The content is available as a PDF (2.9 MB).
Appendices
Appendix 1. Ontario Health Insurance Plan (OHIP) physician billing claims used to identify prostate cancer-related management
| Billing claims - code | Fee code: OHIP definition |
|---|---|
| Androgen-deprivation therapy | G342: implantation of hormone pellets |
| Orchiectomy | S589: orchiectomy; S598: radical orchiectomy |
| Biopsy | Z712: biopsy, needle; Z713 biopsy, needle with drainage of abcess; S644: biopsy, perineal; E780: cystoscopy with needle biopsy of prostate |
| Transurethral resection of the prostate | S654: transurethral resection of prostate for residual tissue; S655:transurethral resection of prostate |
| Radical prostatectomy | S645:perineal prostatectomy; S646:perineal prostatectomy with vesiculectomy; S651: radical retropubic prostatectomy; S653:laparoscopic radical prostatectomy; |
| Pelvic lymph node dissection | S652:staging pelvic lymph node dissection for prostate cancer |
| Brachytherapy | S640: stereotactic prostate brachytherapy; X322: radium (sealed sources) treatment planning dosage; X323:radium (sealed sources) Intracavit. applic. - 1st applic.; X324: radium (sealed sources) - Interstitial; X325: radium (sealed sources) Applic. plaque/mould; X334: radium (sealed sources) Intracavit. applic. - rep. applic. |
| Radiotherapy | X310: simple treatment planning; X311: intermediate treatment planning; X312: complex treatment planning; X313: full 3D treatment preparation |
| Urologist visits | A355: consultation; A935: special surgical consultation; A356: repeat consultation; A353: specific assessment; A354: partial assessment; C355: in-patient consultation; C935: in-patient special surgical consultation; C356: in-patient repeat consultation; C353: in-patient specific assessment; C354: in-patient partial assessment; C352: in-patient subsequent visits – first five weeks; C357: in-patient subsequent visits – sixth to thirteenth week; C359: in-patient subsequent visit – after thirteenth week |
| Radio-oncologist visits | A340: medical specific re-assessment; A341: complex medical specific re-assessment; A343:medical specific assessment; A345: consultation; A346: repeat consultation; A348: partial assessment; A745: limited consultation; C340: in-patient medical specific re-assessment; C341: in-patient complex medical specific re-assessment; C343: in-patient medical specific assessment; C345: in-patient consultation; C346: in-patient repeat consultation; C348: in-patient partial assessment; C745: in-patient limited consultation |
Appendix 2. Description of covariates used in the multilevel mixed models
| Variables | Definition | Type of variable | Categories |
|---|---|---|---|
| Individual-level characteristics | |||
|
| |||
| Age, years | Age at index year | Categorical | Less than 55 years |
| 55–65 years | |||
| 66–75 years | |||
| Index year | Year of diagnosis | Categorical | Year 2002–2004 |
| Year 2005–2007 | |||
| Year 2008–2010 | |||
| Income quintile | Neighborhood average income quintile | Categorical | 1–5, with 1 representing the lowest income quintile and 5 the highest |
| ADG score | ADG summary score | Continuous | Per 1-unit increment |
| Area of residency | Primary area of residency | Categorical | Urban Rural |
|
| |||
| Physician-level characteristics | |||
|
| |||
| Type of primary physician | Specialty of primary caregiver | Categorical | Urologist Radiation oncologist |
| Physician volume, consultation/year | Annual new PCa-related consultation volume during study period - physician | Categorical | First quartile (<37 case/year) Second quartile (37–58 case/year) Third quartile (58–94 case/year) Fourth quartile (≥94 case/year) |
|
| |||
| Institution-level characteristics | |||
|
| |||
| Type of centre | Main treating institution during first year | Categorical | Non cancer centre Cancer centre |
| Institution volume, consultation/year | Annual new PCa-related consultation volume during study period - institution | Continuous | First quartile (<81 case/year) Second quartile (81–165 case/year) Third quartile (165–358 case/year) Fourth quartile (≥358 case/year) |
ADG: Aggregated Diagnosis Groups; PCa: prostate cancer.
