Abstract
Background
People who inject drugs (PWID) face barriers to healthcare due to reasons including comorbidity. We evaluated access to health and social services by three of the most prevalent comorbid conditions among PWID: HIV, hepatitis C (HCV), and mental health, in an urban setting in Canada.
Methods
Data were derived from prospective cohorts of community-recruited PWID between 2005 and 2015. HIV and HCV serostatuses were based on antibody tests, while mental health conditions and inability to access health and social services (barriers to access) were determined by participants’ self-report. We employed generalized linear mixed models controlling for confounders to examine associations between health conditions and barriers to access.
Results
Among 2494 participants, 1632 (65.4%) reported barriers to access at least once over a median of seven (IQR: 3, 12) semi-annual assessments. Mental health conditions were independently associated with increased odds of reporting barriers (adjusted Odds Ratio (aOR): 1.45, 95% Confidence Interval (CI): 1.32, 1.58), while HIV was not (aOR: 0.96, 95% CI: 0.85, 1.08), and HCV was associated with decreased odds (aOR: 0.80, 95% CI: 0.69, 0.93). The associations between mental health conditions and barriers to access were consistent among PWID without HIV/HCV (aOR: 1.35, 95% CI: 1.10, 1.65), with HCV mono-infection (aOR: 1.55, 95% CI: 1.37, 1.75), and HCV/HIV co-infection (aOR: 1.36, 95% CI: 1.15, 1.60).
Conclusions
Targeted strategies to seek and treat mental health conditions in settings that serve PWID, and assist PWID with mental health conditions in navigating healthcare system may improve the publicly-funded health and social services.
Keywords: Service access, Comorbidity, Drug use, Mental health conditions, HIV, HCV
INTRODUCTION
Illicit drug use, particularly injection drug use, is associated with costly health and social impacts. There are an estimated 112,900 active people who inject drugs (PWID) in Canada, accounting for about 0.4% of the Canadian population aged 15 years and older (Public Health Agency of Canada, 2014). About 11% of PWID are living with HIV, approximately 68% have or have had hepatitis C virus (HCV), and up to 10% are co-infected with HIV and HCV, according to data from 11 sentinel sites across Canada (Public Health Agency of Canada, 2012). Concurrent substance use and mental health disorders are also very common (Crawford et al., 2003). Among those who seek help for an addiction, over 50% report additional mental health conditions (Canadian Centre on Substance Abuse, 2009). Moreover, there is prevalent occurrence of mental health conditions either before or following the diagnosis or treatment of HIV and HCV (Schaefer et al., 2012 and World Health Organization, 2008a). Meanwhile, PWID may also experience homelessness, unemployment, physical and sexual abuse, poor family and social relationships, criminalization and incarceration, and stigma and discrimination in healthcare settings (Galea and Vlahov, 2002, Harrison et al., 1997, Neale, 2002 and Richardson et al., 2013).
The implementation of harm reduction and aggressive HIV treatment strategies has led to considerable progress in British Columbia (BC), Canada (Lourenco et al., 2014). The number of clients in opioid agonist treatment across the province rose from 2800 in 1996 to almost 14,000 in 2012 (Nosyk et al., 2013). This was accompanied by a reduction in the incidence of HIV among PWID, with the number of new diagnoses falling to just 29 in 2012, from a high of 352 in 1996 (Montaner et al., 2014). As a result, PWID are living longer (Hogg et al., 2008 and World Health Organization, 2012) and new challenges to their quality of life have arisen, requiring combined efforts from health and social service providers trained in the care of substance use, medical comorbidity and social problems (Neale et al., 2008). Such challenges are faced by many North American cities which have large numbers of people who use drugs (Coffin et al., 2015 and Des Jarlais et al., 2000). In Vancouver, BC’s Downtown Eastside (DTES) neighbourhood, where a large proportion of the population regularly uses drugs (Roe, 2009), there are over fifty health and social service providers deliver services in areas of primary care, mental health and addiction, low-barrier gateway and navigation, housing and shelter, communicable disease prevention, and specialized harm reduction and HIV treatment (Vancouver Coastal Health, 2015).
In many settings, PWID face barriers to accessing health and social services at multiple levels, with some difficulties attributed to their distinct health conditions. These include: early HCV treatment guidelines which exclude PWID (Kensington, 1997); clinicians who withhold antiretroviral therapy (ART) from HIV-infected PWID (Westergaard et al., 2012) or regard substance use or HIV-HCV co-infection as a challenge (Kamarulzaman and Altice, 2015 and Grebely and Tyndall, 2011); addiction treatment which limits access for people with concurrent mental health and substance use disorders (el-Guebaly, 2004); exposure to correctional facilities which disrupt access to evidence-based care (Milloy et al., 2014); and social and structural barriers such as stigma and discrimination, lack of housing, and fear of criminalization (Harris and Rhodes, 2013, Krusi et al., 2010, Neale et al., 2008, Treloar et al., 2013 and Wolfe et al., 2010).
Previous studies have evaluated access to addiction treatment in Vancouver among illicit drug users (Barker et al., 2015, Milloy et al., 2010, Phillips et al., 2014 and Prangnell et al., 2016). However, among PWID, there has been limited research in evaluating access to the wide range of health and social services available. Although people with different health conditions have unique treatment needs and face distinct barriers associated with their conditions, variations in access among PWID by health condition have not been examined. Strategies to improve health outcomes through a more integrated health system have been initiated both internationally and locally (National Treatment Agency for Substance Misuse, 2006 and Vancouver Coastal Health, 2015). Comprehensive evaluation of PWID’s access to the currently existing services, and identifying subgroups of individuals who disproportionately experience increased barriers to access will provide valuable information for the planning and implementation of those strategies.
As such, the current study evaluates PWID’s self-reported inability to access health and social services and investigates the relationship between comorbid health conditions and self-reported inability to access health and social services in an urban setting of Vancouver, Canada.
MATERIALS AND METHODS
Study design and subjects
This analysis uses data on illicit drug users residing in the Greater Vancouver region from a series of ongoing open prospective cohort studies: the AIDS Care Cohort to evaluate Exposure to Survival Services (ACCESS), the Vancouver Injection Drug Users Study (VIDUS), and the At-Risk Youth Study (ARYS). The three cohorts have followed HIV-seropositive illicit drug users (aged greater than 18), HIV-seronegative PWID (aged greater than 18), and street-involved youth (aged 14–26) who use illicit drugs, respectively, through word of mouth, street outreach, and referrals since 2005 (Strathdee et al., 1997). Sampling and follow-up methodologies have been described in detail previously (Strathdee et al., 1997, Tyndall et al., 2003, Wood et al., 2006a and Wood et al., 2006b). At baseline and semi-annual follow-up, individuals complete an interviewer-administered questionnaire that elicits information pertaining to socio-demographic characteristics, drug use, services utilization, HIV risk behaviors and other exposures and outcomes. The cohort instruments are harmonized across cohorts to facilitate pooled analyses. Participants also provide blood specimens for HIV and HCV serology. Participants are offered an honorarium of $30 CAD for each study visit. All studies have been approved by the University of British Columbia/Providence Health Care Research Ethics Board.
