Abstract
Clinicians who care for children with asthma have an obligation to coordinate asthma care with the schools. Aside from routine clinical care of asthmatic children, providers must educate the family and child about the need for an asthma treatment plan in school and support the school nurse meeting the needs of the student requiring school-based asthma care. The following article was developed by multiple stakeholders to address this need. It describes the 4 components of the School-based Asthma Management Program (SAMPRO™). SAMPRO™ details elements necessary for the education of children, families, clinicians, and school-based personnel based on a “circle of support” that would enhance multidirectional communication and promote better care for children with asthma within the school setting.
Keywords: Asthma, school, school nurse, children, asthma action plan, education, environment, triggers
Childhood asthma is a common chronic pediatric condition affecting 6.3 million children.1 Morbidity from childhood asthma adversely affects school performance, with 1 in 2 children reporting school absences caused by asthma each year (www.cdc.gov/nchs/data/series/sr_03/sr03_035.pdf).2 These asthma-related absences influence academic achievement, leading to decreased levels of reading proficiency and increased risk of learning disabilities.3 Improving health and school-related outcomes for children with asthma will require use of school-based partnerships that focus on integrated care coordination among families, clinicians, and school nurses.
In this regard clinicians who care for children with asthma have an obligation to coordinate asthma care with the schools. Aside from routine clinical care of asthma, providers must educate the family and child about the need for an asthma treatment plan in school and support the school nurse meeting the needs of the student requiring school-based asthma care. Developmentally appropriate asthma management, effective communication, and partnership with the schools are essential for quality asthma care.
To address these critical issues, a summit meeting attended by multiple stakeholders (herein termed the SAMPRO™ Workforce; Table E1 in this article’s Online Repository at www.jacionline.org) and sponsored by the American Academy of Allergy, Asthma & Immunology (AAAAI) with additional financial support from the National Association of School Nurses (NASN) was convened in October 2015, with the purpose of creating a central resource (termed the School-based Asthma Management Program [SAMPRO™]) housed within the administrative structure of the AAAAI offices (Office of School-based Management for Asthma). This resource would provide education for children, families, clinicians, and school-based personnel based on a circle of support that would enhance multidirectional communication and promote better care for children with asthma within the school setting (Fig 1). In addition to the recommendations presented herein, resources for SAMPRO™ include the school nurse asthma toolbox (available at www.aaaai.org/SAMPRO).
FIG 1.

The circle of support, including the child, clinician, school personnel, and family and the broader community.
The SAMPRO™ Workforce, based on their experiences in school-based asthma care and educational backgrounds, were divided into 5 groups to address the key elements of SAMPRO™. The first group focused on the role of the clinician in coordinating asthma care with the child, family, and school; integral to this process is the creation and transmission of an Asthma Action Plan (AAP) to the school. The second group addressed the receipt of this information within the school setting along with its processing and appropriate implementation. The third group evaluated various educational programs currently available for children, school personnel, and families to make recommendations regarding which tools would be most appropriate to address different educational needs. The fourth group focused on both the school and home environments to make recommendations on reducing triggers that could affect overall asthma control. Finally, the fifth group tackled the important issues of dissemination, implementation, and sustainability of the SAMPRO™ initiatives. This article will be a comprehensive summary of their observations and recommendations for the creation of SAMPRO™.
SAMPRO™: ESSENTIAL COMPONENTS
The SAMPRO™ Workforce identified the importance of including 4 components (Table I) essential to creating an effective partnership between schools and providers centered around childhood asthma care. These 4 items include development and implementation of a number of components:
A circle of support that facilitates communication among the child, the family, clinicians, school nurses, and the community.
Asthma Management Plans (AMPs), which include both the Asthma Emergency Treatment Plan (AEP) and an AAP. The AEP details an emergency management plan for all students with asthma, including stock albuterol and a way to deliver the medication. An AAP for home and school includes medical authorization for self-carry and administration of asthma medications, along with parental release of information.
A comprehensive education plan for all school personnel.
A plan for assessment of the school environment and remediation of school-based asthma triggers.
TABLE I.
Components for SAMPRO™
| Components | Description |
|---|---|
| (1) Development and implementation of a circle of support that facilitates communication among clinicians, school nurses, families, and the community | A communication network integrating the child, their family, the health care provider, and the school nurse into the asthma care team |
| (2) Implement AMPs: The AMP includes the AEP for emergency management of asthma symptoms, including stock albuterol, where state law allows and a way to deliver the medication. Each student should have an AAP for home and school with medical authorization for self-carry and administration of asthma medications, along with parental release of information. | This is a “generic” asthma emergency treatment plan to address children experiencing an asthma exacerbation, when to use rescue medication, how much rescue medication to administer, and when to call 911. An AAP includes individualized instructions for the student’s AMP and instructions on when to step-up asthma care. |
| (3) A comprehensive asthma education plan for all school personnel | A plan for school personnel regarding what is asthma, how to recognize it, and how to respond to an asthma exacerbation |
| (4) Assessment and remediation of school-based asthma triggers | A plan to assess the school environment and respond to asthma triggers |
These 4 components are described in greater detail in this article. In addition to a complete description and recommendations regarding these components, SAMPRO™ also provides an asthma education toolbox that contains many reference tools and educational videos to complement, supplement, and enhance the utility of using SAMPRO™ for providing comprehensive school-based care for children with asthma.
COMPONENT 1
Circle of support
An effective circle of support for the child with asthma includes the primary care clinician (and asthma specialist), the school nurse, community resources (when available), and the family. Key to the circle of support is an infrastructure of communication centered around the child and his or her asthma management. This communication network allows for patient-centered education and improved asthma management by the school nurse.4 Understanding who is in the circle of support and providing common elements to improve communication and control are key to SAMPRO™. The roles of clinicians, school nurses, other school personnel, and community resources as members of this circle are discussed in the following sections.
Role of clinicians
Clinicians who care for children with asthma have a unique obligation to coordinate asthma care with the schools. The school is the first community-based setting in which children manage asthma symptoms and avoidance of asthma triggers without the supervision of family members.5 Aside from routine clinical asthma care, health care providers must educate the family and child about the need for an AAP in school and should support the school nurse providing school-based asthma care. Students often lack needed and prescribed medications at school.4 Clinicians should ensure that the student has sufficient medications and valved holding chambers available for school use. In addition, clinicians and their office staff should attempt to assist families to obtain these medications for home and school use when barriers exist. Developmentally appropriate asthma management and effective communication and partnership with the schools are essential for optimal asthma care.
In addition to regular follow-up visits for asthma during the year, primary care clinicians and asthma specialists are encouraged to either conduct an asthma-specific visit or to focus a portion of the annual antecedent school visit on asthma.2 Components of this visit should include (1) assessment of asthma severity and current level of asthma control with appropriate adjustment of medications; (2) education about asthma management, triggers, and inhaler/spacer technique; (3) review of the child’s asthma care plan in the school setting; and (4) completion of required school forms. A recommended provider and patient checklist to facilitate this visit is included in Tables E2 and E3 in this article’s Online Repository at www.jacionline.org. These checklists are intended to facilitate the assessment and inform the management of asthma by all members of the circle of support.
