Abstract
PURPOSE
To examine the feasibility of a retinopathy of prematurity (ROP) telemedicine evaluation system of providing timely feedback to a neonatal intensive care unit (NICU) with at-risk premature infants.
METHODS
This was a prospective observational study of premature infants with birth weights of <1251 g in five NICUs in the United States. Infants scheduled for clinically indicated ROP evaluations underwent indirect ophthalmoscopic examinations and digital imaging on the same day. Imaging was performed by nonphysician retinal imagers. Times required were determined from obtaining digital images of both eyes to submission via web-based system to a secure server for grading by trained readers at a central reading center to sending back grading results to the clinical center.
RESULTS
A total of 1,642 image sets of eyes of 292 infants were obtained, from 823 imaging sessions. The mean turnaround time from submission of image sets of both eyes to return of the grading results to the clinical center was 10.1 ± 11.3 hours (standard deviation), with a median of 12.0 hours (1st quartile, 0.9 hours; 3rd quartile, 16 hours). Overall, 95.5% of gradings (95% CI, 93.9%-96.7%) were returned within 24 hours. Subgroup analyses found, for image sets submitted to the reading center before 2 p.m. Eastern Standard Time, median time to report was 1.7 hours (1st quartile, 0.7 hours; 3rd quartile, 15.5 hours) compared with those submitted after 2pm (median, 14.1 hours; 1st quartile, 11.2, hours; 3rd quartile, 16.3 hours).
CONCLUSIONS
An ROP telemedicine approach can provide timely feedback to the NICU regarding the detection of potentially serious ROP and thus referral to an ophthalmologist for examina tion and consideration of treatment.
Retinopathy of prematurity (ROP) is a leading cause of treatable childhood blindness. At present, premature infants requiring treatment are generally identified by skilled ophthalmologists who visit neonatal intensive care units (NICUs) to examine at-risk infants.1-4
There are a number of difficulties in providing the required diagnostic examinations for at-risk infants. First, there is a limited number of ophthalmologists with ROP expertise worldwide to meet the growing demand for eval uations. In addition, that number could decrease as some ophthalmologists stop examining infants because of workflow difficulties, low reimbursement, and legal liability associated with misdiagnosis or missed examinations.5 Second, there is variability between examiners in the diagnosis of ROP using binocular indirect ophthalmoscopy examinations.6 A potential solution to address these issues is to develop an efficient and cost-effective telemedicine system that uses retinal imaging to detect infants with sight-threatening disease. This approach would allow evaluation of images of at-risk infants to identify those with ROP accompanied by high-risk retinal characteristics (ie, plus disease, stage 3 ROP, or zone I ROP)7 who would require ophthalmoscopic examination. However, for ROP telemedicine to be clinically relevant, feedback to clinical centers must be timely enough to allow for an ophthalmologist's examination to consider treatment within the 2-3 days required for optimum outcome.8
In the NIH-NEI funded, multicenter Telemedicine Approaches to Evaluating Acute-phase ROP (e-ROP) Study,9 we proposed to leverage the experience of remote evaluation of digital images of diabetic retinopathy and tailor it to the needs of the population at risk for ROP, following the principles for diabetic retinopathy telemedicine advanced by Lee in 1999.10 In 2014 the e-ROP study demonstrated the validity of a telemedicine system to identify infants requiring an ROP evaluation by an ophthalmologist in a cohort of 1,257 infants with birth weights of <1251 g from 13 clinical centers in the United States and Canada11; however, feasibility of timely feedback to the neonatal intensive care unit (NICU) was not examined in the original study. The primary objective of the present prospective observational study was to determine whether image evaluation could be achieved and grading returned to the NICU within a 24-hour time frame.
Subjects and Methods
At five e-ROP US clinical centers, infants with birth weight of <1251 g scheduled for clinically indicated ROP evaluations underwent both digital retinal imaging and indirect ophthalmoscopic examinations on the same day. Infants were excluded if they had a severe congenital ocular anomaly or major congenital abnormalities.
Participating institutions were Johns Hopkins University, Vanderbilt University, University of Oklahoma, Children's Hospital of Philadelphia and Hospital of the University of Pennsylvania, and University of Utah. Institutional review board approval was obtained from all participating centers.