All participants recruited between September, 2005 and May, 2015 who completed their baseline assessment, and who ever injected drugs during the study period were included in the study. Observations were excluded if individuals never injected drugs at the time of assessment, or their self-reported inability to access health and social services, or covariates of interest were missing.
Measures
The primary outcome of interest was a binary variable capturing self-reported inability to access health and social services (barriers to access) in the last six months determined from the question “In the last six months, was there a time you were in need of a service but could not obtain it?”. In addition, participants were asked to specify the service they were unable to obtain: “If yes, can you tell me what it was; check all that apply: counsellor; drug treatment facility (e.g., detox, rehab); hospital/doctor/nurse/clinic; dentist; optometrist; housing; needle exchange; peer group/support group; police/parole officer; social worker; study staff; welfare; food services; other (specify)”. We selectively categorized those who answered counsellor, drug treatment facilities, dentists, optometrists, hospital/doctor/nurse/clinic and needle exchange as being unable to access health services, and those who answered housing, food services, welfare and social worker as being unable to access social services for further investigation.
Our primary covariates of interest were the three most prevalent comorbid health conditions among PWID: HIV, HCV and mental health conditions (Canadian Centre on Substance Abuse, 2009, Public Health Agency of Canada, 2012, Schaefer et al., 2012 and World Health Organization, 2008a). Diagnosis of HIV and HCV were based on antibody tests conducted at each study visit. Mental health conditions were determined by a binary composite indicator constructed to capture any of the following self-reported markers of mental health conditions in the last six months: 1) diagnosis with one of the following mental illnesses: depression, anxiety, obsessive compulsive disorder, schizophrenia, post-traumatic stress disorder, personality disorder, bipolar, attention deficit disorder, oppositional defiance disorder, other hyperactive disorder; 2) receipt of mental health treatment; 3) suicide attempt or ideation; and 4) hospitalization for a mental illness.
To examine the cumulative effects and interactions between health conditions, a continuous indicator was constructed to capture the number of conditions per individual at each follow-up and a categorical indicator was constructed representing eight mutually exclusive patient subgroups with the occurrence of: HIV; HCV; mental health conditions; HIV and HCV; HIV and mental health conditions; HCV and mental health conditions; HIV, HCV and mental health conditions; and without any of the three conditions at each follow-up.
In addition, we defined an a priori set of covariates to include in the models based on evidence from the literature regarding their associations with inability to access addiction treatment or other health and social services for drug users in Vancouver (Barker et al., 2015, Milloy et al., 2010, Phillips et al., 2014 and Prangnell et al., 2016). These covariates regarding PWID’s sociodemographic characteristics, drug use patterns, criminalization, and other social and structural factors included age (in years), male (yes vs no), Caucasian (yes vs other), ≥daily heroin use, ≥daily stimulants use, ≥daily prescription opioid use, non-fatal overdose, binge alcohol use, incarceration, homelessness, employment, sex work, drug dealing and reporting being the victim of violence. Other than age, gender and race, all covariates were binary and time-dependent, based on the six month period prior to assessment. We additionally included another two covariates, residing in the DTES in the last six months, and calendar year of each assessment (2005–2007, 2008–2010, 2011–2013, and 2014–2015), for the purpose of investigating differences in PWID’s barriers to access by residence and changes in access over time.
Statistical analysis
The analysis proceeded in three steps. First, we carried out a series of exploratory data analysis. We assessed the descriptive characteristics of the study sample at the most recent follow-up; examined the prevalence of different comorbid health conditions among PWID; described the frequency of reporting barriers to access each type of health and social service of interest; and compared the differences in sociodemographic characteristics, health conditions, drug use patterns, and other structural factors among people who ever reported barriers to access against those who never reported barriers to access. Pearson’s χ2 tests and Mann-Whitney tests were used to compare categorical and continuous variables, respectively.
Second, we employed generalized linear mixed multiple regression models (GLMMs) with a logit link and binomial distribution to investigate associations between health conditions and self-reported inability to access health and social services in the last six months. As most individuals had repeated measures over the study period, a random intercept was specified in the model to account for unmeasured individual-specific confounding that is fixed over time (Raudenbush and Bryk, 2002). Comorbid health conditions were modeled in three ways by including different constructed indicators in the models: 1) occurrence of each health condition, adjusting for the other two; 2) the number of health conditions each individual has; 3) eight mutually exclusive patient subgroups, to examine the independent effects, cumulative effects, and interactions between conditions, respectively. In addition, each model also controlled for the a priori decided set of covariates described above.
Lastly, we performed several sensitivity analyses to support the robustness of the results. First, we repeated the analysis for each mental health condition marker independently. Second, we examined the associations between health conditions and barriers to access selected health services, and selected social services. Third, we removed housing from the outcome variable construction and repeated the analysis to assess if the results were mainly driven by individuals’ barriers to access housing services, which was the service most reported to be inaccessible. Fourth, we investigated whether being on agonist treatment or HIV ART modified the association between mental health conditions and barriers to access. All statistical analyses were executed in SAS version 9.4 and figures were produced in R version 3.2.3.
RESULTS
A total of 2575 participants met the study’s inclusion criteria. We excluded 81 (3.1%) participants due to missing information on either the primary outcome or on covariates of interest in all of their assessments. Another 289 observations were excluded as they had never-injected drugs prior to the assessment. As a result, a total of 2494 participants, with 18,028 observations were analyzed in the current study.
Detailed characteristics of the study participants at their most recent follow-up are presented in Table 1. The study sample was comprised of 33.6% females and 62.2% Caucasians, with a median age of 42.9 years (IQR: 29.2, 51.3). Among 2494 participants, 792 (31.8%) tested HIV positive, 1885 (75.6%) tested HCV positive, and 1971 (79.0%) reported a mental health condition. Comorbid health conditions were common in our study sample. A total of 577 (23.1%) participants had HIV, HCV, and a mental health condition, 145 (5.8%) had HIV and HCV, 59 (2.4%) had HIV and mental health conditions, and 884 (35.5%) had HCV and mental health conditions during the study period.
Table 1.