Appendix 3. Definitions of the three sensitivity analyses used to identify men managed by active surveillance
| Sensitivity analysis | Definition |
|---|---|
| Primary definition | Men who underwent repeat biopsies following diagnosis with or without a definitive treatment thereafter. |
| Sensitivity analysis #1 | Men who underwent repeat biopsies following diagnosis with or without a definitive treatment thereafter as well as men who did not undergo a repeat biopsy but underwent definitive treatments more than 12 months after diagnosis. |
| Sensitivity analysis #2 | Men who underwent repeat biopsies following diagnosis with or without definitive treatments thereafter as well as men who did not undergo a repeat biopsy but were treated more than 2 years after diagnosis. |
|
| |
| Sensitivity analysis #3 | Men who underwent repeat biopsies following diagnosis with or without definitive treatments thereafter, men who did not undergo a repeat biopsy but were treated more than 12 months after diagnosis as well as healthy young men who were not treated nor had a repeat biopsy following diagnosis. The latter group was defined as individuals younger than 65 years of age with an ADG score in the lowest tertile. |
ADG: Aggregated Diagnosis Groups.
Appendix 4.
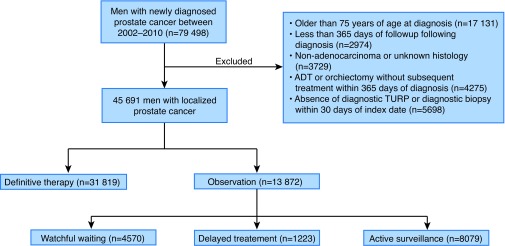
Study flow diagram. ADT: androgen-deprivation therapy; TURP: transurethral resection of the prostate
Appendix 5. Type of management according to year of diagnosis (expectant therapy vs. upfront definitive treatment)
| Year of diagnosis | Expectant therapy n (%) | Definitive treatment n (%) | Total per year n (%) |
|---|---|---|---|
| 2002 | 968 (24) | 3044 (76) | 4012 (9) |
| 2003 | 1057 (26) | 2952 (74) | 4009 (9) |
| 2004 | 1212 (27) | 3321 (73) | 4533 (10) |
| 2005 | 1382 (29) | 3403 (71) | 4785 (11) |
| 2006 | 1650 (31) | 3716 (69) | 5366 (12) |
| 2007 | 1812 (31) | 3974 (69) | 5786 (13) |
| 2008 | 1816 (33) | 3773 (68) | 5589 (12) |
| 2009 | 2011 (34) | 3835 (66) | 5846 (13) |
| 2010 | 1964 (34) | 3701 (66) | 5765 (13) |
| Total | 13 872 (30) | 31 819 (70) | 45 691 (100) |
Cochrane-Armitage test for trend p value <0.001.
