Abstract
Social network analysis (SNA) and social network-based interventions (SNI) are important analytical tools harnessing peer and family influences critical for HIV prevention and treatment among substance users. While SNA is an effective way to measure social network influences, SNI directly or indirectly involves network members in interventions. Even though these methods have been applied in heterogeneous ways, leading to extensive evidence-based practices, systematic reviews are however, lacking. We searched five bibliographic databases and identified 58 studies involving HIV in substance users that had utilized SNA or SNI as part of their methodology. SNA was used to measure network variables as inputs in statistical/mathematical models in 64% of studies and only 22% of studies used SNI. Most studies focused on HIV prevention and few addressed diagnosis (k=4), care linkage and retention (k=5), ART adherence (k=2), and viral suppression (k=1). This systematic review highlights both the advantages and disadvantages of social network approaches for HIV prevention and treatment and gaps in its use for HIV care continuum.
Keywords: social network analysis, social network intervention, HIV prevention, HIV care continuum, substance users
INTRODUCTION
In 2014, the Joint United Nations Program on HIV/AIDS called for a rapid scaling-up of essential HIV prevention and treatment approaches to achieve the target of “90-90-90” by the year 2020 (1). The worldwide “90-90-90” target calls for 90% of people living with HIV (PLH) to be diagnosed, with 90% of those receiving combination antiretroviral therapy (ART), and 90% of PLH on antiretroviral therapy (ART) to sustain virological suppression (1, 2). Achieving this target by 2020 would consequently, by 2030, decrease the global burden of HIV/AIDS by 90% from that in 2010 (1). The target is based on the HIV care continuum model, also known as the HIV treatment cascade. This model outlines the sequential steps or stages of HIV treatment that PLH transition from initial diagnosis to achieving viral suppression, and shows the proportion of PLH who are engaged at each stage. Parallel to the optimistic “90-90-90” target are the discouraging funding cuts to the Global Fund for AIDS, Tuberculosis and Malaria (GFATM) and the United States’ President’s Emergency Plan for AIDS Relief (PEPFAR), which together disproportionately affect practices relating to HIV (prevention and treatment) and addiction (harm reduction) treatment programs (3). This issue has particular significance for Eastern European (e.g. Ukraine, Russia), Central Asian (e.g. Kazakhstan) and Asian (e.g. Vietnam, Malaysia) countries, where HIV epidemics are largely shaped by people who inject (PWIDs) and who use drugs (PWUDs) (2). HIV-infected PWUDs and PWIDs are a key population who, in the absence of scaled-up prevention and treatment interventions, would likely experience suboptimal outcomes along the HIV continuum of care. Achieving the 90-90-90 target, particularly for this population would, therefore, require scaling up of integrated and comprehensive interventions, which are not only sustainable but also cost-effective.
A significant body of evidence, from both theoretical and public health perspectives, points to the influence of network-based strategies such as social network analysis (SNA) and social network based interventions (SNIs) on HIV prevention and treatment outcomes for PWIDs and PWUDs. For the purpose of this paper, we define social networks in a SNA as a group of individuals who knew each other prior to an intervention. In comparison, SNI is a ‘peer-driven-intervention’ (PDI) where the peers (either known or unknown a priori) play the role of educators of HIV prevention information, health advocates, or health buddies, supporting each other to improve ART adherence and retention in HIV care.
Prior research suggests drug users in one’s social network act as dysfunctional role models (4, 5), reinforce risky drug use behaviors (6, 7), increase likelihood of engaging in sexual risk behaviors (8–14), and consequently lead to poor HIV treatment outcomes (15). Conversely, self-reported condom use is strongly associated with positive norms using condoms among social network members (12) and social support increases engagement in needle exchange (16, 17) and addiction treatment programs (18, 19). In terms of structural characteristics of networks (e.g. size, density), several studies indicate strong association between high-risk sexual behavior (20–22), HIV infection (23), HIV transmission (24–26), and increased drug use. Other structural network characteristics, such as being a bridge population (27), centrality (28), and core-periphery relationships (29), have been identified as contributors to both sexual (27, 30) and drug injection-related HIV transmission (31).
From a broader public health perspective, some SNIs have demonstrated promising potential in their ability to reach a higher proportion of key populations (e.g. PWIDs/PWUDs), that are challenging to engage in communities, and populations that may be unable to travel to health services by themselves. These findings imply that efforts to prevent HIV transmission must incorporate the impact of social networks. Social networks can, therefore, play a dual role in HIV transmission: they serve as both the routes of transmission for the virus and the routes of dissemination for information related to HIV prevention and treatment services (32, 33).
The objective of this systematic scoping review was to identify and synthesize such extensive information on evidence-based network approaches (SNA and SNI) that strategically target HIV prevention and treatment in one or more steps along a HIV care continuum. The following key questions guide the scope of this review:
Given the heterogeneity of the usage of social network approaches, what are the different ways SNA and SNI are conducted, analyzed, and reported in the studies?
What is the distribution of the approaches identified in #1 in terms of their targeting outcome measures associated with HIV prevention and steps of a HIV care continuum?
Given the lack of clarity on recruitment methods and whether the networks are defined post-hoc by the researchers, how are the social network members identified and involved in the SNIs?
What type of effect did the SNIs have on the intervention outcomes?
METHODS
We started this scoping review with a systematic literature search and selection of studies in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (34–36). Similar to systematic reviews and meta-analysis, scoping reviews also follow rigorous PRISMA guidelines for identifying a comprehensive set of relevant studies (34–36).
Search Strategy
An exhaustive search strategy was developed based on key terms, synonyms, and subject headings related to two groups: 1) social networks strategies and 2) study population of interest. For group one, the search consisted of the main term ‘social network’ and terms related to measuring and analyzing social networks such as ‘social network analysis’, ‘sociometrics’, ‘sociograms’, ‘sociomaps’, ‘egonetworks’, and ‘respondent driven sampling’. Names of software packages commonly used in SNA e.g. ‘UCINET’, ‘NetDraw’, and ‘Pajek’ were also used. The subject headings included were ‘social support’, ‘interpersonal relationships’, ‘cliques’, and ‘community support’.
For group two, the terms, subject headings, or combination of both included were ‘substance use’, ‘substance use disorder‘, ‘drug use’, ‘injecting drug use’, ‘non-injecting drug use’, ‘HIV’, ‘AIDS’, and ‘mental health’. We searched 5 electronic databases (MEDLINE, PubMed, PsycINFO, Social Science Citation Index, and Web of Science) and the website of International Social Network Analysis (www.insna.org). We also manually searched studies published in the journals of Social Networks and Connections, which are the two flagship publications of INSNA, the professional association for researchers interested in SNA. Studies were managed using an electronic bibliography (Endnote version X7).
Selection Criteria
Two primary inclusion criteria were used to select the studies:
sociometric analysis, egocentric network analysis, respondent-driven sampling (RDS), or social network-based intervention was part of the methodology of the study;
study population included substance users (PWUDs, PWIDs, and people with drinking problems) with or at risk for HIV.
We limited our review to peer-reviewed studies published in English between 1980 through February 2015. While social network approaches have evolved since the 1950s, HIV/AIDS and addiction research began in the 1980s and AIDS was not reported until 1981. Consequently, inclusion of studies was restricted to those published after 1980. Systematic reviews, meta-analysis, and studies that examined tobacco use, criminal justice system, biological studies of HIV/AIDS, and mental health issues not related to HIV/AIDS and substance use disorders as outcome measures were excluded from this review.
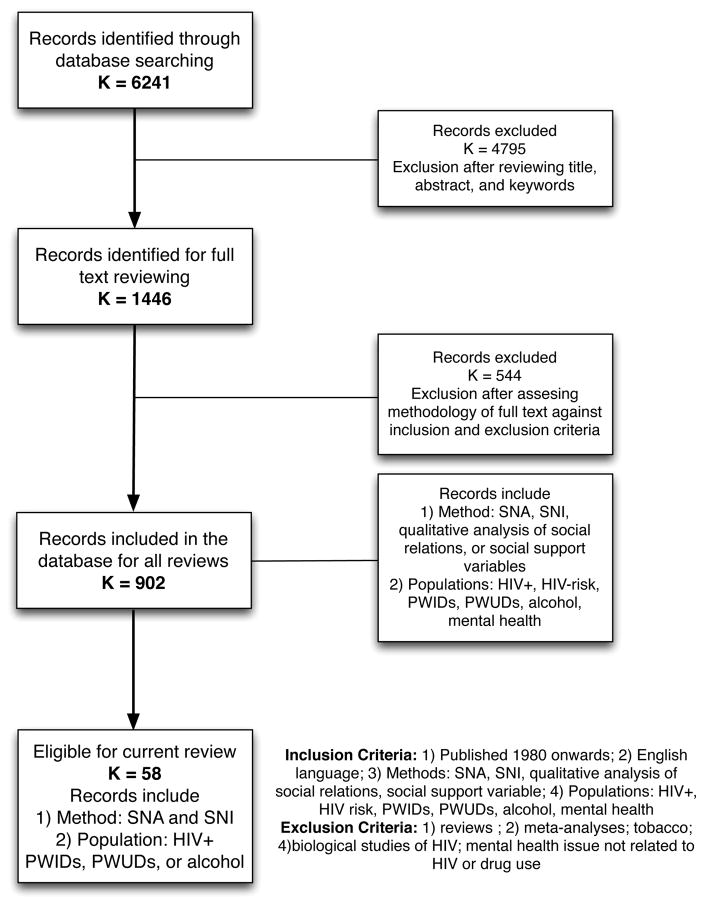
We further selected studies for our review using a two-stage process. First, four authors (DG, AK, BG, and SB) scanned titles, abstracts, and keywords identified from the search strategy (k = 6,241) and excluded them as appropriate based on the above-mentioned inclusion and exclusion criteria. To ensure reliability and consistency, the four authors assessed a pilot sample of 200 randomly selected studies independently on the basis of their title, abstract, and keywords. Both the included and excluded groups of studies from all the four authors were compared for consistency. Undecided studies, which needed further clarifications, were discussed collectively and resolved (either included and excluded). We repeated this pilot step in order for all the authors to understand and follow the inclusion and exclusion criteria consistently. These steps demonstrated good reliability (Cohen’s k = 0.74). A significant number of studies (k = 4,795) were excluded. The primary reason for exclusion was that SNA or SNI was not used as one of the analytical approach and social influence or relationships were measured and described by other techniques (Figure 1).
Figure 1.
Flowchart illustrating the selection of studies for the systematic review
Second, the four authors thoroughly reviewed the methodology section of 1446 studies and further excluded 544 studies, resulting in 902 studies. To clarify, the database of 902 records was for multiple (but related) reviews under preparation by the same authors. This particular review comprised 58 studies where SNA or SNI was part of their methodology and the study population was substance users at-risk for or living with HIV/AIDS (Figure 1).
