: PMCPmc2899146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hsu AR, Diaz HM, Penaranda NRP, Cui HD, Evangelista RHA, Rinsky L, et al. Dynamic skeletal traction spica casts for paediatric femoral fractures in a resource-limited setting. Int Orthop. 2009;33(3):765–71. 10.1007/s00264-008-0621-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Akinyoola AL, Orekha OO, Taiwo FO, Odunsi AO. Outcome of non-operative management of femoral shaft fractures in children. Afr J Paediatr Surg. 2011;8(1):34–9. Epub 2011/04/12. 10.4103/0189-6725.78666 . [DOI] [PubMed] [Google Scholar]
- 78.Fandino-Franky J, Torres M, Narino D, Fandino J. Corpus callosotomy in Colombia and some reflections on care and research among the poor in developing countries. Epilepsia. 2000;41 (Suppl. 4):S22–7. Epub 2000/08/30. . [DOI] [PubMed] [Google Scholar]
- 79.Rao MB, Radhakrishnan K. Is epilepsy surgery possible in countries with limited resources? Epilepsia. 2000;41 (Suppl. 4):S31–4. Epub 2000/08/30. . [DOI] [PubMed] [Google Scholar]
- 80.Agarwal PK, Bowman R, Courtright P. Child Eye Health Tertiary Facilities in Africa. J AAPOS. 2010;14(3):263–6. Epub 2010/07/07. 10.1016/j.jaapos.2010.02.007 . [DOI] [PubMed] [Google Scholar]
- 81.Gogate P, Dole K, Ranade S, Deshpande M. Cost of pediatric cataract surgery in Maharashtra, India. Int J Ophthalmol. 2010;3(2):182–6. Epub 2010/01/01. 10.3980/j.issn.2222-3959.2010.02.22 ; PubMed Central PMCID: PMCPmc3340774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gradin D, Mundia D. Simultaneous bilateral cataract surgery with IOL implantation in children in Kenya. J Pediatr Ophthalmol Strabismus. 2012;49(3):139–44. Epub 2011/08/02. 10.3928/01913913-20110726-01 . [DOI] [PubMed] [Google Scholar]
- 83.Evans CT, Lenhart PD, Lin D, Yang Z, Daya T, Kim YM, et al. A cost analysis of pediatric cataract surgery at two child eye health tertiary facilities in Africa. J AAPOS. 2014;18(6):559–62. Epub 2014/12/03. 10.1016/j.jaapos.2014.08.005 ; PubMed Central PMCID: PMCPmc4268264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Prajna VN, Nirmalan PK, Saravanan S, Srinivasan M. Economic analysis of corneal ulcers in South India. Cornea. 2007;26(2):119–22. 10.1097/ICO.0b013e31802b36dc [DOI] [PubMed] [Google Scholar]
- 85.Vida VL, Leon-Wyss J, Rojas M, Mac KR, Barnoya J, Castaneda AR. Pulmonary artery hypertension: Is it really a contraindicating factor for early extubation in children after cardiac surgery? Ann Thorac Surg. 2006;81(4):1460–5. 10.1016/j.athoracsur.2005.11.050 [DOI] [PubMed] [Google Scholar]
- 86.Vida VL, Barnoya J, O'Connell M, Leon-Wyss J, Larrazabal LA, Castaneda AR. Surgical versus percutaneous occlusion of ostium secundum atrial septal defects—Results and cost-effective considerations in a low-income country. J Am Coll Cardiol. 2006;47(2):326–31. 10.1016/j.jacc.2005.06.086 . [DOI] [PubMed] [Google Scholar]
- 87.Talwar S, Choudhary SK, Airan B, Juneja R, Kothari SS, Saxena A, et al. Reducing the costs of surgical correction of congenitally malformed hearts in developing countries. Cardiol Young. 2008;18(4):363–71. 10.1017/s1047951108002448 . [DOI] [PubMed] [Google Scholar]
- 88.Zeinaloo AA, Meraji SM, Zanjani KS, Mirzaaghayan MR. Device occlusion versus surgery for closure of congenital heart defects: Cost issues in Iran. Journal of Tehran University Heart Center. 2008;3(3):141–4. [Google Scholar]
- 89.Chen B, Hu S, Wang L, Wang K, Zhang G, Zhang H, et al. Economical strategies of laparoscopic splenectomy: A Chinese single-center experience. Chirurgische Gastroenterologie Interdisziplinar. 2007;23(4):387–91. [Google Scholar]
- 90.Mughal AR, Sadiq M, Hyder SN, Qureshi AU, Shah SSA, Khan MA, et al. Socioeconomic status and impact of treatment on families of children with congenital heart disease. Journal of the College of Physicians and Surgeons Pakistan. 2011;21(7):398–402. doi: 07.2011/JCPSP.398402 [PubMed] [Google Scholar]
