Introduction
Spina bifida (SB) is a neurological disorder caused by defective closure of the neural tube during the first four weeks of gestation resulting in varying degrees of paralysis and impairment of bladder or bowel function. The incidence of SB is decreasing due to preventative measures, including routine preconception folic acid supplementation and antenatal detection with the option of termination, yet the Canadian Community Health Survey data 2010–2011 showed a prevalence of approximately 1500 individuals in Ontario.1 Less than a half-century ago, many of these children were unlikely to survive the nursery and now the majority of SB patients will survive into adulthood, most having undergone multiple neurological, orthopedic, and urological surgeries.2,3
Given the spectrum of medical, surgical, developmental, and social problems associated with SB, there is a need for long-term, comprehensive care strategies. The greatest long-term risks to SB patients are urologic complications. The majority require intermittent catheterization, exposing them to risks of infection and bladder stone formation. Patients who have undergone bladder augmentation have an 8% risk of rupture, an often lethal complication, and a markedly increased risk of bladder cancer.2 Other ongoing risks include: latex allergy, electrolyte abnormalities, B-12 deficiency, and renal deterioration. Up to 94% of SB patients have at least one chronic medical condition, emphasizing the need for continuing medical care past childhood. Finally, SB patients experience marked social and developmental impairments.4
In Ontario, pediatric care of SB patients is in the four tertiary pediatric hospitals. Interprofessional teams of physicians, social workers, physical and occupational therapists, psychologists, and nurses care for patients until they reach 18 years of age, when they are discharged to independently manage their care. Some may be referred to an adult urologist; however, the majority do not seek care until a complication arises. Furthermore, two-thirds of SB patients do not seek routine followup as young adults, despite an obvious need for ongoing comprehensive care to mitigate significant risks to their health.5
In major U.S. centres, the concept of establishing regional “transitional” SB clinics for this adolescent and young adult (AYA) population has been suggested.5 Major barriers exist to establishing such programs for SB in Ontario, including funding models for physicians and hospitals. There is a disconnect of physician funding in the province, with pediatric specialists reimbursed on fixed alternative funding plans (AFP) and adult practitioners on a fee-for-service (FFS) basis. Without a hybridized reimbursement system, there is not crossover of care by physicians from the pediatric to adult system, and vice versa. In addition, there is a lack of desire on the patients’ and pediatric providers’ sides to separate long-term care to a new model in the adult arena. This is exacerbated by a lack of expertise and interest to care for these patients by adult providers.5
According to Ouyang et al, there are currently insufficient health services for age-appropriate care to meet the realistic demands for chronic care of patients with SB.2 Novel, patient-centred approaches are necessary to address their complex needs, specifically urological and social, within the constraints of the current healthcare system.
The intervention
The Institute for Healthcare Improvement (IHI) recognizes that increased longevity associated with chronic health problems creates new stresses on medical and social services. As described, in Ontario we are failing to provide any structured system to appropriately care for AYA SB patients. This greatly compromises their health by providing only reactionary, costly acute-care. We seek to develop a cost-effective model to provide integrated and comprehensive, province-wide care. This model of care will allow patients to remain in their community through greater involvement of their local most responsible physician (MRPs).
It is imperative that a change in current practice for the transitioning SB patient occur. Such a change needs to focus on system integration, redesign of primary care and focus on individuals and families.6 By including the following key components, a novel transition program can improve the patient’s experience and the health of the SB population:
Education for community-based providers on the care of SB patients with continued advancement of knowledge as new care strategies evolve.
Creation of a reliable care pathway based on evidence-based practice, expert opinion, and best practice guidelines.
Assure ongoing system-generated databases, decision support, and communication between pediatric SB clinics, MRPs, community urologists, and adult centres.
Empowerment of the maturing patient to become knowledgeable and responsible in managing their lifelong health challenges independently.
Coordination and integration among the four pediatric SB centres in Ontario to better support adult centres in managing the transition of SB patient care.
Each adult patient with SB has unique needs. We propose the development of a SB treatment network (SBTN). The goal of this network is to provide patients with comprehensive medical care, as well as psychosocial and self-management support, including community resources and health information. Treatment plans will be individualized, with a goal to enable self-management and to reduce the risks of developing SB-related complications.