Extraction and Charting the Results
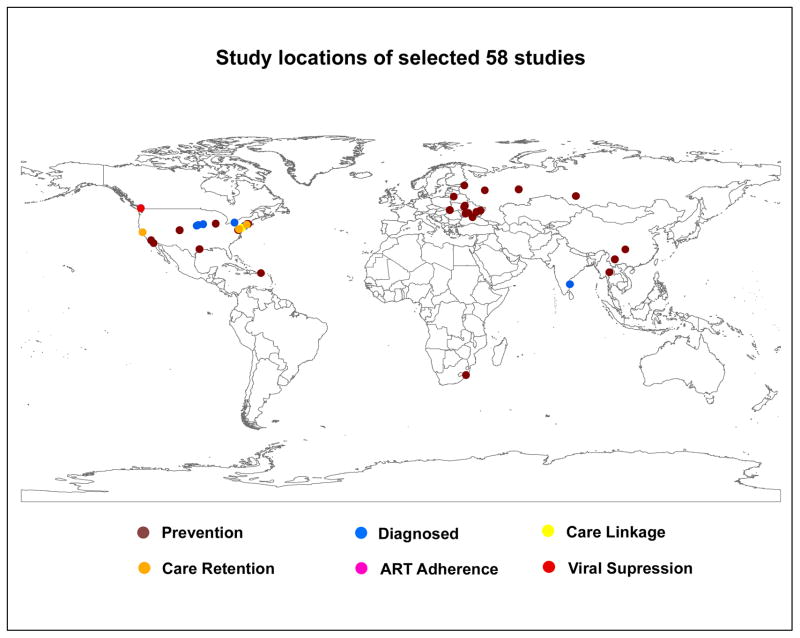
Data extraction and charting of results were done at various stages by one author and thoroughly reviewed and audited by another for consistency, quality, and relevance (36). First, we reviewed the full text of 58 studies and extracted information on the descriptive characteristics: year of publication, number of authors, name of the peer-reviewed journal, study population, study area, sample size, data collection, and types of social networks. Types of social network were further coded into two categories: risk networks (e.g. drug, sexual, and/or alcohol) and support networks (e.g. friends and/or family). We created a map of the different study locations, categorized by the outcome measures (HIV prevention and the steps of HIV care continuum) (Figure 2).
Figure 2.
Map of study locations from 58 included studies
Second, to systematically identify the different social network strategies included in the methodology (refer to #1 key question), we used a data extraction form to collect and code information on: data collection (categories: whole network, egocentric network, or RDS), types of network measures (categories: size, structural, dyads, relation, and social network member properties), network measures as variables in statistical/mathematical models (categories: univariate, bivariate, multivariate regression, structural equation modeling, repeated measures, projection models, and agent-based models), and network-based intervention protocol.
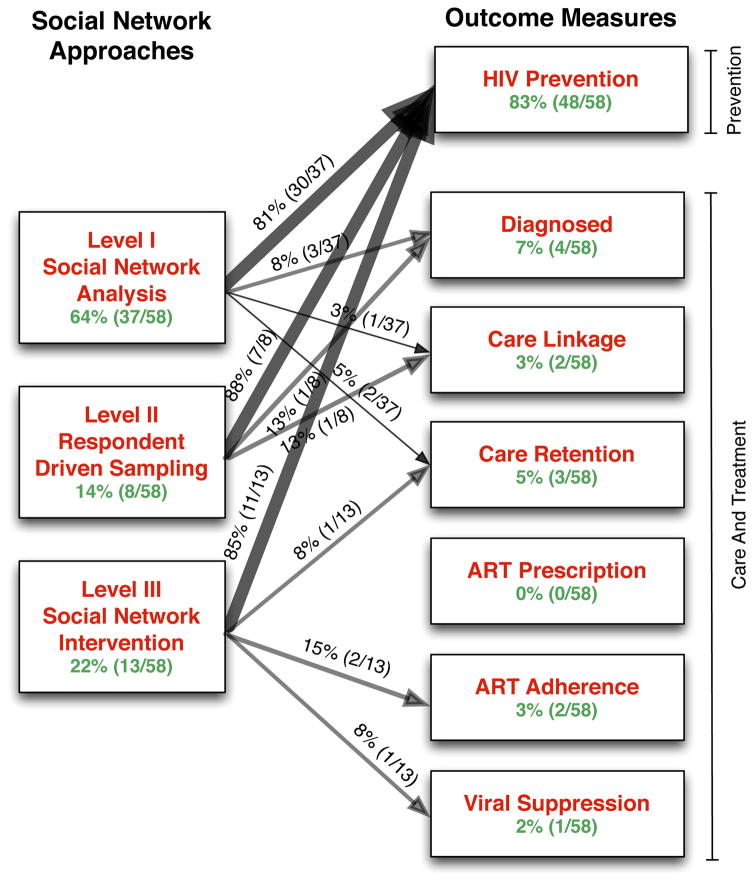
Third, based on the outcome measures, the studies were grouped into 7 categories: HIV prevention, HIV testing and diagnosis, linkage to care, retention in care, ART prescription, ART adherence, and viral suppression. A cross tabulation was conducted between the types of social network strategies and outcomes measures (Figure 3). These steps of synthesizing data addressed key question #2.
Figure 3.
Cross tabulation of studies categorized by social network approaches and study outcomes representing the stages of HIV care continuum
Fourth, for studies that conducted SNI, data on study period, location, population, sample size, study design, intervention aim, randomized control trial (RCT), outcome measures, methods of identifying peer participants, methods of identifying social network participants, control group (if any), major findings, and limitations were extracted. Summary tables of key information were then created (Tables 1, 2, and 3) (refer to key questions #3 and #4).
Table 1.
Descriptive Characteristics of Level III studies (K=13)
| Author | Date of Study | Study Location | Study Population | Sample Size | Intervention Framework | Intervention Aim | Description of Social Network Intervention |
|---|---|---|---|---|---|---|---|
| Broadhead, RS et al. 43 | 1998 | Towns in Eastern and Central Connecticut | PWIDs | 552 | PDI within a social network design | Provide PWIDs with guidance and structured incentives that permit them to play an active role in the outreach process | Peer educator: Peers interviewed, tested for HIV, and provided HIV prevention education and counseling at the storefront. Peers were rewarded for educating and recruiting other PWIDs from their networks. |
| Heckathor n, DD et al. 44 | 1998 | Eastern Connecticut | PWIDs | 258 | PDI within a social network design | Increase the recruitment of PWIDs; reductions on self-reported levels of HIV-risk behaviors | Peer educator: The intervention employed a two-step process. First, the peers were recruited and provided risk reduction education and materials such as bleach and condoms. Second, a structure of secondary incentives was implemented that offered peers encouraging their drug using social network members to carry out prevention activities in their own community. |
| Servegev, B et al. 46 | October 1996 – September 1998 | Yaroslavl, Russia | PWIDs | 484 | PDI within a social network design | Increase the recruitment of PWIDs; reductions on self-reported levels of HIV-risk behaviors | Peer educator: The intervention offered active drug users modest rewards for educating their peers in the community and recruiting them to a storefront for further education. The recruits were interviewed, received free HIV, STD, and hepatitis B and C testing, counseling, a needle exchange, and condoms. |
| Broadhead, RS et al. 49 | January – June 1996 | New Haven, Connecticut | PWIDs and PWUDs with HIV infection and with a clinician’s perception of low adherence to clinical care | 14 | PDI (health advocate) within a social support model | Increasing PWUDs and PWIDs adherence to HIV therapeutics and medications | As a health advocate (HA), each participant was assigned and asked to meet with another participants (peers) once a week at the project’s storefront to provide peer support and counseling. These include keeping clinical appointments, responding to physicians’ referrals, picking up prescriptions on time, adherence to medication, and attending weekly meetings with the HA. |
| Latkin, CA et al. 54 | August 1997 - March 1999 | Baltimore, Maryland | PWIDs and PWUDs with HIV infection | 250 | PDI based on social identity theory and peer outreach model | The intervention participants would be more likely to report HIV prevention advocacy with network members and that they would report greater behavioral risk reduction. A secondary aim was to normalize discussion about HIV within drug users’ networks. | RCT design with two arms: An equal- attention control group and a multisession experimental group. The intervention for experimental group included 10 sessions of 90 minutes each. Sessions covered HIV education, encouraged peers to educate risk reduction among sex and drug partners, family and friends, and other community members, methods of conducting outreach, identifying barriers to outreach and effective strategies to overcome them. Participants were provided with the opportunity to practice street outreach in small groups and receive feedback from the accompanying facilitator. In the final session, participants reviewed knowledge and skills gained in the prior sessions and made a public commitment to continue the learning process and peer education. |
| Broadhead, RS et al. 58 | 2006 | Bragino, Rybinsk, Russia | PWIDs | Bragino = 493; Rybinsk = 364 | Standard PDI and Simplified PDI | Test whether the Simplified PDI (modification in the PDI’s reward structure) affects the model’s recruitment power and educational effectiveness as compared to the standard PDI | Peer educator: PWIDs educate one another in the community about HIV prevention, and recruit peers for enhanced prevention services and education. In the Standard- PDI, IDU- recruiters are offered nominal monetary rewards for both recruiting peers and educating them of HIV- prevention information. In the Simplified- PDI, IDU- recruiters are similarly asked to educate and recruit their peers, but the reward for recruiting is woven into their education efforts. |
| Booth, RE et al. 66 | March - July 2006 | Simferopol and Nikolayev, Ukraine | PWIDs | 206 (61 peer leaders; 145 network members) | PDI (leader) based on social network and outreach model | Assess changes in needle-related risks behaviors | Intervention consisted of five sessions, delivered in small groups over three weeks, designed to motivate peer leaders to become educators within their injection network and provide them with skills training in how to effectively motivate their network members to reduce their HIV risk behaviors. Leaders were encouraged to model safer behaviors to their network members. Each session with the leaders consisted of role-plays and other interactive learning techniques. |
| Deering, KN et al. 67 | January 2007 – January 2008 | Vancouver, CA | HIV positive drug using FSWs | 20 | PDI (health advocates) based on social network design | Increased uptake and adherence to highly active antiretroviral therapy (HAART) | Intervention: weekly peer support meetings, capacity training for women to become health advocates or “buddies” to one another, a peer outreach service, and drop-in onsite nursing service. |
| Sherman, SG et al. 68 | 2009 | Chiang Mai, Thailand | Sexually active youth between 18–25 years on methamphetamine | 983 (Indexes = 415; Network Members = 568) | PDI (educator) based on social network design | Compare the efficacy of a network-oriented peer educator intervention (“peer education”) with a best practice standard life skills curriculum (“life- skills” condition) on methamphetami ne use, sexual risks, and incident STIs | RCT with two arms: Peer education and life-skills Interventions. Both the interventions were comprised of seven 2-hr sessions in a small group format. Sessions were comprised of educational discussions, engaging activities, and homework. |
| Booth, RE et al. 73 | 2004 – 2006 | Kiev, Odessa, and Donetsk, Nikolayev and Simferopol, in Ukraine | PWIDs | 722 | PDI (educator) based on social network design; individual intervention | Evaluate the effects of an individual intervention versus a network intervention on HIV-related injection and sexual risk behaviors | Peer educator intervention consisted of 5-sessions led by outreach workers, and delivered in small groups over 2 weeks. It was designed to empower peer educators to be mentors and provide them with training in how to effectively motivate their network members to reduce HIV risk behaviors. Peer educators were encouraged to model safer behaviors within their network. |
| Li, J. et al. 78 | December 2001 - May 2004 | Hartford, CT | PWIDs | 523 (112 - Peer Health Advocate s; 411 - social contacts) | Peer Health Advocate (PHA) interventions based on diffusion theory of social network model | To test the Risk Avoidance Partnership (RAP) intervention diffusion process and effects based on diffusion theory on processes of social change driven by PWUDs as PHAs within the networks of their peers. | The RAP intervention for PHAs was comprised of 10 sessions including 2-hr in-office sessions and field sessions in the community. The in-office sessions used both didactic and interactive methods to provide information, model peer intervention activities, and role-play delivery of the RAP peer intervention to other drug users in the community. PHA delivered this to their recruited social network members (individual level). Field sessions allowed PHAs to practice effective communication and demonstration of prevention strategies during monthly Community Advocacy Group meetings. Here PHAs organize and implement activities to advocate for and promote drug users’ health and well being at the community level. |
| Smyrnov, P et al. 80 | 2012 | Odesa, Kryvyi Rig, Zaporizhia, Mykolaiv and Bila Tserkva – Ukraine | PWIDs | 2273 | PDI with harm reduction strategies | Effectiveness in rejuvenating harm reduction (HR) projects | PDI used selected “seed” (PWIDs) that were trained to educate three peers who had never received harm reduction (HR) services. Activities include educating IDU-peers in the community about HIV prevention and harm reduction mechanisms and recruiting them to a storefront, where they are offered health/risk assessment interviews, free HIV- testing and counseling, and access to other services. Each recruit is offered the opportunity to serve as a recruiter and educator. |
| Latkin, CA et al. 87 | December 2002 – August 2006 | Philadelphi a, USA | PWIDs | 652 (Index = 232, Social network participan t = 420) | PDI based on social network model | Experimental PDI examined changes in social norms and relationships between HIV injection risk behaviors and social norms among PWIDs | RCT design with two arms: Index participants were divided into a peer education intervention and control condition. The intervention consisted of six 2-hour peer-educator sessions during a 4- week period and two booster sessions at 6 and 12 months after the intervention was completed. The index participants were trained to be peer educators: 1) how to promote safer sex and drug injection skills among network members, and 2) communication strategies to conduct peer outreach and promote norms about HIV risk reduction with their drug and sex network members. Participants were encouraged to model safer behaviors when they were with their peers. Control group did not receive any intervention. |
Note: PWIDs = People who injects drugs; PWUDs = People who uses drugs; PDI = Peer driven intervention; IDU = Injecting drug users; FSWs = Female sex workers
Table 2.
