Abstract
Background
To study male-female and age differences in estimates of rapid transition from first full drink to alcohol dependence among youthful newly incident drinkers in the United States (US).
Method
The study population included 12-to-25-year-old non-institutionalized US civilian residents, sampled for US National Surveys on Drug Use and Health 2002–2013, with assessments via confidential computer assisted self-interviews. Newly incident drinkers are those who had their first full drink soon before the assessment (n=32,562 12–25 year olds). Alcohol dependence (AD) criteria are from DSM-IV.
Results
For 12-to-25-year-old females, the peak risk for making a rapid transition from first full drink to alcohol dependence is seen during adolescence, followed by declining estimates (meta-analysis summary=3% at 12–17 years of age, 95% CI= 2%, 3%). Among males, corresponding estimates fluctuate around 2%, with no appreciable differences across age strata. Among 12-to-17-year-old newly incident drinkers, there is a female excess in the rapid transition to alcohol dependence; a male excess is observed among young adult newly incident drinkers. Evaluated cohort-wise, using an epidemiological mutoscope view, individual cohorts show a congruent pattern, with age at first drink held constant.
Conclusions
Studying multiple replication samples of young newly incident drinkers, we discovered a clear female excess in the risk of a rapid transition from first full drink to alcohol dependence among adolescents, with age patterns differing across males and females.
Keywords: Alcohol Dependence, Adolescents, United States, Male-Female Difference
1. Introduction
Alcohol dependence (AD) causes substantial health and social burdens. Rapid-onset AD occurring soon after the first drink is a marker for what may become a chronically disabling condition, and is linked to adverse physical, mental, and socioeconomic consequences (Schuckit, 2009). Rapid-onset AD can be seen as early as childhood, and might be termed ‘early rapid-onset AD’ when seen before the early adolescent years, in which case there would be concern about permanent brain, behavioral, and social adaptational changes, with potentially exacerbated adverse consequences (Hall et al., 2016; Schuckit, 2009).
There are a growing number of population-based studies on the transition from drinking to alcohol dependence. For example, in the classic longitudinal Lundby Sweden study, an estimated 4% of the initial cohort developed an alcohol related disorder over a course of 15 years (Ojesjo et al., 2000). More recent estimates from two benchmark cross-sectional studies in the United States (US) found that 14–23% of adult drinkers developed alcohol dependence within a span of ten years after their first drink, and 1–2% did so during the first two years (Anthony and Petronis, 1995; Lopez-Quintero et al., 2011; Wagner and Anthony, 2002, 2007). Estimates published by Anthony and Petronis (1995), as well as Behrendt et al. (2009), draw attention to the importance of ‘time since first drink’ or other drug use when estimating transition probabilities of this type.
Several prior studies with US adult population samples suggest that earlier-onset drinking is linked to greater AD transition probabilities (Dawson et al., 2008; Grant and Dawson, 1997; Grant et al., 2001; Reardon and Buka, 2002). To illustrate, Dawson and colleagues (2008) found a three-fold increase in the risk of developing alcohol dependence among individuals with early-adolescent-onset drinking compared to adult-onset drinkers. Nonetheless, these US studies generally show that a large proportion of drinkers have taken their first drink before the 18th birthday. Therefore, these studies have to rely heavily upon long-term memories about ages of first drink and first problem. The result is a limited capacity to produce age-specific estimates; recall bias possibilities are prominent, tend to be proportionate to the elapsed time interval from first drink to survey assessment, and often are described as ‘telescoping’ problems in the general survey research methods literature (Brown et al., 2009; Cheng et al., 2016a; Shillington et al., 2012).
If the goal is to avoid methods problems of this type, there are two common remedies. One remedy is longitudinal research with short between-assessment intervals, as illustrated in Behrendt and colleagues (2009). Studying young people in Germany, they found evidence suggesting a modestly greater risk of developing alcohol dependence within the first two years of drinking among early-onset drinkers as compared to those who started drinking after age 13 (Behrendt et al., 2009). The other remedy is cross-sectional research with large samples of newly incident drinkers and with AD assessment relatively quickly after drinking starts, irrespective of drinking onset age (Vsevolozhskaya and Anthony, 2015).
With respect to male-female differences in AD risk, surveys of adults have disclosed a consistent male excess in the prevalence of alcohol dependence and a higher transition probability from use to dependence (Keyes et al., 2008; Keyes et al., 2011; Keyes et al., 2010; Kuntsche et al., 2015; Wagner and Anthony, 2007). A male excess risk for transitioning from first drink to alcohol dependence also was found in the German longitudinal research project that is noteworthy for its avoidance of the methodological ‘telescoping’ problem just mentioned (Wittchen et al., 2008). In contrast, using multiparametric Hill functions, Vsevolozhskaya and Anthony turned to the large sample remedy and found a null male excess in the transition from use to dependence, holding constant frequencies of use among all newly incident drinkers (Vsevolozhskaya and Anthony, 2015).
Many disciplines have theories and evidence pertinent to the consistently documented male excess in alcohol dependence. From biology, toxicology, and medical sciences, these theories and evidence stress neurocognitive differences, ethanol metabolism and other forms of biotransformation, as well as hormonal differences affecting sensitivity to alcohol. From the behavioral and social sciences, emphasis has been given to sex-differentiated social roles which can promote male drinking and stigmatize female drinking (Kuhn, 2015; Schulte et al., 2009). Despite the complex interplay of determining influences of this type, evidence from multi-country studies tends to support a major influence of socioenvironmental conditions and processes (Rahav et al., 2006; Wilsnack et al., 2009). In this context, we also note that male-female differences in alcohol drinking can vary across developmental stages as individuals experience pubertal and other biological changes, concurrent with acquisition of new social roles during adolescence. A small but growing epidemiological body of evidence from studies of adolescents tends to show smaller, and sometimes null, male-female differences in prevalence estimates for drinking-related outcomes, which can be set against the larger body of adult population evidence about the male excess in these outcomes (Schulte et al., 2009; White et al., 2015).