Study Procedures
From July 7, 2014, to March 31, 2015, digital imaging was performed by e-ROP certified nonphysician retinal imagers (CRIs), including nurses and technicians familiar with working with premature infants. Infants underwent imaging of both eyes using the RetCam Shuttle (Clarity Medical Systems, Pleasanton, CA) in addition to indirect ophthalmoscopy performed by a study-certified ophthalmologist experienced in ROP. Digital images obtained by the CRI were uploaded by secure web-based portal for remote evaluation by a trained and certified nonphysician reader, designated as a trained reader (TR).
At the reading center, uploaded image sets were assigned to a single reading queue for access and grading by one of 3 TRs. Readers used a structured grading protocol in completing electronic grading forms to document the morphological features of ROP seen in the image sets.12
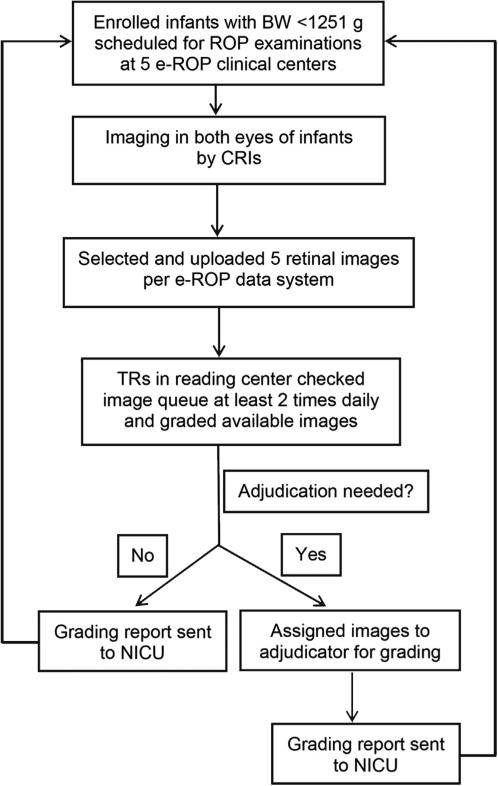
On each workday (7 a.m. Monday to 5 p.m. Friday Eastern Standard Time), each TR logged in using a unique user ID and checked availability of images for grading at least twice a day—on arrival for work in the morning and before departing in the evening. This schedule was modified on October 30, 2014, to require TRs to keep the image queue window open throughout the day while emphasizing that all images were to be graded before the end of each workday. The image set of each eye was graded independently from its fellow eye. TRs were masked from all clinical data. The TR could request additional review of the graded image set before the result was finalized by assigning it to the reading center director queue for review and finalization. The reading center director also logged in using a unique ID on each work day at least twice to check for image sets referred for further review. Once the grading of image sets from both eyes was finalized, the e-ROP grading system automatically sent the grading results to the clinic research coordinator at the NICU in an encrypted message on a secure e-ROP server (Figure 1).
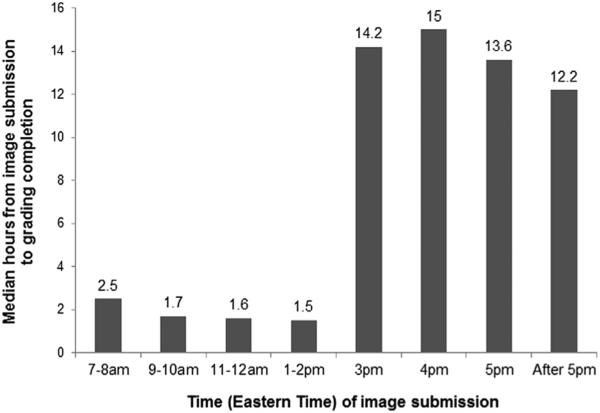
FIG 1.
Median hours from image submission to image grading completion by time (Eastern Standard Time) of image submission.
The time of submission of image sets from both eyes to the e-ROP server and the time when a result report was sent to the clinical center were recorded in the e-ROP image-grading system. We also recorded the time from image acquisition to report sent to clinical center.
