Abstract
Idiopathic spinal cord herniation (ISCH) is a rare cause of progressive spinal myelopathy, which frequently presents as Brown-Sequard syndrome. A 50 year old woman consulted for difficulty in walking. On examination, the patient reported sensory deficit of temperature on the left side, associated with diminished anal sensitivity. Nine months before consultation, a walking disorder began disturbing the activities of everyday life. A single case report with surgical treatment outcome. Idiopathic spinal cord herniation is a potentially treatable condition, which should be diagnosed early and treated. The surgical operation contributed clinical improvement in functional autonomy with modification in McCormick classification in our patient. Despite the existence of growing number of ISCH cases in the literature, misdiagnosis and choice of treatment remains a major concern. SCH is a rare clinical entity that seems to be increasing with the accessibility of MRI imaging. Preoperative diagnosis can be made with magnetic resonance imaging (MRI). ISCH should be considered as differential diagnosis of Brown-Sequard syndrome, especially after fourth decade of life. Although progression of neurologic deficits can be gradually slow, reducing surgically the cord hernia and repair of the defect are vital factors in preventing the deterioration and display reversible improvement. In recent reviews, patients who underwent surgery had better outcomes as with our case.
Keywords: Brown-Sequard syndrome, Myelopathy, Idiopathic Spinal cord herniation, Duraplasty
Introduction
Idiopathic spinal cord herniation (ISCH) is a rare cause of progressive myelopathy described as displacement of the spinal cord out of the dural sac through a defect usually anteriorly or anterolateral in the Dura mater. (1,2) The first reported case was by Wortzman in 1974. (3) In the last decade, the frequency of reports of ISCH in the literature has increased. Most arguments favor surgical indication, with several different procedures proposed wether closing the defect with a dural substitute or direct suture. (4, 5)
Case
A 50 year old woman consulted for diffculty walking, requiring the use of two crutches for 3 years. Examination revealed a decrease in motor power of the right lower limb associated with sharp reflexes, and right Babinski sign. Associated with decresed pain and temperture sensation on the left side of the body up to T4. In summary, the patient had a Brown-Sequard syndrome secondary to a spinal myelopathy.
Results
Initially a laminectomy performed, followed by medial durotomy to repostion the cord and repair the dural defect to avoid relapse. We observed a right ventro-lateral defect of the dura mater through which the spinal cord is a engaged towards the posterior surface of the vertebral body. A surgical artificial dural membrane was introduced between the herniated portion of the cord and the dural defect. The anterior part of spinal cord protected and preserved by interposeing lyophilized patch fixed by PROLENE 5/0 (Figure 2) at the defect level. At discharge, the patient’s neurological examination revelead a motor improvement, and occasionally she only needed a single cane to walk rather then two.
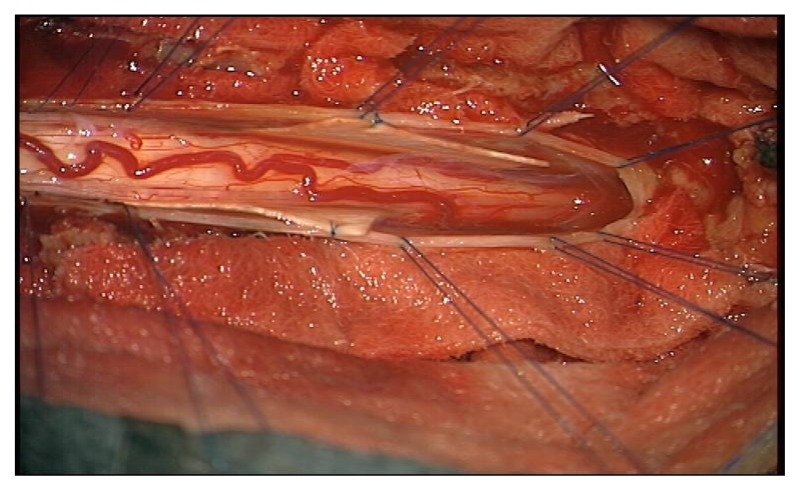
Figure 2.
Intraoperative photograph showing the complementary addition of the dural patch between the spinal cord and the dura mater.
Discussion
The spinal cord hernia is a rare entity with no well-defined theory, causing multiple publications involving different view points over the past few years. (1–22) The duration of symptoms before any treatment was often very long, 4 years on average. Our patient has been treated for upper thoracic spinal cord herniation with a dural repair procedure. Furthermore, the surgical opertion contributed clinical improvement of functional autonomy and enhanced modification in McCormick classification for our patient who had previous history of clinical deteriation. Our case was at the T3 level. After 6 months, the clinical condition remained stable with improvement in functional autonomy to grade 2 according to McCormick. MRI confirmed the resolution of the deformation of the spinal cord (Figure 3).
