Abstract
Streptococcus gallolyticus subsp. pasteurianus is an under-recognized pathogen and zoonotic agent causing opportunistic infections in humans. Despite increasing recognition of this subspecies as a cause for human infectious diseases, limited information is known about its antibiotic resistance mechanism. In this study, we aim to identify the molecular mechanism underlying the high macrolide resistance of six S. gallolyticus subsp. pasteurianus isolates from dead ducklings collected in several natural outbreaks in China during 2010–2013. All isolates exhibited multi-drug resistance including high macrolide resistance (MIC ≥ 1024 mg/L for erythromycin, and 512 mg/L for clarithromycin). Efflux-encoding mefA and mefE genes were not detectable in these isolates. The presence of 23S rRNA mutations in specific isolates did not significantly change macrolide MICs. No nucleotide substitutions were found in genes encoding ribosomal proteins L4 or L22. The ermB and ermT genes were found in the genomes of all isolates. These two genes were acquired independently in one highly virulent isolate AL101002, and clustered with Tn916 and IS1216, respectively. The expression of both ermB and ermT in all isolates was erythromycin inducible and yielded comparable macrolide MICs in all six isolates. Taken together, inducible expression of both ermB and ermT conferred high macrolide resistance in these S. gallolyticus subsp. pasterianus isolates. Our findings reveal new macrolide resistance features in S. gallolyticus subsp. pasteurianus by both ermB and ermT.
Keywords: Streptococcus gallolyticus subsp. pasteurianus, ermB, ermT, macrolide
1. Introduction
Streptococcus gallolyticus subsp. pasteurianus is a member of the group D streptococci. It was previously named Streptococcus bovis biotype II/2, based on its ability to decarboxylate gallate, to produce β-galactosidase and β-glucuronidase, and inability to ferment mannitol or produce trehalose [1,2]. However, owing to frequent ambiguity in S. bovis taxonomy following these phenotypic characterizations, S. bovis biotype II/2 was renamed to S. gallolyticus subsp. pasteurianus according to its genetic properties [3,4], and became one of the three subspecies of S. gallolyticus along with S. gallolyticus subsp. gallolyticus and S. gallolyticus subsp. macedonicus [4].
The ambiguity of S. bovis taxonomy led to limited clinical study on S. gallolyticus subsp. pasteurianus, and it is thus considered as an underreported opportunistic pathogen in both animals and humans. It can cause meningitis in ducklings and septicemia in pigeons, goslings and turkey poults, leading to high mortality in these poultries [5,6,7,8]. In humans, it is increasingly recognized as a cause of infant meningitis and bacteremia [9,10,11,12], and 58.7% of mortality rate has been observed with one-year neonates relating to this subspecies [13]. In adults, it is linked to a wide spectrum of diseases, including meningitis [14], endocarditis [15,16,17], splenic abscess [18], biliary and urinary tract infection [15,19,20,21], as well as gastric, pancreatic, hepatobiliary and colorectal cancers [16,22]. Death cases in adults were also reported in association with infections by this subspecies. Thus far, infections regarding this subspecies have been noted in many countries and regions, including Mainland China, Hong Kong, Taiwan, USA, France, Amsterdam, Spain, Netherlands, Japan, Korea, etc. [9,17,21,23,24,25,26,27,28].
Macrolides are often used to treat infections caused by Gram-positive pathogens or Gram-negative cocci. They are also considered as alternative choices for patients with penicillin allergy. However, macrolide resistance has emerged in S. gallolyticus [22,29,30,31]. In Gram-positive bacteria, active efflux and 23S rRNA modification are two major mechanisms responsible for macrolide resistance [32,33]. Active macrolide efflux has been reported in streptococci [34,35], and it is mediated by a membrane protein encoded by the mefA or mefE gene. Alternatively, 23S rRNA modification confers macrolide-lincosamide-streptogramin B (MLS) resistance. Although this resistance can involve mutations within the L4 and L22 ribosomal proteins or 23S rRNA [36], it is generally conferred by 23S-rRNA methylating Erm enzymes. The methyl group at A2058 of 23S rRNA transferred by Erm proteins sterically disrupts the binding between macrolides and rRNA, thus rendering bacteria resistance [37]. Expression of MLS resistance in streptococci can be either constitutive or inducible [38,39]. Indeed, resistance in reported S. gallolyticus isolates was either caused by the presence of ermB gene [30], ermT gene [31], or to a lesser extent mefA gene [29,30]. While roughly 63% of clinical isolates from Taiwan were macrolide resistant [22,32], very limited information is known about the molecular mechanism of antibiotic resistance in S. gallolyticus subsp. pasteurianus. Thus far, the only mechanistic characterization of antibiotic resistance in this subspecies indicated that the presence of ermT [32] is responsible for macrolide resistance in 60 isolates from Taiwan. To further our understanding and facilitate clinical treatment of infections associated with this subspecies, this study aims to identify the molecular mechanism underlying the high macrolide resistance in the six isolates of S. gallolyticus subsp. pasteurianus from China.
2. Results
2.1. All S. gallolyticus subsp. pasteurianus Isolates Were Multi-Drug Resistant, with High Level Macrolide Resistance
All six isolates were identified as S. gallolyticus subsp. pasteurianus using biochemical characterization and 16S rRNA gene sequencing (Supplementary materials, Table S1, Figure S1). Using the agar dilution method recommended by CLSI [40,41], the MICs of these isolates were determined using ATCC 43144 and ATCC 29213 as controls. MICs of penicillin, cefotaxime and vancomycin for all isolates were smaller than individual breakpoints [40], indicating susceptible or intermediate category of all six isolates to these antibiotics (Table 1). While some isolates demonstrated resistance to chloramphenicol (2/6), levofloxacin (4/6) and gentamicin (3/6), all isolates were resistant to tetracycline (MIC = 25 mg/L (2/6), or >128 mg/L (4/6)), and to lincomycin (MIC ≥ 128 mg/L). Interestingly, all isolates were highly resistant to both erythromycin (MIC ≥ 1024 mg/L) and clarithromycin (MIC = 512 mg/L) (Table 1). The data indicated that all S. gallolyticus subsp. pasteurianus isolates were multi-drug resistant (MDR) and exhibited high macrolide resistance.