The SAMPRO™ Workforce developed 2 options for individualized asthma management to facilitate the development and transmission of AAPs to schools: (1) an AAP for home and school (Fig 2) inclusive of medication authorizations and parental release of information (a complete AAP form can be found in the OLS [see Fig E1 in this article’s Online Repository at www.jacionline.org]); and (2) a School Supplementary Treatment Order Form (inclusive of release of information and medical authorization forms) that might accompany an existing AAP (see Fig E2 in this article’s Online Repository at www.jacionline.org). Collectively, these forms have multiple elements designed to improve communication and reduce clinician burden and are described in greater detail in the following sections. The health care provider should be especially cognizant of the need to tailor the AAP for each child. This individualization will include a careful assessment of literacy, cultural sensitivity, and the overall needs of the family based on socioeconomic status and the home environment. In addition, clinicians should query each family about their knowledge of asthma and how their daily work and school schedules affect asthma symptoms, medication adherence, and exposure to asthma triggers.
FIG 2.
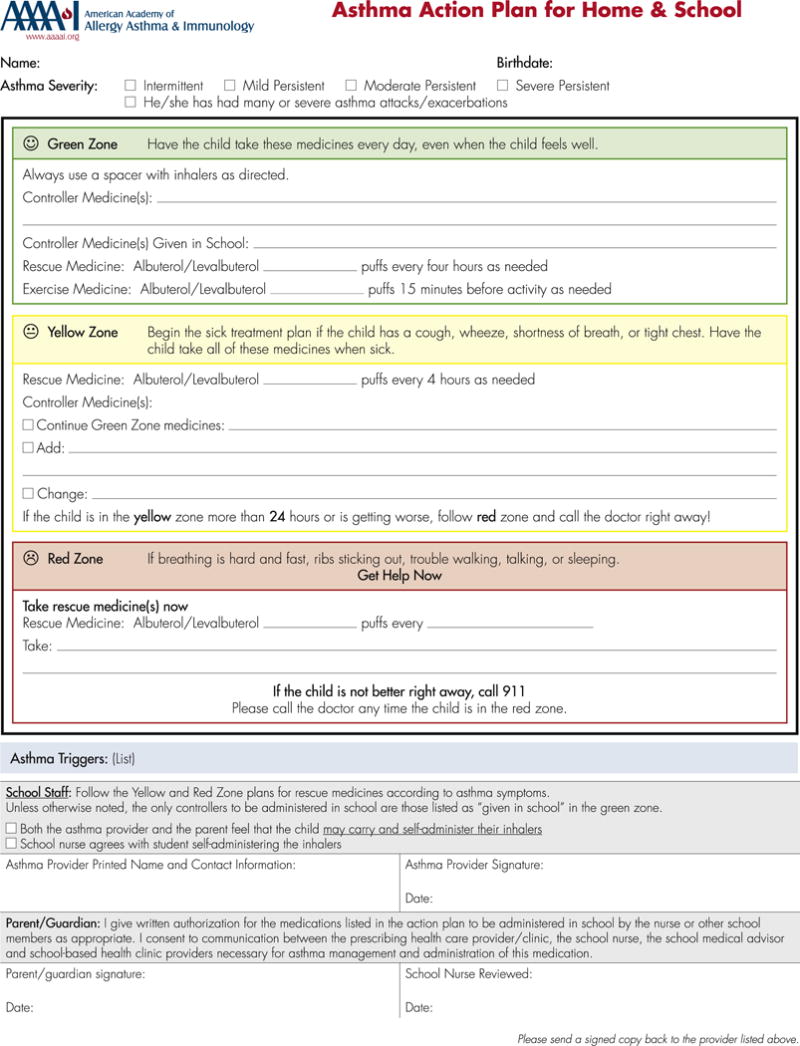
AAP for home and for school.
Role of the school nurse
The NASN has defined school nursing as follows, “a specialized practice of public health nursing [that] protects and promotes student health, facilitates normal development, and advances academic success. School nurses, grounded in ethical and evidence-based practice, are the leaders that bridge health care and education, provide care coordination, advocate for quality student-centered care, and collaborate to design systems that allow individuals and communities to develop their full potentials” (www.nasn.org/rolecareer).
School nurses are an essential part of the health care team because they often coordinate care for students with chronic conditions and oversee the appropriate use of medications in the school setting. School nurse involvement in asthma care coordination has resulted in improvements in health care use, school attendance, medication adherence, and quality of life.3,4,6,7 School nurses are uniquely positioned to provide direct care, adherence counseling, and education for asthmatic patients.8 They can review and reinforce proper inhaler technique and usually have the most recorded data of quick-relief medication use—one of the hallmarks of asthma control. More specifically, the role of the school nurse in caring for the child with asthma can include the activities listed in Table E4 in this article’s Online Repository at www.jacionline.org.
Presently, most communication between asthma providers and schools centers on completion of school medication authorization forms that exist in many types and formats and might seem burdensome to the provider. Despite evidence that school nurse involvement benefits the student in both the academic and health areas, the school nurse is often underused as a member of the asthma care team. The AAP for Home and School developed by the SAMPRO™ Workforce includes not only the components of the medication authorization form but also describes the home management plan for the school nurse to review (see below). The school nurse is in a position to determine how the plan can be implemented and reinforced at school, as well as to provide feedback on whether any additional therapeutic or educational interventions in the school setting are needed. In this way school nurses provide case management because they implement the plan to assist students and their families in managing asthma, decreasing triggers, and obtaining other community resources that will assist in improved management.
Because of limited resources and the varied school nurse staffing across the country, it is important to clearly identify those students with asthma and then prioritize who might benefit from more intensive care coordination. This can be done through an asthma screening questionnaire that can identify current control and/or other at-risk factors. There are also times when the school nurse identifies students with undiagnosed asthma as a result of inquiring about reasons for chronic absenteeism, inability to participate in physical education classes, and assessment of students with persistent respiratory concerns. In these situations the school nurse contacts parents/guardians to connect the student with a health care provider for follow-up on the asthma symptoms.9
The lack of national standards or requirements for school nurse services has resulted in great variation among states and local school districts. Nationally, about 81% of schools have a nurse in some capacity (www.cdc.gov/healthyyouth/data/shpps/pdf/2014factsheets/health_services_shpps2014.pdf). School nurses often cover many schools and large student populations. The need for school nurse services might be greater in school districts that serve large numbers of low-income children who experience higher than average morbidity from asthma. School districts without a school nurse will be challenged to develop strategies to implement AMPs (eg, SAMPRO™), with the ideal being a licensed registered nurse to administer the plan that is best practice and evidence based. When a school nurse is not available all day every day, the school district must follow their state nurse practice act regarding delegation of care in schools. Although the actual health tasks can be carried out by other school staff, the school nurse must be involved in the development of the district AMPs and direct asthma care planning.
Role of the community
The SAMPRO™ Workforce, NASN, and the American Academy of Pediatrics Council of School Health (http://pediatrics.aappublications.org/content/early/2016/05/19/peds.2016-0852) strongly endorse the presence of a full-time licensed registered school nurse in schools. As school districts with limited access to school nurses transition to this model, they can use other community- and school-based health resources to implement SAMPRO™. These resources include the use of school-based health centers (SBHCs), which offer an opportunity for community health care providers to partner with schools in managing asthma, particularly for underserved populations.10 SBHC staff can provide a wide array of primary care services within the school building and complement the care of community providers, including routinely monitoring asthma control and symptoms and addressing social and environmental factors influencing asthma control. Care planning for students with chronic conditions by SBHC providers might improve the number of students with AAPs present in the school.11
Mobile clinics provide increased outreach of quality asthma care for families challenged to maintain good asthma control.12 Breathmobile programs have demonstrated a significant reduction in annual rates of emergency department visits and hospitalizations and school absenteeism and a significant return on investment resulting from reduced asthma morbidity.13 School-based telemedicine and community health care workers are also a potential avenue to increase access to specialty asthma care in underserved populations.14–16
COMPONENT 2
AMPs (AEP and AAP)
A school asthma management program should consist of AMPs that include the school-based AEP, which would apply to all students who present with troublesome asthma symptoms but do not have a documented and updated AAP available for access by the school nurse or alternative designee. A generic plan was developed by the SAMPRO™ Workforce and can be found in Fig E3 in this article’s Online Repository at www.jacionline.org. The AEP might require individual modification to comply with local and state requirements.