In a recent study, our research team documented a female excess in the risk of becoming a new drinker among adolescents; this female excess is not present in adults (Cheng et al., 2016b). A previous study found null male-female differences in the cumulative incidence of alcohol dependence before the age of 18, and a male excess afterwards (Young et al., 2002). Nonetheless, cumulative incidence in all individuals conveys little information about the transition from use to dependence. In this context, a sex-specific estimate in the estimated probability of making a rapid transition from first full drink to AD across different developmental stages is a fundamental but currently missing piece of epidemiologic evidence in contemporary alcohol research.
This gap in evidence led our research group to specify a major research aim for epidemiological field survey research – namely, to estimate sex-specific rapid transition probabilities that lead from drinking onset toward alcohol dependence across developmental stages among 12-to-25-year-old newly incident drinkers in the United States. Based on findings from previous prevalence-oriented surveys, we posited a male excess in the rapid transition from drinking to alcohol dependence across all developmental stages, with a smaller male excess among adolescents compared to adults. In these estimates, a tight focus on the period just prior to survey assessment helps constrain ‘telescoping’ and other errors already noted. As might be compared with corresponding longitudinal studies, the use of cross-sectional national surveys constrains potential biases due to attrition (sample losses over time) and to response reactivity (Cheng et al., 2016a).
2. Materials and Methods
2.1 Study Population and Sample
The study population is that of the US National Surveys on Drug Use and Health (NSDUH), conducted each year from 2002 through 2013. Originating with a sampling frame that encompasses all 50 States and the District of Columbia, the NSDUH multi-stage probability sampling plan sought a nationally representative sample of non-institutionalized community residents of the US aged 12 years and above, with oversampling of 12-to-17-year-olds. In contrast to school or household surveys of adolescents, the NSDUH sample includes young people irrespective of school attendance, and its sampling frame includes non-household group quarters such as homeless shelters and college dormitories. All NSDUH participants were recruited via child assent and parental or adult consent, based upon protocols approved by cognizant human subjects protection committees (United States, 2012). More than 30,000 12-to-25-year-old participants are included in each year’s NSDUH sample (United States, 2012).
2.2 Assessment and measures
In general, most often within the participant’s home, NSDUH assessments have been completed as confidential audio computer-assisted self-interviews (ACASI) designed to promote reliability, accuracy, and truthfulness of participant reports about potentially sensitive behaviors and characteristics. During the assessment, each participant has been asked about the history of drinking experiences, including questions for newly incident drinkers about the month and year when the first full drink was consumed.
The key response variable in this study is alcohol dependence based on diagnostic criteria of the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association, 1994). It was measured via ACASI questions about the seven clinical features of DSM-IV alcohol dependence. Alcohol dependence (AD) cases were newly incident users with dependence manifestations characterized by at least some persistence of use and at least three DSM-IV-aligned AD clinical features observed during the 12 months prior to assessment.
Age and age at first full drink have been derived via self-reports (e.g., date of birth relative to assessment date). Sex is based on participant responses that indicate male or female (with no allowance for gender identities such as trans-gender). NSDUH drew upon dwelling unit roster information to create variables for age and sex when survey items were skipped.
For this study’s primary estimates, the newly incident drinkers are those who took their first full drink during the 12 months prior to the NSDUH assessment. Due to concerns about confidentiality, the exact date of assessment is not disclosed in the publicly downloadable datasets, but the quarter of the year is available. On this basis, it was possible to identify a subgroup of newly incident drinkers who had initiated drinking within the four quarters prior to assessment, and who had taken at least one drink during the past 12 months (n = 32,562 12-to-25-year-olds). Supplementary Table S1 provides a description of sample sizes for each sex- and age-group, based on this ’12-month’ approach.
In some prior research, the process of ascertaining newly incident users did not have the benefit of survey assessments about the month of first use. Instead, users with recent onsets were identified using a ‘24-month approach’ in place of the ‘12-month approach’ just described. In subsidiary analyses intended to produce approximations of an ‘annual incidence rate’ with a denominator of roughly 12 person-months, and in order to be consistent with the prior approach (e.g., Barondess et al., 2010), we applied the previously developed ‘24-month’ approach and identified the ever-users (1) whose age at first use was equal to the age at the time of assessment, or no more than one year different from the age of assessment, and included all of them in the denominators for our estimated transition probabilities. As described in a previous study, this ‘24-month’ approach is one that includes some newly incident users who started as long as 23–24 months prior to dependence assessment, as well as those with no more than 1–2 months between the first use and that assessment, with an expectation (based on life table principles) that the elapsed time from the first full drink until AD assessment should be roughly 12 months, as is the case for ‘annual incidence rate’ estimates (Barondess et al., 2010).
A careful study of the ‘24-month approach’ and its use in prior research will disclose that has a sensitivity limitation because it will fail to detect cases that originated with a ’rapid-onset-and-rapid-offset’ profile. A hypothetical case example would be an early teen user who quickly gets into trouble as AD forms, and whose vigilant family mobilizes for an almost immediate entry into an effective treatment intervention followed by no more persistence of use and no AD clinical features observed during the 12 months prior to assessment. We return to this ’sensitivity’ problem in Section 4 as well as online supplementary material which provides details about this approach and the assessment of assumptions (section S2).