Methodology and Intervention design of Level III studies (K=13)
| Author | Randomization Method (if any) | Methods of Identifying Index | Method of Identifying social network members | Network Member Involvement | Comparison/Control Group |
|---|---|---|---|---|---|
| Broadhead, RS et al. 43 | None | Recruited through street outreach, word of mouth, ads and referrals from community agencies. | Peer educators identified and recruited network members who were previous sexual and/or drug using partners | Indexes and recruited network members became part of the study population | Yes. Comparison group is TOI |
| Heckathorn, DD et al. 44 | None | Recruited through street outreach, word of mouth, ads and referrals from community agencies. | Peers educators are motivated to recruit other drug users via a coupon system. | Indexes and recruited network members became part of the study population | Yes. Comparison group is TOI |
| Servegev, B et al. 46 | None | Recruited through street outreach, word of mouth, ads and referrals from community agencies | Peers educators are motivated to recruit other drug users via a coupon system. | Indexes and recruited network members became part of the study population | No |
| Broadhead, RS et al. 49 | None | There were no ‘indexes’. All participants were recruited through referrals from local health care providers and peers | From the study population, project staff identified HAs and peers and then assigned one HA to a peer. No two participants played both roles for one another. | All participants became part of the study. There was no distinction between index and network members | No |
| Latkin, CA et al. 54 | Randomly assigned in a ratio of 2:1 to the intervention or control condition respectively | Recruited through targeted outreach. Recruitment areas in Baltimore City were identified through ethnographic observations, focus groups, and geographical coding of drug- related arrests in Baltimore in the prior 3 years of the study | Index participants recruited network members | Indexes were asked to recruit a maximum of two network members for assessment at baseline and follow-ups. The network members did not receive the intervention | Yes. Control group with no intervention |
| Broadhead, RS et al. 58 | None | Indexes were referred to the project by local narcologists or physicians | Index participants recruited a maximum of 3 IDU peers from their community | Indexes and recruited network members became part of the study population | Yes. Standard PDI |
| Booth, RE et al. 66 | None | Peer leaders were recruited through street outreach by former IDUs | Index participants recruited a maximum of 3 IDU peers from their injecting network | Received communication from peer leaders, completed baseline and follow-up surveys. Network members did not receive the intervention | Yes. Individual based intervention |
| Deering, KN et al. 67 | None | There were no indexes. All participants were recruited into the PDI through referral by an HIV specialist, family care physician, or other health provider, friend, or by self-referral | Project staff allocated the pairing of a health advocate- peer dyad | All participants were part of the study population | No |
| Sherman, SG et al. 68 | Random allocation to two arms | Index participants were recruited based on an extensive 18- month formative, ethnographic research stage prior to the RCT | Index participants enrolled at least one of their sex or drug network members in the study within 45 days of screening. | Received communication/conversation from peer leaders, completed baseline and follow-up surveys. Network members did not receive the intervention | Yes. Comparison group is Life- Skill curriculum |
| Booth, RE et al. 73 | None | Peer educators and those in the individual intervention were recruited by recovering drug users serving as outreach workers | Index participants recruited a maximum of 3 members of their injecting network. | Received communication from peer educators, completed baseline and follow-up surveys | Yes. Comparison group is Individual Intervention. |
| Li, J. et al. 78 | None | Index participants or PHAs were recruited by outreach workers’ judgment, based on their familiarity with participants, about the candidates’ links in the drug-using community | Indexes were asked to refer 2 – 3 drug using peers (injection or non-injection heroin or cocaine/crack users) | Received intervention from PHAs, recruited in the study and completed baseline and follow-up social network egocentric surveys | No |
| Smyrnov, P et al. 80 | None | The health educators (HEs) chose active IDUs to serve as indexes, known to be knowledgeable of the local drug- using community | Index participants recruited a maximum of 3 members of their injecting network. | Indexes and recruited network members became part of the study population | Yes. Comparison group is TOI |
| Latkin, CA et al. 87 | Yes. Indexes were randomized into a peer education intervention or control condition | Index participants were identified through a community-based recruitment, which included ethnography and outreach in zip codes with high rates of HIV/AIDS cases based on data from the Philadelphia Department of Public Health. Outreach workers disseminated verbal and written information about the study | Peer educators identified and recruited network members from their sexual and or drug sharing networks | Received communication from peer educators, completed baseline and follow-up surveys. Social network members did not receive the intervention | Yes. Control group with no intervention |
Notes: PDI = Peer driven intervention; IDU = Injecting drug users; Peers are same as Indexes; TOI = traditional outreach intervention
Table 3.
Summary of outcome measures, major findings, and intervention related limitations of Level III studies (K=13)
| Author | Outcome measures | Important Results | Major Findings | Limitations |
|---|---|---|---|---|
| Broadhead, RS et al. 43 | HIV prevention education; HIV-risk behaviors (sharing syringes, sharing cookers and filters, sharing rinse water, frequency of injection, safer sex) | PDI outperformed the TOI with respect to the number of PWIDs recruited, the ethnic and geographic representativeness of the recruits, and the effectiveness of HIV prevention education. The costs of recruiting PWIDs into the intervention was one- thirtieth as much in the PDI as in the TOI. | In contrast to TOI, the PDI reached a larger and more diverse set of PWIDs at much less expense. | Participants were not randomly assigned to two groups; the lack of randomization in a quasi- experiment introduces the potential for bias resulting from differences among the study groups and sites. |
| Heckathorn, DD et al. 44 | HIV prevention education; HIV-risk behaviors (sharing syringes, sharing cookers and filters, sharing rinse water, frequency of injection, safer sex) | PDI outperforms the TOI with respect to number of people accessed, reductions in self- reported levels of HIV risk behavior and cost. | Network features such as structure, composition, and relations pay a dual role of both HIV transmission and increase the effectiveness of network-based HIV- prevention interventions. | Not mentioned |
| Servegev, B et al. 46 | HIV prevention education; HIV-risk behaviors (sharing syringes, sharing cookers and filters, sharing rinse water, frequency of injection, safer sex); and harm reduction | The rate of drug injection among the participants remained stable during the intervention until the third follow-up visit, when the rate dropped to 53% (p = 0.005). Results also suggested large and highly significant reductions in sharing of syringes, cookers/filters, and rinse water over time, which could be linked to the client’s continuing exposures to the intervention. | Not mentioned. | |
| Broadhead, RS et al. 49 | Retention in care (%of appointments kept), adherence to medication (pill- count) | Results support the feasibility of HIV positive drug users willingness and ability to play active roles in helping one another keep up with their medical treatments. The participants kept 95% of their appointments. The peers succeeded in keeping 80% of their health advocate’s appointments. The overall adherence score for all participants was 90%. 75% of participants enrolled in drug treatment by the end of the study. | The results suggest that an alternative social support structure to drug treatment is feasible for increasing active drug users’ adherence to medical care. | Single dyads may not be especially feasible for projects that work with larger numbers of individuals. Instead, use of “chains” consisting between five and eight participants was recommended for larger projects. This would allow subjects to substitute for no-shows at the weekly meeting by serving as both a peer and an advocate for those in attendance. A collective approach that relies on chains of participants can also pool and divide the rewards that participants- in-attendance collectively earn in any given week. Such a reward arrangement may further enhance the pressure that peers exert on one another to maintain high rates of adherence for the good of the group overall. Another challenge to replicate this project on a larger scale will be the recruitment of HDUs who are not receiving any medical care. |
| Latkin, CA et al. 54 | HIV-risk behaviors (Injection and sexual risk behaviors) | Experimental group were 3 times more likely to report reduction of injection risk behaviors and 4 times more likely to report increased condom use with casual sex partners compared to the control group. Participants in the experimental condition, compared with those in the control condition, were more likely to report talking about HIV with family members, sex partners, and drug users at the 6-month follow-up. | Results suggest that psychosocial intervention emphasizing social roles and incorporating peer outreach strategies, can reduce HIV risk in low- income and drug-using communities. | Not mentioned. |
| Broadhead, RS et al. 58 | HIV prevention education, HIV-risk behaviors (sharing syringes, sharing cookers and filters, sharing rinse water, frequency of injection, safer sex) | Both PDIs achieved high baseline recruitment rates, although the Standard-PDI out-performed the Simplified-PDI by approximately 35% (493 recruits versus 365 recruits, respectively). However, the IDU-recruiters in the Simplified-PDI did a significantly better job educating their recruits at both baseline (an average knowledge test score of 5.19 versus 4.07 on an 8-point scale) and at follow-up 6 months later (an average knowledge test score of 7.21 versus 5.56 on an 8-point scale). Both PDIs demonstrated about equal and significant efficacy in reducing respondents’ injection frequency, the sharing of syringes and other equipment, and rates of unprotected sex. | Holding all costs constant between the two interventions except for the different rewards offered to recruiters for educating peers and recruiting them to the project, the Simplified-PDI is approximately 50% less costly in respondent fees than the Standard-PDI although the latter results in a 35% higher recruitment rate. The study appears to have demonstrated that intervention projects get what they pay for. | This is a quasi- experiment, unable to control many variables that may have influenced the results. The cities had similar characteristics but were not identical. There may be other factors at work within the two cities, or in one but not the other, which are producing the differences. |
| Booth, RE et al. 66 | HIV-related injection and sexual risk behaviors | Both peer educators and network members in the network intervention reduced injection-related risk behaviors significantly more than did those in the individually based intervention. Peer educators increased condom use significantly more than did those in the individual intervention. Individual intervention participants, however, showed significantly greater improvements than did network members with respect to reductions in sexual risk behaviors. | Social network interventions may be more effective than individually based interventions in changing injection risk behaviors among both peer educators and network members | Although there were many similarities between the two studies, possible differences cannot be eliminated. |