In addition, individual students with a diagnosis of asthma should have an AAP. Ideally, the AEP and AAP would be complementary and result in a comprehensive approach to the management of asthma (both acute and chronic) within the school setting that would include access to stock albuterol. Both the AAP for home and school and the school-based AEP should be viewed as essential components of a school’s overall implementation of SAMPRO™.
The AAP for home and school
The AAP represents the cornerstone of an effective patient education and communication system, allowing the child, family, and school staff to step up asthma care at the first signs of exacerbation, according to the National Heart, Lung, and Blood Institute’s “Expert panel report 3: guidelines for the diagnosis and management of asthma.”2 These guidelines recommend that all asthmatic patients have an AAP created that is individualized for each patient and provided to all patients.
The AAP for Home and School developed by the SAMPRO™ Workforce is an individualized treatment plan for the chronic and acute management of asthma at home and school (Fig 2; also see Fig E1 for a sample form). The AAP should be developed jointly between the health care provider and the family with input and feedback from the school nurse. AAPs for the home alone might not be acceptable or sufficient for all school districts because care plans for schools might require a specific signed release form for medications administered at school. Given findings of alarmingly low rates of care plans and AAPs in schools,17,18 the SAMPRO™ Workforce recommends an AAP that integrates the home AAP and the school authorization form into a single workflow document. This type of provider workflow allows and facilitates communication that is (1) clear for multiple users; (2) efficient to complete by providers; and (3) consistent across multiple settings. The AAP for Home and School provided in the toolbox integrates the home AAP with medication and self-carry authorizations and the Health Care Information and Privacy Act (HIPAA)/Family Educational Rights and Privacy Act (FERPA) release (Fig 2).
Key features within the AAP are an identification of asthma control and asthma severity. Asthma control involves a careful assessment of daily impairment by asthma symptoms and risk of future exacerbations. Missed school days (absenteeism) are an important indicator of functional impairment and quality of life. Frequent asthma symptoms/exacerbations can result in missed classroom time for school nurse visits, disrupt instructional time, and result in decreased standardized test scores.19 A discordance between the number of school days missed and the perception of control might also indicate poor understanding of the disease state or poor symptom recognition.20
Asthma disease severity and the risk of future severe exacerbations are important assessments for health care providers, families, or both to communicate to school nurses. Understanding that a student requires controller medications (persistent asthma) allows the school nurse to assess adherence and, with appropriate medical orders, administer controller medications at school when necessary. Furthermore, identifying children with a history of severe asthma exacerbations allows the school nurse to recognize students who might require closer observation, more aggressive use of bronchodilators, and/or a step-up of asthma treatment. Recognition of when a higher level of care is needed is particularly critical for those with infrequent but severe exacerbations because symptoms can be initially underrecognized. If a child with intermittent asthma precipitously requires a change in the frequency of bronchodilator therapy, a school nurse can advocate for reassessment by the clinician.
The AAP for Home and School also includes information about asthma triggers specific for the student and about the child’s history of severe asthma exacerbations. Allergens and irritants in the school environment can be potent triggers of asthma symptoms and are identified on the form.21 With this information, school nurses can work with students, families, and school administrators to minimize exposure for susceptible subjects. Clear recognition of common asthma triggers is a hallmark of an asthma-friendly school and helps facilitate a healthy school environment for all students.
Alternatively, an existing home AAP can be modified to meet an individual patient’s and school district’s needs to contain the essential elements of the AAP. For providers and schools who are using AAPs that meet the essential criteria, an alternative form is provided that can be combined with an existing AAP to coordinate authorizations and school treatment orders (Fig 3). A detailed description of each of the elements of the AAP for Home and School is included in the online supplement (see Table E2).
FIG 3.
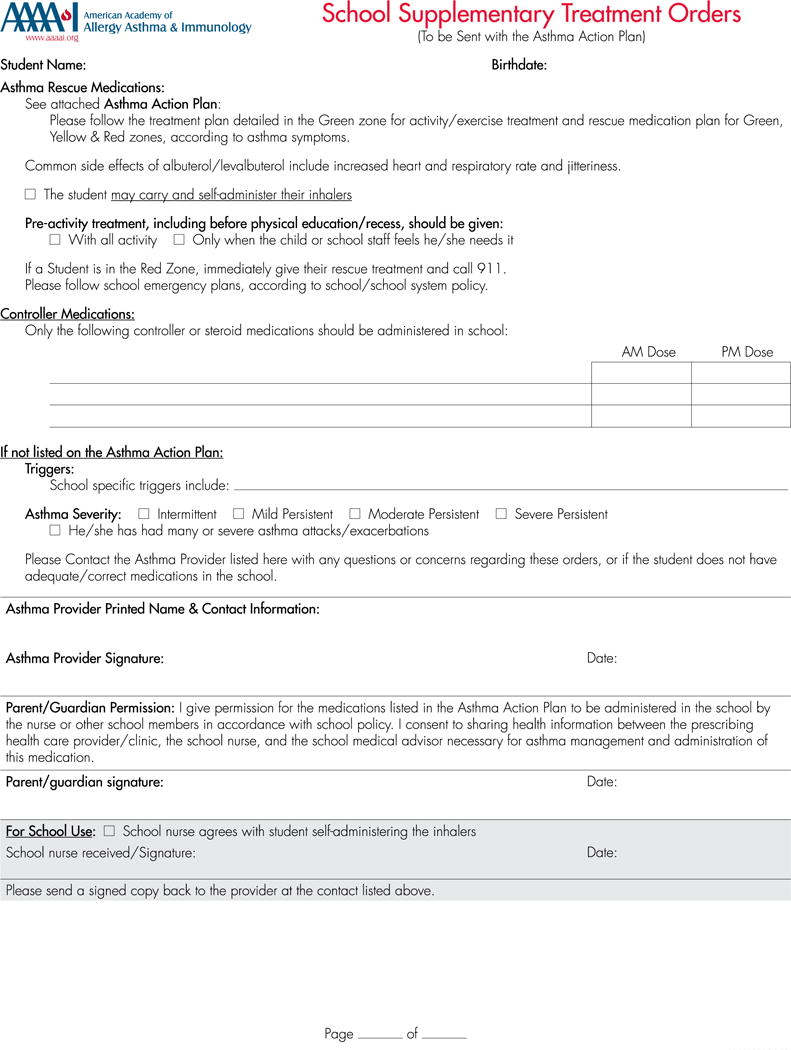
School supplementary treatment orders form.
Transmitting the AAP within the circle of support
Ideal communication between providers and school nurses should be accessible and bidirectional and use simple standardized processes that are customizable for individual students (see Table E5 in this article’s Online Repository at www.jacionline.org). As the primary driver for schoolchildren’s asthma assessment and management, the asthma provider has a critical role in ensuring that a coordinated student-centered asthma care network is established. In addition to completing and transmitting an AAP with associated authorization forms, prescriptions and education regarding school-based asthma care need to be provided to the patient and school nurse. By integrating the school nurse into the circle of communication and asthma care, the clinician should strive to actively involve the school nurse as part of the asthma care team.