Implementation of the SBTN will require significant system changes and, unlike current models, this integrated collaborative network will focus on transitions and not transfer of care. It will be innovative in the use of technology to create the platform for a lifelong support system, which has been identified as a critical factor in successful transition from pediatric to adult care.7,8
We will develop this network in collaboration with Ontario’s four major pediatric tertiary centres, the Spina Bifida and Hydrocephalus Association of Ontario, and adult urologists. Pediatric providers will identify patients for the network and care will be coordinated by adult nurse practitioners (NPs) with expertise in the care of congenital diseases. As well as treatment of comorbidities, and complications, AYA SB patients will receive age-appropriate psychosocial support from peers, teachers, and healthcare clinicians. The care provided will be as virtual as possible; however, to provide continuity, the patient will be referred to the nearest SBTN adult urologist.
The SBTN will be supported by an electronic health record (EHR) containing the patient’s comprehensive medical history and a modifiable ongoing care plan. The care plan is a living document developed in partnership with the patient and is inclusive of the patient’s self-management goals. An annual review is performed in collaboration with the care coordinator in-person or virtually (i.e., Skype, FaceTime). The EHR will be maintained with up-to-date guidelines and clinical decision-making support tools. The NP/care coordinator will ensure that arrangements are made for any required investigations or preventive health measures. At any point if the patient or a provider caring for a network patient requires assistance, they will be able to access the network through the on-call NP.
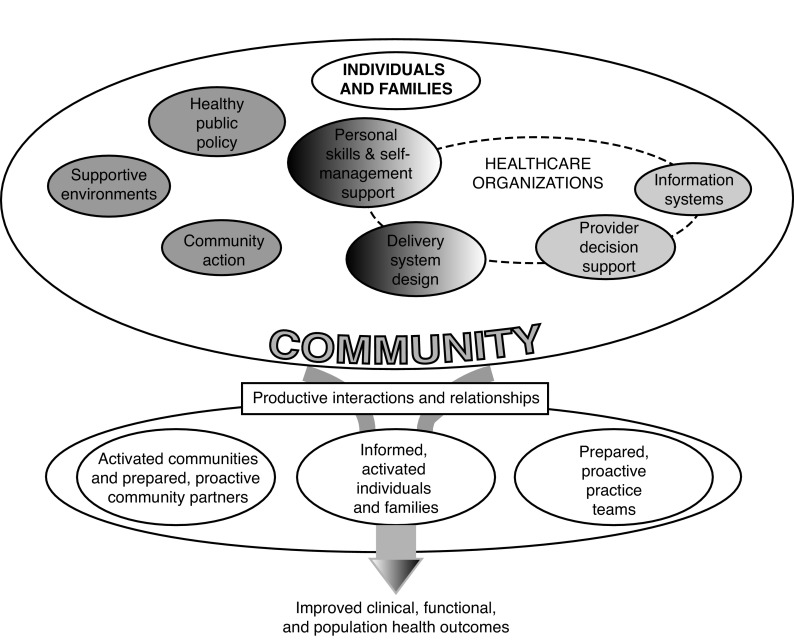
The network will adopt the Ontario Ministry of Health and Long-Term Care (MOHLTC) evidence-based, population-based, and client-centred framework for chronic disease prevention and management (CDPM) framework that includes key elements of system changes found to improve the delivery of chronic care: personal skills and self-management support, delivery system design, provider decision support, and information systems, all elements of which will be interconnected and interdependent (Fig. 1).9
Fig. 1.
Ontario’s chronic disease prevention and management framework delivery system design.