Appendix 6. Individual, physician, and institution-level effects on the uptake of active surveillance (multivariable non-linear mixed model adjusted for physician and institution-level clustering)
|
Individuals: 45 691 Physicians: 424 Institutions: 215 |
Model 1 (null model) | Model 2 (plus individual-level char.) | Model 3 (plus physicians-level char.) | Model 4 (plus institution level char.) | Model 5 (Full model) |
|---|---|---|---|---|---|
| −2 log likelihood |
32148 OR (95% CI) |
30169 OR (95% CI) |
32233 OR (95% CI) |
32258 OR (95% CI) |
31656 OR (95% CI) |
| Individual-level characteristics | |||||
|
| |||||
| Age (years old) | |||||
| Less than 55 | REF | REF | |||
| 55–65 | 1.17 (1.07–1.28) | 1.18 (1.08–1.29) | |||
| 66–75 | 1.55 (1.41–1.70) | 1.56 (1.42–1.72) | |||
| Index year | |||||
| 2002–2004 | REF | REF | |||
| 2005–2007 | 1.54 (1.54–1.81) | 1.66 (1.54–1.80) | |||
| 2008–2010 | 1.89 (1.89–2.23) | 2.04 (1.88–2.22) | |||
| Neighbourhood income quintile | |||||
| First quintile (lowest) | REF | REF | |||
| Second quintile | 1.04 (0.94–1.14) | 1.04 (0.94–1.15) | |||
| Third quintile | 0.98 (0.89–1.09) | 0.98 (0.89–1.09) | |||
| Fourth quintile | 1.03 (0.94–1.15) | 1.04 (0.94–1.14) | |||
| Fifth quintile (highest) | 1.16 (1.06–1.29) | 1.17 (1.06–1.28) | |||
| ADG score, per 1-unit increase rural | 1.00 (0.997–1.003) | 1.00 (0.998–1.003) | |||
| Rural living | REF | REF | |||
| Urban living | 1.28 (1.16–1.42) | 1.28 (1.16–1.42) | |||
|
| |||||
| Physician-level characteristics | |||||
|
| |||||
| Type of primary physician | |||||
| Radiation oncologist | REF | REF | |||
| Urologist | 2.10 (1.61–2.73) | 2.26 (1.73–2.97) | |||
| Annual volume | |||||
| First quartile (lowest) | REF | REF | |||
| Second quartile | 0.95 (0.70–1.28) | 0.95 (0.70–1.28) | |||
| Third quartile | 0.97 (0.67–1.39) | 0.98 (0.68–1.40) | |||
| Fourth quartile (highest) | 1.28 (0.85–1.91) | 1.31 (0.87–1.96) | |||
|
| |||||
| Institution-level characteristics | |||||
|
| |||||
| Type of centre | |||||
| Non-cancer centre | REF | REF | |||
| Cancer centre | 0.95 (0.68–1.33) | 1.13 (0.80–1.60) | |||
| Institution volume | |||||
| First quartile (lowest) | REF | REF | |||
| Second quartile | 0.68 (0.32–1.48) | 0.60 (0.28–1.26) | |||
| Third quartile | 0.71 (0.28–1.80) | 0.87 (0.24–1.50) | |||
| Fourth quartile (highest) | 0.94 (0.22–4.01) | 1.13 (0.25–4.29) | |||
| Level 2 (physician) variance | 1.13 | 1.15 | 0.95 | 1.13 | 0.95 |
| Level 3 (institution) variance | 2.51 | 2.46 | 2.46 | 2.48 | 2.40 |
| Intra-class correlation, physician | 16% | 17% | 14% | 16% | 14% |
| Intra-class correlation, institution | 36% | 36% | 37% | 36% | 36% |
ADG: Aggregated Diagnosis Groups; CI: confidence interval; OR: odds ratio.
Appendix 7. Comparison of the fixed effects estimates (full models) modelling the uptake of active surveillance using each of the different definitions
| Main definition | Sensitivity analysis #1‡ | Sensitivity analysis #2* | Sensitivity analysis #3† | |
|---|---|---|---|---|
|
| ||||
| −2 log likelihood |
31656 OR (95% CI) |
35230 OR (95% CI) |
33648 OR (95% CI) |
37911 OR (95% CI) |