| Deering, KN et al. 67 | Pharmacy records (PR) and indirectly with self-report adherence and viral load (VL) outcomes, risk behaviors including drug use and unstable housing | Overall self-reported adherence was high (92%) and most women (11) reported increased adherence from the first to the last 13 PDI meetings attended (average increase = 18%). The number of viral load tests ≤ 50 copies/mL increased by 40% from the pre-PDI period (1 year before enrollment), to the PDI period (duration enrolled). PR adherence and improvements in VL outcomes were higher among participants with greater housing instability and frequency of injecting/smoking drugs. | The study suggests that the PDI may have had a positive impact on adherence and HIV treatment outcomes. Although this would not predict long-term treatment success, the PDI approach to HIV treatment support is a promising program for women who might otherwise be excluded from treatment altogether. | Did not have a comparison group for the PDI attendees. |
| Sherman, SG et al. 68 | Self-reported methamphetamine use; condom use; incidence of STI | Over time, participants in both conditions showed a significant and dramatic decline in self-reported methamphetamine use (99% at baseline versus 53% at 12- months, p <0.0001) and significant increase in consistent condom use (32% baseline versus 44% at 12 months, p <0.0001). Incident STIs were common, with no differences between arms. Chlamydia had the highest incidence rate, 9.85/100 person-years and HIV had a low incidence rate of 0.71/100 person-years. | The study found that a peer educator intervention was associated with reductions in methamphetamine use, increases in condom use, and reductions in incident STIs over 12 months. Parallel reductions with the life-skills condition were also significant. Small group interventions are an effective means of reducing methamphetamine use and sexual risk among Thai youth. | Firstly, the study utilized nonrandom sampling recruitment methods and had inclusion criteria regarding regular sexual behavior and methamphetamine use; therefore generalizability of the study’s results could be limited. Secondly, condoms were available to study participants who were underwent HIV/STI counseling and testing as well as upon request. This could have affected condom use in both arms but we do not know the extent that this effected condom use over time. Lastly, there is the possibility that tight social networks were randomized to both control and intervention arms, leading to a high degree of contamination that resulted in a bias towards the null. |
| Booth, RE et al. 73 | Needle risks, perceived risks, injection related risk behaviors | Peer leaders recruited an average of 2.4 network members; two-thirds attended at least four of the five training sessions; and a positive relationship was observed between greater session attendance by peer leaders and increased communication with network members about HIV prevention. Leaders who did not engage in high-risk behaviors at follow-up were much more likely to have had network members who did not engage in high-risk activities compared to leaders who continued high- risk behaviors. | The findings from this study suggest that a peer leader intervention approach to reducing HIV risk behaviors among IDUs in Ukraine may be effective. | The peer leaders were identified as leaders either by outreach workers or by the members of their network. It is not possible to know how representative the samples were of IDU leaders or their standing within their network. The absence of a comparison condition of IDUs not receiving the peer leader intervention prevented from making causal inferences. |
| Li, J. et al. 78 | Adoption of innovative peer intervention delivery (self reported ‘gave’ intervention ties and self reported “received intervention ties); reduction of HIV transmission risk behaviors | The RAP innovation of peer intervention delivery and modeling had clearly diffused from PHAs to their network members and to the broader drug using community. At 6- months follow-up, more than 90% of trained PHAs had become active peer interventionists, and more than 2/3 of all study participants had adopted the peer intervention delivery and modeling innovation. Innovation diffusion is likely to reach a “critical mass” and will be efficiently adopted by the rest of the population. Sociometric network analysis showed that adoption of and exposure to an intervention was associated with proximity to a PHA, being directly linked to multiple PHAs, and being located in a network sector where multiple PHAs were clustered. | The network analysis of the RAP intervention diffusion process demonstrated that training active drug users as peer interventionist can be successful, has the potential to reach a “critical mass”, cost- effective than RCTs, and is delivered and adopted at multiple levels (individual, network, and community). | Network analysis for this study continued for 3- year long pre- and post- intervention design with only two time-point measures for each participant. It was possible that fine differences and trends in effects were not measured between the two-points. For example, network ties used in these analyses reflected relations at two time points for each participant (his/her own baseline and 6-month surveys); some of these ties may not have been continuous over the 3- year period of data collection. Another limitation of the study is the lack of a control group. |
| Smyrnov, P et al. 80 | Number and composition: age, gender) of new recruits; knowledge test score | PDIs recruited 455 new respondents on average in each city during their six months of operation, indicating that the PDI was 6.3 times more powerful as a recruitment mechanism. Compared to TOI, the PDIs resulted in significant increases in the recruitment of women- and young- injectors, and IDUs who injected a more diverse variety of drugs. | The PDI can have a rejuvenating effect when added to HR projects. There was an increase in the number and diversity of new IDU-respondents, thereby reaching hard-to- reach critical population. | The PDI model did not perform equally in all sites, which called for more detailed analyses of contextual or geographical effects of the sites on the model’s performance. There was no pre/post test comparison of respondents’ knowledge scores, which limited the ability to conclude with confidence about the PDI’s effectiveness in increasing respondents’ overall knowledge levels. Nor can respondents’ knowledge test scores be viewed as a simple measure of recruiters’ educational effectiveness. Another limitation of the study was the inability to measure respondents’ response to the PDI’s reward structure by demographics or type of drug used. Although the PDI demonstrated statistically significant increases in the number and proportion of new recruits by age, gender and types of drug used, because we cannot exclude other possible explanations for these increases. |
| Latkin, CA et al. 87 | Injection related HIV risk behaviors (sharing needles, sharing cookers, sharing cotton, front/back-loaded); social norm of these 4 risk behaviors | There was a statistically significant intervention effect on all four social norms of injection behaviors, with participants in the intervention reporting less risky social norms compared with controls. There was statistically significant bidirectional association with social norms predicting injection risk behaviors at the next assessment and risk behaviors predicting social norms at the subsequent visits. Through social network interventions it is feasible to change both injection risk behaviors and associated social norms. | It is critical that social network interventions focus on publically highlighting behavior changes, as changing social norms without awareness of behaviors change may lead to relapse of risk behaviors. | The assessment of social norms may have overlap with some of the risk behaviors. Since these behaviors are social behaviors, the basis of making judgments about social norms may be due in part to observations of one’s own behaviors. In the data analyses, collapsing norms and behaviors into dichotomous variables reduced investigators ability to examine linear trends. |
Notes: TOI = Traditional outreach intervention; PDI = Peer driven intervention; PWIDs = People who injects drugs; PWUDs = People who uses drugs; HDUs = HIV-positive drug users; HR = Harm reduction
RESULTS
Descriptive Characteristics
Among the final 58 studies, 11 (19%) were conducted in the 1990s (24, 37–46), 24 (41%) from 2000 to 2009 (20, 47–69), and 23 (40%) studies after 2009 (30, 70–89). The populations in the studies were divided into two broad groups: 1) PWID/PWUD and HIV-infected and 2) individuals at high-risk for HIV who used or injected drugs. Some specific high-risk groups were homeless men (82, 84), homeless youth (45, 64, 72), black men who have sex with men (MSM) (63), HIV-infected women (61, 74), and female sex workers (FSW) (37, 62, 67). The sample size of the studies varied significantly with the majority of studies (64%) sampling 250 to 1000 participants. Two were pilot studies with sample sizes fewer than 25 participants (49, 67) and two were large-scale multi-site studies with sample sizes over 2000 participants (80, 83). Using World Bank’s designation (90) for country income level, most studies (k=50, 86%) were conducted in high-income countries, three studies in upper middle-income countries (62, 65, 68), four studies in lower middle-income (66, 73, 76, 80), and none in low-income countries. Fifty-one studies (88%) were conducted in the United States, Canada, or Europe, four studies in East and Southeast Asia (68, 76, 77, 85), three in Central America (50, 56, 65), one in South Africa (62), and no studies were conducted in Australia or South America (Figure 2). The studies that focused on HIV prevention were primarily conducted in the United States or Europe (88%), with few in South-Southeast Asia, Central America, and Africa. All studies where outcome measures were associated with the various steps of the HIV-care continuum of care, however, were conducted in North America, including studies on: HIV-testing (61, 72) (New York, Iowa, and Nebraska), linkage to care (70) (San Francisco), retention in care (39, 49, 57) (San Francisco, Connecticut, and Maryland), and ART adherence and viral suppression (49, 67) (Connecticut and Vancouver) (Figure 2). No studies focused on ART prescription.
What are the different ways SNA and SNI are conducted, analyzed, and reported in the studies?
Based on how social network approaches were conducted, we divided the included studies into three categories: Level I, II, and III.
Level I (Social Network Analysis)
Studies where i) social networks, including support and risk networks, were described in terms of their size (38, 40, 42, 74, 86), composition (19, 51, 53, 56, 72, 84), and structure (30, 37, 59, 66), ii) sociometric and/or egocentric network analyses were conducted to calculate network metrics such as centrality (30), density (38, 40, 42, 63), assortivity, and constraints, iii) network metrics were used as predictor variables in statistical/mathematical models to identify correlates of substance use and HIV/AIDS were included in this category. There were 37 (64%) studies in Level I. One consistent trend identified in the majority of these studies (85%) was that univariate, bivariate, and multivariate statistical analyses were conducted with the calculated network properties or metrics. The most common sequence of analytical steps was to first describe the summary statistics of the network properties; second, conduct a bivariate cross-tabulation or correlation between the outcome variables and the network properties; and third, include the network properties as variables with individual level variables in a multivariate regression analysis. It is important to note here that for these studies, SNA was used to support the preprocessing and creation of new variables to quantify social relationships and was not the primary analytical technique of the methodology.
Level II (Respondent Driven Sampling)
This category included studies that exclusively reported using social networks for sampling, such as RDS or contact sampling. Most of the studies focused on the mathematics and statistics of the sampling design and then subsequently conducted a descriptive analysis of the participants and their social networks. There were 8 studies (14%) in Level II (41, 65, 69, 77, 83, 88, 89).
Level III (Social Network Interventions)
Studies that reported the involvement of peers and/or network members and used the results of a typical whole or egocentric network analysis as part of an HIV prevention and treatment intervention were classified as Level III studies. There were 13 studies in Level III (43, 44, 46, 49, 54, 58, 66–68, 73, 78, 80, 87).