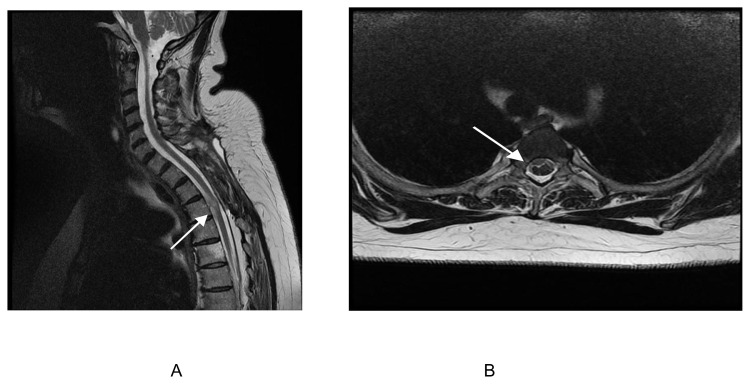
Figure 3.
(A) postoperative MRI (T2 sagittal) showing a return to physiological position of the spinal cord, and reappearance of CSF flow anterior to the cord which no longer appears to be attached to the vertebral body (arrow). (B) postoperative MRI (axial section).
Conclusion
The pathogensis of spinal cord hernia has not been clearly established, but it is assumed as result of collaboration between the biomechanism and congenital development process. The magnetic resonance imaging (MRI) is the choice of imaging used in the diagnosis, in which the pathology is spotted clearly as a “gooseneck” appearance. The surgery consists of a posterior laminectomy initial approach, and then duraotomy. Surgical treatment seems to have un upper hand as the choice of the management by most groups.(1–5) The time intravel between diagnosis and surgery could be a very essential predicative factor in treatment results.
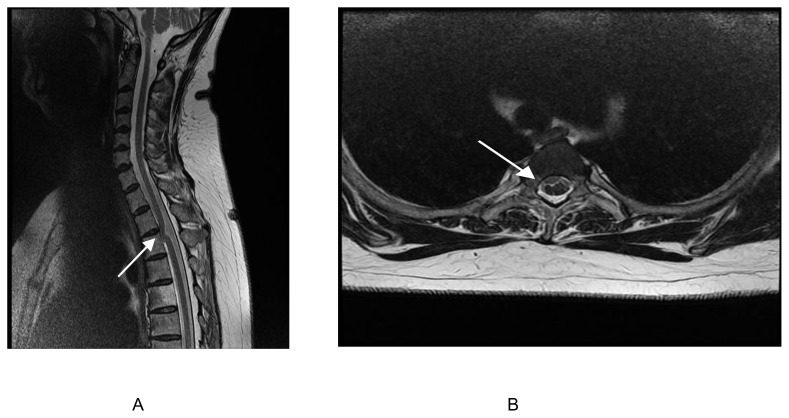
Figure 1.
(A): Preoperative MRI (T2 sagittal) showing the anterior displacement of the cord, with enlargement of the retro medullary space at T3 (arrow). (B): Preop. MRI (T2 axial) showing the spinal cord drawn forward and the outside right.
References
- 1.Cellerini M, Bayon S, Scazzeri F, Mangiafico S, Amantini A, Guizzardi GC, et al. Idiopathic spinal cord herniation: a treatable cause of Brown-Séquard syndrome. Acta Neurochir. 2002;144:321–325. doi: 10.1007/s007010200044. [DOI] [PubMed] [Google Scholar]
- 2.Massicotte EM, Montanera W, Ross Fleming JF, Tucker WS, Willinsky R, TerBrugge K, et al. Idiopathic spinal cord herniation: report of eight cases and review of the literature. Spine. 2002;27:E233–41. doi: 10.1097/00007632-200205010-00025. [DOI] [PubMed] [Google Scholar]
- 3.Wortzman G, Tasker RR, Rewcastle NB, Richardson JC, Pearson FG. Spontaneous incarcerated herniation of the spinal cord into a vertebral body: A unique cause of paraplegia: Case report. J Neurosurg. 1974;41:631–5. doi: 10.3171/jns.1974.41.5.0631. [DOI] [PubMed] [Google Scholar]
- 4.Spissu A, Peltz MT, Matta G, Cannas A. Traumatic transdural spinal cord herniation and the nuclear trail sign: Case report. Neurol Sci. 2004;25:151–3. doi: 10.1007/s10072-004-0251-2. [DOI] [PubMed] [Google Scholar]
- 5.Darbar A, Krishnamurthy S, Holsapple JW, Hodge CJ., Jr Ventral thoracic spinal cord herniation: Frequently misdiagnosed entity. Spine (Phila Pa 1976) 2006;31:E600–E605. doi: 10.1097/01.brs.0000229247.69171.a1. [DOI] [PubMed] [Google Scholar]