| Individual-level characteristics | ||||
|
| ||||
| Age (years old) | ||||
| Less than 55 | REF | REF | REF | REF |
| 55–65 | 1.18 (1.08–1.29) | 1.13 (1.04–1.24) | 1.13 (1.04–1.24) | 1.18 (1.09–1.28) |
| 65–75 | 1.56 (1.42–1.72) | 1.56 (1.43–1.71) | 1.56 (1.43–1.71) | 1.36 (1.26–1.48) |
| Index year | ||||
| 2002–2004 | REF | REF | REF | REF |
| 2005–2007 | 1.66 (1.54–1.80) | 1.48 (1.37–1.59) | 1.59 (1.48–1.72) | 1.52 (1.42–1.63) |
| 2008–2010 | 2.04 (1.88–2.22) | 1.83 (1.69–1.98) | 1.89 (1.75–2.04) | 1.86 (1.73–2.00) |
| Neighbourhood income quintile | ||||
| First quintile (lowest) | REF | REF | REF | REF |
| Second quintile | 1.04 (0.94–1.15) | 1.04 (0.94–1.15) | 1.04 (0.94–1.15) | 1.01 (0.92–1.11) |
| Third quintile | 0.98 (0.89–1.09) | 0.99 (0.90–1.10) | 1.00 (0.90–1.10) | 0.95 (0.86–1.04) |
| Fourth quintile | 1.04 (0.94–1.14) | 1.07 (0.97–1.17) | 1.06 (0.96–1.16) | 1.00 (0.92–1.10) |
| Fifth quintile (highest) | 1.17 (1.06–1.28) | 1.20 (1.09–1.32) | 1.17 (1.07–1.29) | 1.11 (1.02–1.21) |
| ACG score, per 1-unit increase rural | 1.00 (0.998–1.003) | 1.002 (0.999–1.004) | 1.001 (0.998–1.004) | 0.997 (0.995–1.00) |
| Rural living | REF | REF | REF | REF |
| Urban living | 1.28 (1.16–1.42) | 1.33 (1.21–1.47) | 1.28 (1.17–1.29) | 1.23 (1.13–1.34) |
|
| ||||
| Physician-level characteristics | ||||
|
| ||||
| Type of primary physician | ||||
| Radiation oncologist | REF | REF | REF | REF |
| Urologist | 2.26 (1.73–2.97) | 2.46 (1.80–3.36) | 2.10 (1.61–2.73) | 2.16 (1.69–2.77) |
| Annual volume | ||||
| First quartile (lowest) | REF | REF | REF | REF |
| Second quartile | 0.95 (0.70–1.28) | 0.96 (0.72–1.28) | 0.90 (0.67–1.20) | 1.00 (0.76–1.32) |
| Third quartile | 0.98 (0.68–1.40) | 0.89 (0.63–1.26) | 0.91 (0.64–1.29) | 0.85 (0.61–1.19) |
| Fourth quartile (highest) | 1.31 (0.87–1.96) | 1.16 (0.78–1.71) | 1.16 (0.79–1.72) | 1.10 (0.75–1.59) |
|
| ||||
| Institution-level characteristics | ||||
|
| ||||
| Type of centre | ||||
| Non-cancer centre | REF | REF | REF | REF |
| Cancer centre | 1.13 (0.80–1.60) | 0.66 (0.19–2.29) | 1.16 (0.84–1.62) | 1.32 (0.97–1.80) |
| Institution volume | ||||
| First quartile (lowest) | REF | REF | REF | REF |
| Second quartile | 0.60 (0.28–1.26) | 0.73 (0.34–1.58) | 0.56 (0.28–1.13) | 0.50 (0.23–1.06) |
| Third quartile | 0.87 (0.24–1.50) | 0.77 (0.30–1.96) | 0.61 (0.26–1.44) | 0.42 (0.17–2.71) |
| Fourth quartile (highest) | 1.13 (0.25–4.29) | 0.99 (0.21–4.68) | 1.29 (0.34–4.82) | 0.65 (0.16–1.80) |
| Level 2 (physician) variance | 0.95 | 0.91 | 0.91 | 0.84 |
| Level 3 (institution) variance | 2.40 | 2.48 | 2.04 | 2.45 |
| Intra-class correlation, physician | 14% | 14% | 15% | 13% |
| Intra-class correlation, institution | 36% | 37% | 33% | 37% |
Active surveillance defined as a repeat biopsy or delayed treatment (12 months after diagnosis);
active surveillance defined as a repeat biopsy or delayed treatment (24 months after diagnosis);
active surveillance defined as a repeat biopsy, delayed treatment (12 months after diagnosis) or no repeat biopsy and no treatment in a young and healthy patient. ADG: Aggregated Diagnosis Groups; CI: confidence interval; OR: odds ratio.