What is the distribution of the network approaches in terms of their application in addressing outcome measures associated with HIV prevention and stages of a HIV care continuum?
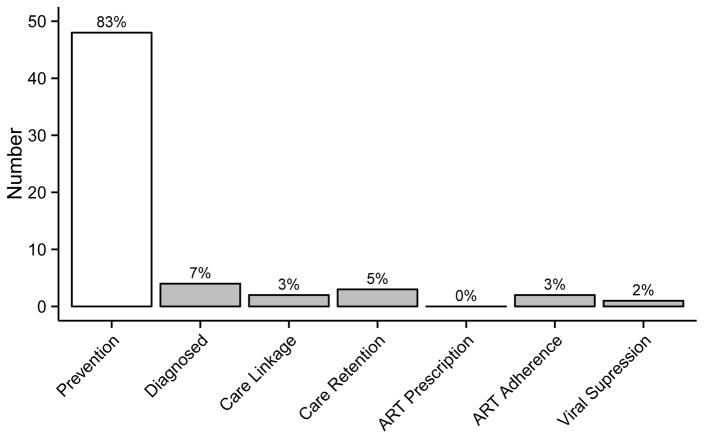
The majority of studies (k = 48, 83%) focused on HIV prevention, whereas a few (k = 10, 17%) addressed the different steps in the HIV care continuum. Only four studies included outcome measures associated with HIV diagnosis and testing (7%) (61, 72, 76, 88), five (9%) (39, 49, 57, 70, 89) for HIV care linkage and retention, and even fewer for ART adherence (k=2, 3%) (49, 67) and viral suppression (k=1, 2%) (49). ART prescription, a crucial step between being eligible for and initiating ART, was not addressed at all (Figure 4). A cross-tabulation of social network approaches (Level I, II, and III) with outcome measures further provided important results (Figure 3). In line with Figure 4, Figure 3 also showed the considerable concentration of research on HIV prevention across the Level I, II, and III studies (above 80%). Less than 10% of the studies were applying the potential of social network approaches to address HIV care and treatment. Among the studies in the Levels I and II, only eight studies (18%) addressed three components of the HIV care continuum: HIV diagnosis, HIV care linkage, and retention (39, 57, 61, 70, 72, 76, 88, 89). Additionally, of the thirteen social network intervention (Level III) studies, only one study, which was a pilot intervention (sample size = 20), had a primary biological outcome of viral load and a secondary outcome measure of adherence to ART (pharmacy records and self-reported adherence) (67). Another pilot intervention (sample size = 14) measured retention in HIV care (percentage of appointments) and ART adherence (pill-counts) as primary outcomes (49).
Figure 4.
Distribution of selected studies categorized by outcome measures of HIV prevention and Care Continuum
How are the social network members recruited, identified, and involved in the SNIs?
All 13 SNIs were based on the conceptual framework of ‘peer-driven-interventions’ (PDI) with minor variations. The basic framework of a typical PDI involves two stages: first, peers, or index participants, are recruited and provided training to understand and perform in a HIV prevention or treatment intervention; second, peers deliver the intervention among family or members from their drug and sexual networks in the community.
In most studies (64, 65, 67, 79, 87, 94, 99) identified in this review, the peers were recruited through street outreach, word of mouth, advertisements, and referrals from community health agencies and former drug users. Latkin et. al.(54, 87) and Sherman et. al.(68) followed a much more targeted outreach strategy to recruit peers from the cities of Baltimore and Philadelphia (USA) and Chiang Mai (Thailand), respectively. The targeted recruitment procedures included ethnographic observations, focus groups, and stratified sampling based on geographical units (e.g. zip codes or US Census block groups) with higher drug-related arrests or higher prevalence of HIV/AIDS (Table 2). An alternative strategy deployed by Broadhead et. al. was that the RDS and PDI were linked. The RDS was used to recruit and identify peers within the network in which the health advocate and peers would work to reduce HIV transmission (91).
The composition of the recruited peers and social network members also varied. For SNIs focused on HIV prevention (k=11), peer educators or leaders recruited participants from their drug using and/or sexual social networks. Of these eleven, there were six studies (56%), where the both the peer and their recruited social network members, had equal participation in the study, and everyone received the intervention (43, 44, 46, 58, 78, 80). In the remaining five studies (44%), network members did not participate in the intervention directly, but were recipients of diffusion of HIV prevention information from peers and participated in the baseline and/or follow-up assessments (54, 66, 68, 73, 87). For the SNIs focused on HIV treatment (k=2), the project personnel identified the health advocates (HAs) and their peers from the enrolled study population (49, 67) (Table 2).
In most of the identified interventions (k=10/13, 77%), peers played the role of educators of HIV prevention information. In the remaining three studies (49, 67, 78), peers played the role of health advocates or health buddies supporting each other to improve adherence to ART and retention in HIV care (Table 1). The HIV prevention interventions in these studies included: providing educational information on practicing and promoting safe sexual and drug using behaviors with social network members throughout the study period (43, 44, 46, 58, 80); distribution of materials such as bleach, condoms, and needles in the community (44, 46, 80); and hands-on experimental sessions on HIV prevention education of 90–120 minutes over a period of 2 to 4 weeks. The experimental sessions included information on communication strategies to conduct peer outreach and how to promote social norms and act as a role model in the community (54, 66, 68, 73, 87). As part of the intervention, peers also recruited other substance users from their social networks to become peer educators, thereby reaching a larger group in the community. The HIV care and treatment interventions included weekly sessions where peers serving as health advocates encouraged other participants on keeping their clinical appointments, responding to physicians’ referrals, picking up prescriptions on time, and adhering to ART (49, 67). The theoretical frameworks used in the SNI included behavior change theories, social identity theory, social cognitive theory, diffusion theory, and social support theories.
What type of effect did the SNIs have on the intervention outcomes?
All the nine HIV prevention studies that included controls showed substantial improvement in more than one HIV-risk reduction behavior (sharing syringes, sharing cookers and filters, frequency of injection, unprotected sex) and HIV education communication among social networks comparing control and intervention conditions (43, 44, 46, 54, 58, 66, 68, 78, 80). Four studies documented that SNIs, compared to the control conditions, were successful in recruiting a higher proportion of hard to reach at-risk population, which is the first step of any HIV prevention or treatment programs (43, 44, 58, 80) (Table 3). The recruited population had diverse ethnic backgrounds (43), wide geographic distribution (43), low-income (54), women, young-injectors, and people who injected a variety of drugs (80). HIV prevention outcome measures were assessed in four studies at multiple follow-up periods (54, 58, 68, 78): HIV education communication among groups (e.g. peers and social network members) was higher at 6 month follow-up (54, 58), more than 90% of the peers or indexes (e.g. peer health advocates) became active peer interventionists and two-third of study populations had adopted the intervention by the 6 month follow-up (78), reduction in methamphetamine use and increase in condom use were evident at the 12 month follow-up (68), and decrease in drug injection started by the 3 month follow-up (46) (Table 3). One study (73), however, showed that the comparison group (individual intervention) experienced significantly greater reductions in sexual risk behaviors than the SNI group.
Both social network-based HIV treatment interventions were pilot studies and successfully showed the feasibility of HIV infected drug users’ willingness and ability to provide direct social support to their peers (49, 67). In Broadhead et. al.(49), health advocates (HAs) succeeded in keeping 80% of their peers’ HIV care appointments. Additionally, medication adherence score for all participants (peers and health advocates) was 90%, and 75% of participants enrolled in drug treatment by the end of the study. Results from the Deering et. al. (67) intervention were supporting, showing that with increasing frequency of intervention meetings, the self-reported rate of ART adherence increased and by the end of the intervention period, overall ART adherence was as high as 92% among FSWs with HIV and who used drugs. The number of participants achieving viral suppression (HIV-1 RNA<50 copies/mL) increased by 40% from the pre-intervention period (one year before enrollment) to the end of the study (duration enrolled) (67). Although the encouraging results from these two pilot studies do not predict long-term treatment successes, the SNI approach to HIV treatment was a promising strategy for vulnerable population who might otherwise be excluded from the HIV care continuum altogether.
DISCUSSION
This systematic scoping review describes how SNA and SNI was measured, analyzed, and utilized to examine the influence of social networks on HIV prevention, and treatment outcomes for substance-using people with or at-risk for HIV. To the best of our knowledge, this is the first review with a primary focus on evaluating the state of research in SNA and SNI-based studies, which are sustainable and cost-effective strategies to improve behavior change and reach hidden populations (92).
What was striking was that the majority of the studies (Level I and Level II) conducted egocentric SNA as an exploratory tool to sample hidden populations, quantify interpersonal relationships, and describe the structural characteristics of risk and support networks. Here, SNA was not the primary methodology deployed but facilitated in calculating network variables for confirmatory or causal analysis using other mathematical and statistical models. Even when a range of modeling techniques provided convincing evidence that risk behaviors for HIV transmission and loss from HIV care continuum were linked to network factors, few studies (k=10, 27%) recommended optimizing the advantages of these approaches for implementing network-based interventions. Of the 58 included studies, only 13 conducted SNIs. This clearly reflects a lack of research involving social networks as part of an intervention and underscores for the imperative for future network interventionists to fill this critical research gap.
Another prominent finding of this systematic scoping review was that social network approaches were utilized predominantly for HIV prevention research (83%). This trend was true for all three levels of studies. A plausible explanation could be that HIV prevention had been emphasized more by funders or, alternatively, the achievements in HIV prevention were needed to spur innovation for its use in treatment. This is supported by relatively recent findings that HIV treatment is an extremely effective strategy for prevention (93–95). Few studies from Level I and II had primary or secondary outcomes associated with the first two steps of HIV continuum (diagnosis and linkage to HIV care) and none for the later stages (ART adherence and viral suppression). Interestingly, except for one study conducted in southern India (76), all HIV treatment based studies were located in the United States.
Among the thirteen SNIs studies, only two studies strategically targeted one or more steps along a HIV care continuum (49, 67). For example, the outcome measures in Broadhead et. al.(49), conducted in New Haven, CT in 2002, were retention in care and ART adherence. A biological outcome of viral load was measured in only one study conducted by Deering et. al. (67) in Vancouver in 2006. These two HIV treatment studies were conducted at a time (between 2002 and 2006) when HIV prevention research was perhaps the major focus worldwide. Even though the results supported the feasibility of SNI, where drug-using PLH serving as health advocates were capable of providing support to their network members to remain engaged in HIV care and ultimately achieve viral suppression, the two studies were pilot interventions with sample sizes less than 25 participants. It is unclear whether the authors later adapted these pilot studies to large-scale interventions, but findings suggest that larger challenges existed with intervention expansion for HIV treatment (96). Regardless, these finding undoubtedly show that although there has been considerable progress of social network research in HIV prevention, there still remains a wide gap in utilizing the potential of SNIs in HIV treatment research.