During the same time period at a single high-volume center (University of Oklahoma), two e-ROP CRIs also collected data on the time required for each component of imaging, including camera preparation, image acquisition, selecting and saving images, cleaning the camera, and final sorting and uploading of images to the server. The entire data flow from image acquisition to completion of image grading is depicted in eFigure 1.
EFIG 1.
Data flow for the process of image acquisition to image grading completion. BW, birth weight; CRI, certified nonphysician retinal imager; ROP, retinopathy of prematurity; TR, trained reader.
Although results of the e-ROP Study showed no serious adverse events related to the e-ROP Study procedures,13 adverse events were monitored and documented by the study clinical coordinator.
Sample Size and Statistical Analysis
We estimated that 1,000 imaging sessions were needed for a sufficiently precise estimate of the percentage of image grading completion within 24 hours after image submission, with half width of 95% confidence interval within 3%.
For the calculation of time intervals between image acquisition and submission to the completion of grading images from an image session, we did not consider time intervals during weekends and holidays. The grading time was described using mean, standard deviation, median, first quartile (Q1), third quartile (Q3), and range. We also calculated the percentage of completion of image gradings within certain time intervals (≤4 hours, 4-8 hours, 8-16 hours, 16-24 hours, 24-32 hours, 32-40 hours, 40-48 hours, and ≥48 hours). We performed these analyses among all image sessions combined, and in subgroups defined by the time of image submission, by the status of referral-warranted ROP (RW-ROP; defined as zone I ROP, stage 3 or worse ROP, or plus disease) in the image evaluation, and by the study period. We used the χ2 test to compare proportions, the two-group t test for comparing means and the Wilcoxon rank sum test for comparing medians. All statistical analyses were performed in SAS V9.4 (SAS Institute Inc, Cary, NC).
Results
There were 1,642 image sets of eyes of 292 subjects in 823 imaging sessions. All were graded by TRs with a mean turnaround time from image set submission from both eyes to return of the results to the NICU of 10.1 ± 11.3 hours, with a median of 12 hours (Q1 0.9, hours; Q3, 16 hours). Approximately 95.5% (95% CI, 93.9%-96.7%) of gradings were returned within 24 hours of submission (Table 1).
Table 1.
The frequency distribution of time from image acquisition to image submission and image grading completiona
| Time intervals, hours | Time from image acquisition to submission
(n= 823 sessions) |
Time from image submission to grading
completion (n = 823 sessions) |
Time from image acquisition to grading
completion (n = 823 sessions) |
|---|---|---|---|
| No. sessions (%) | No. sessions (%) | No. sessions (%) | |
| ≤4 | 73 (8.9) | 236 (28.7) | 4 (0.5) |
| >1 to ≤4 | 331 (40.2) | 131 (15.9) | 158 (19.2) |
| >4 to ≤8 | 226 (27.5) | 18 (2.2) | 108 (13.1) |
| >8 to ≤16 | 25 (3.0) | 234 (28.4) | 28 (3.4) |
| >16 to ≤24 | 40 (4.9) | 167 (20.3) | 298 (36.2) |
| >24 to ≤32 | 43 (5.2) | 20 (2.4) | 96 (11.7) |
| >32 to ≤40 | 2 (0.2) | 9 (1.1) | 5 (0.6) |
| >40 to ≤48 | 23 (2.8) | 6 (0.7) | 47 (5.7) |
| ≥48 | 60 (7.3) | 2 (0.2) | 79 (9.6) |
| Median (Q1, Q3) | 4.1 (2, 7.7) | 12 (0.9, 16) | 19.2 (5.1, 24.8) |
| Minimum, maximum | 0.1, 607 | 0, 189 | 0.9, 620 |
Weekend days not included in the time calculations.
The median time from obtaining images at the bedside to uploading images sets for grading was 4.1 hours (Q1, 2 hours; Q3, 7.7 hours), although more than 75% were uploaded within 8 hours. Despite the range in time from image acquisition to grading completion with results sent to the NICU, nearly 3 of 4 image results were returned within 24 hours after acquisition. Submitting images earlier during the workday led to quicker receipt of the grading results at the clinical center (Table 2, eFigure 1). When image sets arrived at the reading center before 2 p.m. Eastern Time, results were returned quickly (median, 1.7 hours; Q1, 0.7 hours; Q3, 15.5 hours) compared with those submitted after 2 p.m. (median, 14.1 hours; Q1, 11.2 hours; Q3, 16.3 hours).