2.3 Analysis
Analyses are based on the age at the first full drink. In initial analyses, we used the ’12-month approach’ with the same configuration of age-of-onset groups as in the Dawson et al. study (2008) and estimated the transition probability from first drink to alcohol dependence among newly incident drinkers for three groups based on their age of drinking onset: 12–14, 15–17, and 18–25 years. For this primary analysis, transition probability was conceptualized with an analysis-weighted numerator consisting of alcohol dependence cases arising from an analysis-weighted denominator of newly incident drinkers who had their first drink, all events occurring within 12 months of the assessment date. Next, guided by an alternative conceptual model that the risks of developing alcohol dependence differ across four subgroups (i.e., adolescents, underage adult drinkers, law-abiding individuals who have their first drink at 21 years, and those with post-21 drinking onset), we estimated transition probabilities for these four age-of-onset groups.
The resulting estimates in this work make use of NSDUH analysis weights that account for sample selection probabilities and post-stratification adjustment factors to replicate the US Census subpopulation counts. To ensure reasonable precision of the estimates, we combined survey years into year-pairs. Results are presented in tables with year-pair and age-groups as rows and columns. Therefore, row-wise, the table cells depict age patterns; column-wise, the table cells show the consistency of estimates. In the age-pair and year-pair aligned table, The mutoscope view is gained by reading the same table cells down the diagonals in evaluation of whether cohort-specific patterns are congruent with age-specific patterns (Cheng and Anthony, 2016; Cheng et al., 2016a, b; Seedall and Anthony, 2015). Standard errors and 95% confidence intervals (CI) are from complex survey delta methods.
Next, logarithms were taken and meta-analysis summaries of age-group-specific estimates were derived, with each NSDUH year-pair treated as an independent replication (Deandrea et al., 2013; DerSimonian and Laird, 1986). The Cochran’s Q and I2 statistics have been used to evaluate heterogeneity across replications (DerSimonian and Laird, 1986; Higgins et al., 2003). When heterogeneity across replications was observed (i.e., Cochran’s Q chi-squared test p<0.05 and I2>50%), a random effects estimator has been substituted for the default fixed effect estimator. Whereas the short period from 2002–2013 impedes formal statistical evaluation of age-period-cohort effects, we turned to a constrained regression approach, and constrained the 2010–2011 and 2012–2013 period values to be equal, in a post-estimation confirmation of our assumption about null period-related changes (Cheng et al., 2016a; Harper, 2015). Technical details about the meta-analysis and constrained regression age-period-cohort analysis are discussed in a previous publication (Cheng et al., 2016a).
3. Results
Meta-analytic summary estimates are presented in Figure 1. Rapid transition from drinking to alcohol dependence occurs in less than 4% of 12–25 adolescent and young adult newly incident drinkers. The two ways of categorization produced consistent patterns. In females, adolescent-onset drinkers are at a higher risk of transitioning to alcohol dependence compared to adult-onset drinkers; in males, the transition probability does not vary appreciably across age at first drink. Table 1 presents point estimates and 95% confidence intervals for each year-pair. Age-group-specific meta-analysis summary estimates are shown at the bottom of each panel. Estimates are fairly consistent across year-pairs.
Figure 1.
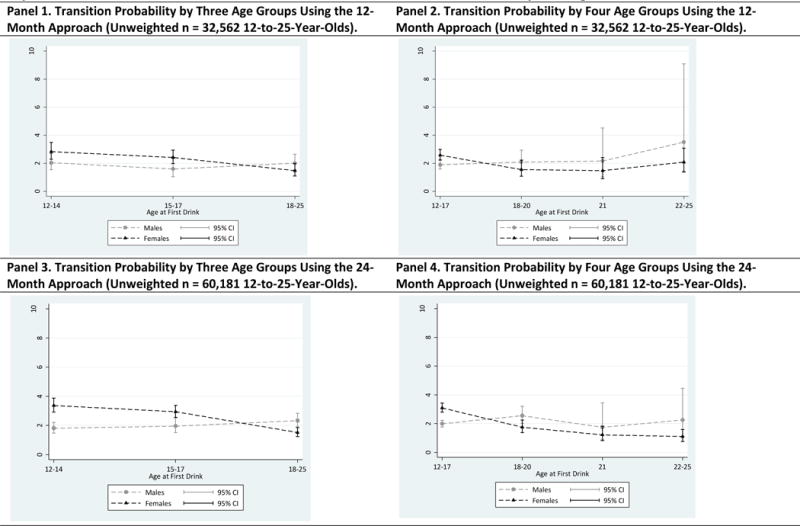
Comparison of Meta-Analytic Summary Estimates for Sex-Specific Probability (%) of Transitioning From 1st Drink to DSM-IV Alcohol Dependence Within 12 or 24 Months After 1st Drink. Data From United States National Surveys on Drug Use and Health, 2002–2013.
Note: Meta-analysis summary estimates with each year-pair treated as an independent replication using a fixed-effect estimator. For 21-year-old males in 4-age-group analysis, heterogeneity across replications motivated use of the random effects variance estimation approach. For 24-month transition probability, only those who had their 1st drink at the current age or one year younger were included. Therefore, the estimated transition probability may be an under-estimate of the actual transition probability. Please see the Methods and Discussion sections for details on this issue.
Table 1.