Characteristics of 2494 Participants at the Most Recent Follow-Up, and Comparisons between Who Ever/Never Reported Inability to Access Health and Social Services.
| Total (N = 2494) |
Ever (N = 1632) |
Never (N = 862) |
P- value |
|
|---|---|---|---|---|
| Characteristics (N (%)) | ||||
| Study visits (Median [IQR]) | 7 [3,12] | 8 [4,13] | 4 [2,10] | <0.001 |
| Age in years (Median [IQR]) | 42.9 [29.2, 51.3] |
43.6 [29.7, 51.5] |
41.0 [27.9, 51.0] |
0.026 |
| Male | 1657 (66.4) | 1075 (65.9) | 582 (67.5) | 0.41 |
| Caucasian | 1551 (62.2) | 1011 (61.9) | 540 (62.6) | 0.73 |
| Residing in DTES, L6M | 1334 (53.5) | 870 (53.3) | 464 (53.8) | 0.81 |
| In a stable relationshipa, L6M | 702 (28.2) | 469 (28.8) | 233 (27.1) | 0.38 |
| Education, less than high school | 1318 (53.0) | 862 (53.0) | 456 (52.9) | 0.97 |
| Employment, L6M | 657 (26.3) | 423 (25.9) | 234 (27.1) | 0.51 |
| Daily heroin use, L6M | 343 (13.8) | 208 (12.7) | 135 (15.7) | 0.044 |
| Daily prescription opioids use, L6M |
108 (4.3) | 71 (4.4) | 37 (4.3) | 0.95 |
| Daily stimulants use, L6M | 665 (26.7) | 430 (26.3) | 235 (27.3) | 0.62 |
| Overdose, ever | 1485 (59.5) | 1022 (62.6) | 463 (53.7) | <0.001 |
| Binge alcohol use, ever | 2209 (88.6) | 1478 (90.6) | 731 (84.8) | <0.001 |
| Incarceration, ever | 1957 (78.5) | 1304 (79.9) | 653 (75.8) | 0.017 |
| Homelessness, ever | 2262 (90.7) | 1526 (93.5) | 736 (85.4) | <0.001 |
| Dealing drugs, ever | 1985 (79.6) | 1323 (81.1) | 662 (76.8) | 0.012 |
| Sex work, ever | 762 (30.6) | 537 (32.9) | 225 (26.1) | <0.001 |
| Victim of violence, L6M | 443 (17.8) | 316 (19.4) | 127 (14.7) | 0.004 |
| HIV positive | 792 (31.8) | 490 (30.0) | 302 (35.0) | 0.011 |
| HCV positive | 1885 (75.6) | 1230 (75.4) | 655 (76.0) | 0.73 |
| Mental health conditions, ever | 1971 (79.0) | 1372 (84.1) | 599 (69.5) | <0.001 |
| Calendar year | <0.001 | |||
| 2005–2007 | 325 (13.0) | 155 (9.5) | 170 (19.7) | |
| 2008–2010 | 406 (16.3) | 251 (15.4) | 155 (18.0) | |
| 2011–2013 | 1036 (41.5) | 734 (45.0) | 302 (35.0) | |
| 2014–2015 | 727 (29.1) | 492 (30.1) | 235 (27.3) | |
| Cohort | 0.008 | |||
| ACCESS | 785 (31.5) | 485 (29.7) | 300 (34.8) | |
| VIDUS | 1139 (45.7) | 780 (47.8) | 359 (41.6) | |
| ARYS | 570 (22.9) | 367 (22.5) | 203 (23.5) |
Abbreviatios: DTES: downtown eastside; L6M: last six months; ACCESS: the AIDS Care Cohort to evaluate Exposure to Survival Services; VIDUS: the Vancouver Injection Drug Users Study; ARYS: the At-Risk Youth Study.
Legally married/common law/regular partner.
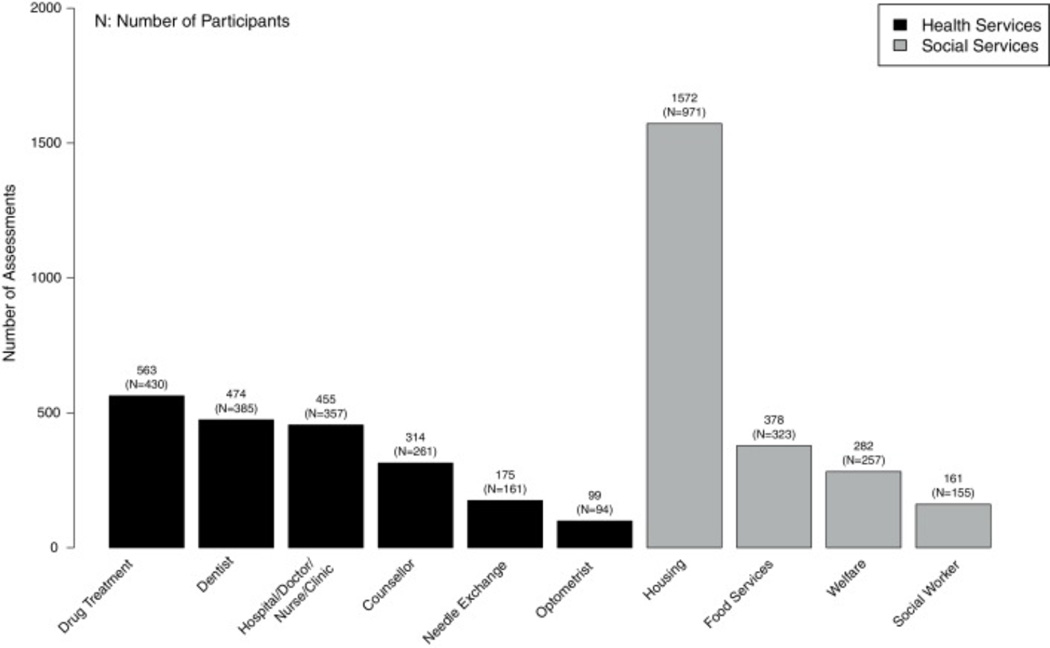
Over a median of seven study visits (IQR: 3, 12), 1632 participants (65.4%) reported barriers to access at least once during the study period. Barriers to access were reported in 3642 (20.2%) of the 18,028 assessments included in the study, with the proportion decreasing from 24.0% in 2005–2007 to 17.2% in 2014–2015. Specifically, 988 (39.6%) participants ever reported inability to access health services, and 1161 (46.6%) participants ever reported inability to access social services. Fig. 1 shows the frequency of reporting inability to access these selected types of services in the six months prior to assessment. Compared to those who never reported barriers to access, those who reported positively at least once during the study period were more likely to have mental health conditions (84.1% vs. 69.5%), but were less likely to be HIV positive (30.0% vs. 35.0%). They were also significantly more likely to have ever overdosed (62.6% vs. 53.7%), binged on alcohol (90.6% vs. 84.8%), been incarcerated (79.9% vs. 75.8%), been homeless (93.5% vs. 85.4%), dealt drugs (81.1% 76.8%), and been involved in sex work (32.9% 26.1%) (Table 1).
Figure 1.
Frequency of self-reporting inaccessible health and social services in the previous 6 months of assessment among 2494 participants
In our multiple regression analysis, after controlling for socio-demographics, drug use patterns, and other social and structural factors, self-reported mental health conditions in the last six months were significantly associated with increased odds of reporting barriers to access (adjusted Odds Ratio (aOR): 1.45, 95% Confidence Interval (CI): 1.32, 1.58), while HIV was not (aOR: 0.96, 95% CI: 0.85, 1.08). HCV was associated with decreased odds of reporting barriers to access (aOR: 0.80, 95% CI: 0.69, 0.93) (Table 2).
Table 2.