Table 2.
Distribution of time from image submission to image grading completion by the time of day of image submissiona
| Time of image submission (Eastern Time) | No. | Hours from image submission to
grading completion, n (%) |
|||||
|---|---|---|---|---|---|---|---|
| Median (Q1, Q3) | ≤1 | >1, ≤4 | >4 to ≤8 | >8 to ≤24 | >24 | ||
| 7-8 am | 49 | 2.5 (0.9, 3.9) | 14 (28.6) | 23 (46.9) | 2 (4.1) | 8 (16.3) | 2 (4.1) |
| 9-10 am | 87 | 1.7 (0.7, 4.6) | 28 (32.2) | 32 (36.8) | 9 (10.3) | 7 (8.1) | 11 (12.6) |
| 11-12 am | 93 | 1.6 (0.7, 4.6) | 38 (40.9) | 31 (33.3) | 5 (5.4) | 15 (16.1) | 4 (4.3) |
| 1-2 pm | 167 | 1.5 (0.6, 16.3) | 65 (38.9) | 40 (24.0) | 1 (0.6) | 56 (33.5) | 5 (3.0) |
| 3 pm | 127 | 14.2 (0.4, 16.3) | 52 (40.9) | 3 (2.4) | 0 (0) | 67 (52.8) | 5 (3.9) |
| 4 pm | 153 | 15.0 (12.3, 17.8) | 36 (23.5) | 2 (1.3) | 0 (0) | 107 (69.9) | 8 (5.2) |
| 5 pm | 84 | 13.6 (12.9, 15.6) | 3 (3.6) | 0 (0) | 0 (0) | 79 (94.1) | 2 (2.4) |
| After 5 pm | 63 | 12.2 (11.5, 13.2) | 0 (0.0) | 0 (0) | 1 (1.6) | 62 (98.4) | 0 (0) |
The reading center was located in the Eastern Time Zone; 2 clinical centers were located in the Eastern Time Zone and 3 were located in the Central Time Zone.
The time from image submission to grading completion increased slightly when RW-ROP was present in the retinal images of one or both eyes of an infant (Table 3). For image sessions that did not show RW-ROP, more than 96% of gradings were returned in ≤24 hours, whereas sessions with RW-ROP in one or both eyes decreased to 94.9% but dropped to 90.9% for sessions when the RWROP status was indeterminate.
Table 3.
The frequency distribution of time from image submission to image grading completion by RW-ROPa status from image grading
| Time intervals, hours | Time from image submission to
image grading completion |
P value | ||
|---|---|---|---|---|
| RW-ROP absent in an image session (n = 500
sessions) |
RW-ROP present in an image session (n = 290
sessions) |
RW-ROP indeterminate in an image session (n
= 33 sessions) |
||
| No. of sessions (%) | No. of sessions (%) | No. of sessions (%) | ||
| ≤1 | 147 (29.4) | 80 (27.6) | 9 (27.3) | 0.048 |
| >1, ≤4 | 89 (17.8) | 34 (11.7) | 8 (24.2) | |
| >4, ≤8 | 11 (2.2) | 7 (2.41) | 0 (0) | |
| >8, ≤16 | 123 (24.6) | 104 (35.9) | 7 (21.1) | |
| >16, ≤24 | 111 (22.2) | 50 (17.2) | 6 (18.2) | |
| >24, ≤32 | 11 (2.2) | 7 (2.4) | 2 (6.1) | |
| >32, ≤40 | 6 (1.2) | 3 (1.0) | 0 (0) | |
| >40, ≤48 | 1 (0.2) | 4 (1.4) | 1 (3.0) | |
| ≥48 | 1 (0.2) | 1 (0.3) | 0 (0) | |
| Median (Q1, Q3) | 9.75 (0.8, 16.2) | 12.7 (0.9, 15.7) | 3.5 (1.0, 17.4) | 0.88 |
| Minimum, maximum | 0, 189 | 0.1, 65.6 | 0.20, 46.8 | |
| Adjudicated (%) | 61 (12.2%) | 62 (21.4%) | 12 (36.4%) | <0.0001 |
RW-ROP, referral-warranted ROP; ROP, retinopathy of prematurity.