Sex-, Cohort-, and Time-Specific Estimates for Rapid Transition From Drinking to DSM-IV Alcohol Dependence (%, 95% CI) Within 12 Months After the 1st Full Drink per Year-Pair Among Newly Incident Drinkers. Data From the United States National Survey on Drug Use and Health, 2002–2013 (Unweighted n=32,562 12–25 Year Olds)a
| Panel A. Females by Three Age Groups | Panel B. Females by Four Age Groups | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Age at First Drink | 12–14 | 15–17 | 18–25 | 12–17 | 18–20 | 21 | 22–25 |
| Year-Pair | |||||||
| 2002–2003 | 3 (2,5) | 3 (2,4) | 2 (1,3) | 3 (2,4) | 2 (1,4) | 1 (>0,4) | 2 (>0,8) |
| 2004–2005 | 2 (1,3) | 2 (1,3) | 2 (1,4) | 2 (1,3) | 3 (1,6) | 1 (>0,3) | 2 (>0,14) |
| 2006–2007 | 3 (2,5) | 3 (2,5) | 1 (>0,2) | 3 (2,5) | 1 (>0,2) | 2 (>0,7) | 0 (.,.) |
| 2008–2009 | 3 (2,4) | 3 (2,6) | 1 (>0,1) | 3 (2,5) | <1 (>0,2) | 1 (>0,3) | 0 (.,.) |
| 2010–2011 | 3 (2,6) | 2 (1,3) | 2 (1,3) | 2 (2,3) | 1 (1,4) | 2 (1,7) | 2 (1,3) |
| 2012–2013 | 4 (2,6) | 2 (1,3) | 2 (1,3) | 2 (1,4) | 2 (1,4) | 2 (1,5) | 0 (.,.) |
|
| |||||||
| Meta-Analysis Estimateb | 3 (2,3) | 2 (2,3) | 1 (1,2) | 3 (2,3) | 2 (1,2) | 1 (1,2) | 2 (1,3) |
|
| |||||||
| Panel C. Males by Three Age Groups | Panel D. Males by Four Age Groups | ||||||
|
| |||||||
| 2002–2003 | 2 (1,3) | 4 (2,5) | 3 (1,4) | 3 (2,4) | 2 (1,5) | 4 (1,12) | 0 (.,.) |
| 2004–2005 | 2 (1,4) | 2 (1,3) | 2 (1,4) | 2 (1,3) | 2 (1,5) | 0 (.,.) | <1 (.,.) |
| 2006–2007 | 2 (1,4) | 2 (1,3) | 3 (1,6) | 2 (1,3) | 3 (1,6) | 2 (>0,8) | 5 (1,20) |
| 2008–2009 | 2 (1,4) | 1 (>0,2) | 2 (1,5) | 1 (1,2) | 2 (1,5) | 5 (2,12) | <1 (.,.) |
| 2010–2011 | 3 (1,5) | 1 (1,3) | 1 (1,2) | 2 (1,3) | 1 (1,3) | 1 (>0,2) | 4 (>0,22) |
| 2012–2013 | 2 (1,4) | 1 (>0,2) | 2 (1,3) | 1 (1,2) | 2 (1,5) | 2 (1,4) | 2 (>0,12) |
|
| |||||||
| Meta-Analysis Estimateb | 2 (2,3) | 2 (1,2) | 2 (2,3) | 2 (2,2) | 2 (1,3) | 2 (1,5) | 3 (1,9) |
DSM-IV, American Psychiatric Association Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition.
Meta-analysis summary estimates with each year-pair treated as an independent replication. For 21-year old males, heterogeneity across replications motivated use of the random effects variance estimation approach.
The most interesting finding may be that the transition probability tends to be higher among female adolescent-onset drinkers compared to their male counterparts. For example, girls who initiate drinking at 12–17 are approximately 1.5 times as likely to rapidly transition to alcohol dependence as compared to boys who had their first drink at the same age, although we note that the confidence intervals touch (Panel 2 of Figure 1). Afterwards, the point estimates suggest a male excess, but the confidence intervals overlap.
The female excess in adolescent-onset drinkers becomes more prominent when we shift from the ’12-month’ approach to the ‘24-month’ approach (Table 2 and Figure 1). Among adult-onset newly incident drinkers, males are more likely to make a rapid transition to alcohol dependence compared to female counterparts (Panel 3 of Figure 1). As shown in Panel 3 and 4 of Figure 1, the ‘24-month’ approach shows age-of-onset patterns for the rapid transition from the time of first full drink to alcohol dependence that are similar to those obtained using the ’12-month’ approach.
Table 2.