Communication challenges among school nurses, parents, and health care providers often impede a coordinated, comprehensive, and integrated approach to asthma management. When there is no provider-initiated AAP, the school nurse can only focus on acute symptom management, with limited ability to adjust controller and pre-exercise therapy. To develop a cohesive overall school-based AMP, written communication should proceed directly from the health care provider to the school nurse and should include complete quick-relief and controller medication and treatment orders, recent hospitalizations, and emergency department visits and establish periodic updates on students’ health status. The AAP needs to clearly communicate what medications are to be administered in the school setting. Direct verbal communication is difficult when both the school nurse and health care provider seek to fit in telephone calls throughout their work days. Thus there is a need for streamlined communication.
Electronic health records (EHRs) that school nurses can view with parental permission would be an ideal format for effective transmission of the AAP to schools. Interoperability of EHRs is the ideal scenario for such communications, providing immediate relevant feedback regarding treatment efficacy and adherence. Federal and state laws, as well as local school policies and protocols, establish uniform standards for clinicians and school nurses to communicate about students’ asthma while respecting student confidentiality.
Electronic sharing capabilities, both within the EHR and beyond, have created a variety of options for easy transmission of information, including to local schools. The EHR can streamline the creation of AAPs into a more concise and patient-centered format.22 The most common mode of transmission through the EHR is the electronic fax. This can be done as part of the normal provider workflow, with AAPs being easily sent to multiple recipients at a time, including schools. Although most schools use the direct fax for communication with providers, the fax machine is often shared with the main school office. It is important to include cover sheets and protect health information in compliance with the HIPAA and FERPA privacy laws.
Electronic health information exchanges, Web portals, continuity of care documents, and direct secure messaging are HIPAA-compliant methods that can be applied to the school setting for efficient transmission of AAPs to the school. Direct secure messaging between school nurses and other health care providers will require that the nurse have access to an health information exchange; however, AAPs can be transmitted electronically by using intranet access from an approved IP address. In some communities secure portals, such as Kidsehealth.com, allow providers to upload AAPs directly from the EHR to the portal. School nurses can then access the portal to obtain updated AAPs.23 Streamlining processes to automatically upload documents, such as the AAP, into portals in real time optimizes clinic workflows, although it does not allow for bidirectional communication, which is important.24
Despite being the most common workflow, providing a copy of the AAP to the student for manual delivery to the school nurse is an unreliable means of AAP transmission.25 If electronic capabilities are not available, faxing or mailing the AAP is preferable but requires that the health care provider have an up-to-date fax number or address for the schools. There is a potential risk of breach in confidentiality by direct fax in that most faxes come to a shared fax machine in the main school office. Schools should have policies in place to ensure that confidential faxes coming to a shared fax include a cover letter clearly defining the document as “confidential” (protected health information) and list the school nurse as the recipient of this information. Ideally, faxing to an accurate number that is direct to the school health office can mitigate the risk.8
Having easily accessible and accurate school contact information can also be challenging. School districts can have a central nursing office in which forms can be sent if the exact school/contact is not clear.26 This process can be improved by developing a partnership whereby area schools provide local health care providers with a list of school contact information (and vice versa), preferably with similar lists being built into the EHR. School-based community programs and state-supported school health programs can aid in this process and partnership.
National and local laws, including both HIPAA and FERPA, require that health care providers and school employees exchange information responsibly, securely, and with parental permission. The HIPAA privacy rule allows health care providers to disclose protected health information about students to school nurses, physicians, or other health care providers for treatment purposes without the authorization of the student or student’s parent. For example, a student’s primary care physician can discuss the student’s medication and other health care needs with a school nurse who will administer the student’s medication and provide care to the student while the student is at school (www.hhs.gov/hipaa/for-professionals/faq/517/does-hipaa-allow-a-health-care-provider-to-isclose-information-to-a-school-nurse/index.html).
Conversely, although the FERPA privacy rule requires that the parent provide written authorization for the release of protected school-related information, such as absences, by the school nurse, it does not allow school personnel to release information without written parental authorization to a medical provider who is providing treatment. The bidirectional exchange of relevant school-related and health information between health care providers and schools requires parental permission for both HIPAA- and FERPA-protected information.
Measurable outcomes for successful AAP implementation
The resources and skills of the asthma providers are an important asset in the testing and measurement of success of school-focused interventions to make improved school-based management of asthma sustainable. Challenges to outcome measurement include the variety of data systems and EHRs used in schools and health organizations, with a paucity of systems that interface bidirectionally. Outcomes of AAP use have been reported, demonstrating fewer deaths and emergency department visits for patients with AAPs.27,28 Current studies have suggested that the use of AAPs by school-based asthma programs can improve school attendance and performance.4,5 Future efforts should focus on creating interoperable systems that report asthma-specific outcomes relevant to patient care. Examples of potential outcome and process measures are listed in Table E6 in this article’s Online Repository at www.jacionline.org. Efficient and meaningful outcomes evaluation will require a multistakeholder approach and specific enhancements in currently available electronic technology to improve interoperability and local collaborations. Funding these programs is an investment in both optimal health outcomes and the academic success of our students.
COMPONENT 3
Education of school personnel in SAMPRO™
One of the 10 components of the whole-school, whole-community, whole-child model is health education. This includes any combination of planned learning experiences that provide the student with an opportunity to acquire the skills and knowledge to make sound decisions about health-promoting behavior. Such education, when based on the assessment of student health needs, in collaboration with the community can reinforce health messages that are relevant to the student’s health. Furthermore, the collaboration of multiple school staff can help to advance health and academic outcomes.29 A consensus document developed by the Asthma and School subcommittee of the National Heart, Lung, and Blood Institute’s National Asthma Education and Prevention Program stressed the importance of asthma education for all school staff as integral to the establishment of a successful school asthma management program (www.nhlbi.nih.gov/health-pro/resources/lung/managing-asthma-guide-schools-2014-edition-html). In addition to asthma basics education, this resource also contains comprehensive information about the roles that each school staff member can play in a school asthma program, as well as ideas on action items for various staff members that are briefly covered in this white paper. Additional resources for health aides (see Table E7 in this article’s Online Repository at www.jacionline.org), school administrators and support staff (see Table E8 in this article’s Online Repository at www.jacionline.org), physical education teachers and coaches (see Table E9 in this article’s Online Repository at www.jacionline.org), and custodial staff (see Table E10 in this article’s Online Repository at www.jacionline.org) are listed in the Online Repository. These individuals can be integral team members in the early identification of children with poorly controlled asthma and the mitigation of environmental asthma triggers.
The amount and focus of that education will differ depending on a person’s role in the school, but there are components of asthma education that, ideally, all should receive. These components include epidemiology, pathophysiology, symptoms, triggers, and asthma medications. A critical component of this education is recognizing worsening asthma symptoms, lack of asthma control, or both. This awareness of warning signs, including when and where to get help, should be provided to all school staff and students. Knowledge and understanding of the AAP, AEP, or both are also necessary components of the asthma care of the student and education of the staff.