What are some of the advantages and disadvantages of SNIs, which make them a common approach for HIV prevention interventions but not so prevalent in HIV care and treatment research? Social network-based HIV prevention and care interventions have several advantages that were highlighted in the included studies. Eleven of the thirteen studies (Level III) showed substantial reductions in HIV-risk behaviors and increase in HIV prevention communication among social network members. Among these eleven studies, five studies showed sustained positive effects of the interventions beyond the study period indicating that SNIs could be an effective sustainable approach. The remaining two studies showed the feasibility of HIV treatment interventions with drug-using PLH as peer health educators. Most importantly, these SNIs all used social networks that were defined by the study participants themselves. The Community Popular Opinion Leader (CPOL) or the Targeted Outreach Intervention (TOI) models chose leaders from the community with a possibility of missing smaller yet critical social networks that impact one’s daily interactions (92, 97). In most of the reviewed SNIs, the network members were either directly involved in the intervention or indirectly when receiving information from the peers. This structure has the potential of delivering an intervention to a larger population at a much lesser cost. In addition, the majority of studies had higher retention rates (exceeding 80%) at the last follow-up visits. This further suggests that groups who are recruited through social network based methods may be better connected and easier to follow and retain compared to non-network recruitment methods. Thus, SNIs may also be valuable for recruiting hard-to-reach populations and giving peers an opportunity to serve a positive role for individuals who are members of disenfranchised and stigmatized groups in the community.
This systematic scoping review also highlighted several limitations of SNIs. First, contamination has been a persistent challenge in these studies, whereby individuals in the experimental intervention group talk to and encourage those in the control group to alter their behaviors. This scenario is more critical for studies that use densely connected social networks. However, while contamination does impact the evaluation of effect sizes by biasing towards the null hypotheses, it does not compromise the end goal of implementing network based HIV prevention and treatment interventions. In a recent study, Simmons et. al.(98) evaluated a measure based on recall of intervention terms to assess contamination in a randomized, prospective trial of a social network-based, peer-driven education intervention. Another approach is to consider location and geographic distance between the experiment and the control groups to assess contamination. If experimental and controls are in close proximity for several minutes, that could be a measure of potential contamination.
Second, instability and incidents of rapid network turnover may prohibit sufficient interaction between peers educators, health advocates, or support groups with their respective social network members. Such limited interactions may prohibit effective diffusion of intervention and behavior change. This limitation will disproportionately affect HIV treatment interventions because peers need to encourage and support each other consistently and in a timely manner to stay on HIV care, pick up prescriptions, and adhere to medications. To circumvent this limitation, a plausible solution would be to train a sufficient number of peers to ensure their steady presence. For SNIs to become a widely adopted approach for HIV treatment, however, cutting edge analytical techniques for collecting sociometric data and modeling network change over time must be developed.
Third, for SNIs to perform effectively, the peers should be motivated, willing, and able to recruit network participants as well as deliver accurate information among their social networks. For example, it is possible that peer educators, instructed to deliver specific intervention content among their network members or in the community, might alter the content of the actual intervention. While PDIs are culturally competent because they allow information to be expressed as it would among peers, health educators often need to ensure that accurate intervention content is included. It is also possible that in interventions where peers are trained to be leaders or role models, they refuse to reduce their own high-risk behaviors.
Fourth, for HIV treatment interventions, it is important to assess the disclosure dynamics of an individual’s HIV status to their social network members (96). This is related to another long lasting issue of what type of information can be ethically collected or shared among the social network members. For interventions focused on measures related to retention in HIV care and ART adherence, a lot of personal health information will be required to be disclosed to peers for them to effectively support each other with their HIV treatment regimen. This will further complicate the protocol of whom and how participants (including peers and social network members) need to be consented during a social network based intervention. Last, another challenge for interventions targeting to increase retention in HIV care is to recruit a control population of PLH with no medical care. This could also raise ethical and moral issues for researchers of not providing medical care to PLH who are in need.
LIMITATIONS
While rigorous methods were used to identify studies and extract information to inform collective knowledge on HIV-related SNA and SNIs in substance users, some limitations do exist. The included studies differed substantially in their study design, duration of the intervention, timing of outcome assessment, and outcome measures used. The high degree of heterogeneity in both the studies and the reporting of outcomes precluded a meta-analysis (35, 36, 99, 100). Studies (with same study population and data) that used both egocentric SNA and SNI but reported findings in different peer- reviewed journal articles were included twice: egocentric analysis study was included in Level I and SNI in the Level II categories. Additionally, the thirteen SNI studies that we reviewed had different recruitment methods and differed slightly in the way in which networks were defined and analyzed. Measurement of study quality was not conducted because currently there is no gold standard for assessing study quality in social network based intervention studies. Finally, although we conducted an extensive search of the literature databases, it is possible that our review missed some studies where SNA and/or SNI were conducted only on PLH but who were not active substance users. Even when peer outreach is central to HIV prevention efforts for PWUDs and/or PWIDs, many studies do not assess network components and social diffusion of information and behavior change. In addition, there may be studies where social-structural settings, such as bars or shooting galleries, are conceptualized as networks settings for diffusion of intervention for behavior change. However, such studies do not directly or indirectly involve existing social network members in the intervention.
CONCLUSIONS AND IMPLICATIONS FOR FUTURE RESEARCH AND PRACTICE
This systematic scoping review began by discussing the presence of large amount of evidence that showed the positive influence of social networks and network-based interventions on HIV prevention and treatment outcomes. Some studies have also reported sustained benefits beyond the study period. Due to the heterogeneity and lack of clarity of network-based approaches and how they strategically targeted one or more steps along a HIV care continuum, this paper systematically identified the dominant patterns of using SNA and SNI methods and showed the pressing need for more SNI research at various care stages, especially those addressing ART prescription. The review also highlighted the potential advantages of SNIs as a sustainable approach and whose effects continue beyond the study period. They are also cost-effective strategies to deliver an intervention to a larger population, recruit from hard to reach populations, and provide an opportunity for members of disenfranchised groups in the community to serve as a positive role for individuals. Based on the limitations of social network approaches identified by the review there are several implications for future research on best theoretical and applied practices: recruiting intervention and control groups, training an effective group of peer educators or care supporters, assessing relationship between treatment regimen and behavior changes over time, and maximum diffusion of intervention in a cost effective way. The goal of the next generation of network interventionists, therefore, is to ensure that research practices are aligned with the complexities of social network dynamics and optimally use the power of social networks to reduce HIV transmission and optimize HIV care.
Acknowledgments
The authors would like to thank Librarian Janis Glover from Yale University for assistance with search strategy and comprehensive searches from the multiple databases. For this study, the authors DG (K01DA037794) and FLA (K24DA017072 and R01DA030768) were funded by the National Institute of Health.
Funding: This study was funded by National Institute of Health (K01DA037794; K24DA017072 and R01DA030768).
Footnotes
COMPLIANCE WITH ETHICAL STANDARDS
Ethical Approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Joint United Nations Programme on HIV/AIDS. 90-90-90- An ambitious treatment target to help end the AIDS epidemic. New York: 2014. [Available from: http://www.unaids.org/en/resources/documents/2014/2090-2090-2090. [Google Scholar]
- 2.Kamarulzaman A, Altice FL. Challenges in managing HIV in people who use drugs. Current opinion in infectious diseases. 2015;28(1):10–6. doi: 10.1097/QCO.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook C, Bridge J, McLean S, Phelan M, Barrett D. The funding crisis for harm reduction: Donor retreat, government neglect and the way forward. London, UK: International Harm Reduction Association; 2014. [Google Scholar]
- 4.Stein J, Newcomb M, PMB An 8-year study of multiplt influences on drug use consequences. J Pers Soc Psychol. 1987;53:1094–105. doi: 10.1037//0022-3514.53.6.1094. [DOI] [PubMed] [Google Scholar]
- 5.Krishnan A, Brown SE, Ghani M, Khan F, Kamarulzaman A, Altice FL. Pre-treatment Drug Use Characteristics and Experiences among Patients in a Voluntary Substance Abuse Treatment Center in Malaysia: A Mixed Methods Approach. Substance Abuse. 2016 doi: 10.1080/08897077.2016.1146648. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu J, Witkiewitz K. Network support for drinking: an application of multiple groups growth mixture modeling to examine client-treatment matching. J Stud Alcohol. 2008;69(1):21–9. doi: 10.15288/jsad.2008.69.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu LT, Ling W, Burchett B, Blazer DG, Yang C, Pan JJ, et al. Use of item response theory and latent class analysis to link poly-substance use disorders with addiction severity, HIV risk, and quality of life among opioid-dependent patients in the Clinical Trials Network. Drug and alcohol dependence. 2011;118(2–3):186–93. doi: 10.1016/j.drugalcdep.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimbrough LW, Fisher HE, Jones KT, Johnson W, Thadiparthi S, Dooley S. Accessing social networks with high rates of undiagnosed HIV infection: The social networks demonstration project. American Journal of Public Health. 2009;99(6):1093–9. doi: 10.2105/AJPH.2008.139329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gorbach PM, Sopheab H, Phalla T, Leng HB, Mills S, Bennett A, et al. Sexual bridging by Cambodian men - Potential importance for general population spread of STD and HIV epidemics. Sexually Transmitted Diseases. 2000;27(6):320–6. doi: 10.1097/00007435-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Jenness SM, Neaigus A, Hagan H, Murrill CS, Wendel T. Heterosexual HIV and Sexual Partnerships Between Injection Drug Users and Noninjection Drug Users. Aids Patient Care and Stds. 2010;24(3):175–81. doi: 10.1089/apc.2009.0227. [DOI] [PubMed] [Google Scholar]