The key to the SBTN will be the NP care coordinator supporting both the pediatric clinics and the virtual network. The NP, our key asset for this initiative with their expanded scope of practice, will provide the link on an ongoing basis from the pediatric SB patient into adulthood. They are the key person in each centre that will be able to assess, treat when possible, and most importantly triage when there are urgent issues that have arisen. They would hold the role of the integrator within the collaborative and through their role in the SB clinics, develop a provider relationship with the AYA patients and be responsible for assessing readiness for transition (Alriksson-Schmidt et al, 2010) in collaboration with the patient, family, and team.10 Each patient will require an individualized transition plan.7,8,11 The development of this network will also require a change in focus within the pediatric centres to consider transition planning beginning in early adolescence instead of the age of 18. The other crucial component of system design is the network of adult urologists, primary care providers, and other health professionals throughout Ontario. Team members will collaborate to develop an agreed-upon step-by-step process at all four SB tertiary centres to develop a standardized plan for transition, but will be individualized for each patient, with early introduction to the adult providers prior to any transition occurring. Importantly, standardized communication between adult and pediatric providers will assure documentation of the scope of each surgical procedure that was performed while in the pediatric centre is received by the adult provider. This implementation plan will enable necessary overlap with providers, team members, and patients, in order to allow for a seamless transition. This will require changes in physician compensation that allows this flexibility in timing of transition and need for joint visits with pediatric and adult urologists, in particular those who have complicated needs.11,12
Personal skills and self-management support (SMS)
The self-management component of the SBTN will empower individuals with SB to adopt healthy self-care behaviours. AYA with SB are less physically active compared to the general population and are three times more likely to be overweight.13,14 Moreover, SB patients experience substance abuse and have higher rates of depression than the general population.13,15 The SMS will include counselling services and peer-support linked with the Spina Bifida and Hydrocephalus Association of Ontario to enable strategies for wellness management. SMS users can link to health and social resources in the community to help find housing, employment, and encourage physical and social activity. The SMS also enables AYA learn the warning signs and symptoms of deteriorating physical and mental health to independently and proactively seek medical and professional help.
Information systems
A comprehensive information system (IS) includes the EHR, a patient portal, and registry for SB transition patients. The EHR will link the primary care teams with the NP and specialist providers within the networks so that information on the patient’s health status, tests results, prescriptions, and prevention and treatment plans are shared in real time across the primary care level and the specialist. The patient portal system will offer 24/7 access and give patients the opportunity to be fully informed and play an active role in decisions regarding their health. Key components of the portal will include interactive education resources, links to relevant community services, appointment reminders, and full access to their EHR. The registry will serve as a means to continually gather population-based data on SB transition patients and share clinical and process outcomes that offer opportunities for multisite research. Such EHRs are costly and difficult to implement. In the current climate of e-health innovation in the province, this would be an extraordinary effort, but is ultimately necessary to provide appropriate, timely, and cost-effective care to SB patients.
Provider decision support
An identified limitation in current AYA SB care is a lack of interested adult-centred care providers.12 The SBTN would allow for networking and cooperative care models between health professionals and provide educational support and resources needed to make clinical decisions. This form of teamwork is innovative, as it would be virtual, but conducted through the shared platform of the EHR. In addition, the EHR could have built-in evidence-based decision support for standards of care, which could increase comfort of the primary care physician in the community to take on these patients within their practice.
Which of these changes might be feasible within the current patterns of health delivery and health policy in Ontario?
Ontario is advocating for a systems- and population-level approach to redefine health services provision that includes many of the factors we propose in the SBTN (www.publichealthontario.ca); this approach would empower the AYA SB population to play a greater role in managing their health, to become an integral part of the care team by incorporating self-management, embracing both the interdisciplinary care team to ensure the right care by the right provider and the supports that are proactive and coordinated to navigate the system.
A framework where the transition from pediatric to adult SB providers is formally integrated will reduce stressors for patients and the system. The key to this will be to establish formal links with adult centres that have the specialist capacity to manage the AYA or adult SB patient. Currently, this occurs only infrequently and with limited success, given the realities of hospital funding. Transition is often difficult; this population is no exception, given issues of compliance and dependence.16 Key areas to address will be identifying team members, ensuring consensus on the care plan, preparing for transition between providers, clear communication between patient and provider, appreciation of the patient’s goals, and knowledge of when the transition will occur will assist with a seamless process. The provider collaborative component of the network is vital to ensuring viable support to primary care physicians with easy linkages to specialists and resources. Presently, these relationships are limited, as communication between providers is rarely ongoing and often “after-the-fact,” with communication being predominantly by consultation and procedure notes. Providing reliable on-demand access to community-based expertise and care when it is required will reduce the need for hospitalization or readmissions.
Support from the Local Integrated Health Networks (LHIN) would be beneficial as a jumping-off point, together with a group of pediatric and adult urologists, interested NPs, and primary care partners. Our premise is that this intervention bundle will provide lifelong support and focus on prevention and proactive management of complications. Through its evidence-based framework, the expectation is that the SBTN will improve care, population health, and reduce costs in the long-term.