Table 1.
Minimum inhibitory concentrations of six S. gallolyticus subsp. pasteurianus isolates.
| Antibiotics | MIC (mg/L) of Subspecies | |||||||
|---|---|---|---|---|---|---|---|---|
| AL 101002 | GX 130304 | GX 130307 | GX 130630 | GX 130723 | GX 130809 | ATCC 43144 | ATCC 29213 | |
| Erythromycin | 1024 | 1280 | 1280 | 1280 | 1280 | 1024 | <0.25 | 0.25 |
| Clarithromycin | 512 | 512 | 512 | 512 | 512 | 512 | <0.25 | 0.25 |
| Lincomycin | 128 | >256 | >256 | 256 | 128 | 256 | 0.5 | 0.5 |
| Tetracyclin | 25 | 128 | 128 | 25 | 256 | 256 | 1 | 0.5 |
| Chloramphenicol | 2 | 32 | 32 | 2 | 2 | 2 | 2 | 2 |
| Levofloxacin | 8 | 8 | 4 | 8 | 4 | 8 | 4 | 0.25 |
| Gentamycin | 1 | 8 | 8 | 1 | 512 | 0.5 | 8 | 0.5 |
| Penicillin | 0.25 | 0.25 | 0.25 | 0.25 | 0.25 | 0.25 | 0.25 | 2 |
| Cefotaxime | 0.25 | 0.25 | 0.25 | 0.25 | 0.25 | 0.125 | <0.0625 | 2 |
| Vancomycin | <1 | <1 | <1 | <1 | <1 | <1 | <1 | 2 |
2.2. The High Macrolide Resistance Was neither Mainly Caused by Efflux Pump nor by Mutations within L4, L22, or 23S rRNA
In order to identify the molecular mechanism of high macrolide resistance in these isolates, we first tried to isolate plasmid DNA from these isolates. Interestingly, no plasmid was extracted from the isolates. PCR was then done to amplify known macrolide resistance determinants from genomic DNAs. The results revealed the absence of mefA and mefE genes (Table S2). This conclusion was also confirmed by whole genome sequencing of AL101002 (Genbank accession number LJPL00000000). These data demonstrated that mefA and mefE efflux pumps did not account for the high macrolide resistance in these isolates.
Since mefA and mefE efflux pumps were not the cause of high macrolide resistance, we further tested if L4 and L22 ribosomal proteins or 23S rRNA carried any mutations. The rplD and rplV genes encoding ribosomal proteins L4 and L22, respectively, were PCR-amplified and sequenced. In all isolates, sequence analysis did not reveal any nucleotide substitutions within these two genes, using rplD and rplV sequences from macrolide-susceptible ATCC 43144 as references. Additional PCRs to amplify 23S rRNA gene followed by DNA sequencing revealed nucleotide substitutions within 23S rRNA in all isolates. Taken together, these mutations included U2828C, G1355U, A1384G, A1490G and C2880U according to E. coli 23S rRNA numbering. Nevertheless, these mutations only produced MICs ≤ 32 mg/L (Table 2), as tested in BL21DE3 carrying individual mutant 23S rRNA. The MIC values were much lower than those observed in the six isolates (Table 1). Thus, neither ribosomal protein mutations in L4 or L22, nor nucleotide changes in 23S rRNA were mainly responsible for high resistance to macrolides in these isolates.
Table 2.
MICs of macrolides contributed by nucleotide substitutions in 23S rRNA.
| Mutation in 23S rRNA | Found in Isolates | Location in 23S rRNA | MIC (mg/L) | ||
|---|---|---|---|---|---|
| S. pasteurianus Numbering | E. coli Numbering | Erythromycin | Clarithromycin | ||
| Wild Type | ATCC 43144 | 1 | 1 | ||
| U2824C | U2828C | AL101002 | Domain VI | 1 | 4 |
| GX130307 | |||||
| GX130630 | |||||
| GX130809 | |||||
| C2876U | C2880U | GX130723 | Domain VI | 2 | 8 |
| U2824C + C2876U | U2828C + C2880U | GX130723 | Domain VI | 4 | 16 |
| G1380U + A1409G + A1515G | G1355U + A1384G + A1490G | GX130304 | Domain III | 32 | 32 |
2.3. The ermB and ermT Genes Were Integrated into All Isolate Genomes
As efflux or mutations within L4, L22 or 23S rRNA did not play a major role for the high macrolide resistance of the six isolates, we then attempted to amplify erm genes responsible for 23S rRNA methylation, including ermA, ermB, ermC, ermT and ermTR. Among these erm genes, fragments matching only ermB and ermT were detected in the genomes of all isolates and confirmed by DNA sequencing (Table S2). PCR also detected the presence of tetM and tetL genes in all isolates (Table S2), which may explain the observed tetracycline resistance in these isolates (Table 1).
To further validate the presence of ermB and ermT genes and to elucidate the composition of the resistance gene cluster, whole genome sequencing (WGS) was performed for AL101002, a previously characterized subspecies [5]. The WGS yielded 23 contigs (Genbank accession number LJPL00000000). The 16S rDNA resides in Contig 15 and matches exactly with that from ATCC 43144, further supporting species identification in present study (Supplementary materials, Table S1, Figure S1). The flanking sequences of ermB and ermT were further identified by DNA sequencing in combination with cloning of PCR fragments. The sequencing data revealed two antibiotic resistance gene clusters of 5.731 and 11.244 kb (Genbank accession number KU511281 and KU511280), respectively. The 5′ portion of the 5.731 kb fragment encodes an ABC-type transporter, a putative conjugative transposon protein, and a leader peptide, followed by ermB. Downstream of ermB, it consisted of genes for a putative RNA polymerase σ factor, Tn916-like excisionase and integrase, along with a truncated α/β superfamily hydrolase (Figure 1A). This fragment shared 98% nucleotide identity with one fragment from Clostridium difficile 630 (accession number AM180355), a human pathogen with MDR, suggesting the possibility in exchanging resistance elements between these two types of pathogens.