- 11.Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Social Science & Medicine. 2003;56(3):465–76. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- 12.Latkin CA, Mandell W, Vlahov D. The relationship between risk networks’ patterns of crack cocaine and alcohol consumption and HIV-related sexual behaviors among adult injection drug users: A prospective study. Drug and Alcohol Dependence. 1996;42(3):175–81. doi: 10.1016/s0376-8716(96)01279-3. [DOI] [PubMed] [Google Scholar]
- 13.El-Bassel N, Chen DR, Cooper D. Social support and social network profiles among women on methadone. Social Service Review. 1998;72(3):379–401. [Google Scholar]
- 14.Prentice D, Miller D. Pluralistic ignorance ans alcohol use on campus: some consequences of misperceiving the social norm. J Pers Soc Psychol. 1993;64:243–56. doi: 10.1037//0022-3514.64.2.243. [DOI] [PubMed] [Google Scholar]
- 15.Goehl L, Nunes E, Quitkin F, Hilton I. Social networks and methadone treatment outcome: the costs and benefits of social ties. Am J Drug Alcohol Abuse. 1993;19(3):251–62. doi: 10.3109/00952999309001617. [DOI] [PubMed] [Google Scholar]
- 16.De P, Cox J, Boivin J-F, Platt RW, Jolly AM. Social network-related risk factors for bloodborne virus infections among injection drug users receiving syringes through secondary exchange. J Urban Health. 2008;85(1):77–89. doi: 10.1007/s11524-007-9225-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Latkin CA, Davey MA, Hua W. Social context of needle selling in Baltimore, Maryland. Substance Use & Misuse. 2006;41(6–7):901–13. doi: 10.1080/10826080600668720. [DOI] [PubMed] [Google Scholar]
- 18.el-Bassel N, Cooper DK, Chen DR, Schilling RF. Personal social networks and HIV status among women on methadone. AIDS Care. 1998;10(6):735–49. doi: 10.1080/09540129848352. [DOI] [PubMed] [Google Scholar]
- 19.Gordon AJ, Zrull M. Social networks and recovery: one year after inpatient treatment. Journal of Substance Abuse Treatment. 1991;8(3):143–52. doi: 10.1016/0740-5472(91)90005-u. [DOI] [PubMed] [Google Scholar]
- 20.El-Bassel N, Gilbert L, Wu E, Chang M. A social network profile and HIV risk among men on methadone: do social networks matter? J Urban Health. 2006;83(4):602–13. doi: 10.1007/s11524-006-9075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Latkin C. A persona network approach to AIDS prevention: an experimental peer group intervention for street-injecting drug users: the SAFE study. NIDA Research Monograph. 1995;151:181–95. [PubMed] [Google Scholar]
- 22.Neaigus A, Friedman S, Goldstein M, Ildefonso G, Curtis R, Jose B. Using dyadic data for a network analysis of HIV infection and risk behaviors among injecting drug users. NIDA Research Monograph. 1995;151:20–37. [PubMed] [Google Scholar]
- 23.Friedman S. Promising social network research results and suggestions for a research agenda. NIDA Research Monograph. 1995;151:196–215. [PubMed] [Google Scholar]
- 24.Neaigus A, Friedman SR, Curtis R, Des Jarlais DC, Furst RT, Jose B, et al. The relevance of drug injectors’ social and risk networks for understanding and preventing HIV infection. Social Science & Medicine. 1994;38(1):67–78. doi: 10.1016/0277-9536(94)90301-8. [DOI] [PubMed] [Google Scholar]
- 25.Latkin CA, Mandell W, Vlahov D, Oziemkowska M, Celentano DD. The long-term outcome of a personal network-oriented HIV prevention intervention for injection drug users: The SAFE study. American Journal of Community Psychology. 1996;24(3):341–64. doi: 10.1007/BF02512026. [DOI] [PubMed] [Google Scholar]
- 26.Miller M, Paone D. Social network characteristics as mediators in the relationship between sexual abuse and HIV risk. Social science & medicine. 1998;47(6):765–77. doi: 10.1016/s0277-9536(98)00156-7. [DOI] [PubMed] [Google Scholar]
- 27.Adimora AA, Schoenbach VJ, Doherty IA. HIV and African Americans in the southern United States: sexual networks and social context. Sexually transmitted diseases. 2006;33(7 Suppl):S39–45. doi: 10.1097/01.olq.0000228298.07826.68. [DOI] [PubMed] [Google Scholar]
- 28.Young AM, Jonas AB, Mullins UL, Halgin DS, Havens JR. Network structure and the risk for HIV transmission among rural drug users. Aids Behav. 2013;17(7):2341–51. doi: 10.1007/s10461-012-0371-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedman SR, Neaigus A, Jose B, Curtis R, Goldstein M, Ildefonso G, et al. Sociometric risk networks and risk for HIV infection. American Journal of Public Health. 1997;87(8):1289–96. doi: 10.2105/ajph.87.8.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gyarmathy VA, Caplinskiene I, Caplinskas S, Latkin CA. Social Network Structure and HIV Infection Among Injecting Drug Users in Lithuania: Gatekeepers as Bridges of Infection. Aids and Behavior. 2014;18(3):505–10. doi: 10.1007/s10461-014-0702-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Howard DL, Latkin CA. A bridge over troubled waters: factors associated with non-injection drug users having injection drug-using sex partners. Journal of acquired immune deficiency syndromes. 2006;42(3):325–30. doi: 10.1097/01.qai.0000214819.88163.22. [DOI] [PubMed] [Google Scholar]
- 32.Albarracin D, Tannenbaum MB, Glasman LR, Rothman AJ. Modeling structural, dyadic, and individual factors: the inclusion and exclusion model of HIV related behavior. AIDS and behavior. 2010;14(Suppl 2):239–49. doi: 10.1007/s10461-010-9801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Latkin C, Weeks MR, Glasman L, Galletly C, Albarracin D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS and behavior. 2010;14(Suppl 2):222–38. doi: 10.1007/s10461-010-9804-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arksey H, O’Malley L. Scoping studies: Towards a Methodological Framework. International Journal of Social Research Methodology. 2005;8:19–32. [Google Scholar]
- 36.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 37.Klovdahl AS, Potterat JJ, Woodhouse DE, Muth JB, Muth SQ, Darrow WW. Social networks and infectious disease: the Colorado Springs Study. Social Science & Medicine. 1994;38(1):79–88. doi: 10.1016/0277-9536(94)90302-6. [DOI] [PubMed] [Google Scholar]
- 38.Latkin C, Mandell W, Oziemkowska M, Vlahov D, Celentano D. THE RELATIONSHIPS BETWEEN SEXUAL-BEHAVIOR, ALCOHOL-USE, AND PERSONAL NETWORK CHARACTERISTICS AMONG INJECTING DRUG-USERS IN BALTIMORE, MARYLAND. Sexually Transmitted Diseases. 1994;21(3):161–7. doi: 10.1097/00007435-199405000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Johnston D, Stall R, Smith K. RELIANCE BY GAY MEN AND INTRAVENOUS-DRUG-USERS ON FRIENDS AND FAMILY FOR AIDS-RELATED CARE. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv. 1995;7(3):307–19. doi: 10.1080/09540129550126533. [DOI] [PubMed] [Google Scholar]
- 40.Latkin C, Mandell W, Oziemkowska M, Celentano D, Vlahov D, Ensminger M, et al. Using social network analysis to study patterns of drug use among urban drug users at high risk for HIV/AIDS. Drug Alcohol Depend. 1995;38(1):1–9. doi: 10.1016/0376-8716(94)01082-v. [DOI] [PubMed] [Google Scholar]
- 41.Neaigus A, Friedman SR, Jose B, Goldstein MF, Curtis R, Ildefonso G, et al. High-risk personal networks and syringe sharing as risk factors for HIV infection among new drug injectors. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1996;11(5):499–509. doi: 10.1097/00042560-199604150-00011. [DOI] [PubMed] [Google Scholar]
- 42.Hoffmann JP, Su SS, Pach A. Changes in network characteristics and HIV risk behavior among injection drug users. Drug Alcohol Depend. 1997;46(1–2):41–51. doi: 10.1016/s0376-8716(97)00038-0. [DOI] [PubMed] [Google Scholar]
- 43.Broadhead R, Heckathorn D, Weakliem D, Anthony D, Madray H, Mills R, et al. Harnessing Peer Networks as an Instrument for AIDS Prevention: Results from a Peer-Driven Intervention. Public Health Reports. 1998;113(Supplement 1):42–57. [PMC free article] [PubMed] [Google Scholar]
- 44.Heckathorn D, Broadhead R, Anthony D, Weakliem D. AIDS and Social Networks: HIV Prevention through Network Mobilization. Sociological Focus. 1998;32:159–79. [Google Scholar]
- 45.Ennett ST, Bailey SL, Federman EB. Social network characteristics associated with risky behaviors among runaway and homeless youth. J Health Soc Behav. 1999;40(1):63–78. [PubMed] [Google Scholar]
- 46.Servegev B, Oparina T, Rumyantseva TP, Volkanevskii VL, Broadhead RS, Heckathorn DD, et al. HIV prevention in Yaroslavl, Russia: A peer-driven intervention and needle exchange. Journal of Drug Issues. 1999;29(4):777–804. [Google Scholar]
- 47.Bell DC, Montoya ID, Atkinson JS. Partner concordance in reports of joint risk behaviors. Journal of Acquired Immune Deficiency Syndromes. 2000;25(2):173–81. doi: 10.1097/00042560-200010010-00012. [DOI] [PubMed] [Google Scholar]
- 48.Bell DC, Montoya ID, Atkinson JS, Yang S-J. Social networks and forecasting the spread of HIV infection. J Acquir Immune Defic Syndr. 2002;31(2):218–29. doi: 10.1097/00126334-200210010-00013. [DOI] [PubMed] [Google Scholar]
- 49.Broadhead RS, Heckathorn DD, Altice FL, van Hulst Y, Carbone M, Friedland GH, et al. Increasing drug users’ adherence to HIV treatment: results of a peer-driven intervention feasibility study. Soc Sci Med. 2002;55(2):235–46. doi: 10.1016/s0277-9536(01)00167-8. [DOI] [PubMed] [Google Scholar]
- 50.Friedman SR, Kang SY, Deren S, Robles R, Colon HM, Andia J, et al. Drug-scene roles and HIV risk among Puerto Rican injection drug users in East Harlem, New York and Bayamon, Puerto Rico. J Psychoactive Drugs. 2002;34(4):363–9. doi: 10.1080/02791072.2002.10399977. [DOI] [PubMed] [Google Scholar]
- 51.Kottiri BJ, Friedman SR, Neaigus A, Curtis R, Des Jarlais DC. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. Journal of Acquired Immune Deficiency Syndromes. 2002;30(1):95–104. doi: 10.1097/00042560-200205010-00013. [DOI] [PubMed] [Google Scholar]
- 52.Bell DC, Mosier V, Atkinson JS. Protecting oneself from human immunodeficiency virus: Are prevention messages being heard? Clinical Infectious Diseases. 2003;37:S433–S8. doi: 10.1086/377544. [DOI] [PubMed] [Google Scholar]
- 53.Latkin CA, Hua W, Forman VL. The relationship between social network characteristics and exchanging sex for drugs or money among drug users in Baltimore, MD, USA. Int J STD AIDS. 2003;14(11):770–5. doi: 10.1258/09564620360719831. [DOI] [PubMed] [Google Scholar]
- 54.Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychology. 2003;22(4):332–9. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- 55.Knowlton A, Hua W, Latkin C. Social support among HIV positive injection drug users: implications to integrated intervention for HIV positives. Aids Behav. 2004;8(4):357–63. doi: 10.1007/s10461-004-7320-7. [DOI] [PubMed] [Google Scholar]
- 56.Kang SY, Deren S, Andia J, Colon HM, Robles R. Egocentric HIV risk networks among Puerto Rican crack users in New York and in Puerto Rico: Impact on sex risk behaviors over time. Aids Education and Prevention. 2005;17(1):53–67. doi: 10.1521/aeap.17.1.53.58684. [DOI] [PubMed] [Google Scholar]
- 57.Knowlton AR, Hua W, Latkin C. Social support networks and medical service use among HIV-positive injection drug users: implications to intervention. AIDS Care. 2005;17(4):479–92. doi: 10.1080/0954012051233131314349. [DOI] [PubMed] [Google Scholar]