What changes do we recommend to realize achievable goals in the short-term (1–3 years) and in the longer-term?
A SB client’s mother we interviewed stated: “I strongly feel that Bonnie (age 26) would not be alive today without my participation and advocacy. If she had not had a parent working in healthcare and knowing how to navigate the healthcare system, she would have died years ago.” (Visit online version of this article at www.cuaj.ca for full interview notes [Appendix A].)
To be successful, the SBTN would need strong local and provincial leadership to drive change in the system, in addition to support through the LHIN mandate to lead care integration.17 The first step in developing innovative care for these patients is to identify leaders to provide the linkage that will begin collaborative work between organizations, physicians, NPs, and other providers within communities. Next, financial and human resources will be required to launch this idea. Current reimbursement structures need to be realigned to encourage overlap of care between physicians in the pediatric and adult realms. Bundled payments based on this population’s needs would provide better flexibility. Furthermore, we will need to see a shift from performance measures related to productivity and acute indicators for this to be a patient-centred innovation. Our approach is about how and when the care is delivered, not what care is delivered as we determine outcomes. By including the SB patients and their families’ voices we will define quality from their perspective.
Technology will be a great enabler to this project, but also a significant obstacle, with limited funding. We will need to investigate other patient portals to understand the success of these and incorporate their learning and feedback. The technology may be the last piece as we gather stakeholders, SB patients, and families to understand the needs and identify what is required to encourage independence. In the meantime, strong links with community partners could provide the local expertise, information, time, and resources to further the momentum. As referrals are made, programs and services will be identified.18
In the long-term, we will:
Continue to collaborate with all stakeholders to enhance the SBTN and improve the lives of those living with SB.
Continue to pursue care delivery and funding policy redesigns that will continually improve the care transitions for this population.
Continue to ask “why are we doing this?” and apply the triple aim: experience, health outcomes, cost.
Ensure we are developing systems and supports that are patient-centred, while remaining cost-conscious and incorporate feedback as we identify new learnings.
Contribute positively to the health, quality, and patient experience of the SB population through careful planning, monitoring, and adaptation along the way
Conclusion
The evidence has shown effective practices for improving transitions from pediatric to adult SB, but the challenge is to coordinate the effort among various healthcare providers. This would be a new culture of care in Ontario, ensuring lifelong followup. It requires strong leadership and engagement of a significant number of stakeholders. Clear accountability between providers as they share in the patient care during transitions will be imperative. Moving Ontario’s healthcare forward will entail embracing innovative technologies, which in and of themselves will pose challenges of privacy and security. Nonetheless, the use of technology would facilitate outcome measurement, speed processes, ease work burdens, and improve sharing of useful information and protocols for this population. It is important to move from acute care activities and build community support for social housing, mental and addiction health services, and vocations as part of our system. An open-minded dialogue among members of an interdisciplinary team is the beginning. This plan will need government support, coordination of services, and system redesign to facilitate patient navigation. By transforming the delivery of healthcare services and creating greater innovation and flexibility within the system, we can create synergies by sharing knowledge development, best practices, and engage patients as partners in care. Ultimately, once well-established, the network could expand to include other urological diseases with common medical care and lifelong management needs and, therefore, reap efficiency gains.
Acknowledgments
This paper was completed as part of the requirements for the MSc (Quality Improvement and Patient Safety) program through the Institute of Health Policy, Management and Evaluation at the University of Toronto (Class of 2015). The authors acknowledge the support of their colleagues and mentors in IHPME.
Footnotes
Competing interests: Dr. Hillis is an Advisory Board member for Bristol-Myers Squibb and Novartis Oncology; has received research grants and speaker fees from Amgen, Bristol-Myers Squibb, Celgene, Lundbeck, Novartis Oncology, and Sanofi; and has participated in clinical trials for Bristol-Myers Squibb and Novartis Oncology. Ms. Oldershaw was part of a Baxter Advisory Board for Spectrum Infusion pumps, for which she received an honorarium plus travel and accommodation. The remaining authors report no competing personal or financial interests.
This paper has been peer-reviewed.