The school nurse has an instrumental role in addressing the components of asthma education through interactions with students, school staff, and families (see Tables E7 and E8). She or he is in a unique position to identify gaps in asthma care and knowledge and to address these needs through referral and education. Opportunities for asthma education occur in the school setting through both formal education programs and also through informal “teachable moments” with the student, staff, and parent/guardian. The degree of this education will vary depending on the role of the school staff and the amount of direct contact with the child. Regarding the education of the student with asthma, the school nurse is in a unique position to provide asthma education because school nurses have the education and knowledge to teach children about asthma, children spend a large portion of their day in school, and the school setting is associated with learning. There are multiple validated student asthma education programs available (see Table E11 in this article’s Online Repository at www.jacionline.org).
Finally, the school nurse is confronted with the task of advancing his or her own asthma knowledge. There are numerous online asthma resources that are summarized in the AAAAI School Nurse Asthma Toolbox contained within SAMPRO™ (www.aaaai.org/SAMPRO). One novel program is eSchoolCare, an online resource for school nurses to support managing chronic diseases in children, including asthma (http://son.wisc.edu/eSchoolCare.htm). School districts would also benefit from supporting school nurses in becoming certified asthma educators (www.naecb.com/).
COMPONENT 4
Addressing environmental triggers in SAMPRO™
Twenty percent of the US population spends the majority of the day in school buildings, and indoor air quality in the school setting has the ability to affect both children and the staff who care for them.30 Furthermore, poor indoor air quality has been shown to have a negative effect on health and well-being.31 It is imperative that a sustainable environmental program be initiated in every school to prevent unnecessary illness, school absences, lost time from work, and the associated academic and financial costs.
Schools can reduce exposure to environmental triggers through effective Indoor Air Quality (IAQ) management plans. According to the US Center for Disease Control and Prevention’s 2015 School Health Policies and Practices Study (www.cdc.gov/healthyyouth/data/shpps/index.html),32 46% of schools in the United States have implemented an IAQ management program. More than 34% of these schools use the Environmental Protection Agency (EPA)’s IAQ Tools for Schools, which provides schools with usable resources to manage programs and deliver education about healthy school environments (www.epa.gov/iaq/schools/managingasthma.html). These data indicate that many children with asthma are not protected by IAQ management programs. It is important that we continue to promote practices that reduce environmental asthma triggers and provide children a healthy and productive learning environment. The essential elements to include in any air quality program for school-based asthma management, including SAMPRO™, are described subsequently.
Pest control and green schools
Since 1996, the EPA has been working with schools to practice Integrated Pest Management (IPM). This approach encourages schools to avoid routine and scheduled applications of pesticides and favors a plan that requires initially evaluating the need for pesticide application. The 3 most commonly used strategies to control pests recommended by IPM are (1) sealing openings in walls, floors, doors, and windows with caulk or weather stripping; (2) storing food in plastic, glass, or metal containers with tight lids that are inaccessible to pests; and (3) applying pesticides by using spot treatment protocols and baiting pests versus widespread applications of pesticides (www.cdc.gov/healthyyouth/data/shpps/index.htm).
The majority of school districts (55%) require campus-wide pest inspections (ants, roaches, bees, mice, and/or rats) at a minimum of once a month. Notification of families of pesticide application varies widely, with 35% of schools required to notify families before pesticide use (www.cdc.gov/healthyyouth/data/shpps/index.htm). A significant percentage of schools only notify families of pesticide application annually (6.1%), and in 24% of schools, notifications are not required. In 2012, the EPA launched “School IPM 2015: a strategic plan for integrated pest management in schools in the United States.” This initiative calls for a 70% reduction in both pest complaints and pesticide use in schools. It relies on the coordinated efforts of teachers, custodians, food service staff, school administrators, pest management professionals, US Department of Agriculture Agricultural Extension staff, regulators, architects, and parents to reduce pesticide risk in our schools (http://www.epa.gov/pesticides/ipm/schoolipm2015.htm).
Commonly used school materials, such as floor coverings, furniture, paint, cleaners, and markers, emit chemical fumes or vapors and can vary in the amount of emissions produced. Increasing public interest is focused on creating “green” physical school environments that favor use of low-emitting materials and products. In 2014, more than half of schools have adopted policies to purchase low-emitting materials and green cleaning products.
IAQ protocols
The establishment of IAQ protocols is effective in limiting exposure to environmental triggers in school and promoting a sustainable program that promotes school environmental health. For over a decade, the EPA has been working with schools to promote IAQ practices by implementing “Indoor air quality tools for schools” (www.epa.gov/iaq/schools). During this time, the promotion of IAQ practices have raised awareness for the need to fund IAQ programs and to educate school personnel at the state, district, and school level regarding healthy indoor school environments.
Other types of periodic school inspections commonly required include inspection of (1) building foundation, walls, and roofs for cracks, leaks, or past water damage; (2) clutter that prevents effective cleaning and maintenance; (3) the plumbing system; and (4) condensation in and around the school facilities. Of the set of specific activities for preventing and resolving IAQ problems, 86% of schools conduct periodic inspections for mold, and 96.2% require periodic inspections of the heating, ventilation, and air conditioning systems. Importantly, 62.6% of schools have adopted a policy for addressing mold problems. Progress continues to be made to prevent exposure to harmful pollutants from vehicles. In 2014, 23% of schools have implemented an engine-idling reduction program for school buses, and 10% have implemented a program that included commercial vehicles, such as delivery trucks. Few schools (9%) have extended this program to personal vehicles, such as cars (www.cdc.gov/healthyyouth/data/shpps/pdf/shpps-508-final_101315.pdf).
The SAMPRO™ Workforce recommends that school personnel develop an IAQ management program, which is consistent with EPA recommendations, in their school or district that includes asthma management strategies. Use of the “Framework for effective school IAQ management” can improve the school environment by reducing exposure to pesticides, promote pest control, and decrease exposures to asthma triggers, including mold, dust mites, and diesel exhaust. These measures will safeguard children’s health by promoting a healthy school environment. Also, for interested subjects, using the School IAQ Assessment Mobile App can help to identify, solve, and prevent IAQ problems that can exacerbate asthma symptoms. Conducting a walkthrough of school buildings using the IAQ Tools for Schools Action Kit and the EPA checklists to determine whether asthma triggers exist is also recommended (www.epa.gov/iaq-schools/walk-through-inspection-checklist-indoor-air-quality-tools-schools). If triggers are found, a remediation plan should be developed and implemented. Components of a comprehensive school environment policy are listed in Table E12 in this article’s Online Repository at www.jacionline.org and include environmental assessment and monitoring, integrated pest management, and use of low-emitting products.
Environmental education for school staff
Staff development and training opportunities are essential for the successful implementation of policies and practices to promote healthy learning environments. Although the interest and need for professional training (workshops, conferences, and continuing education) is high, there is a clear lack of funding for such training. Less than 50% of districts have provided funding for professional development or offered professional development on indoor air quality, integrated pest management, and radon testing and mitigation. Given that custodial and maintenance staff are the “eyes, ears, and noses” of the school facility, the EPA recommends targeted training for this key stakeholder group. Furthermore, the use of practices limiting air pollutants continues to be an area in need of future work.
Empowering the school nurse to advocate for environmental change
One of the essential elements in managing health and the factors affecting school health is the presence of a professional school nurse. As a champion of a “healthy environment,” the school nurse can assemble an advisory team to plan and implement a coordinated environmental program for the school-based management of asthma. Ideally, the advisory team members should include the school nurse, a school administrator, a custodian, community members/parents, an education staff member, a nutrition service member, a health care provider, and representatives from other relevant community organizations. The components of the environmental program created by the advisory team should initially be communicated and periodically updated to health care providers.