Bivariate and Multiple Regression Analyses of Factors Associated with Self-reported Inability to Access Health and Social Services in the Previous 6 Months of Assessment (aN = 2494).
| Bivariate | Multivariable | |||
|---|---|---|---|---|
| Unadjusted OR (95% CI) |
P- value |
Adjusted OR (95% CI) |
P- value |
|
| Mental health conditions, L6M | 1.61 (1.48–1.75) | <0.001 | 1.45 (1.32–1.58) | <0.001 |
| HIV positive | 0.69 (0.61–0.78) | <0.001 | 0.96 (0.85–1.08) | 0.50 |
| HCV positive | 0.51 (0.45–0.58) | <0.001 | 0.80 (0.69–0.93) | 0.003 |
| Age in years | 0.96 (0.96, 0.97) | <0.001 | 1.00 (0.99, 1.00) | 0.37 |
| Male | 0.91 (0.81–1.03) | 0.14 | 0.82 (0.73–0.93) | 0.002 |
| Caucasian | 1.33 (1.19–1.50) | <0.001 | 1.23 (1.10–1.38) | <0.001 |
| Residing in DTES, L6M | 1.00 (0.91–1.10) | 0.97 | 0.90 (0.82–0.99) | 0.034 |
| Employment, L6M | 1.10 (1.00–1.22) | 0.050 | 1.08 (0.98–1.20) | 0.12 |
| Daily heroin use, L6M | 1.32 (1.18–1.48) | <0.001 | 0.97 (0.86–1.09) | 0.60 |
| Daily prescription opioids use, L6M |
1.04 (0.86–1.25) | 0.71 | 0.91 (0.75–1.11) | 0.36 |
| Daily stimulants use, L6M | 1.28 (1.17–1.40) | <0.001 | 0.95 (0.85–1.05) | 0.29 |
| Overdose, L6M | 1.91 (1.63–2.23) | <0.001 | 1.39 (1.18–1.63) | <0.001 |
| Binge alcohol use, L6M | 1.56 (1.42–1.72) | <0.001 | 1.25 (1.14–1.39) | <0.001 |
| Incarceration, L6M | 1.89 (1.67–2.14) | <0.001 | 1.19 (1.04–1.36) | 0.009 |
| Homelessness, L6M | 3.22 (2.95–3.53) | <0.001 | 2.57 (2.33–2.84) | <0.001 |
| Sex work, L6M | 1.41 (1.21–1.64) | <0.001 | 1.07 (0.91–1.25) | 0.41 |
| Dealing drugs, L6M | 1.76 (1.59–1.94) | <0.001 | 1.21 (1.08–1.34) | <0.001 |
| Victim of violence, L6M | 2.59 (2.35–2.85) | <0.001 | 1.95 (1.76–2.16) | <0.001 |
| Calendar year | ||||
| 2005–2007 | Reference | Reference | ||
| 2008–2010 | 0.92 (0.84–1.02) | 0.12 | 1.10 (0.99–1.22) | 0.064 |
| 2011–2013 | 0.56 (0.50–0.63) | <0.001 | 0.80 (0.71–0.90) | <0.001 |
| 2014–2015 | 0.62 (0.52–0.73) | <0.001 | 0.80 (0.67–0.96) | 0.018 |
Abbreviations: DTES: downtown eastside; L6M: last six months.
A total of 2494 participants with 18,028 observations were analyzed.
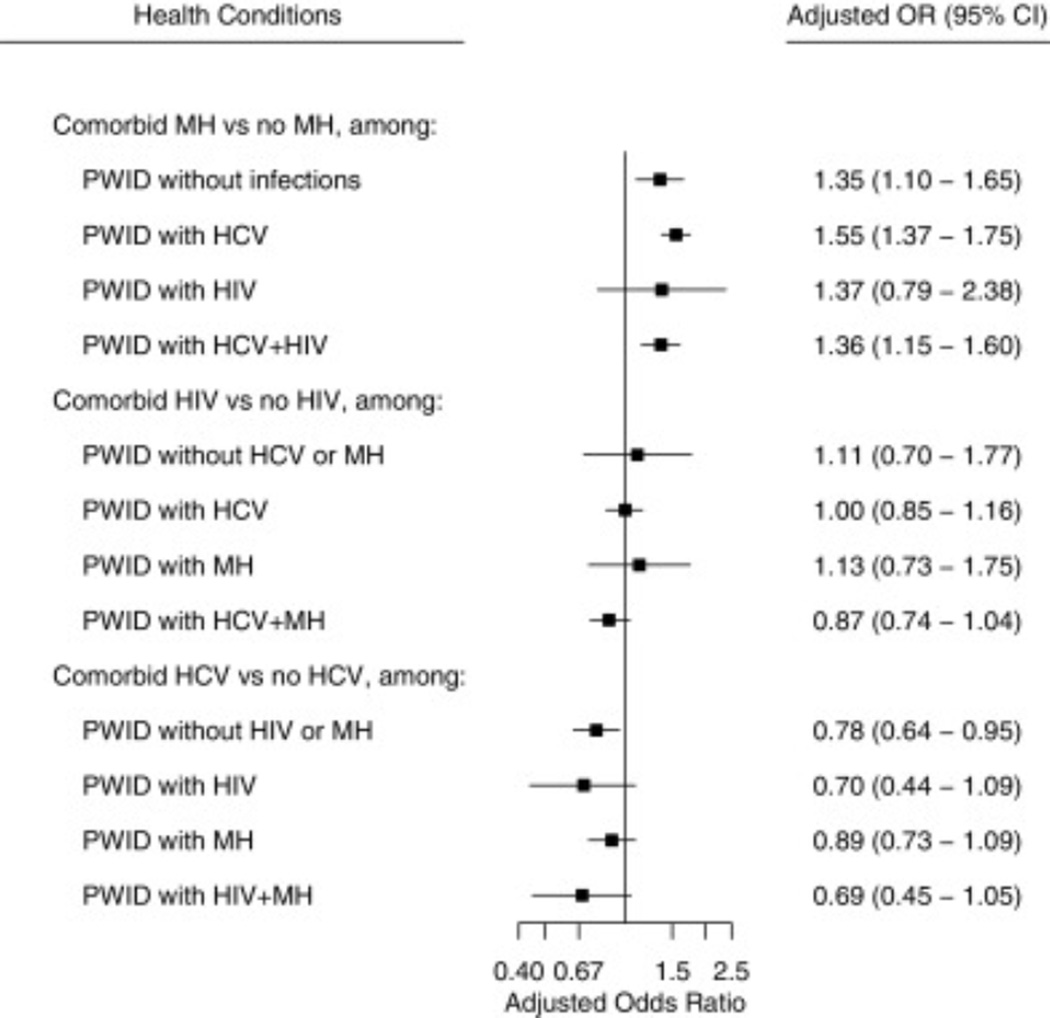
In addition, we observed an increasing trend (P < 0.001) between the number of health conditions and barriers to access (aOR: 1.13, 95% CI: 1.07, 1.21). A comprehensive comparison of barriers to access among PWID with comorbid health conditions is shown in Fig. 2. There appeared to be no interaction between health conditions. Notably, mental health conditions were consistently associated with increased barriers to access among PWID without HIV or HCV (aOR: 1.35, 95% CI: 1.10, 1.65), with HCV mono-infection (aOR: 1.55, 95% CI: 1.37, 1.75), and HCV and HIV co-infection (aOR: 1.36, 95% CI: 1.15, 1.60) (Fig. 2). Our sensitivity analysis which examined the barriers to accessing health services and barriers to accessing social services separately (Supplementary Table 1), and on barriers to accessing services excluding housing (Supplementary Table 2) supported the results from the main analysis.