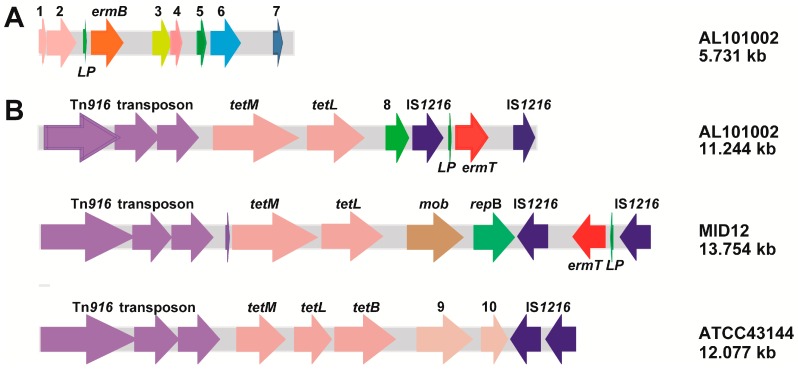
Figure 1.
Resistance gene clusters in AL101002: (A) A 5.731-kb fragment harboring ermB. It is composed of: ABC-type transporter (1 and 2); ermB, putative RNA polymerase σ factor (3); Tn916-like transposon (4); excisionase (5); and integrase (6). Arrow 7 indicates a fragment (nt 799772–800524) of ATCC 43144 genomic DNA (Genbank accession number AP012054); (B) An 11.244-kb resistance gene cluster. It consists of Tn916, tetM, tetL, mob, repB, and IS1216-ermT-IS1216 sandwich sequence. The numbers 8, 9 and 10 designate a plasmid replication protein, a plasmid recombination enzyme and a truncated plasmid replication initiation protein, respectively.
The 11.244 kb fragment harbored the ermT gene sandwiched by a 3′ portion of IS1216 insertion sequence (Figure 1B). Interestingly, a leader peptide was also located upstream of ermT. Within the upstream region a long fragment carried the Tn916 transposon followed by tetM and tetL. In addition, a plasmid replication gene was found between tetL and the upstream IS1216. This resistance gene cluster exhibited 99% and 98% nucleotide identity with part of uncultured bacterium MID12 (accession number GU951538) and human isolate ATCC 43144 genome (accession number AP012054), respectively. The sequence identity was mainly composed of Tn916 elements and tetracycline resistance, in addition to genes involved in plasmid replication. Variation was noted in the downstream portion of the fragment. While macrolide resistance genes were not found in ATCC 43144, ermT was integrated into this fragment in AL101002. This is similar to MID12, yet the sandwich sequence containing ermT and IS1216 elements in AL101002 were reversed as compared with that in MID12 (Figure 1B).
2.4. Both ermB and ermT Were Expressed in the Isolates, and the Expression Was Erythromycin-Inducible
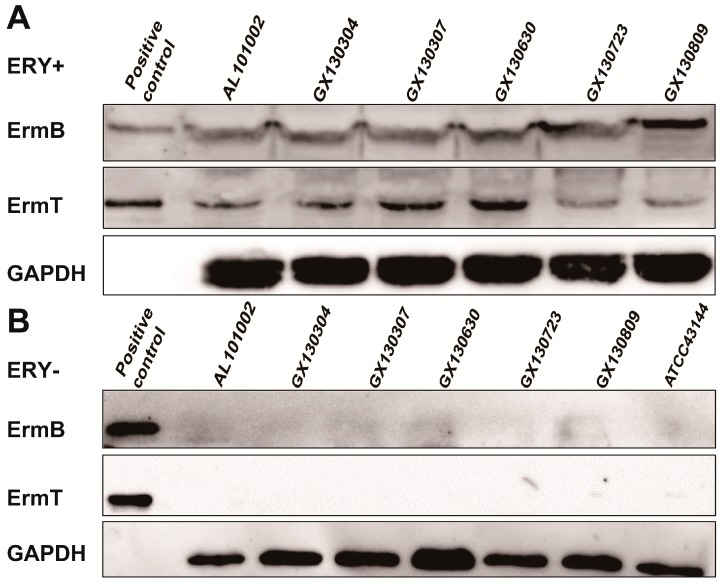
As genes in a genome may not be expressed, we further tested whether ermB and ermT genes in these isolates were expressed by Western blot (Figure 2), using in-house generated mouse serum against purified recombinant ErmB or ErmT proteins (Supplementary materials). With erythromycin, both ermB and ermT were expressed in all six isolates (Figure 2A), while without erythromycin, no ErmB or ErmT protein was detected (Figure 2B). The faint band without erythromycin could be due to non-specific recognition, as it also showed up in ATCC 43144, which does not contain any erm genes [31]. Additional control experiments did not reveal cross recognition of the serums for the two recombinant proteins. The data suggested that the expression of the two genes was erythromycin-inducible.
Figure 2.
Erythromycin-inducible expression of ermB and ermT: (A) ErmB and ErmT protein expression in six isolates with erythromycin; and (B) dormancy of ermB and ermT genes in six isolates without erythromycin. Positive controls are purified recombinant ErmB and ErmT proteins tagged with a His6 tail. ErmB and ErmT bands were blotted with mouse serum against above recombinant ErmB or ErmT proteins. GAPDH was used for loading controls and was visualized by monoclonal human GAPDH antibody. ATCC 43144 is a negative control as it lacks ermB and ermT genes.
Due to immature genetic manipulation system in S. gallolyticus subsp. pasteurianus, we cloned ermB and ermT with the leader peptide into pET21a vector (Figure S2). These clones were used to test the expression of the two genes. In BL21DE3 cells, the two genes carried in pET21a were also expressed in the presence of erythromycin, as blotted by monoclonal anti-Histag antibody (Figure S2). This is in agreement with the inducible expression of the two genes in six isolates (Figure 2). The expressed ErmB and ErmT proteins without erythromycin could be due to leaky expression off the lac promoter in pET21a vector.