- 58.Broadhead RS, Volkanevsky VL, Rydanova T, Ryabkova M, Borch C, van Hulst Y, et al. Peer-driven HIV interventions for drug injectors in Russia: First year impact results of a field experiment. International Journal of Drug Policy. 2006;17(5):379–92. [Google Scholar]
- 59.Neaigus A, Gyarmathy VA, Miller M, Frajzyngier VM, Friedman SR, Des Jarlais DC. Transitions to injecting drug use among noninjecting heroin users: social network influence and individual susceptibility. J Acquir Immune Defic Syndr. 2006;41(4):493–503. doi: 10.1097/01.qai.0000186391.49205.3b. [DOI] [PubMed] [Google Scholar]
- 60.Friedman SR, Mateu-Gelabert P, Curtis R, Maslow C, Bolyard M, Sandoval M, et al. Social capital or networks, negotiations, and norms? A neighborhood case study. American Journal of Preventive Medicine. 2007;32(6 Suppl):S160–70. doi: 10.1016/j.amepre.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Miller M, Korves CT, Fernandez T. The social epidemiology of HIV transmission among African American women who use drugs and their social network members. AIDS Care. 2007;19(7):858–65. doi: 10.1080/09540120701191540. [DOI] [PubMed] [Google Scholar]
- 62.Needle R, Kroeger K, Belani H, Achrekar A, Parry CD, Dewing S. Sex, drugs, and HIV: Rapid assessment of HIV risk behaviors among street-based drug using sex workers in Durban, South Africa. Social Science & Medicine. 2008;67(9):1447–55. doi: 10.1016/j.socscimed.2008.06.031. [DOI] [PubMed] [Google Scholar]
- 63.Tobin KE, Latkin CA. An examination of social network characteristics of men who have sex with men who use drugs. Sexually Transmitted Infections. 2008;84(6):420–4. doi: 10.1136/sti.2008.031591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tyler KA. Social network characteristics and risky sexual and drug related behaviors among homeless young adults. Social Science Research. 2008;37(2):673–85. doi: 10.1016/j.ssresearch.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 65.Abramovitz DV, EM, Strathdee SA, Patterson TL, Vera A, Frost SDW, Proyecto ElCuete. Using Respondent-Driven Sampling in a Hidden Population at Risk of HIV Infection: Who Do HIV-Positive Recruiters Recruit? Sexually Transmitted Diseases. 2009;36(12):750–6. doi: 10.1097/OLQ.0b013e3181b0f311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Booth RE, Lehman WEK, Latkin CA, Brewster JT, Sinitsyna L, Dvoryak S. USE OF A PEER LEADER INTERVENTION MODEL TO REDUCE NEEDLE-RELATED RISK BEHAVIORS AMONG DRUG INJECTORS IN UKRAINE. Journal of Drug Issues. 2009;39(3):607–25. [Google Scholar]
- 67.Deering KN, Shannon K, Sinclair H, Parsad D, Gilbert E, Tyndall MW. Piloting a peer-driven intervention model to increase access and adherence to antiretroviral therapy and HIV care among street-entrenched HIV-positive women in Vancouver. AIDS Patient Care and STDs. 2009;23(8):603–9. doi: 10.1089/apc.2009.0022. [DOI] [PubMed] [Google Scholar]
- 68.Sherman SG, Sutcliffe C, Srirojn B, Latkin CA, Aramratanna A, Celentano DD. Evaluation of a peer network intervention trial among young methamphetamine users in Chiang Mai, Thailand. Social Science & Medicine. 2009;68(1):69–79. doi: 10.1016/j.socscimed.2008.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Youm YM-A, Ellen Mary, Williams Chyvette T, Ouellet Lawrence J. Identifying hidden sexual bridging communities in Chicago. J Urban Health. 2009;86(Suppl 1):107–20. doi: 10.1007/s11524-009-9371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hahn JA, Evans JL, Davidson PJ, Lum PJ, Page K. Hepatitis C virus risk behaviors within the partnerships of young injecting drug users. Addiction. 2010;105(7):1254–64. doi: 10.1111/j.1360-0443.2010.02949.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Latkin CY, Cui, Tobin Karin, Hulbert Alicia. Factors associated with recruiting an HIV seropositive risk network member among injection drug users. Aids Behav. 2010;14(5):1137–41. doi: 10.1007/s10461-010-9676-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tyler K, Melander L. The effect of drug and sexual risk behaviours with social network and non-network members on homeless youths’ sexually transmissible infections and HIV testing. Sexual Health. 2010;7(4):434–40. doi: 10.1071/SH09113. [DOI] [PubMed] [Google Scholar]
- 73.Booth RE, Lehman WEK, Latkin CA, Dvoryak S, Brewster JT, Royer MS, et al. Individual and network interventions with injection drug users in 5 Ukraine cities. American Journal of Public Health. 2011;101(2):336–43. doi: 10.2105/AJPH.2009.172304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Davey-Rothwell MA, Chander G, Hester L, Latkin CA. Social network characteristics and heavy episodic drinking among women at risk for HIV/sexually transmitted infections. J Stud Alcohol. 2011;72(6):1041–7. doi: 10.15288/jsad.2011.72.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gyarmathy VAL, Nan, Tobin Karin E, Hoffman Irving F, Sokolov Nikolai, Levchenko Julia, Batluk Julia, Kozlov Andrei A, Kozlov Andrei P, Latkin Carl A. Unprotected sex in heterosexual partnerships of injecting drug users in st. Petersburg, Russia. Aids Behav. 2011;15(1):58–64. doi: 10.1007/s10461-010-9721-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Latkin CY, Cui, Srikrishnan Aylur K, Solomon Suniti, Mehta Shruti H, Celentano David D, Kumar Muniratnam Suresh, Knowlton Amy, Solomon Sunil Suhas. The relationship between social network factors, HIV, and Hepatitis C among injection drug users in Chennai, India. Drug Alcohol Depend. 2011;117(1):50–4. doi: 10.1016/j.drugalcdep.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Li J, Liu H, Li J, Luo J, Koram N, Detels R. Sexual transmissibility of HIV among opiate users with concurrent sexual partnerships: an egocentric network study in Yunnan, China. Addiction. 2011;106(10):1780–7. doi: 10.1111/j.1360-0443.2011.03459.x. discussion 1788–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li J, Weeks MR, Borgatti SP, Clair S, Dickson-Gomez J. A social network approach to demonstrate the diffusion and change process of intervention from peer health advocates to the drug using community. Subst Use Misuse. 2012 Apr;47(5):474–490. doi: 10.3109/10826084.2012.644097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Richardson L, Grund T. Modeling the impact of supra-structural network nodes: The case of anonymous syringe sharing and HIV among people who inject drugs. Social Science Research. 2012;41(3):624–36. doi: 10.1016/j.ssresearch.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 80.Smyrnov P, Broadhead RS, Datsenko O, Matiyash O. Rejuvenating harm reduction projects for injection drug users: Ukraine’s nationwide introduction of peer-driven interventions. International Journal of Drug Policy. 2012;23(2):141–7. doi: 10.1016/j.drugpo.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 81.Adams J, Moody J, Morris M. Sex, Drugs, and Race: How Behaviors Differentially Contribute to the Sexually Transmitted Infection Risk Network Structure. American Journal of Public Health. 2013;103(2):322–9. doi: 10.2105/AJPH.2012.300908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brown RA, Kennedy DP, Tucker JS, Golinelli D, Wenzel SL. Monogamy on the Street A Mixed Methods Study of Homeless Men. Journal of Mixed Methods Research. 2013;7(4):328–46. doi: 10.1177/1558689813480000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Eritsyan K, Heimer R, Barbour R, Odinokova V, White E, Rusakova MM, et al. Individual-level, network-level and city-level factors associated with HIV prevalence among people who inject drugs in eight Russian cities: a cross-sectional study. Bmj Open. 2013;3(6) doi: 10.1136/bmjopen-2013-002645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Green HD, Jr, de la Haye K, Tucker JS, Golinelli D. Shared risk: who engages in substance use with American homeless youth? Addiction. 2013;108(9):1618–24. doi: 10.1111/add.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Guo W, Bao SL, Lin W, Wu GH, Zhang W, Hladik W, et al. Estimating the Size of HIV Key Affected Populations in Chongqing, China, Using the Network Scale-Up Method. PLoS ONE. 2013;8(8) doi: 10.1371/journal.pone.0071796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Latkin C, Davey-Rothwell M, Yang J-y, Crawford N. The relationship between drug user stigma and depression among inner-city drug users in Baltimore, MD. J Urban Health. 2013;90(1):147–56. doi: 10.1007/s11524-012-9753-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Latkin C, Donnell D, Liu T-Y, Davey-Rothwell M, Celentano D, Metzger D. The dynamic relationship between social norms and behaviors: the results of an HIV prevention network intervention for injection drug users. Addiction. 2013;108(5):934–43. doi: 10.1111/add.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.White K, Rudolph AE, Jones KC, Latkin C, Benjamin EO, Crawford ND, et al. Social and individual risk determinants of HIV testing practices among noninjection drug users at high risk for HIV/AIDS. AIDS Care. 2013;25(2):230–8. doi: 10.1080/09540121.2012.701269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Williams C, Eisenberg M, Becher J, Davis-Vogel A, Fiore D, Metzger D. Racial Disparities in HIV Prevalence and Risk Behaviors Among Injection Drug Users and Members of Their Risk Networks. Jaids-Journal of Acquired Immune Deficiency Syndromes. 2013;63:S90–S4. doi: 10.1097/QAI.0b013e3182921506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.World Bank. 2015 [Available from: http://data.worldbank.org/about/country-and-lending-groups - Low_income.
- 91.Broadhead RS, Heckathorn DD, Weakliem DL, Anthony DL, Madray H, Mills RJ, et al. Harnessing peer networks as an instrument for AIDS prevention: results from a peer-driven intervention. Public health reports. 1998;113(Suppl 1):42–57. [PMC free article] [PubMed] [Google Scholar]
- 92.Latkin CA, Davey-Rothwell MA, Knowlton AR, Alexander KA, Williams CT, Boodram B. Social network approaches to recruitment, HIV prevention, medical care, and medication adherence. Journal of acquired immune deficiency syndromes. 2013;63(Suppl 1):S54–8. doi: 10.1097/QAI.0b013e3182928e2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.De Cock KM, Crowley SP, Lo YR, Granich RM, Williams BG. Preventing HIV transmission with antiretrovirals. Bull World Health Organ. 2009;87(7):488–488A. doi: 10.2471/BLT.09.067330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 95.Montaner JS. Treatment as prevention: toward an AIDS-free generation. Topics in antiviral medicine. 2013;21(3):110–4. [PMC free article] [PubMed] [Google Scholar]
- 96.Broadhead RS, Borch C, Hulst YV, Gauchat G, Tehrani S, Stringer KL, et al. Relying on injection drug users to access and adhere to HIV therapeutics: Bittersweet lessons using respondent-driven sampling and a peer-driven intervention. J Drug Issues. 2012;42(2):127–46. [Google Scholar]
- 97.Wang K, Brown K, Shen SY, Tucker J. Social network-based interventions to promote condom use: a systematic review. AIDS and Behavior. 2011;15(7):1298–308. doi: 10.1007/s10461-011-0020-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Simmons N, Donnell D, Ou SS, Celentano DD, Aramrattana A, Davis-Vogel A, et al. Assessment of Contamination and Misclassification Biases in a Randomized Controlled Trial of a Social Network Peer Education Intervention to Reduce HIV risk Behaviors Among Drug Users and Risk Partners in Philadelphia, PA and Chiang Mai, Thailand. AIDS and Behavior. 2015;19(10):1818–27. doi: 10.1007/s10461-015-1073-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Anderson S, Allen P, Peckham S, Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst. 2008;6:7. doi: 10.1186/1478-4505-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]