Empowering members of the advisory team to advocate for the health of the school community is critical for the implementation and sustainability of the environmental management of asthma in the school setting. In addition, the advisory team might play an important role in obtaining information and educating families regarding harmful asthma triggers, such as tobacco smoke exposure (both active and passive), in the home. The advisory team should implement an environmental advocacy plan to students, parents, the school community, and health care providers in the community and the community at large by using the concepts reviewed above.
Outcomes of environmental action
Outcomes related to the school and home environment are 2-fold: (1) objective measures to determine whether there is a reduction of exposure to the school or home-based trigger(s); and (2) evaluation of any direct correlation in these reductions to improved health outcomes. Although the concept is standard and fundamental, there is a paucity of comprehensive data regarding the school-specific environment and asthma morbidity. This is likely due to the complexity of obtaining objective measures of exposures (dust, air, and surfaces) without significant funding. Nevertheless, well-established data on reductions in home environmental triggers and improved health outcomes can be a model to bridge our comprehensive understanding of the complexity between school and home triggers. Furthermore, simple inspection surveys and walkthrough protocols are low in cost and easily accessible.33 Simple, low-cost educational efforts can then be implemented as a starting point to reduce triggers, acknowledging that larger-scale interventions are hard to implement.
IMPLEMENTATION, DISSEMINATION, AND SUSTAINABILITY: PROGRAM FIDELITY AND ASSESSMENT
The SAMPRO™ Workforce discussed how to disseminate SAMPRO™ and ways in which the plan could be implemented and applied in diverse school systems, including systems with and without a school nurse. The participants were guided by principles of implementation and dissemination research34 and recommended a well-established, easy-to-use analytic framework to assess program effectiveness.35 The SAMPRO™ Workforce also considered both costs to school districts and time constraints, especially for school nurses. The SAMPRO™ Workforce recommended national legislation to raise awareness of the need for school-based asthma care support, as well as accelerate adoption of SAMPRO™. After the summit meeting, the AAAAI’s lobbyists were able to garner bipartisan support for this initiative and legislation that would support the 4 components of SAMPRO™, which has now been introduced in the US House of Representatives in the Energy and Commerce Committee as bill number HR4662. Finally, the SAMPRO™ Workforce discussed stewardship at the national, state, and local levels to maintain program quality and a system for evaluation to determine the reach and effectiveness of the program.
Stewardship
As previously described, SAMPRO™ was created with input from multiple stakeholder organizations (see Table E1) at an asthma summit that was conducted in October 2015 under the leadership of the AAAAI and the NASN. Within the next year, additional endorsement will be sought by multiple pediatric, family medicine, specialty, and nursing organizations and the National Education Association. All program-related materials will be available on a Web site and are free of charge (www.aaaai.org/SAMPRO). Patient/student materials will be available initially in English and Spanish; other languages can be added later. Registration to participate in SAMPRO™ is encouraged to help the AAAAI and NASN track use, confirm agreement to terms of use, facilitate follow-up communication, and provide outreach for technical assistance. Materials are divided into 4 components that enable a state or school district to have a fully developed program. Other supplemental tools include a toolbox to guide schools and school districts and states to implement the program, a sample business plan, steps to make the case for program adoption, and methods to measure effectiveness. SAMPRO™, which is located within the AAAAI infrastructure, will be continuously monitored and updated by a steering committee of stewards composed of the various summit group leaders and administrative AAAAI staff. SAMPRO™ will also provide reports and technical assistance for participating schools and school districts.
Dissemination and adoption
As stated previously, national legislation is currently being considered (Bill #HR4662) that will encourage states to implement the 4 components of SAMPRO™. The AAAAI through the Office of School-based Management for Asthma, NASN, and their national partners are working together to secure passage of this legislation and are committed to implementing this legislation through their local affiliates. Adoption of the SAMPRO™ components will be facilitated by the Office of School-based Management of Asthma, working through other key stakeholders, to provide states with guidance and examples of how to implement SAMPRO™ components in the legislation. The AAP is a key element that has already been developed as part of SAMPRO™. This plan is a student-specific authorization for medication administration by school personnel and parental consent for communication between the clinician and the school nurse into a single document. Although adoption of this AAP is recommended, the critical components of this plan can be added to existing state and district management plans for children with asthma. Additional materials will include information about how to identify potential schools, organize partners, engage local providers, and educate school nurses and providers.
Assessment and implementation fidelity
Assessment of SAMPRO™’s success will include both process and outcome measures at the local and national levels. Five important principles have been articulated to guide program evaluation.
Dissemination of a sustainable program is rooted in demonstration that the program is effective.
Program fidelity is essential to the determination of effectiveness.
The program must be of value to the school nurse and must be associated with a low burden for implementation and reporting if widespread adoption and sustainability are to be achieved. School nurses serve in only 81% of the nation’s public schools, leaving many students underserved, and advocating for a school nurse in every school might be critical.
The program must have sufficient flexibility to meet local needs without losing fidelity. In addition, there must be a balance between the time required by the nurse to administer proper asthma care and education versus the time the student is away from normal but essential classroom educational activities.
When possible, data reports should be standardized across school-based asthma programs to reduce burden.
Multiple analytic frameworks for the program were considered, and the analytic framework that has been chosen for the evaluation of the program is RE-AIM,36 which examines the reach, effectiveness, adoption, implementation, and maintenance of the program. Each component as it pertains to the national office and state and local school districts is shown in Table E13 in this article’s Online Repository at www.jacionline.org. At the national level, the reach will include the number of times the materials have been downloaded from the Web site and the number of different communities (by type) that have adopted any of the program elements. At the state level, reach will be assessed by examining the number of schools or school districts trained in the program and the number of students, schools, and school districts using the program. Effectiveness, both nationally and at the state level, will be assessed by using measures that school nurses or school districts often track, including missed school days, use of the school nurse’s office for albuterol administration not related to exercise, and the number of 911 calls for asthma emergencies. Tracking school absences specifically for asthma can be difficult, however, because the reason for a school absence is generally classified as excused or unexcused or possibly by some general category, such as medical or family trip. Attributing an absence to an asthma exacerbation, when available, is often in a “free text” field as opposed to a dropdown menu that makes it difficult to retrieve. Recent experience in Wisconsin when school nurses worked directly with the companies that create and maintain electronic School Information Systems showed that it is possible to collect attendance information for individuals and groups of students with a specific chronic condition and compare rates from selected time periods or from year to year (personal communication). Schools can also assess other outcome measures that are meaningful to their community, such as the nurse’s confidence in knowing when and how to administer albuterol during an emergency and the availability of stock albuterol in the office. These measures will be used for local, state, and national planning of educational activities to enhance program maintenance.
A second tier of data collection has also been created for those districts and states that have access to use data. To again minimize burden, 2 measures (ie, number of follow-up visits to the doctor’s office and number of filled controller medications) have been recommended as important indicators of family, nurse, and clinician interaction and medication adherence.
A system for collecting and using data at the local, state, and national levels is imperative in this process but can vary from state to state. Most school districts use a School Information System to manage information related to school matters (eg, attendance, classes, transcripts, and grades). Many of these systems have a health module in which asthma-related information could be entered and retrieved for subsequent analysis. Educating school nurses in the technology to design a query to yield the desired information might be necessary.