Sex-, Cohort-, and Time-Specific Estimates for Rapid Transition From Drinking to DSM-IV Alcohol Dependence (%, 95% CI) Within 24 Months After the 1st Full Drink per Year-Pair Among Newly Incident Drinkers. Data From the United States National Survey on Drug Use and Health, 2002–2013 (Unweighted n=60,181 12–25 Year Olds)a
| Panel A. Females by Three Age Groups | Panel B. Females by Four Age Groups | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Age at First Drink | 12–14 | 15–17 | 18–25 | 12–17 | 18–20 | 21 | 22–25 |
| Year-Pair | |||||||
| 2002–2003 | 3 (2,4) | 3 (2,4) | 2 (1,3) | 3 (2,4) | 2 (1,3) | 1 (>0,4) | 2 (1,6) |
| 2004–2005 | 3 (2,4) | 3 (2,4) | 2 (1,3) | 3 (2,4) | 2 (1,4) | 1 (>0,2) | 1 (>0,7) |
| 2006–2007 | 4 (3,5) | 4 (3,5) | 1 (1,2) | 4 (3,5) | 1 (1,3) | 1 (>0,4) | 0 (.,.) |
| 2008–2009 | 3 (2,5) | 3 (2,4) | 1 (1,2) | 3 (3,4) | 2 (1,3) | 1 (>0,3) | 1 (>0,4) |
| 2010–2011 | 4 (2,5) | 2 (2,3) | 1 (1,2) | 3 (2,4) | 1 (1,3) | 2 (1,4) | 1 (1,2) |
| 2012–2013 | 4 (3,6) | 2 (1,4) | 2 (1,3) | 3 (2,4) | 2 (1,3) | 1 (1,3) | 1 (0,6) |
|
| |||||||
| Meta-Analysis Estimateb | 3 (3,4) | 3 (3,3) | 2 (1,2) | 3 (3,3) | 2 (1,2) | 1 (1,2) | 1 (1,2) |
|
| |||||||
| Panel C. Males by Three Age Groups | Panel D. Males by Four Age Groups | ||||||
|
| |||||||
| 2002–2003 | 2 (1,3) | 3 (2,4) | 2 (1,3) | 3 (2,3) | 2 (1,4) | 3 (1,7) | 0 (.,.) |
| 2004–2005 | 2 (1,3) | 2 (1,2) | 2 (1,4) | 2 (2,3) | 3 (2,5) | 0 (.,.) | 1 (>0,8) |
| 2006–2007 | 2 (1,3) | 3 (2,4) | 3 (2,5) | 2 (2,3) | 3 (2,6) | 3 (1,6) | 4 (1,14) |
| 2008–2009 | 2 (1,3) | 1 (1,2) | 3 (2,5) | 2 (1,2) | 3 (1,5) | 4 (2,8) | 1 (>0,7) |
| 2010–2011 | 2 (1,3) | 2 (1,2) | 2 (1,3) | 2 (1,2) | 2 (1,3) | 2 (>0,5) | 3 (1,11) |
| 2012–2013 | 1 (1,2) | 2 (1,2) | 2 (1,3) | 1 (1,2) | 2 (1,4) | 2 (1,3) | 1 (>0,7) |
|
| |||||||
| Meta-Analysis Estimateb | 2 (1,2) | 2 (2,3) | 2 (2,3) | 2 (2,2) | 3 (2,3) | 2 (1,3) | 2 (1,4) |
DSM-IV, American Psychiatric Association Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition. For 24-month transition probability, only those who had their 1st drink at the current age or one year younger were included. Therefore, the estimated transition probability may be an under-estimate of the actual transition probability. Please see the Methods and Discussion sections for details on this issue.
Meta-analysis summary estimates with each year-pair treated as an independent replication. For 21-year old males, heterogeneity across replications motivated use of the random effects variance estimation approach.
More fine grained age-pair estimates are presented in Figure 2. Point estimates suggest female excess for all age-pairs during adolescence, but there are overlapping confidence intervals for those who had their first full drink at age 12 to 15. For those who had their first full drink at age 16 or 17, there is a robust female excess. Age-pair and year-pair aligned results are presented in Table 3. For females, the age view (row by row) and the cohort view (diagonals) reveal congruent patterns with the one from meta-analytic estimates (i.e., a monotonic decrease in the rapid transition from drinking to alcohol dependence with age at first drink). Among males, neither the age view nor the cohort view show appreciable differences across ages at first full drink.
Figure 2.
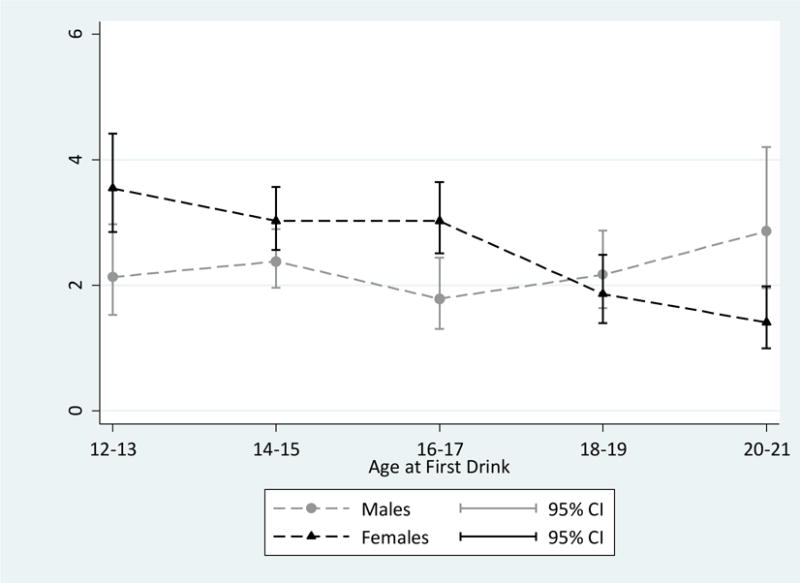
Comparison of Meta-Analytic Summary Estimates for Sex-Specific Probability (%) of Transitioning From 1st Drink to DSM-IV Alcohol Dependence Within 24 Months After 1st Drink per Age Pair. Data From United States National Surveys on Drug Use and Health, 2002–2013 (Unweighted n = 60,181 12-to-25-Year-Olds).
Note: Meta-analysis summary estimates with each year-pair treated as an independent replication using a fixed-effect estimator. For 16–17 and 20–21 year old males, heterogeneity across replications motivated use of the random effects variance estimation approach. Estimates for 22–23 and 24–25 year olds are presented in Table 1 and 2 but not in Figure 2 due to low precision of estimates. For 24-month transition probability, only those who had their 1st drink at the current age or one year younger were included. Therefore, the estimated transition probability may be an under-estimate of the actual transition probability. Please see the Methods and Discussion sections for details on this issue.