2.5. The Inducible Expression of ermB and ermT Conferred High Level of Macrolide Resistance
All ermB and ermT clones with or without the leader peptide in pET28a or PHT01 were transformed into BL21DE3 cells for antibiotic sensitivity testing (Table 3). MIC values for erythromycin and clarithromycin were recorded with 30 μg/mL PAβN, an efflux inhibitor [42]. While empty vectors generated an MIC of 1 mg/L for both erythromycin and clarithromycin, both ermB and ermT plasmids yielded high macrolide resistance, with an MIC of 1024 mg/L for erythromycin, and ≥128 mg/L for clarithromycin. These plasmids also exhibited high resistance to lincomycin (MIC = 512 mg/L). Interestingly, when both plasmids were introduced, MICs increased by at least two-fold for erythromycin, and to an even larger extent for clarithromycin. Similar pattern was observed for ermBL and ermTL, the clones with the leader peptide. Notably, the leader peptide appeared to reduce MIC values (Table 3). The MIC levels produced by both ermBL and ermTL plasmids were comparable to that obtained from the six S. gallolyticus subsp. pasteurianus isolates (Table 1), indicating that the presence of both ermB and ermT genes was responsible for the high macrolide resistance in these isolates.
Table 3.
MICs of ermB and ermT clones. ermTL and ermBL represent the ermT and ermB clones with upstream leader peptide.
| erm Genes and Plasmids | MICs (mg/L) | ||
|---|---|---|---|
| Erythromycin | Clarithromycin | Lincomycin | |
| pET28a | 1 | 1 | 128 |
| PHT01 | 1 | 1 | 128 |
| ermT in pET28a | 1024 | 512 | 512 |
| ermTL in pET28a | 512 | 256 | 512 |
| ermB in pET28a | 1024 | 128 | 512 |
| ermBL in pET28a | 512 | 8 | 512 |
| ermT in PHT01 | 128 | 16 | – |
| ermTL in PHT01 | 16 | 4 | – |
| ermB in pET28a + ermT in PHT01 | 2048 | >1024 | 2560 |
| ermBL in pET28a + ermTL in PHT01 | 1024 | 1024 | 2048 |
3. Discussion
In this report, we have demonstrated that the inducible expression of both ermB and ermT confers high macrolide resistance in multidrug resistant S. gallolyticus subsp. pasteurianus from China.
All six isolates exhibited no resistance to penicillin, cefataxime or vancomycin, but to tetracyclin, lincomycin, arithromycin and clarithromycin among tested antibiotics. Only some isolates demonstrated resistance to chloramphenicol, levoflaxacin and gentamycin (Table 1). Limited by small number of isolates, we did not further characterize the molecular mechanism underlying the resistance to chloramphenicol, levoflaxacin and gentamycin. The tetracyclin resistance in all our isolates appeared to be conferred by tetM and tetL, as indicated by PCR amplification followed by DNA sequencing (Table S2). As lincomycin and macrolides share similar mechanism of action and MLS resistance element including erm [38], the lincomycin resistance in our isolates is likely contributed by the presencce of both ermB and ermT (Table 1 and Table 3). Detailed mechanisms remain to be addressed for tetracyclin and lincomycin.
While 63% of macrolide resistance was observed among S. gallolyticus subsp. pasteurianus isolates from human clinic in Taiwan [22,32], all our isolates exhibited high macrolide resistance, and acquired ermB as additional macrolide-resistant determinant.
Although macrolide resistance in Gram-positive bacteria is mainly contributed by active efflux and 23S rRNA modification [32,33], the high macrolide resistance in our isolates was not caused by efflux pump (Table S2). 23S rRNA modification can originate from mutations within L4, L22 and 23S rRNA or from Erm methylases [36,43]. Our study demonstrated that neither L4, L22 nor 23S mutation but the presence of both ermB and ermT (Table 1, Table 2 and Table 3) was responsible for high macrolide resistance in these isolates. The ermB and ermT genes appeared to be acquired independently (Figure 1), and their expression in all six isolates was erythromycin inducible (Figure 2).
To our knowledge, this is the first detailed mechanistic report on the presence of ermB and ermT conferring high macrolide resistance in bacteria. Previously, the presence of ermB and ermT has been reported in one single S. bovis isolate from Hong Kong [44] and one single group B Streptococcus [45], while detailed mechanism was not addressed in either report. Our data revealed not only the presence of both ermB and ermT, but also the erythromycin-inducible expression of the two genes conferring high macrolide resistance in all six isolates. Erm proteins including ErmB and ErmT are believed to methylate A2058 of 23S rRNA [46]. The acquisition of both ermB and ermT in bacterial genome is intriguing. MIC testing data using ermB and ermT clones indicated that the leader peptide led to reduced MIC values for all tested macrolides (Table 3), suggesting reduced expression of both ErmB and ErmT in the presence of the leader peptide. The leader peptide of erm genes is known to cause translation attenuation, and expose the open reading frame of downstream erm gene, thus turning on its expression [47,48]. The ribosome stalls between the 10th amino acid and the 11th incoming aminoacyl-tRNA. The translational pause largely relies on the sequence content of the leader peptide [49,50]. The reduced expression of a single erm gene with an upstream leader peptide in our isolates may not sustain macrolide resistance pressure. This may favor the emergence of second erm gene in these bacteria. The inducible expression of both ermB and ermT with an upstream leader peptide may be able to generate sufficient methylation at A2058 of 23S rRNA, thus excluding macrolides from the ribosomal polypeptide exit tunnel more efficiently than either enzyme alone, leading to enhanced macrolide resistance in host cells (Table 3). The detailed ribosomal methylation mechanisms and expression pattern of these two Erm proteins still remain to be addressed.