Webinars with states, school nurses, and school districts will be used to present SAMPRO™ and discuss how the program could be improved and how community needs could be better met by SAMPRO™. Programs at national meetings of the various stakeholders will be developed to promote dissemination by using program-specific data to maintain interest and support for SAMPRO™. Driven by evidence-based recommendations and the principles of dissemination and implementation science, the Office for School-based Management of Asthma at the AAAAI and its stakeholder partners could become the leader in school-based asthma health.
CONCLUSION
It is important to emphasize that the development of SAMPRO™ involved input and consensus from a variety of stakeholders with extensive knowledge and experience in school-based care for children with asthma. Thus it is a unique program based on the diversity of educational backgrounds of the persons who unselfishly and devotedly shared their expertise to create this resource. Importantly, the intentions behind the creation of SAMPRO™ were never to replace existing asthma education programs that are working well to improve asthma care in their communities. Rather, it was created to provide and disseminate tools that develop the circle of support for communities without this communication infrastructure. It is hoped that communities can work at the local, state, and national levels to implement, disseminate, and sustain the 4 components of SAMPRO™ so that children with asthma will get the best care possible in their school environments.
Supplementary Material
Acknowledgments
Supported by funds provided by the American Academy of Allergy, Asthma & Immunology and the National Association of School Nurses.
Abbreviations
- AAAAI
American Academy of Allergy, Asthma & Immunology
- AAP
Asthma Action Plan
- AEP
Asthma Emergency Treatment Plan
- AMP
Asthma Management Plan
- EHR
Electronic health record
- EPA
Environmental Protection Agency
- IAQ
Indoor Air Quality
- IPM
Integrated Pest Management
- NASN
National Association of School Nurses
- SAMPRO™
School-based Asthma Management Program
- SBHC
School-based health center
Footnotes
This statement was endorsed by the American Academy of Pediatrics; the American College of Allergy, Asthma & Immunology; the American Thoracic Society; the Allergy & Asthma Network; and the National Association of School Nurses.
Disclosure of potential conflict of interest: R. F. Lemanske has received travel support from the American Academy of Allergy, Asthma & Immunology (AAAAI); is employed by the University of Wisconsin; has received grants from the National Heart, Lung, and Blood Institute (NHLBI) and Pharmaxis; has received royalties from Elsevier and UpToDate; and has received speaker honoraria from the Kuwait Allergy Society, Lurie Children’s Hospital, Boston Children’s Hospital, Health Star Communications, LA Children’s Hospital, Northwestern University, the Asthma and Allergy Foundation of America–Alaska Chapter, and the Egyptian Allergy Society. S. Kakumano has received royalties from UpToDate. K. Shanovich has received travel support, payment for writing or reviewing the manuscript, and employment from the AAAAI. N. Antos received travel support from the AAAAI School Based Management of Asthma Summit. M. M. Cloutier has received travel support from the AAAAI; has consultant arrangements with ProHealth Physicians; has received grants from the National Institutes of Health, the NHLBI, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development; and has received payment for lectures from Nationwide. S. Szefler has consultant arrangements with Roche, AstraZeneca, Aerocrine, Daiichi Sankyo, Boehringer Ingelheim, Genentech, and Novartis and has received grants from GlaxoSmithKline. P. Williams has received travel support from the AAAAI and is employed by Northwest Asthma & Allergy Center. The rest of the authors declare that they have no relevant conflicts of interest.
The following were active participants at the Summit meeting that led to the development of SAMPRO™ and all of its components. The AAAAI and NASN would like to express their sincere gratitude for their scholarly and tireless contributions to this project: Freddi Adelson (Department of Public Instruction, State of Wisconsin); Marty Alemán (Olmsted County Public Health Services); Dr Gail Allen (University of Wisconsin School of Medicine and Public Health); Laura Allen (Montgomery County Department of Health and Human Services, Public Health Services); Dr Eric S. Armbrecht (Saint Louis University, Center for Health Outcomes Research); Margaret Beall (National Education Association, Healthy Futures Board of Directors and National Education Association Board of Directors); Marjorie Cole (Missouri Department of Health and Senior Services and National Association of Chronic Disease Directors, School Health Steering Committee); Mary Ellen Conley (Abington Public School and Asthma and Allergy Foundation of America); Deb Cook (Kennett Public Schools, Missouri); Brenda Doroski (US Environmental Protection Agency); Dr Cheryl D. De Pinto (American Academy of Pediatrics); Dr Kurt Elward (American Academy of Family Physicians); Dr Michael Foggs (American College of Allergy, Asthma and Immunology); Dr Michelle Freemer (National Heart, Lung and Blood Institute); Dr Paul Garbe (Centers for Disease Control and Prevention); Dr Peter Gergen (National Institute of Allergy and Infectious Disease, National Institutes of Health); Melanie Gleason (Children’s Hospital of Colorado, Breathing Institute); Kristen Grimes (Children’s Health Alliance of Wisconsin); Christy Haas-Howard (Denver Public Schools, Department of Nursing & Student Health Services); Dr Seiji Hayashi (Unity Health Care); Dr Jessica Hollenbach (Connecticut Children’s Asthma Center); Kayla Jackson (American Association of School Administrators); Evilia Jankowski (Asthma Initiative of Michigan [AIM]); Dr Eileen Kintner (Luci Baines Johnson Fellow in Nursing, the University of Texas at Austin, School of Nursing); Lisa Klotzbach (Public Health Informatics, Olmstead County Public Health Service; Dr Pamela Luna (American Public Health Association); Tabatha Magobet (National Association for the Advancement of Colored People); Beth Mattey (National Association of School Nurses); Dr Erin Maughan (National Association of School Nurses); Lisa Meadows (St Louis Children’s Hospital); Dr Giselle Mosnaim (Rush University Prevention Center); Lynn Morrison (Washington Health Advocates); Katherine Pruitt (American Lung Association); Dr Gary Rachelefsky (American Academy of Allergy, Asthma & Immunology); Gayle Rieland (Minneapolis Public Schools); Sally Schoessler (Allergy & Asthma Network); Valerie Schend (University of Wisconsin School of Pharmacy, Department of Asthma, Allergy & Pulmonary Clinical Research); Rachael L. Tracy (National Heart, Lung, and Blood Institute); and Paul Tremblay (University of Rochester, New York).