References
- 1.Government of Canada Publications Your community, your health. 2013. Available at http://www.publications.gc.ca/pub?id=9.505018&sl=0. Accessed August 30, 2016.
- 2.Ouyang L, Grosse SD, Armour BS, et al. Health care expenditures of children and adults with spina bifida in a privately insured U.S. population. Birth Defects Res A Clin Mol Teratol. 2007;79:552–8. doi: 10.1002/bdra.20360. [DOI] [PubMed] [Google Scholar]
- 3.Bol KA, Collins JS, Kirby RS. Survival of infants with neural tube defects in the presence of folic acid fortification. Pediatrics. 2006;117:803–13. doi: 10.1542/peds.2005-1364. [DOI] [PubMed] [Google Scholar]
- 4.Hunt GM. Open spina bifida: outcome for complete cohort treated unselectively and followed into adulthood. Dev Med Child Neurol. 1990;32:108–18. doi: 10.1111/j.1469-8749.1990.tb16910.x. [DOI] [PubMed] [Google Scholar]
- 5.Summers SJ, Elliott SM, Oottamasthathien S, et al. Urologic problems in spina bifida patients transitioning to adult care. Urology. 2014;84:440–4. doi: 10.1016/j.urology.2014.03.041. [DOI] [PubMed] [Google Scholar]
- 6.Berwick DM, Nolan TW, Whittington J. The triple aim: Care, health, and cost. Health Affairs. 2008;273:759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 7.Shalaby MS, Gibson A, Granitsiotis P, et al. Assessment of the introduction of an adolescent transition urology clinic using a validated questionnaire. J Pediatr Urol. 2015;11:89.e1–5. doi: 10.1016/j.jpurol.2014.11.024. [DOI] [PubMed] [Google Scholar]
- 8.Timberlake MD, Corbett ST, Costabile RA, et al. Identification of adolescent and adult patients receiving pediatric urologic care and establishment of a dedicated transition clinic. J Pediatr Urol. 2015;11:62.e1–6. doi: 10.1016/j.jpurol.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Ministry of Health and Long-Term Care Preventing and managing chronic disease: Ontario’s framework. May, 2007. Available at http://www.health.gov.on.ca/en/pro/programs/cdpm/pdf/framework_full.pdf. Accessed August 30, 2016.
- 10.Alriksson-Schmidt A, Adams E, Bellin M, et al. Spina Bifida: Health and Development Across the Life Course. Philadelphia: WB Saunders; 2010. [Google Scholar]
- 11.Hepburn CM, Cohen E, Bhawra J, et al. Health system strategies supporting transition to adult care. Arch Dis Child. 2015;100:559–64. doi: 10.1136/archdischild-2014-307320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Binks JA, Barden WS, Burke TA, et al. What do we really know about the transition to adult-centred healthcare? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88:1064–73. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 13.Soe MM, Swanson ME, Bolen JC, et al. Health risk behaviors among young adults with spina bifida. Dev Med Child Neurol. 2012;54:1057–64. doi: 10.1111/j.1469-8749.2012.04402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McPherson AC, Leo J, Church P, et al. An environmental scan of weight assessment and management practices in pediatric spina bifida clinics across Canada. J Pediatr Rehabil Med. 2014;7:207–17. doi: 10.3233/PRM-140290. [DOI] [PubMed] [Google Scholar]
- 15.Stubberud J, Langenbahn D, Levine B, et al. Emotional health and coping in spina bifida after goal management training: A randomized controlled trial. Rehabil Psychol. 2015;60:1–16. doi: 10.1037/rep0000018. [DOI] [PubMed] [Google Scholar]
- 16.Young L. Apr 18, 2015. Personal communication.
- 17.Government of Ontario 2006. Local Health System Integration Act, 2006, S.O. 2006, Chapter 4, Part V: Integration and Devolution. Available at https://www.ontario.ca/laws/statute/06l04?search=local+health+integration+networks#BK27. Accessed September 19, 2016.
- 18.Registered Nurses Association of Ontario RNAO’s Enhancing Community Care for Ontarians (ECCO) - A three-year plan (White Paper) 2012. Available at http://rnao.ca/policy/submissions/rnao-enhancing-community-care-ontarians-ecco-three-plan-white-paper. Accessed August 30, 2016.