Figure 2.
Associations between Comorbid Health Conditions and Self-reported Inability to Access Health and Social Services in the Previous 6 Months of Assessment. The scale corresponds to the logarithmic scale of odds ratio. Model adjusted for age, gender, race, daily heroin use, daily stimulants use, daily prescription opioid use, overdose, alcohol binge, incarceration, homelessness, employment, sex work, drug dealing, victim of violence, reside in DTES, and calendar year. Abbreviations: MH: mental health conditions; HCV: hepatitis C; OR: odds ratio; DTES: downtown eastside.
The association between mental health conditions and barriers to access also remained significant regardless of the measure of mental health conditions. The adjusted odds ratios ranged from 1.31 (95% CI: 1.19, 1.45) for those who reported receipt of mental health treatment in the last six months, to 1.48 (95% CI: 1.31, 1.68) for those who had suicide ideation or attempt in the last six months, when compared against their counterparts (Table 3). Moreover, mental health conditions were associated with increased barriers to access regardless of PWID’s participation in agonist treatment, or ART (Table 3).
Table 3.
Associations between Mental Health Conditions and Self-reported Inability to Access Health and Social Services in the Previous 6 Months of Assessment, byaMental Health Condition Indicators and bybTreatment Access.
| Unadjusted OR (95% CI) |
P- value |
cAdjusted OR (95% CI) |
P- value |
|
|---|---|---|---|---|
| Mental health condition indicators, L6M | ||||
| Diagnosis with a mental illness | 1.86 (1.68–2.06) | <0.001 | 1.41 (1.26–1.58) | <0.001 |
| Receipt of mental health treatment |
1.34 (1.22–1.47) | <0.001 | 1.31 (1.19–1.45) | <0.001 |
| Suicide attempt or ideation | 1.82 (1.61–2.06) | <0.001 | 1.48 (1.31–1.68) | <0.001 |
| Hospitalization for a mental illness |
1.87 (1.57–2.22) | <0.001 | 1.35 (1.12–1.61) | 0.001 |
| Agonist treatment accessd,e | ||||
| PWID on agonist treatment, L6M |
1.58 (1.41, 1.78) | <0.001 | 1.41 (1.25, 1.59) | <0.001 |
| PWID not on agonist treatment, L6M |
1.68 (1.48, 1.91) | <0.001 | 1.51 (1.33, 1.72) | <0.001 |
| ART accesse | ||||
| HIV-positive PWID on ART, current |
1.38 (1.14, 1.66) | 0.001 | 1.31 (1.05, 1.62) | 0.015 |
| HIV-positive PWID not on ART, current |
1.75 (1.33, 2.29) | <0.001 | 1.45 (1.06, 1.99) | 0.021 |
Abbreviations: OR: odds ratio; CI: confidence interval; PWID: people who inject drugs; L6M: last six months; ART: antiretroviral therapy.
Analysis was repeated for four self-reported mental health condition indicators to examine the associations between different mental health condition indicators and the outcome.
Analysis was repeated for PWID by agonist treatment access, and among HIV-positive PWID by ART access.
Adjusted for HIV, HCV, age, gender, race, daily heroin use, daily stimulants use, daily prescription opioid use, overdose, alcohol binge, incarceration, homelessness, employment, sex work, drug dealing, victim of violence, reside in DTES, and calendar year.
Agnoist treatment includes methadone program, cocaine treatment program, detox centre, in-patient and out-patient treatment centre and others.
No statistically-significant differences in the adjusted odds ratios by agonist treatment access (P = 0.42) and ART access (P = 0.92).
Finally, Table 2 also shows other factors independently associated with barriers to access. Residing in DTES appeared to be associated with lower odds of reporting barriers to access (aOR: 0.90, 95% CI: 0.82, 0.99). We also observed improvement in barriers to access over time. Compared to years 2005–2007, the adjusted odds ratios of reported barriers to access were 1.10 (95% CI, 0.99, 1.22) for years 2008–2010, 0.80 (95% CI, 0.71, 0.90) for years 2011–2013, and 0.80 (95% CI, 0.67, 0.96) for years 2014–2015 (Table 2).
DISCUSSION
The current study analyzed self-reported inability to access a wide range of health and social services among PWID in Vancouver, Canada and found variations by health condition. Over 65% of participants reported an inability to access services at some point during the study period. We found mental health conditions were independently associated with increased barriers to access health and social services.
According to the 2002 Canadian Community Health Survey, 39% of Canadians with a mental disorder or substance dependence sought formal and informal health services in the year before data collection compared with 10% of general Canadians, revealing notable and elevated service needs associated with a mental disorder or substance dependence (Urbanoski et al., 2007). Moreover, there is a growing demand for mental health services, which may outpace the current system’s capacity. In Vancouver hospitals, mental health-related emergency visits increased from 6520 to roughly 10,000, and substance use-related visits increased from 2779 to 5660, between 2009 and 2014 (Lupick, 2015a and Vancouver Police Department, 2013). For patients who attempt to access services outside the acute care setting, there is a long wait time for mental health services. In the first half of 2014, the median time an individual waited for the first meeting with a Vancouver regional comminuty mental heath team or an outpatient psychiatric team was between 10 and 20, and 20 and 40 days, respectively (Lupick, 2015b). In addition, a previous study of homeless people in urban settings within BC observed very low proportions of participants had seen a psychiatrist (14.9%) and a mental health team (12.7%), despite over 90% of them having a mental health disorder (Krausz et al., 2013). Participants perceived being poorly connected to the system of care as one of the primary reasons for not using services (Krausz et al., 2013). Lastly, the double stigma of mental health and substance abuse increased barriers for patients’ care-seeking (Clement et al., 2015). Therefore, PWID with mental health conditions may have greater service needs than those without, need more health and social services than are available, or systematically encounter barriers to existing services, resulting in the observed elevated self-reported barriers to access. Consistently, several other studies revealed that mental health conditions were associated with increased barriers to access care among homeless people, adolescents and young adults (Gulliver et al., 2010 and Krausz et al., 2013).
In addition, we found mental health conditions were associated with increased barriers to access services despite individual’s participation in addiction treatment, suggesting the need to link patients within addiction treatment programs to mental health services. One US study found 70% of HIV-negative PWID on drug treatment reported unmet mental health treatment needs (Stein and Friedmann, 2002). As context to these findings, mental health and addiction treatment services have matured independently in North America with treatment programs developed on a paradigm that treats one condition exclusively as the primary focus (el-Guebaly, 2004 and Health. and Rush, 2002). Consequently, addiction treatment settings often lack the mental health personnel and resources to treat mental health conditions (McGovern et al., 2006) and substance use often causes barriers for PWID to access regular mental health services. Strategies such as providing integrated mental health and addiction treatment services have shown to be associated with improved treatment outcomes (Grella et al., 2010). Continued efforts to integrate these two services are important in reducing barriers faced by PWID with mental health conditions. If integration cannot be achieved in all settings or in a short time, screening consenting clients for common mental health conditions in addiction treatment and harm reduction programs could help facilitate comprehensive care if such programs are linked with and make referrals to mental health services.