RW-ROP is any zone I ROP, stage 3 or worse ROP, or plus disease.
The TRs requested adjudication by the reading center director for 135 image set sessions of the 823 sessions (16.4%). When adjudication was requested, time from image submission to grading completion increased (Table 4) from a median of 10.4 hours (Q1, 0.7 hours; Q3, 15.5 hours) to 15.4 hours (Q1, 3.0 hours; Q3, 20.9 hours). Adjudication reduced the percentage of sessions in which the process could be completed in ≤24 hours from 98.2% to 81.5% (Table 4). Adjudication was more common in image sessions in which RW-ROP was found (21.4%) or was indeterminate (36.4%) than images sessions without RW-ROP (12.2%; Table 3).
Table 4.
Frequency distribution for time from image submission to image grading completion by need for adjudication
| Time intervals, hours | Time from image submission to
image grading completion |
|
|---|---|---|
| Sessions required adjudication (n = 135
sessions) |
Session not required adjudication (n = 688
sessions) |
|
| No. sessions (%) | No. sessions (%) | |
| ≤1 | 15 (11.1) | 221 (32.1) |
| >1, ≤4 | 26 (19.3) | 105 (15.3) |
| >4, ≤8 | 7 (5.2) | 11 (1.6) |
| >8, ≤16 | 28 (20.7) | 206 (29.9) |
| >16, ≤24 | 34 (25.2) | 133 (19.3) |
| >24, ≤32 | 12 (8.9) | 8 (1.2) |
| >32, ≤40 | 5 (3.7) | 4 (0.6) |
| >40, ≤48 | 6 (4.4) | 0 (0) |
| ≥48 | 2 (1.5) | 0 (0) |
| Median (Q1, Q3) | 15.4 (3.0, 20.9) | 10.4 (0.7, 15.5) |
| Minimum, maximum | 0.5, 189 | 0, 39.2 |
The importance of frequent monitoring by TRs for image sets available for grading is highlighted in Table 5. After changing from a twice-a-day surveillance to more sustained surveillance throughout work day, there was a significant decrease in time from submission to grading completion from a median of 15.2 hours before October 30, 2014, to 1.8 hours thereafter. Similarly, the percentage of gradings returned within 24 hours increased from 91.4% before October 30, 2014 to 98.8% thereafter. The percentage of image sessions requiring adjudication was unchanged.
Table 5.
Frequency distribution of time from image submission to image grading completion by grading perioda
| Time intervals, hours | From image submission to image
grading completion |
From image acquisition to image
grading completion |
||||
|---|---|---|---|---|---|---|
| Before or on October 30, 2014 (n = 357
sessions) |
After October 30, 2014 (n = 466
sessions) |
P value | Before or on October 30, 2014 (n = 357 sessions) | After October 30, 2014 (n = 466 sessions) | P value | |
| No. sessions (%) | No. sessions (%) | |||||
| ≤1 | 63 (17.7) | 173 (37.1) | <0.0001 | 0 (0) | 4 (0.9) | <0.0001 |
| >1, ≤4 | 37 (10.4) | 94 (20.2) | 46 (12.9) | 112 (24.0) | ||
| >4, ≤8 | 9 (2.5) | 9 (1.9) | 44 (12.3) | 64 (13.7) | ||
| >8, ≤16 | 98 (27.5) | 136 (29.2) | 9 (2.5) | 19 (4.1) | ||
| >16, ≤24 | 119 (33.3) | 48 (10.3) | 156 (43.7) | 142 (30.5) | ||
| >24, ≤32 | 18 (5.0) | 2 (0.4) | 64 (17.9) | 32 (6.9) | ||
| >32, ≤40 | 7 (2.0) | 2 (0.4) | 3 (0.8) | 2 (0.4) | ||
| >40, ≤48 | 5 (1.4) | 1 (0.2) | 20 (5.6) | 27 (5.8) | ||
| ≥48 | 1 (0.3) | 1 (0.2) | 15 (4.2) | 64 (13.7) | ||
| Median (Q1, Q3) | 15.2 (2.9, 19.4) | 1.8 (0.6, 14.1) | <0.0001 | 20.2 (7.6, 24.4) | 17.7 (4.1, 26.1) | 0.003 |
| Minimum, maximum | 0, 65.6 | 0.1, 189 | 1.2, 620 | 0.9, 216 | ||
| Adjudicated (%) | 59 (16.5) | 76 (16.3) | 1.00 | |||
After October 30, 2014, the reading center implemented more systematic grading approach that required trained readers check the queue at least 3 times daily and complete all available gradings by the end of the day.