References
- 1.Akinbami L. Centers for Disease Control and Prevention National Center for Health Statistics. The state of childhood asthma, United States, 1980–2005. Adv Data. 2006:1–24. [PubMed] [Google Scholar]
- 2.Committee NSB. Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma—summary report 2007. J Allergy Clin Immunol. 2007;120(suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 3.Bruzzese JM, Evans D, Kattan M. School-based asthma programs. J Allergy Clin Immunol. 2009;124:195–200. doi: 10.1016/j.jaci.2009.05.040. [DOI] [PubMed] [Google Scholar]
- 4.Cicutto L, Gleason M, Szefler SJ. Establishing school-centered asthma programs. J Allergy Clin Immunol. 2014;134:1223–30. doi: 10.1016/j.jaci.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Hollenbach JP, Cloutier MM. Implementing school asthma programs: lessons learned and recommendations. J Allergy Clin Immunol. 2014;134:1245–9. doi: 10.1016/j.jaci.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Kuhn L, Reeves K, Taylor Y, Tapp H, McWilliams A, Gunter A, et al. Planning for action: the impact of an asthma action plan decision support tool integrated into an electronic health record (EHR) at a large health care system. J Am Board Fam Med. 2015;28:382–93. doi: 10.3122/jabfm.2015.03.140248. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez E, Rivera DA, Perlroth D, Becker E, Wang NE, Landau M. School nurses’ role in asthma management, school absenteeism, and cost savings: a demonstration project. J Sch Health. 2013;83:842–50. doi: 10.1111/josh.12102. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics Council on School Health. Magalnick H, Mazyck D. Role of the school nurse in providing school health services. Pediatrics. 2008;121:1052–6. doi: 10.1542/peds.2008-0382. [DOI] [PubMed] [Google Scholar]
- 9.Moricca ML, Grasska MA, BMarthaler M, Morphew T, Weismuller PC, Galant SP. School asthma screening and case management: attendance and learning outcomes. J Sch Nurs. 2013;29:104–12. doi: 10.1177/1059840512452668. [DOI] [PubMed] [Google Scholar]
- 10.Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120:e887–94. doi: 10.1542/peds.2006-2314. [DOI] [PubMed] [Google Scholar]
- 11.Webber MP, Carpiniello KE, Oruwariye T, Lo Y, Burton WB, Appel DK. Burden of asthma in inner-city elementary schoolchildren: do school-based health centers make a difference? Arch Pediatr Adolesc Med. 2003;157:125–9. doi: 10.1001/archpedi.157.2.125. [DOI] [PubMed] [Google Scholar]
- 12.Liao O, Morphew T, Amaro S, Galant SP. The Breathmobile: a novel comprehensive school-based mobile asthma care clinic for urban underprivileged children. J Sch Health. 2006;76:313–9. doi: 10.1111/j.1746-1561.2006.00119.x. [DOI] [PubMed] [Google Scholar]
- 13.Morphew T, Scott L, Li M, Galant SP, Wong W, Garcia Lloret MI, et al. Mobile health care operations and return on investment in predominantly underserved children with asthma: the breathmobile program. Popul Health Manag. 2013;16:261–9. doi: 10.1089/pop.2012.0060. [DOI] [PubMed] [Google Scholar]
- 14.Bergman DA, Sharek PJ, Ekegren K, Thyne S, Mayer M, Saunders M. The use of telemedicine access to schools to facilitate expert assessment of children with asthma. Int J Telemed Appl. 2008;159276 doi: 10.1155/2008/159276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frey S, Fagnano M, Halterman J. Medication identification among caregivers of urban children with asthma. Acad Pediatr. 2016 doi: 10.1016/j.acap.2016.04.005. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell JD, Brooks M, Hosokawa P, Robinson J, Song L, Krieger J. Community health worker home visits for Medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015;105:2366–72. doi: 10.2105/AJPH.2015.302685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanson TK, Aleman M, Hart L, Yawn B. Increasing availability to and ascertaining value of asthma action plans in schools through use of technology and community collaboration. J Sch Health. 2013;83:915–20. doi: 10.1111/josh.12110. [DOI] [PubMed] [Google Scholar]
- 18.Borowsky B, Little A, Cataletto M. Determining the relative burden of childhood asthma at the local level by surveying school nurses. Pediatr Allergy Immunol Pulmonol. 2013;26:76–80. doi: 10.1089/ped.2013.0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moonie S, Sterling DA, Figgs LW, Castro M. The relationship between school absence, academic performance, and asthma status. J Sch Health. 2008;78:140–8. doi: 10.1111/j.1746-1561.2007.00276.x. [DOI] [PubMed] [Google Scholar]
- 20.Yoos HL, Kitzman H, Henderson C, McMullen A, Sidora-Arcoleo K, Halterman JS, et al. The impact of the parental illness representation on disease management in childhood asthma. Nurs Res. 2007;56:167–74. doi: 10.1097/01.NNR.0000270023.44618.a7. [DOI] [PubMed] [Google Scholar]
- 21.Huffaker M, Phipatanakul W. Introducing an environmental assessment and intervention program in inner-city schools. J Allergy Clin Immunol. 2014;134:1232–7. doi: 10.1016/j.jaci.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yin HS, Gupta RS, Tomopoulos S, Wolf MS, Mendelsohn AL, Antler L, et al. Readability, suitability, and characteristics of asthma action plans: examination of factors that may impair understanding. Pediatrics. 2013;131:e116–26. doi: 10.1542/peds.2012-0612. [DOI] [PubMed] [Google Scholar]
- 23.Chute CG, Hart LA, Alexander AK, Jensen DW. The Southeastern Minnesota Beacon Project for Community-driven Health Information Technology: origins, achievements, and legacy. EGEMS (Wash DC) 2014;2:1101. doi: 10.13063/2327-9214.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Voigt C, Torzewski S. Direct results. An HIE tests simple information exchange using the direct project. J AHIMA. 2011;82:38–41. [PubMed] [Google Scholar]
- 25.Richmond CM, Hobson A, Pike E, Kleiss J, Wottowa J, Sterling DA. Breathe Your Best for School Success: evaluation of an initiative to enhance asthma action plans in the school setting. J Urban Health. 2011;88(suppl 1):68–72. doi: 10.1007/s11524-010-9478-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson KH, Guthrie S. Harnessing the power of student health data: selecting, using, and implementing electronic school health documentation systems. NASN Sch Nurse. 2012;27:26–33. doi: 10.1177/1942602X11429828. [DOI] [PubMed] [Google Scholar]
- 27.Abramson MJ, Bailey MJ, Couper FJ, Driver JS, Drummer OH, Borbes AB, et al. Are asthma medications and management related to deaths from asthma? Am J Respir Crit Care Med. 2001;163:12–8. doi: 10.1164/ajrccm.163.1.9910042. [DOI] [PubMed] [Google Scholar]
- 28.Cowie RL, Revitt SG, Underwood MF, Field SK. The effect of a peak flow-based action plan in the prevention of exacerbations of asthma. Chest. 1997;112:1534–8. doi: 10.1378/chest.112.6.1534. [DOI] [PubMed] [Google Scholar]
- 29.Hunt P, Barrios L, Telljohann SK, Mazyck D. A whole school approach: collaborative development of school health policies, processes, and practices. J Sch Health. 2015;85:802–9. doi: 10.1111/josh.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.A Guide to Implementing an IAQ Indoor Air Quality: IAQ Tools for Schools Action Kit. Available at: https://www.epa.gov/iaq-schools/guide-implementing-iaq-indoor-air-quality-iaq-tools-schools-action-kit. Accessed July 21, 2016.
- 31.The inside story: a guide to indoor air quality. 2015 Available at: http://www2.epa.gov/indoor-air-quality-iaq/inside-story-guide-indoor-air-quality. Accessed July 21, 2016.
- 32.Results from the School Health Policies and Practice Study. Atlanta: Centers for Disease Control and Prevention; 2012. Available at: http://www.cdc.gov/HealthyYouth/shpps/index.htm. Accessed July 21, 2016. [Google Scholar]
- 33.Tortolero SR, Bartholomew LK, Tyrrell S, Abramson SL, Sockrider MM, Markham CM, et al. Environmental allergens and irritants in schools: a focus on asthma. J Sch Health. 2002;72:33–8. doi: 10.1111/j.1746-1561.2002.tb06509.x. [DOI] [PubMed] [Google Scholar]
- 34.Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43:337–50. doi: 10.1016/j.amepre.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Briggs AH, Bousquet J, Wallace MV, Busse WW, Clark TJ, Pedersen SE, et al. Cost-effectiveness of asthma control: an economic appraisal of the GOAL study. Allergy. 2006;61:531–6. doi: 10.1111/j.1398-9995.2006.01038.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