- 91.Panni RZ, Ashfaq A, Amanullah MM. Earlier surgical intervention in congenital heart disease results in better outcome and resource utilization. BMC Health Serv Res. 2011;11:353 Epub 2011/12/31. 10.1186/1472-6963-11-353 ; PubMed Central PMCID: PMCPmc3277492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sadoh WE, Nwaneri DU, Owobu AC. The cost of outpatient management of chronic heart failure in children with congenital heart disease. Cardiovasc J Afr. 2011;22(3):S22. [DOI] [PubMed] [Google Scholar]
- 93.Liu SX, Chen F, Ding XY, Zhao ZZ, Ke W, Yan Y, et al. Comparison of results and economic analysis of surgical and transcatheter closure of perimembranous ventricular septal defect. Eur J Cardiothorac Surg. 2012;42(6):E157–E62. 10.1093/ejcts/ezs519 . [DOI] [PubMed] [Google Scholar]
- 94.Costa R, Pedra CA, Ribeiro M, Pedra S, Ferreira-Da-Silva AL, Polanczyk C, et al. Incremental cost-effectiveness of percutaneous versus surgical closure of atrial septal defects in children under a public health system perspective in Brazil. Expert Rev Cardiovasc Ther. 2014;12(11):1369–78. Epub 2014/10/07. 10.1586/14779072.2014.967216 . [DOI] [PubMed] [Google Scholar]
- 95.Vasquez JC, Montesinos E, Peralta J, Rojas L, DeLaRosa J, Leon JJ. Need for lung resection in patients with intact or ruptured hydatid cysts. Thorac Cardiovasc Surg. 2009;57(5):295–302. Epub 2009/07/25. 10.1055/s-0029-1185604 . [DOI] [PubMed] [Google Scholar]
- 96.Yang YR, Williams GM, Craig PS, McManus DP. Impact of increased economic burden due to human echinococcosis in an underdeveloped rural community of the People's Republic of China. PLoS Negl Trop Dis. 2010;4(9). Epub 2010/09/22. 10.1371/journal.pntd.0000801 ; PubMed Central PMCID: PMCPmc2939032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang L, Wen H, Feng X, Jiang X, Duan X. Analysis of economic burden for patients with cystic echinococcosis in five hospitals in northwest China. Trans R Soc Trop Med Hyg. 2012;106(12):743–8. Epub 2012/11/06. 10.1016/j.trstmh.2012.09.003 . [DOI] [PubMed] [Google Scholar]
- 98.Asiedu K, Etuaful S. Socioeconomic implications of Buruli ulcer in Ghana: A three-year review. Am J Trop Med Hyg. 1998;59(6):1015–22. [DOI] [PubMed] [Google Scholar]
- 99.Adoga A, Nimkur T, Silas O. Chronic suppurative otitis media: Socio-economic implications in a tertiary hospital in Northern Nigeria. Pan Afr Med J. 2010;4:3 Epub 2010/12/02. ; PubMed Central PMCID: PMCPmc2984311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nursal TZ, Yildirim S, Tarim A, Caliskan K, Ezer A, Noyan T. Burns in Southern Turkey: Electrical burns remain a major problem. J Burn Care Rehabil. 2003;24(5):309–14. 10.1097/01.BCR.0000085876.28504.EE [DOI] [PubMed] [Google Scholar]
- 101.Allorto NL, Clarke DL, Thomson SR. A cost model case comparison of current versus modern management of burns at a regional hospital in South Africa. Burns. 2011;37(6):1033–7. 10.1016/j.burns.2011.04.004 [DOI] [PubMed] [Google Scholar]
- 102.Zhu L, Zhang Y, Liu L, Jiang J, Liu Y, Shi F, et al. Hospitalized pediatric burns in North China: a 10-year epidemiologic review. Burns. 2013;39(5):1004–11. Epub 2013/01/30. 10.1016/j.burns.2012.12.014 . [DOI] [PubMed] [Google Scholar]
- 103.Alinia S, Rezaei S, Daroudi R, Hadadi M, Akbari Sari A. Extent, nature and hospital costs of fireworks-related injuries during the Wednesday Eve festival in Iran. J Inj Violence Res. 2013;5(1):11–6. Epub 2011/10/04. 10.5249/jivr.v5i1.146 ; PubMed Central PMCID: PMCPmc3591727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vida VL, Leon-Wyss J, Larrazabal A, Cruz S, Castaneda AR. Mediastinitis in pediatric cardiac surgery—Treatment and cost- effectiveness in a low-income country. Pediatr Cardiol. 2007;28(3):163–6. 10.1007/s00246-006-0008-1. 10.1007/s00246-006-0008-1 [DOI] [PubMed] [Google Scholar]
- 105.Hong L, Wu Y, Yan Z, Xu M, Chu J, Chen QM. Laparoscopic surgery for choledochal cyst in children: a case review of 31 patients. Eur J Pediatr Surg. 2008;18(2):67–71. Epub 2008/04/26. 10.1055/s-2008-1038486 . [DOI] [PubMed] [Google Scholar]