In summary, the present study reveals new features of macrolide resistance in S. gallolyticus subsp. pasteurianus, in which the inducible expression of both ermB and ermT conferred high macrolide resistance.
4. Materials and Methods
4.1. Bacterial Isolates and Culture Conditions
Six isolates of S. gallolyticus subsp. pasteurianus were obtained from dead ducklings collected in Hubei and Guangxi in China during several natural outbreaks in 2010–2013. The isolates were identified using biochemical characterization and 16S rRNA gene sequencing [51] (Table S1). S. gallolyticus subsp. pasteurianus ATCC 43144 and S. aureus ATCC 29213 were used as controls [31,52]. The S. gallolyticus subsp. pasteurianus were routinely cultured at 37 °C in trypticase soy broth (TSB) supplemented with 5% fetal bovine serum. E. coli TG1 and BL21DE3 were cultured in LB medium at 37 °C, and used for gene cloning and recombinant protein expression, respectively. Materials and reagents were purchased from Sigma Aldrich (Shanghai, China), unless otherwise stated.
4.2. Antimicrobial Susceptibility Testing
The standard agar dilution method recommended by CLSI [40,41] was used to determine MICs of various antibiotics for the six isolates. The resistance contribution by ermB and ermT genes and by 23S rRNA mutations was tested in 96-well plates using BL21DE3 cells. Each well contained 200 μL of Mueller-Hinton (MH) medium with 1000 log-phase CFUs and 30 μg/mL Phenylalanine-Arginine β-Naphthylamide (PAβN) [42]. Then, 1 mM IPTG was added to cells carrying ermB and/or ermT plasmid(s) to induce protein expression but not to cells with mutant 23S rRNA. Next, 50 μg/mL kanamycin was added to clones in pET28a, while 100 μg/mL ampicillin was used for clones in PHT01 or PUC19. Finally, the culture was incubated at 37 °C for 20 h. The cell density was determined by OD600 using a μQuant plate reader (BioTek, Beijing, China).
4.3. Sequence Analysis and Molecular Cloning
Genomic DNA of six isolates was extracted using TIANamp Bacteria genomic DNA kit from Tiangen Biotech (Beijing, China). PCR followed by DNA sequencing was used to detect the presence of antibiotic resistance genes and mutations within rplD, rplV and 23S rRNA gene. All PCRs were done using Phu DNA polymerase (Thermo Scientific, Waltham, MA, USA) and primers synthesized by Sangon Biotech (Shanghai, China) (Table S3). Sequence alignment was done using BLAST (NCBI web) or Clustal at http://www.ebi.ac.uk/tools/clustalw2. ermB and ermT sequences from Genbank (accession number JN899586 and AY894138) were referenced, while 23S rRNA gene, rplD and rplV sequences from ATCC 43144 (accession number AP012054) were used for detecting mutations in all isolates.
The ermB and ermT genes with or without the leader peptide from GX130630 were cloned into pET28a via NheI and XhoI sites or pET21a via NheI and NdeI sites, or into PHT01 via BamHI and XbaI sites. The 23S rRNA gene sequence from ATCC 43144 was cloned into PUC19 vector via BamHI and EcoRI sites. All clones were confirmed by DNA sequencing.
The flanking sequences of ermT were identified by whole genome sequencing, while those of ermB were determined by DNA sequencing of cloned PCR fragments. Briefly, AL101002 genomic DNA was digested by HindIII. The resulting DNA fragments were amplified and cloned using LA-PCR in vitro clone kit from Takara. Primers C1 and C2 were provided by manufacturer, while gene-specific primers were designed according to ermB sequence and were from Sangon Biotech, China (Table S3).
4.4. Whole-Genome Sequencing
The whole genome of S. gallolyticus subsp. pasteurianus AL101002 was sequenced using the Illumina HiSeq 2500 platform at Shanghai Bohao Biotechnology, China. The Whole Genome Shotgun sequence of AL101002 was de-novo assembled using SPAdes 2.5.1 (Algorithmic Biology Lab, St Petersburg, Russia) (http://bioinf.spbau.ru/spades) and has been deposited at GenBank under the accession number LJPL00000000.
4.5. Western Blot Analysis
The ErmB and ErmT levels in six isolates were detected by immunoblotting. The cells were cultured in TSB medium at 37 °C to early stationary phase. The cell pellet was collected after centrifugation and washed. After one freeze-thaw cycle, total protein was extracted using the Bacterial Protein Extraction Kit from Jiangsu KeyGEN BioTECH, Nanjing, China. SDS-PAGE and blotting were performed using Bio-Rad electrophoresis and blotting systems (Bio-Rad, Wuhan, China). The ErmB and ErmT proteins were detected using in-house mouse serum (1:2000) raised against recombinant ErmB or ErmT protein. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was detected using monoclonal antibody against human GAPDH (1:5000) from Proteintech (Wuhan, China). Monoclonal goat anti-mouse IgG-HRP (1:2000) from Wuhan Boster (Wuhan, China) was used as a secondary antibody. Enhanced chemiluminescence (ECL) substrate from Seven Sea Biotech (Shanghai, China) was used for visualization. Digital images were taken using the ImageQuant LAS 4000 instrument from GE Healthcare (Beijing, China).
Acknowledgments
We thank Sebastian Kalamajski at Lund University, Sweden, and Howard Gamper at Thomas Jefferson University, Philadelphia, USA for their kind suggestions with English writing, and Kidon Sung at FDA for comments on the manuscript. This work was supported by the Start Package for Chutian Scholar Professors to CL, the Natural Science Fund of China (Grant number 31370801 to CL), Project 2013PY003 Supported by Fundamental Research Funds for Central Universities to CL and Natural Science Fund of Hubei Province (Grant number 2013CFB189 to CL).