At a single center, two imagers collected times for the various tasks for ROP telemedicine. For the 157 sessions, mean time for preparation of imaging was 6.8 minutes, 7.2 minutes for image acquisition at the bedside, and 7.1 minutes for image selection at the bedside. Mean times for final sorting and uploading image sets were 5.7 and 6.4 minutes, respectively. Mean total time for all tasks was 19.2 minutes with a range of 7-37 minutes.
Discussion
Telemedicine in ROP must rapidly and effectively identify those infants with sight-threatening ROP for timely treatment. The purpose of this implementation project was to determine the feasibility of returning image gradings from at-risk infants to NICUs within 24 hours so that an ophthalmic consultation can be undertaken urgently if indicated. This goal was accomplished in more than 95% of the image sessions, although we did not require weekend gradings in this research study. Turnaround times must be narrowed before using a telemedicine system for clinical care. Ideally results would be available to the NICU and the responsible ophthalmologist on the same day as imaging occurred. One obvious improvement that we implemented in this study was to tighten the monitoring schedule that readers used (Table 5). Turnaround time within 24 hours improved from 95% to almost 99% with this tighter schedule and would allow for no clinically important delay in obtaining a needed examination by an ophthalmologist and treatment.
A secondary goal of this implementation project was to identify potential gaps in the process of care between obtaining images from an at-risk infant and receipt of the report at the infant's NICU. This complex process includes many steps including acquiring, selecting, and uploading images for each eye to reading queues for the readers, further review of the grading if needed, and then returning results to the NICU. One problem encountered often was an extended time from acquisition of the images to uploading. The protocol did not mandate this timing for the imagers to allow them to complete their imaging visit to the NICU as quickly as possible. This lag could be minimized with improved technology for selecting and submitting images, with this task ideally completed before leaving the bedside. A second issue was the dramatic effect of time of day when images are submitted to the readers’ queue. Another simple improvement would be coordinating the time of the examinations and submission of image sets with the reading center capac ity. As shown in Table 2, the time from submission to completion of grading increases substantially later in the day. This could be improved by increased staffing to meet the peak demand times or by having clinical centers and reading centers better coordinate timing for their imaging and reading sessions. In addition, an improved system for notifications (eg, text message) to readers when images are received, rather than periodic checking of a queue, would reduce the time to final report. Finally, in a widely used system of telemedicine for ROP, multiple reading centers distributed across several time zones would improve response times.
At a single center, two imagers collected times to completion of their tasks. Mean total time for all tasks was 19.2 minutes (range, 7-37 minutes). These data indicate that imaging of an infant and submission of those image sets for grading can be accomplished generally in <20 minutes, a time that is likely to decrease with improvements in technology and protocols.
The need for additional review of image grading substantially increases the grading turnaround time. An adjudication process tailored specifically to characteristics of RW-ROP versus not RW-ROP, that is, determining plus versus no plus, zone I ROP versus not Zone I ROP, or stage 3 versus not stage 3, and ignoring stage 1 versus stage 2 and normal vessels vs pre-plus, could make the assessment faster for potentially critical image sets. If the TR judged the images unreadable, rapid notification of this result to the clinical center would allow for reimaging quickly or requesting an ophthalmological examination.
There are some process changes that should be considered when translating this telemedicine approach to clinical practice in ROP. This research project was not designed for “round the clock” grading or imaging. However, from the results of this implementation study, image sets submitted before 2 p.m. were graded and reports returned to the clinical centers more rapidly than those submitted in the late afternoon (Table 2, eFigure 1). However, it would be impractical during clinical care to plan imaging of all infants in the early morning with quick submission of those images. A reasonable compromise might be for the reading center to have the capacity to read as many images as possible by early afternoon leading to the same day return of the result. Supporting that suggestion is the quick turnaround we observed for images submitted to the reading center between 11 a.m. and 2 p.m. in this study. Submission of images late in the day markedly increased times from submission to completion, largely because gradings were not completed until the next day.