Furthermore, our findings reveal the need to improve the connection between HIV treatment settings and other services. We observed HIV was not associated with barriers to access services. Mental health conditions, however, were consistently associated with increased barriers to access services among PWID with or without infections, even among HIV-positive PWID with or without ART. In BC, ART is freely available for PWID (Montaner et al., 2010), and considerable efforts have been made to engage PWID into HIV treatment and harm reduction services through integrated approaches (Lourenco et al., 2014). Studies have demonstrated improvements in HIV treatment engagement within a cohort of Vancouver-based PWID, with the proportion of HIV-positive PWID who achieve an undetectable viral load under treatment increasing from 30% in 2006 to 71% in 2012 (Milloy, 2015). However, uptake of HCV treatment among PWID in BC remains low despite therapeutic advances (Alavi et al., 2014, Grebely et al., 2009 and Lima et al., 2015). The low self-reported inability to access services among HCV-positive PWID may be partially explained by the long latency period for the disease, poor tolerability of pegylated interferon-based regimens, and low perceived need for treatment (Doab et al., 2005, Jordan et al., 2013, Mehta et al., 2008 and Swan et al., 2010). Poor coordination between services (Harris and Rhodes, 2013, Hoffman et al., 2004, Krusi et al., 2010 and Nosyk et al., 2014), however, largely compromised access to care among PWID, especially when managing comorbid health conditions. The improved engagement in HIV treatment provides an important opportunity to seek and treat mental health conditions and HCV among HIV-positive PWID on ART. Future efforts need to continue the integration of HIV care and addiction treatment and extend the integration to mental health and HCV. The ideal would be a comprehensive integrated care model, with all required services located at the same setting, or if not possible, through referral pathways and linkages to local services (World Health Organization, 2008b).
On a more positive note, we found PWID residing in the DTES were less likely to report barriers to access than those residing outside of the DTES, which may be attributed to the concentration of health and social service providers in the DTES (Vancouver Coastal Health, 2015). Moreover, the observed decreases in barriers to access in more recent years compared with earlier periods also indicate improvements in service availability or integration.
Our study has several limitations. First, self-reported information was used to identify mental health conditions among PWID. Nevertheless, consistent results observed using different indicators of mental health conditions in the current study suggest our findings are robust against the measure. Second, our outcome was determined from a question that was constructed in a way that compared people who needed but did not receive services to both those who did not need a service and those who needed and received services. Therefore, we could not separately examine the degree of increased self-reported inability to access services attributed to increased needs of services or increased barriers to access services. Third, although we have controlled for a number of covariates that are potentially associated with the outcome, we cannot rule out unmeasured confounding in the relationships we’ve tested. We limit our purpose to examining whether our defined health conditions were associated with barriers to access besides other known factors, rather than make any causal inference, which is also consistent with our objective to identify access variations by health condition. Finally, caution must be exercised in applying our estimates to PWID populations in different settings, which may feature substantially different levels and quality of health and social services available to populations of PWID.
CONCLUSIONS
A large proportion of our sample of PWID within the Greater Vancouver Area reported an inability to access health and social services. Mental health conditions were independently associated with increased barriers to access. Targeted strategies to seek and treat mental health conditions in settings that serve PWID, and assist PWID with mental health conditions in navigating the healthcare system may improve the efficiency and effectiveness of publicly-funded health and social services.
Supplementary Material
Highlights.
Over 65% of people who inject drugs (PWID) reported inability to access care in Vancouver (2005–2015).
Mental health conditions were associated with increased barriers to access care.
Need to assist PWID with mental health conditions to navigate the healthcare system.
Need to seek and treat mental health conditions in settings that serve PWID.
Acknowledgments
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff.
Role of funding source
The study was supported by the US National Institutes of Health (U01DA038886, R01DA021525) and the Canadian Institutes of Health Research (MOP-102742). This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine, which supports Dr. Evan Wood. Dr. Kora DeBeck is supported by a Michael Smith Foundation for Health Research/St. Paul’s Hospital-Providence Health Care Career Scholar Award. Dr. M-J Milloy is supported by a Michael Smith Foundation for Health Research Scholar award and the National Institutes of Health (R01-DA021525). His institution has received unstructured funding from NG Biomed, Ltd., to support his research. Dr. Kanna Hayashi is supported by a Canadian Institutes of Health Research New Investigator Award (MSH-141971). Dr. Bohdan Nosyk is supported by a Michael Smith Foundation for Health Research Scholar award.
Footnotes
Conflict of interest
No conflict declared.
Contributors
LW designed the study, managed data, performed analyses, and drafted the manuscript. DP interpreted results and drafted the manuscript. JEM reviewed the analysis and revised the manuscript. KD secured data, revised the manuscript and provided critical comments. MJ secured data, revised the manuscript and provided critical comments. TK secured data, revised the manuscript and provided critical comments. KH designed the study, secured data, revised the manuscript and provided critical comments. BN designed the study, revised the manuscript and provided critical comments. LW had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved of the final manuscript.