Table 3.
Sex-, Cohort-, and Time-Specific Estimates for Rapid Transition From Drinking to DSM-IV Alcohol Dependence (%) Within 24 Months After 1st Full Drink per Age- and Year-Pair Among Newly Incident Drinkers. Data From the United States National Survey on Drug Use and Health, 2002–2013 (Unweighted n=60,181 12–25 Year Olds)a
| Panel A. Females | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Age at First Drink | 12–13 | 14–15 | 16–17 | 18–19 | 20–21 | 22–23 | 24–25 |
| Year-Pair | |||||||
| 2002–2003 | 3 (2,4) | 3 (2,4) | 3 (2,4) | 2 (1,4) | 1 (>0,3) | 3 (1,8) | 0 (.,.) |
| 2004–2005 | 3 (2,6) | 3 (2,4) | 3 (2,4) | 3 (1,5) | 1 (>0,3) | 2 (>0,12) | 0 (.,.) |
| 2006–2007 | 5 (3,8) | 5 (3,7) | 3 (2,5) | 1 (1,3) | 1 (>0,3) | 0 (.,.) | 0 (.,.) |
| 2008–2009 | 3 (2,5) | 3 (2,4) | 4 (2,6) | 2 (1,3) | 2 (1,4) | 1 (>0,7) | 0 (.,.) |
| 2010–2011 | 4 (2,8) | 3 (1,4) | 3 (2,4) | 2 (1,4) | 1 (1,4) | 2 (1,3) | 0 (.,.) |
| 2012–2013 | 4 (2,8) | 2 (1,4) | 3 (1,6) | 2 (1,4) | 1 (1,3) | 0 (.,.) | 0 (.,.) |
|
| |||||||
| Meta-Analysis Estimateb | 4 (3, 4) | 4 (3,4) | 4 (3,4) | 2 (1,2) | 1 (1,2) | 1 (1,3) | 0 (.,.) |
| Panel B. Males | |||||||
|---|---|---|---|---|---|---|---|
| 2002–2003 | 2 (1,5) | 2 (1,4) | 3 (2,5) | 2 (1,3) | 4 (2,7) | 0 (.,.) | 0 (.,.) |
| 2004–2005 | 2 (1,6) | 2 (1,3) | 2 (1,3) | 2 (1,4) | 2 (>0,6) | 2 (>0,13) | 0 (.,.) |
| 2006–2007 | 2 (1,3) | 4 (2,5) | 2 (1,3) | 3 (1,5) | 5 (2,8) | 8 (2,25) | 0 (.,.) |
| 2008–2009 | 3 (1,6) | 2 (1,3) | 1 (1,2) | 2 (1,5) | 4 (2,8) | 2 (>0,11) | 0 (.,.) |
| 2010–2011 | 2 (1,6) | 3 (2,4) | 1 (<1,2) | 2 (1,4) | 1 (>0,4) | 4 (>0,22) | 0 (.,.) |
| 2012–2013 | 2 (1,4) | 1 (1,4) | 2 (1,3) | 2 (1,5) | 2 (1,3) | 2 (>0,11) | 0 (.,.) |
|
| |||||||
| Meta-Analysis Estimateb | 2 (2, 3) | 2 (2, 3) | 2 (1, 2) | 2 (2, 3) | 3 (2, 4) | 4 (2, 8) | 0 (.,.) |
Cells with the same shade trace the experience of individual cohort-pairs. DSM-IV, American Psychiatric Association Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition. For 24-month transition probability, only those who had their 1st drink at the current age or one year younger were included. Therefore, the estimated transition probability may be an under-estimate of the actual transition probability. Please see the Methods and Discussion sections for more discussion on this issue.
Meta-analysis summary estimates with each year-pair treated as an independent replication. For 16–17 and 20–21 year old males, heterogeneity across replications motivated use of the random effects variance estimation approach.
The constrained regression models confirmed our assumption of no tangible ‘period effects’ in either set of estimates. With age and period ‘effects’ held constant, the estimated ‘cohort effects’ were null.
4. Discussion
In this study, we estimated incidence rates from nationally representative samples of young people (including an approximation of annual incidence rates). Our results suggest that an alcohol dependence syndrome can develop quite rapidly after the first full drink. The AD syndrome affects an estimated 2% to 4% of 12-to-17-year-olds in the US within 24 months after drinking onset. These estimates for young people who start drinking are not appreciably different from corresponding AD hazard rates estimated for 15-to-64-year-olds during the first 1–2 years after the first drink (Wagner and Anthony, 2002).
Perhaps the most interesting finding in this study’s consideration of male-female differences is an apparently modest female excess in the rapid transition from drinking to alcohol dependence among adolescent newly incident drinkers. It also is of interest that we are seeing no marked onset-age-related variation in the rapid transition from drinking to dependence among males. These findings may run counter to widely held beliefs about male excess risk, as well as ‘early-onset-associated risk’ such that delaying first drink to the legal minimum drinking age should reduce risk of problems such as alcohol dependence. We note, however, that most evidence on these topics is from studies of adult samples and relatively long spans of recall and reporting (DeJong and Blanchette, 2014; Pitts et al., 2014; Wechsler and Nelson, 2010), with a few longitudinal exceptions (e.g., Behrendt et al., 2009). Of course, one explanation for this study’s ‘onset-risk’ patterns might be that a 12–24 month interval after the first full drink is too short a time to discover the excess risk observed by others. For example, a life table analysis showed no ‘early-onset-associated’ excess risk of the first drug problem during the first 1–5 years after first drug use, but did find an excess risk pattern that emerged 6–7 years after first drug use (Anthony and Petronis, 1995).