Abbreviations
| MIC | Minimum inhibitory concentration |
| ATCC | American type culture collection |
| CLSI | Clinical and laboratory standards institute |
| MLS | Macrolide-lincosamide-streptogramin B |
| TSB | Trypticase soy broth |
| MH | Mueller-hinton |
| IPTG | Isopropyl β-d-1-thiogalactopyranoside |
| ECL | Enhanced chemiluminescence |
| GAPDH | Glyceraldehyde-3-phosphate dehydrogenase |
| PAβN | Phenylalanine-arginine beta-naphthylamide |
Supplementary Materials
Supplementary materials can be found at www.mdpi.com/1422-0067/17/10/1599/s1.
Author Contributions
Meixia Li performed most experiments and analyzed data; Chao Cai did Western blotting in all six isolates; Juan Chen and Changwei Cheng repeated MIC analysis in Table 1 as different operators; Guofu Cheng and Xueying Hu designed experiments in strain isolation; and Cuiping Liu designed experiments, analyzed data and wrote the paper.
Conflicts of Interest
The authors declare no competing interests.
References
- 1.Osawa R., Fujisawa T., Sly L.I. Streptococcus gallolyticus sp. nov.; gallate degrading organisms formerly assigned to Streptococcus bovis. Syst. Appl. Microbiol. 1995;18:1942–1946. doi: 10.1016/S0723-2020(11)80451-0. [DOI] [Google Scholar]
- 2.Ruoff K.L., Whiley R.A., Beighton D. Manual of Clinical Microbiology. 8th ed. ASM Press; Washington, DC, USA: 2003. Streptococcus; pp. 405–421. [Google Scholar]
- 3.Poyart C., Quesne G., Trieu-Cuot P. Taxonomic dissection of the Streptococcus bovis group by analysis of manganese-dependent superoxide dismutase gene (sodA) sequences: Reclassification of ′Streptococcus infantarius subsp. coli′ as Streptococcus lutetiensis sp. nov. and of Streptococcus bovis biotype 11.2 as Streptococcus pasteurianus sp. nov. Int. J. Syst. Evol. Microbiol. 2002;52:1247–1255. doi: 10.1099/00207713-52-4-1247. [DOI] [PubMed] [Google Scholar]
- 4.Schlegel L., Grimont F., Ageron E., Grimont P.A.D., Bouvet A. Reappraisal of the taxonomy of the Streptococcus bovis/Streptococcus equinus complex and related species: Description of Streptococcus gallolyticus subsp. gallolyticus subsp. nov., S. gallolyticus subsp. macedonicus subsp. nov. and S. gallolyticus subsp. pasteurianus subsp. nov. Int. J. Syst. Evol. Microbiol. 2003;53:632–645. doi: 10.1099/ijs.0.02361-0. [DOI] [PubMed] [Google Scholar]
- 5.Li M., Gu C., Zhang W., Li S., Liu J., Qin C., Su J., Cheng G., Hu X. Isolation and characterization of Streptococcus gallolyticus subsp. pasteurianus causing meningitis in ducklings. Vet. Microbiol. 2013;162:930–936. doi: 10.1016/j.vetmic.2012.11.038. [DOI] [PubMed] [Google Scholar]
- 6.Kimpe A., Decostere A., Martel A., Pevriese L.A., Haesebrouck F. Phenotypic and genetic characterization of resistance against macrolides and lincosamides in Streptococcus gallolyticus strains isolated from pigeons and humans. Microb. Drug Resist. 2003;9:35–38. doi: 10.1089/107662903322541874. [DOI] [PubMed] [Google Scholar]
- 7.Barnett J., Ainsworth H., Boon J.D., Twomey D.F. Streptococcus gallolyticus subsp. pasteurianus septicaemia in goslings. Vet. J. 2008;176:251–253. doi: 10.1016/j.tvjl.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Saumya D., Wietunge S., Dunn P., Wallner-Pendleton E., Lintner V., Matthews T., Pierre T., Kariyawasam S. Acute septicemia caused by Streptococcus gallolyticus subsp. pasteurianus in turkey poults. Avian Dis. 2014;58:318–322. doi: 10.1637/10617-071813-Case.1. [DOI] [PubMed] [Google Scholar]
- 9.Klatte J.M., Clarridge J.E., Bratcher D., Selvarangan R. A longitudinal case series description of meningitis due to Streptococcus gallolyticus subsp. pasteurianus in infants. J. Clin. Microbiol. 2012;50:57–60. doi: 10.1128/JCM.05635-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagamatsu M., Takaqi T., Ohyanagi T., Yamazaki S., Nobuoka S., Takemura H., Akita H., Miyai M., Ohkusu K. Neonatal meningitis caused by Streptococcus gallolyticus subsp. pasteurianus. J. Infect. Chemother. 2012;18:265–268. doi: 10.1007/s10156-011-0320-4. [DOI] [PubMed] [Google Scholar]
- 11.Takahashi Y., Ishiwada N., Tanaka J., Okusu K., Ichimura S., Hishiki H., Ota S., Kohno Y. Streptococcus gallolyticus subsp. pasteurianus meningitis in an infant. Pediatr. Int. 2014;56:282–285. doi: 10.1111/ped.12254. [DOI] [PubMed] [Google Scholar]
- 12.Hede S.V. Diagnosis and treatment of childhood meningitis caused by Streptococcus bovis group. Curr. Infect. Dis. Rep. 2016;18:11. doi: 10.1007/s11908-016-0519-8. [DOI] [PubMed] [Google Scholar]
- 13.Marmonlin E.S., Hartmeyer G.N., Christensen J.J., Nielsen X.C., Dargis R., Skov M.N., Knudsen E., Kemp M., Justesen U.S. Bacteremia with the bovis group streptococci: Species identification and association with infective endocarditis and with gastrointestinal disease. Diagn. Microbiol. Infect. Dis. 2016;85:239–242. doi: 10.1016/j.diagmicrobio.2016.02.019. [DOI] [PubMed] [Google Scholar]
- 14.Sturt A.S., Yang L., Sandhu K., Pei Z.H., Cassai N., Blaser M.J. Streptococcus gallolyticus subspecies pasteurianus (biotype II/2), a newly reported cause of adult meningitis. J. Clin. Microbiol. 2010;48:2247–2249. doi: 10.1128/JCM.00081-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lazarovitch T., Sango M., Levine M., Brusovansky R., Akins R., Hayakawa K., Lephart P.R., Sobel J.D., Kaye K.S., Marchaim D. The relationship between the new taxonomy of Streptococcus bovis and its clonality to colon cancer, endocarditis, and biliary disease. Infection. 2013;41:329–337. doi: 10.1007/s15010-012-0314-x. [DOI] [PubMed] [Google Scholar]