REFERENCES
- Alavi M, Raffa JD, Deans GD, Lai C, Krajden M, Dore GJ, Tyndall MW, Grebely J. Continued low uptake of treatment for hepatitis C virus infection in a large community-based cohort of inner city residents. Liver Int. 2014;34:1198–1206. doi: 10.1111/liv.12370. [DOI] [PubMed] [Google Scholar]
- Barker B, Kerr T, Nguyen P, Wood E, DeBeck K. Barriers to health and social services for street-involved youth in a Canadian setting. J. Public Health Pol. 2015;36:350–363. doi: 10.1057/jphp.2015.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Centre on Substance Abuse. Substance Abuse In Canada: Concurrent Disorders. Ottawa: Canadian Centre on Substance Abuse; 2009. [Google Scholar]
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Morgan C, Rusch N, Brown JS, Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015;45:11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- Coffin PO, Jin H, Huriaux E, Mirzazadeh A, Raymond HF. Trends in use of health care and HIV prevention services for persons who inject drugs in San Francisco: results from National HIV Behavioral Surveillance 2005–2012. Drug Alcohol Depend. 2015;146:45–51. doi: 10.1016/j.drugalcdep.2014.10.025. [DOI] [PubMed] [Google Scholar]
- Crawford V, Crome IB, Clancy C. Co-existing problems of mental health and substance misuse (dual diagnosis): a literature review. Drugs Educ. Prev. Policy. 2003;10:S1–S74. [Google Scholar]
- Des Jarlais DC, Marmor M, Friedmann P, Titus S, Aviles E, Deren S, Torian L, Glebatis D, Murrill C, Monterroso E, Friedman SR. HIV incidence among injection drug users in New York City, 1992–1997: evidence for a declining epidemic. Am. J. Public Health. 2000;90:352–359. doi: 10.2105/ajph.90.3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doab A, Treloar C, Dore GJ. Knowledge and attitudes about treatment for hepatitis C virus infection and barriers to treatment among current injection drug users in Australia. Clin. Infect. Dis. 2005;40:S313–S320. doi: 10.1086/427446. [DOI] [PubMed] [Google Scholar]
- Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Rep. 2002;117(Suppl. 1):S135–S145. [PMC free article] [PubMed] [Google Scholar]
- Grebely J, Tyndall MW. Management of HCV and HIV infections among people who inject drugs. Curr. Opin. Hiv. Aids. 2011;6:501–507. doi: 10.1097/COH.0b013e32834bcb36. [DOI] [PubMed] [Google Scholar]
- Grebely J, Raffa JD, Lai C, Krajden M, Kerr T, Fischer B, Tyndall MW. Low uptake of treatment for hepatitis C virus infection in a large community-based study of inner city residents. J. Viral Hepat. 2009;16:352–358. doi: 10.1111/j.1365-2893.2009.01080.x. [DOI] [PubMed] [Google Scholar]
- Grella CE, Stein JA, Weisner C, Chi F, Moos R. Predictors of longitudinal substance use and mental health outcomes for patients in two integrated service delivery systems. Drug Alcohol Depend. 2010;110:92–100. doi: 10.1016/j.drugalcdep.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10 doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M, Rhodes T. Hepatitis C treatment access and uptake for people who inject drugs: a review mapping the role of social factors. Harm Reduct. J. 2013;10:7. doi: 10.1186/1477-7517-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison PA, Fulkerson JA, Beebe TJ. Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse Neglect. 1997;21:529–539. doi: 10.1016/s0145-2134(97)00013-6. [DOI] [PubMed] [Google Scholar]
- Rush BR. Health, C.f.A.a.M. Best Practices: Concurrent Mental Health and Substance Use Disorders. Ottawa: Health Canada; 2002. [Google Scholar]
- Hoffman HL, Castro-Donlan CA, Johnson VM, Church DR. The Massachusetts HIV, hepatitis, addiction services integration (HHASI) experience: responding to the comprehensive needs of individuals with co-occurring risks and conditions. Public Health Rep. 2004;119:25–31. doi: 10.1016/j.phr.2004.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogg R, Lima V, Sterne JAC, Grabar S, Battegay M, Bonarek M, Monforte AD, Esteve A, Gill MJ, Harris R, Justice A, Hayden A, Lampe F, Mocroft A, Mugavero MJ, Staszewski S, Wasmuth JC, van Sighem A, Kitahata M, Guest J, Egger M, May M, Coll ATC. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan AE, Masson CL, Mateu-Gelabert P, McKnight C, Pepper N, Bouche K, Guzman L, Kletter E, Seewald RM, Des-Jarlais DC, Sorensen JL, Perlman DC. Perceptions of drug users regarding Hepatitis C screening and care: a qualitative study. Harm Reduct. J. 2013;10 doi: 10.1186/1477-7517-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamarulzaman A, Altice FL. Challenges in managing HIV in people who use drugs. Curr. Opin. Infect. Dis. 2015;28:10–16. doi: 10.1097/QCO.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kensington MD. National institutes of health consensus development conference panel statement: management of hepatitis C. Hepatology. 1997;26:2S–10S. doi: 10.1002/hep.510260701. [DOI] [PubMed] [Google Scholar]
- Krausz RM, Clarkson AF, Strehlau V, Torchalla I, Li K, Schuetz CG. Mental disorder, service use, and barriers to care among 500 homeless people in 3 different urban settings. Soc. Psychiatry Psychiatr. Epidemiol. 2013;48:1235–1243. doi: 10.1007/s00127-012-0649-8. [DOI] [PubMed] [Google Scholar]
- Krusi A, Wood E, Montaner J, Kerr T. Social and structural determinants of HAART access and adherence among injection drug users. Int. J. Drug Policy. 2010;21:4–9. doi: 10.1016/j.drugpo.2009.08.003. [DOI] [PubMed] [Google Scholar]
- Lima VD, Rozada I, Grebely J, Hull M, Lourenco L, Nosyk B, Krajden M, Yoshida E, Wood E, Montaner JSG. Are interferon-free direct-acting antivirals for the treatment of HCV enough to control the epidemic among people who inject drugs? PLoS One. 2015;10 doi: 10.1371/journal.pone.0143836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lourenco L, Lima VD, Heath K, Nosyk B, Gilbert M, Colley G, Consolacion T, Barrios R, Hogg R, Krajden M, Konrad S, Murti M, Nelson J, May-Hadford J, Haggerstone J, Pick N, Gustafson R, Rusch M, Day I, Montaner JS, et al. Process monitoring of an HIV treatment as prevention program in British Columbia, Canada. J. Acquir. Immune Defic. Syndr. 2014;67:E94–E109. doi: 10.1097/QAI.0000000000000293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupick T. The Georgia Straight. Vancouver: Vancouver Free Press Publishing Corp; 2015a. A five-year snapshot of Vancouver’s mental-health crisis (graphic) [Google Scholar]
- Lupick T. The Georgia Straight. Vancouver: Vancouver Free Press Publishing Corp; 2015b. Vancouver’s ill and addicted lost In a mental-health care maze. [Google Scholar]
- McGovern MP, Xie HY, Segal SR, Siembab L, Drake RE. Addiction treatment services and co-occurring disorders: prevalence estimates, treatment practices, and barriers. J. Subst. Abuse Treat. 2006;31:267–275. doi: 10.1016/j.jsat.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Mehta SH, Genberg BL, Astemborski J, Kavasery R, Kirk GD, Vlahov D, Strathdee SA, Thomas DL. Limited uptake of hepatitis C treatment among injection drug users. J. Commun. Health. 2008;33:126–133. doi: 10.1007/s10900-007-9083-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milloy MJS, Kerr T, Zhang R, Tyndall M, Montaner J, Wood E. Inability to access addiction treatment and risk of HIV infection among injection drug users recruited from a supervised injection facility(dagger) J. Public Health-UK. 2010;32:342–349. doi: 10.1093/pubmed/fdp089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milloy MJ, Montaner JSG, Wood E. Incarceration of people living with HIV/AIDS: implications for treatment-as-prevention. Curr. HIV-AIDS Rep. 2014;11:308–316. doi: 10.1007/s11904-014-0214-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milloy MJ. HIV TasP for PWID and implications for HCV TasP: the North American experience. 8th International AIDS Society Conference on HIV Pathogenesis, Treatment, and Prevention; Vancouver. 2015. [Google Scholar]