Our study has important strengths. We used well-trained retinal imagers who were familiar with the camera, handling premature infants, and the e-ROP imaging system. Nurseries were familiar with the imaging protocol, having been involved in the preceding e-ROP study.
There are some limitations to our results. Interpretation of the study results should take into account that it was conducted in high-intensity NICUs with well-trained imagers in a research protocol. This level of imaging expertise will need to be reached and maintained in NICUs that undertake telemedicine in ROP. Further, we have studied a single approach with trained non-physician readers with physician review if needed. The turnaround times may be different with clinician readers who would likely have other clinical responsibilities. Another factor that must be considered is that all nurseries in this study had readily available ophthalmic consultation that might not be as available in other nursery settings. The generalizability of these findings to less intensity NICUs that likely have fewer infants at high risk for serious ROP must be further examined.
Acknowledgments
Funded by National Eye Institute of the National Institutes of Health, Department of Health and Human Services. U10 EY017014.
Footnotes
clinicaltrials.gov national registry number: NCT01264276.
References
- 1.Gilbert C, Fielder A, Gordillo L, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005;115:e518–25. doi: 10.1542/peds.2004-1180. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert C, Foster A. Blindness in children: control priorities and research opportunities. Br J Ophthalmol. 2001;85:1025–7. doi: 10.1136/bjo.85.9.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kemper AR, Wallace DK. Neonatologists’ practices and experiences in arranging retinopathy of prematurity screening services. Pediatrics. 2007;120:527–31. doi: 10.1542/peds.2007-0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kemper AR, Freedman SF, Wallace DK. Retinopathy of prematurity care: patterns of care and workforce analysis. J AAPOS. 2008;12:344–8. doi: 10.1016/j.jaapos.2008.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Altersitz K, Piechock IM. AAO Retinopathy of Prematurity Survey. Lawrenceville; New Jersey: 2006. Survey of 224 pediatric ophthalmologists and retina specialists. [Google Scholar]
- 6.Reynolds JD, Dobson V, Quinn GE, et al. Evidence-based screening criteria for retinopathy of prematurity: natural history data from the CRYO-ROP and LIGHT-ROP studies. Arch Ophthalmol. 2002;120:1470–76. doi: 10.1001/archopht.120.11.1470. [DOI] [PubMed] [Google Scholar]
- 7.Ells AL, Holmes JM, Astle WF, et al. Telemedicine approach to screening for severe retinopathy of prematurity: a pilot study. Ophthalmology. 2003;110:2113–17. doi: 10.1016/S0161-6420(03)00831-5. [DOI] [PubMed] [Google Scholar]
- 8.Early Treatment For Retinopathy Of Prematurity Cooperative G. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94. doi: 10.1001/archopht.121.12.1684. [DOI] [PubMed] [Google Scholar]
- 9.Quinn G, on behalf of the e-ROP Cooperative Group Telemedicine approaches to evaluating acute-phase retinopathy of prematurity: study design. Ophthalmic Epidemiol. 2014;21:256–67. doi: 10.3109/09286586.2014.926940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee P. Telemedicine: opportunities and challenges for the remote care of diabetic retinopathy (editorial). Arch Ophthalmol. 1999;117:1639–40. doi: 10.1001/archopht.117.12.1639. [DOI] [PubMed] [Google Scholar]
- 11.Quinn GE, Ying GS, Daniel E, et al. Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmol. 2014;132:1178–84. doi: 10.1001/jamaophthalmol.2014.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniel E, Quinn GE, Hildebrand PL, et al. Validated System for Centralized Grading of Retinopathy of Prematurity: Telemedicine Approaches to Evaluating Acute-Phase Retinopathy of Prematurity (e-ROP) Study. JAMA Ophthalmol. 2015;133:675–82. doi: 10.1001/jamaophthalmol.2015.0460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wade K, Pistilli M, Baumritter A, et al. Safety of ROP Examination and imaging in Premature Infants in the e-ROP Telemedicine Study. J Pediatr. 2015;167:994–1000. doi: 10.1016/j.jpeds.2015.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]