- 16.Takamura N., Kenza T., Minami K., Matsumura M. Infective endocarditis caused by Streptococcus gallolyticus subspecies pasteurianus and colon cancer. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-203476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chirouze C., Patry I., Duval X., Baty V., Tattevin P., Aparicio T., Pagenault M., Carbonnel F., Couetdic G., Hoen B. Streptococcus bovis/Streptococcus equinus complex fecal carriage, colorectal carcinoma, and infective endocarditis: A new appraisal of a complex connection. Eur. J. Clin. Microbiol. Infect. Dis. 2013;32:1171–1176. doi: 10.1007/s10096-013-1863-3. [DOI] [PubMed] [Google Scholar]
- 18.Su Y., Miao B., Wang H., Wang C., Zhang S.W. Splenic abscess caused by Streptococcus gallolyticus subsp. pasteurianus as presentation of a pancreatic cancer. J. Clin. Microbiol. 2013;51:4249–4251. doi: 10.1128/JCM.01709-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corredoira J., Alonso M.P., García-Garrote F., Garcia-Pais M.J., Coira A., Rabunal R., Gonzalez-Ramirez A., Pita J., Matesanz M., Velasco D., et al. Streptococcus bovis group and biliary tract infections: An analysis of 51 cases. Clin. Microbiol. Infect. 2013:405–409. doi: 10.1111/1469-0691.12333. [DOI] [PubMed] [Google Scholar]
- 20.Matesanz M., Rubal D., Iñiguez I., Rabuñal R., García-Garrote F., Coira A., García-País M.J., Pita J., Rodriguez-Macias A. Is Streptococcus bovis a urinary pathogen? Eur. J. Clin. Microbiol. Infect. Dis. 2015;34:719–725. doi: 10.1007/s10096-014-2273-x. [DOI] [PubMed] [Google Scholar]
- 21.Poulsen L.L., Bisqaard M., Son N.T., Trung N.V., An H.M., Dalsgaard A. Enterococcus and Streptococcus spp. associated with chronic and self-medicated urinary tract infections in Vietnam. BMC Infect. Dis. 2012;12:1599. doi: 10.1186/1471-2334-12-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheng W.H., Chuang Y., Teng L.J., Hsueh P.P. Bacteraemia due to Streptococcus gallolyticus subspecies pasteurianus is associated with digestive tract malignancies and resistance to macrolides and clindamycin. J. Infect. Chemother. 2014;69:145–153. doi: 10.1016/j.jinf.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 23.Lee C.K., Chan H.M., Ho P.L., Wong H.K., Leung J.N., Tsoi W.C., Lin C.K. Long-term clinical outcomes after Streptococcus bovis isolation in asymptomatic blood donors in Hong Kong. Transfusion. 2013;53:2207–2210. doi: 10.1111/trf.12087. [DOI] [PubMed] [Google Scholar]
- 24.Saegeman V., Cossey V., Loens K., Schuermans A., Glaser P. Streptococcus gallolyticus subsp. pasteurianus infection in a neonatal intensive care unit. Pediatr. Infect. Dis. J. 2016 doi: 10.1097/INF.0000000000001290. [DOI] [PubMed] [Google Scholar]
- 25.Samkar A., Brouwer M.C., Pannekoek Y., Ende A., Beek D. Streptococcus gallolyticus meningitis in adults: Report of five cases and review of the literature. Clin. Microbiol. Infect. 2015;21:1077–1083. doi: 10.1016/j.cmi.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 26.García-Pais M.J., Rabuñal R., Corredoira J. Alonso MPSpondylodiscitis due to Streptococcus gallolyticus subsp. pasteurianus. Enferm. Infecc. Microbiol. Clin. 2016;34:141–142. doi: 10.1016/j.eimc.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Matsubara K., Takegawa H., Sakizono K., Nomoto R., Yamamoto G., Osawa R. Transient bacteremia due to Streptococcus gallolyticus subsp. pasteurianus in a 3-year-old infant. Jpn. J. Infect. Dis. 2015;68:251–253. doi: 10.7883/yoken.JJID.2014.423. [DOI] [PubMed] [Google Scholar]
- 28.Park J.W., Eun S.H., Kim E.C., Seong M.W., Kim Y.K. Neonatal invasive Streptococcus gallolyticus subsp. pasteurianus infection with delayed central nervous system complications. Korean J. Pediatr. 2015;58:33–36. doi: 10.3345/kjp.2015.58.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kimpe A., Decostere A., Martel A., Haesebrouck F., Devriese A. Prevalence of antimicrobial resistance among pigeon isolates of Streptococcus gallolyticus, Escherichia coli and Salmonella enterica serotype Typhimurium. Avian Pathol. 2002;31:393–397. doi: 10.1080/03079450220141679. [DOI] [PubMed] [Google Scholar]
- 30.Leclercq R., Huet C., Picherot M., Trieu-Cuot P., Trieu-Cuot P., Poyart C. Genetic basis of antibiotic resistance in clinical isolates of Streptococcus gallolyticus (Streptococcus bovis) Antimicrob. Agents Chemother. 2005;49:1646–1648. doi: 10.1128/AAC.49.4.1646-1648.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsai J.C., Hsueh P.R., Chen H.J., Tseng S.P., Cheng P.Y., Teng L.J. The erm(T) gene is flanked by IS1216V in inducible erythromycin-resistant Streptococcus gallolyticus subsp. pasteurianus. Antimicrob. Agents Chemother. 2005;49:4347–4350. doi: 10.1128/AAC.49.10.4347-4350.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Teng L.J., Hsueh P.R., Ho S.W., Luh K.T. High prevalence of inducible erythromycin resistance among Streptococcus bovis isolates in Taiwan. Antimicrob. Agents Chemother. 2001;45:3362–3365. doi: 10.1128/AAC.45.12.3362-3365.