Several of the more important study limitations merit attention. The NSDUH self-report assessment has shown generally good measurement properties (United States, 2012), but we remind our readers about the ‘sensitivity’ problem mentioned in Section 2 in relation to the ‘24-month’ approach used to estimate ‘annual incidence’ of AD after the first full drink. In the supplementary material, we present several approaches to assess potential bias due to this ‘sensitivity’ issue and we did not find evidence for substantial age-related bias. On one hand, in future research, it should be possible to estimate the degree to which this study’s observed early female excess in rapid-onset AD can be traced back to AD-affected female teens being accelerated into effective treatment services versus possible treatment admission delays for AD-affected male teens. This same ‘sensitivity’ problem may help explain why the male age-specific pattern of risk is relatively flat across the years of adolescence. On the other hand, the just-mentioned female excess risk and the relatively flat male risk pattern also can be seen in estimates from the ’12-month’ approach, whereas this ‘sensitivity’ problem is not present. We also must acknowledge the possibility of a ’rapid-onset-rapid-remission’ sequence for some unknown number of newly incident drinkers. This might occur when a very young drinker’s problems come to attention with clinical intervention that effectively terminates or ameliorates the alcohol problems so fast that they are not detected in the NSDUH assessment. Our estimates for the frequency of these ’rapid-onset-rapid-remit’ cases are presented in an online supplement (Section S2).
Important study strengths include its meta-analysis approach, with multiple independent replications used to ensure reproducibility. In addition, the research approach (e.g., with a focus on newly incident drinkers) helps constrain two major sources of information bias: long-term recall telescoping and measurement reactivity (Cheng et al., 2016a; Shillington and Clapp, 2000; Shillington et al., 2012).
If study strengths counterbalance weaknesses of the type just mentioned, an initial point of discussion might be a possibility that youthful alcohol dependence may reflect poor decision-making more than loss of control over alcohol (Dawson et al., 2008; Hooper et al., 2004), and perhaps can be traced to greater impulsivity among adolescents generally (Dougherty et al., 2015; Steinberg et al., 2008). If so, age-appropriate interventions with focus upon decision-making might be important for all underage drinkers, especially when rapid-onset alcohol dependence problems become apparent. Surveillance of otherwise ignored precocious drinking by parents, other adults, and pediatricians can be strengthened, barriers to early treatment can be reduced, and waiting lists for adolescent alcohol treatment services can be eliminated.
Adolescence is the key period to gain social skills and form gender roles. Parents, teachers, and peers play differential roles in early-, mid-, and late-adolescence (Schulte et al., 2009). Despite the current incomplete understanding of mechanisms for adolescent alcohol drinking, alcohol can induce general changes to the adolescent brain, which in turn may increase the susceptibility to alcohol dependence (Crews et al., 2007). Therefore, future studies should consider the interacting roles of parental monitoring, peer affiliation, exposure to alcohol advertisement, general psychopathology, genetic vulnerability, and drinking motives (which may be different for males versus females and for earlier- versus later-onset drinkers) in order to provide the most effective interventions for girls and boys.
5. Conclusions
Studying multiple replication samples of young newly incident drinkers, we discovered that roughly 2% to 4% of young newly incident drinkers show rapid-onset alcohol dependence – i.e., at a rate that is not too different from corresponding rates for 15-to-64-year-old drinkers observed 1–2 years after first drink. There is an apparently modest female excess in the risk of rapid transition from first full drink to alcohol dependence among adolescents, with age patterns differing across males and females.
Supplementary Material
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-IV. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug Alcohol Depend. 1995;40:9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]
- Barondess DA, Meyer EM, Boinapally PM, Fairman B, Anthony JC. Epidemiological evidence on count processes in the formation of tobacco dependence. Nicotine Tob Res. 2010;12:734–741. doi: 10.1093/ntr/ntq073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrendt S, Wittchen HU, Hofler M, Lieb R, Beesdo K. Transitions from first substance use to substance use disorders in adolescence: is early onset associated with a rapid escalation? Drug Alcohol Depend. 2009;99:68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, Martin C, Chung T, Tapert SF, Sher K, Winters KC, Lowman C, Murphy S. Underage alcohol use: summary of developmental processes and mechanisms: ages 16–20. Alcohol Res Health. 2009;32:41–52. [PMC free article] [PubMed] [Google Scholar]