- Montaner JSG, Lima VD, Barrios R, Yip B, Wood E, Kerr T, Shannon K, Harrigan PR, Hogg RS, Daly P, Kendall P. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–539. doi: 10.1016/S0140-6736(10)60936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montaner JSG, Lima VD, Harrigan PR, Lourenco L, Yip B, Nosyk B, Wood E, Kerr T, Shannon K, Moore D, Hogg RS, Barrios R, Gilbert M, Krajden M, Gustafson R, Daly P, Kendall P. Expansion of HAART coverage is associated with sustained decreases in HIV/AIDS morbidity, mortality and HIV transmission: the HIV treatment as prevention experience in a Canadian setting. PLoS One. 2014;9 doi: 10.1371/journal.pone.0087872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Treatment Agency FOR Substance Misuse. Models Of Care For Treatment Of Adult Drug Misusers: Update 2006. National Treatment Agency FOR Substance Misuse; 2006. [Google Scholar]
- Neale J, Tompkins C, Sheard L. Barriers to accessing generic health and social care services: a qualitative study of injecting drug users. Health Soc. Care Community. 2008;16:147–154. doi: 10.1111/j.1365-2524.2007.00739.x. [DOI] [PubMed] [Google Scholar]
- Neale J. Drug Users in Society. New York: Palgrave; 2002. Nosyk, B., Anglin, M.D., Brissette, S., Kerr, T., Marsh, D.C., Schackman, B.R., Wood, E. [Google Scholar]
- Montaner JS. A call for evidence-based medical treatment of opioid dependence in the United States and Canada. Health Aff. (Millwood) 2013;32:1462–1469. doi: 10.1377/hlthaff.2012.0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyk B, Anglin MD, Brissette S, Kerr T, Marsh DC, Schackman BR, Wood E, Montaner JS. A call for evidence-based medical treatment of opioid dependence in the United States and Canada. Health Aff. (Millwood) 2013;32:1462–1469. doi: 10.1377/hlthaff.2012.0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyk B, Fischer B, Sun HY, Marsh DC, Kerr T, Rehm JT, Anis AH. High levels of opioid analgesic co-prescription among methadone maintenance treatment clients in British Columbia, Canada: results from a population-level retrospective cohort study. Am. J. Addict. 2014;23:257–264. doi: 10.1111/j.1521-0391.2014.12091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M, DeBeck K, Desjarlais T, Morrison T, Feng C, Kerr T, Wood E. Inability to access addiction treatment among street-involved youth in a Canadian setting. Subst. Use Misuse. 2014;49:1233–1240. doi: 10.3109/10826084.2014.891618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prangnell A, Daly-Grafstein B, Dong HR, Nolan S, Milloy MJ, Wood E, Kerr T, Hayashi K. Factors associated with inability to access addiction treatment among people who inject drugs in Vancouver, Canada. Subst. Abuse Treat. Prev. Policy. 2016;11:9. doi: 10.1186/s13011-016-0053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada. Summary of key findings from I-track phase 3 (2010–2012). Surveillance and Epidemiology Division, Professional Guidelines and Public Health Practice Division; Centre for Communicable Diseases and Infection Control; Public Health Agency of Canada. 2012. [Google Scholar]
- Public Health Agency of Canada. HIV/AIDS Epi Updates Chapter 1: National HIV Prevalence and Incidence Estimates for 2011. Centre for Communicable Diseases and Infection Control, Public Health Agency of Canada; 2014. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Newbury Park: Sage; 2002. [Google Scholar]
- Richardson L, Wood E, Kerr T. The impact of social, structural and physical environmental factors on transitions into employment among people who inject drugs. Soc. Sci. Med. 2013;76:126–133. doi: 10.1016/j.socscimed.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roe GW. Fixed in place: Vancouver’s downtown eastside and the community of clients. BC Stud. 2009;1:26. [Google Scholar]
- Schaefer M, Capuron L, Friebe A, Diez-Quevedo C, Robaeys G, Neri S, Foster GR, Kautz A, Forton D, Pariante CM. Hepatitis C infection, antiviral treatment and mental health: a European expert consensus statement. J. Hepatol. 2012;57:1379–1390. doi: 10.1016/j.jhep.2012.07.037. [DOI] [PubMed] [Google Scholar]
- Stein MD, Friedmann P. Need for medical and psychosocial services among injection drug users: a comparative study of needle exchange and methadone maintenance. Am. J. Addict. 2002;11:262–270. doi: 10.1080/10550490290088063. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Patrick DM, Currie SL, Cornelisse PG, Rekart ML, Montaner JS, Schechter MT, O’Shaughnessy MV. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS. 1997;11:7. doi: 10.1097/00002030-199708000-00001. [DOI] [PubMed] [Google Scholar]
- Swan D, Long J, Carr O, Flanagan J, Irish H, Keating S, Keaveney M, Lambert J, McCormick PA, McKiernan S, Moloney J, Perry N, Cullen W. Barriers to and facilitators of hepatitis C testing, management, and treatment among current and former injecting drug users: a qualitative exploration. Aids Patient Care STDS. 2010;24:753–762. doi: 10.1089/apc.2010.0142. [DOI] [PubMed] [Google Scholar]
- Treloar C, Rance J, Backmund M. Understanding barriers to hepatitis C virus care and stigmatization from a social perspective. Clin. infect. Dis. 2013;57(Suppl. 2):S51–S55. doi: 10.1093/cid/cit263. [DOI] [PubMed] [Google Scholar]
- Tyndall MW, Currie S, Spittal P, Li K, Wood E, O’Shaughnessy MV, Schechter MT. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003;17:887–893. doi: 10.1097/00002030-200304110-00014. [DOI] [PubMed] [Google Scholar]
- Urbanoski KA, Rush BR, Wild TC, Bassani DG, Castel S. Use of mental health care services by Canadians with co-occurring substance dependence and mental disorders. Psychiatr. Serv. 2007;58:962–969. doi: 10.1176/ps.2007.58.7.962. [DOI] [PubMed] [Google Scholar]
- Vancouver Coastal Health. Vancouver Coastal Health; 2015. Downtown Eastside Second Generation Health System Strategy: Design Paper. [Google Scholar]
- Vancouver Police Department. Vancouver’s Mental Health Crisis: An Update Report. Vancouver: 2013. [Google Scholar]
- Westergaard RP, Ambrose BK, Mehta SH, Kirk GD. Provider and clinic-level correlates of deferring antiretroviral therapy for people who inject drugs: a survey of North American HIV providers. J. Int. Aids Soc. 2012;15 doi: 10.1186/1758-2652-15-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe D, Carneri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376:355–366. doi: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]
- Wood E, Stoltz JA, Li K, Montaner JSG, Kerr T. Changes in Canadian heroin supply coinciding with the Australian heroin shortage. Addiction. 2006a;101:689–695. doi: 10.1111/j.1360-0443.2006.01385.x. [DOI] [PubMed] [Google Scholar]
- Wood E, Stoltz JA, Montaner JS, Kerr T. Evaluating methamphetamine use and risks of injection initiation among street youth: the ARYS study. Harm Reduct. J. 2006b;3:1. doi: 10.1186/1477-7517-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Geneva: World Health Organization; 2008a. HIV/AIDS And Mental Health. [Google Scholar]
- World Health Organization. Geneva: World Health Organization; 2008b. Management Of Common Health Problems Of Drug Users. [Google Scholar]
- World Health Organization. Treatment And Care For Injecting Drug Users. Switzerland: World Health Organization Geneva; 2012. WHO, UNODC, UNAIDS technical guide for countries to set targets for universal access to HIV prevention. 2012 Revision. [Google Scholar]
- el-Guebaly N. Concurrent substance-related disorders and mental illness: the North American experience. World Psychiatry. 2004;3:182–187. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.