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reyes J., Hidalgo M., Díaz L., Rincon S., Moreno J., Vanegas N., Castaneda E. Characterization of macrolide resistance in Gram-positive cocci from Colombian hospitals: A countrywide surveillance. Int. J. Infect. Dis. 2007;11:329–336. doi: 10.1016/j.ijid.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 34.Wierzbowski A.K., Boyd D., Mulvey M., Hoban D.J., Zhanel G.G. Expression of the mef(E) gene encoding the macrolide efflux pump protein increases in Streptococcus pneumoniae with increasing resistance to macrolides. Antimicrob. Agents Chemother. 2005;49:4635–4640. doi: 10.1128/AAC.49.11.4635-4640.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang Y., Tatsunol I., Okada R., Hata N., Matsumoto M., Isaka M., Isobe K., Haseqawa T. Predominant role of msr(D) over mef(A) in macrolide-resistance in Streptococcus pyogenes. Microbiology. 2015;162:46–52. doi: 10.1099/mic.0.000206. [DOI] [PubMed] [Google Scholar]
- 36.Hawkins P.A., Chochua S., Jackson D., Beall B., McGee L. Mobile elements and chromosomal changes associated with MLS resistance phenotypes of invasive pneumococci recovered in the United States. Microb. Drug Resist. 2015;21:121–129. doi: 10.1089/mdr.2014.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dunkle J.A., Xiong L., Mankin A.S., Cate J.H. Structures of the Escherichia coli ribosome with antibiotics bound near the peptidyl transferase center explain spectra of drug action. Proc. Natl. Acad. Sci. USA. 2010;107:17152–17157. doi: 10.1073/pnas.1007988107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leclercq R. Mechanisms of resistance to macrolides and lincosamides: Nature of the resistance elements and their clinical implications. Clin. Infect. Dis. 2002;34:482–492. doi: 10.1086/324626. [DOI] [PubMed] [Google Scholar]
- 39.Rosato A., Vicarini H., Leclercq R. Inducible or constitutive expression of resistance in clinical isolates of streptococci and enterococci cross-resistant to erythromycin and lincomycin. J. Antimicrob. Chemother. 1999;43:559–562. doi: 10.1093/jac/43.4.559. [DOI] [PubMed] [Google Scholar]
- 40.Clinical and Laboratory Standards Institute . Performance Standards for Antimicrobial Susceptibility Testing: Twentieth Informational Supplement M100-S20. CLSI; Wayne, PA, USA: 2010. [Google Scholar]
- 41.Clinical and Laboratory Standards Institute . Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically: Approved Standard-Ninth Edition, M07-A9. CLSI; Wayne, PA, USA: 2012. [Google Scholar]
- 42.Moore S.D., Sauer R.T. Revisiting the mechanism of macrolide-antibiotic resistance mediated by ribosomal protein L22. Proc. Natl. Acad. Sci. USA. 2008;105:18261–18265. doi: 10.1073/pnas.0810357105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zaman S., Fitzpatrick M., Lindahl L., Zengel J. Novel mutations in ribosomal proteins L4 and L22 that confer erythromycin resistance in Escherichia coli. Mol. Microbiol. 2007;66:1039–1050. doi: 10.1111/j.1365-2958.2007.05975.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee R.A., Woo P.C.Y., To A.P.C., Lau S.K.P., Wong S.S.Y., Yuen K.Y. Geographical difference of disease association in Streptococcus bovis bacteraemia. J. Med. Microbiol. 2003;52:903–908. doi: 10.1099/jmm.0.05199-0. [DOI] [PubMed] [Google Scholar]
- 45.DiPersio L.P., DiPersio J.R. Identification of an erm(T) gene in strains of inducibly clindamycin-resistant group B Streptococcus. Diagn. Microbiol. Infect. Dis. 2007;57:189–193. doi: 10.1016/j.diagmicrobio.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 46.Skinner R., Cundliffe E., Schmidt F.J. Site of action of a ribosomal RNA methylase responsible for resistance to erythromycin and other antibiotics. J. Biol. Chem. 1983;258:12702–12706. [PubMed] [Google Scholar]
- 47.Weisblum B. Insights into erythromycin action from studies of its activity as inducer of resistance. Antimicrob. Agents Chemother. 1995;39:797–805. doi: 10.1128/AAC.39.4.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Horinouchi S., Weisblum B. Posttranscriptional modification of mRNA conformation: Mechanism that regulates erythromycin-induced resistance. Proc. Natl. Acad. Sci. USA. 1980;77:7079–7083. doi: 10.1073/pnas.77.12.7079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arenz S., Ramu H., Gupta P., Berninghausen O., Beckmann R., Vazquez-Laslop N., Mankin A.S., Wilson D.N. Molecular basis for erythromycin-dependent ribosome stalling during translation of the ErmBL leader peptide. Nat. Commun. 2014;5:3501. doi: 10.1038/ncomms4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lovett P.S., Rogers E.J. Ribosome regulation by the nascent peptide. Microbiol. Rev. 1996;60:366–385. doi: 10.1128/mr.60.2.366-385.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson K.H., Blitchinqton R., Greene R.C. Amplification of bacterial 16S ribosomal DNA with polymerase chain reaction. J. Clin. Microbiol. 1990;28:1942–1946. doi: 10.1128/jcm.28.9.1942-1946.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Prunier A.L., Malbruny B., Tandé D., Picard B., Leclercq R. Clinical isolates of Staphylococcus aureus with ribosomal mutations conferring resistance to macrolides. Antimicrob. Agents Chemother. 2002;46:3054–3056. doi: 10.1128/AAC.46.9.3054-3056.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.