- 106.Ramachandran R, Jha V. Kidney transplantation is associated with catastrophic out of pocket expenditure in India. PLoS One. 2013;8(7):e67812 Epub 2013/07/19. 10.1371/journal.pone.0067812 ; PubMed Central PMCID: PMCPmc3701634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hamamci EO, Besim H, Bostanoglu S, Sonisik M, Korkmaz A. Use of laparoscopic splenectomy in developing countries: analysis of cost and strategies for reducing cost. J Laparoendosc Adv Surg Tech A. 2002;12(4):253–8. Epub 2002/09/25. 10.1089/109264202760268023 . [DOI] [PubMed] [Google Scholar]
- 108.Chen Z, Chen L, Wu L. Transcatheter amplatzer occlusion and surgical closure of patent ductus arteriosus: comparison of effectiveness and costs in a low-income country. Pediatr Cardiol. 2009;30(6):781–5. Epub 2009/04/15. 10.1007/s00246-009-9440-3 . [DOI] [PubMed] [Google Scholar]
- 109.Dave HB, Gordillo L, Yang Z, Zhang MS, Hubbard GB 3rd, Olsen TW. The societal burden of blindness secondary to retinopathy of prematurity in Lima, Peru. Am J Ophthalmol. 2012;154(4):750–5. Epub 2012/07/27. 10.1016/j.ajo.2012.04.003 . [DOI] [PubMed] [Google Scholar]
- 110.Sancaktutar AA, Soylemez H, Bozkurt Y, Penbegul N, Atar M. Treatment of forgotten ureteral stents: how much does it really cost? A cost-effectiveness study in 27 patients. Urol Res. 2012;40(4):317–25. Epub 2011/08/13. 10.1007/s00240-011-0409-3 . [DOI] [PubMed] [Google Scholar]
- 111.Kerr G, Tuomi S, Muller A. Costs involved in using a cochlear implant in South Africa. S Afr J Commun Disord. 2012;59:16–26. Epub 2013/02/16. . [PubMed] [Google Scholar]
- 112.Baltussen R, Stolk E, Chisholm D, Aikins M. Towards a multi-criteria approach for priority setting: an application to Ghana. Health Econ. 2006;15(7):689–96. Epub 2006/02/24. 10.1002/hec.1092 . [DOI] [PubMed] [Google Scholar]
- 113.Mock C, Cherian M, Juillard C, Donkor P, Bickler S, Jamison D, et al. Developing priorities for addressing surgical conditions globally: furthering the link between surgery and public health policy. World J Surg. 2010;34(3):381–5. Epub 2009/10/31. 10.1007/s00268-009-0263-4 . [DOI] [PubMed] [Google Scholar]
- 114.Shrime MG, Sleemi A, Ravilla TD. Charitable platforms in global surgery: a systematic review of their effectiveness, cost-effectiveness, sustainability, and role training. World J Surg. 2015;39(1):10–20. Epub 2014/04/01. 10.1007/s00268-014-2516-0 ; PubMed Central PMCID: PMCPmc4179995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mock CN, Donkor P, Gawande A, Jamison DT, Kruk ME, Debas HT. Essential surgery: key messages from Disease Control Priorities, 3rd edition. Lancet. 2015;385(9983):2209–19. Epub 2015/02/11. 10.1016/s0140-6736(15)60091-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Haagsma JA, Polinder S, Cassini A, Colzani E, Havelaar AH. Review of disability weight studies: comparison of methodological choices and values. Population health metrics. 2014;12:20 Epub 2014/01/01. 10.1186/s12963-014-0020-2 ; PubMed Central PMCID: PMCPmc4445691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Higashi H, Barendregt JJ, Kassebaum NJ, Weiser TG, Bickler SW, Vos T. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: cleft lip and palate, congenital heart anomalies and neural tube defects. Arch Dis Child. 2015;100(3):233–8. Epub 2014/09/28. 10.1136/archdischild-2014-306175 . [DOI] [PubMed] [Google Scholar]
- 118.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223. Epub 2012/12/19. 10.1016/s0140-6736(12)61689-4 . [DOI] [PubMed] [Google Scholar]
- 119.Marseille E, Morshed S. Essential surgery is cost effective in resource-poor countries. Lancet Glob Health. 2014;2(6):e302–3. Epub 2014/08/12. 10.1016/s2214-109x(14)70236-0 . [DOI] [PubMed] [Google Scholar]
- 120.Siegel JE, Weinstein MC, Russell LB, Gold MR. Recommendations for reporting cost-effectiveness analyses. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276(16):1339–41. Epub 1996/10/23. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.