- Cheng HG, Anthony JC. Does our legal minimum drinking age modulate risk of first heavy drinking episode soon after drinking onset? Epidemiological evidence for the United States, 2006–2014. PeerJ. 2016;4:e2153. doi: 10.7717/peerj.2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng HG, Cantave MD, Anthony JC. Alcohol Experiences Viewed Mutoscopically: Newly Incident Drinking of Twelve- to Twenty-Five-Year-Olds in the United States, 2002–2013. J Stud Alcohol Drugs. 2016a;77:405–412. doi: 10.15288/jsad.2016.77.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng HG, Cantave MD, Anthony JC. Taking the first full drink: Epidemiological evidence on male-female differences in the United States. Alcohol Clin Exp Res. 2016b;40:816–825. doi: 10.1111/acer.13028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86:189–199. doi: 10.1016/j.pbb.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Chou SP, Ruan WJ, Grant BF. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcohol Clin Exp Res. 2008;32:2149–2160. doi: 10.1111/j.1530-0277.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deandrea DC, Troost JP, Anthony JC. Toward primary prevention of extra-medical OxyContin(R) use among young people. Prev Med. 2013;57:244–246. doi: 10.1016/j.ypmed.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeJong W, Blanchette J. Case closed: research evidence on the positive public health impact of the age 21 minimum legal drinking age in the United States. J Stud Alcohol Drugs Suppl. 2014;75(Suppl 17):108–115. doi: 10.15288/jsads.2014.s17.108. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Lake SL, Mathias CW, Ryan SR, Bray BC, Charles NE, Acheson A. Behavioral Impulsivity and Risk-Taking Trajectories Across Early Adolescence in Youths With and Without Family Histories of Alcohol and Other Drug Use Disorders. Alcohol Clin Exp Res. 2015;39:1501–1509. doi: 10.1111/acer.12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Harford TC. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: a 12-year follow-up. J Subst Abuse. 2001;13:493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- Hall WD, Patton G, Stockings E, Weier M, Lynskey M, Morley KI, Degenhardt L. Why young people’s substance use matters for global health. Lancet Psychiatry. 2016;3:265–279. doi: 10.1016/S2215-0366(16)00013-4. [DOI] [PubMed] [Google Scholar]
- Harper S. Invited Commentary: A-P-C … It’s Easy as 1-2-3! Am J Epidemiol. 2015;182:313–317. doi: 10.1093/aje/kwv052. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper CJ, Luciana M, Conklin HM, Yarger RS. Adolescents’ performance on the Iowa Gambling Task: implications for the development of decision making and ventromedial prefrontal cortex. Dev Psychol. 2004;40:1148–1158. doi: 10.1037/0012-1649.40.6.1148. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: a review and synthesis. Alcohol Clin Exp Res. 2011;35:2101–2112. doi: 10.1111/j.1530-0277.2011.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Martins SS, Blanco C, Hasin DS. Telescoping and gender differences in alcohol dependence: new evidence from two national surveys. Am J Psychiatry. 2010;167:969–976. doi: 10.1176/appi.ajp.2009.09081161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn C. Emergence of sex differences in the development of substance use and abuse during adolescence. Pharmacol Ther. 2015;153:55–78. doi: 10.1016/j.pharmthera.2015.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Wicki M, Windlin B, Roberts C, Gabhainn SN, van der Sluijs W, Aasvee K, Gaspar de Matos M, Dankulincova Z, Hublet A, Tynjala J, Valimaa R, Bendtsen P, Vieno A, Mazur J, Farkas J, Demetrovics Z. Drinking motives mediate cultural differences but not gender differences in adolescent alcohol use. J Adolesc Health. 2015;56:323–329. doi: 10.1016/j.jadohealth.2014.10.267. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Perez de los Cobos J, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2011;115:120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojesjo L, Hagnell O, Otterbeck L. The course of alcoholism among men in the Lundby Longitudinal Study, Sweden. J Stud Alcohol. 2000;61:320–322. doi: 10.15288/jsa.2000.61.320. [DOI] [PubMed] [Google Scholar]
- Pitts JR, Johnson ID, Eidson JL. Keeping the case open: responding to DeJong and Blanchette’s “Case closed” on the minimum legal drinking age in the United States. J Stud Alcohol Drugs. 2014;75:1047–1049. doi: 10.15288/jsad.2014.75.1047. [DOI] [PubMed] [Google Scholar]
- Rahav G, Wilsnack R, Bloomfield K, Gmel G, Kuntsche S. The influence of societal level factors on men’s and women’s alcohol consumption and alcohol problems. Alcohol Alcohol Suppl. 2006;41:i47–55. doi: 10.1093/alcalc/agl075. [DOI] [PubMed] [Google Scholar]
- Reardon SF, Buka SL. Differences in onset and persistence of substance abuse and dependence among whites, blacks, and Hispanics. Public Health Rep. 2002;117(Suppl 1):S51–59. [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA. Alcohol-use disorders. Lancet. 2009;373:492–501. doi: 10.1016/S0140-6736(09)60009-X. [DOI] [PubMed] [Google Scholar]
- Schulte MT, Ramo D, Brown SA. Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clin Psychol Rev. 2009;29:535–547. doi: 10.1016/j.cpr.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedall RB, Anthony JC. Monitoring by Parents and Hypothesized Male-Female Differences in Evidence from a Nationally Representative Cohort Re-sampled from Age 12 to 17 Years: An Exploratory Study Using a “Mutoscope” Approach. Prev Sci. 2015;16:696–706. doi: 10.1007/s11121-014-0517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shillington AM, Clapp JD. Self-report stability of adolescent substance use: are there differences for gender, ethnicity and age? Drug Alcohol Depend. 2000;60:19–27. doi: 10.1016/s0376-8716(99)00137-4. [DOI] [PubMed] [Google Scholar]
- Shillington AM, Woodruff SI, Clapp JD, Reed MB, Lemus H. Self-Reported Age of Onset and Telescoping for Cigarettes, Alcohol, and Marijuana Across Eight Years of the National Longitudinal Survey of Youth. J Child Adolesc Subst Abuse. 2012;21:333–348. doi: 10.1080/1067828X.2012.710026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, Banich M, Graham S, Woolard J. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: evidence for a dual systems model. Dev Psychol. 2008;44:1764–1778. doi: 10.1037/a0012955. [DOI] [PubMed] [Google Scholar]
- United States. Comparing and evaluating youth substance use estimates from the National Survey on Drug Use and Health and other surveys. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2012. Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. (HHS Publication No. SMA 12-4727, Methodology Series M-9). [PubMed] [Google Scholar]
- Vsevolozhskaya OA, Anthony JC. Transitioning from First Drug Use to Dependence Onset: Illustration of a Multiparametric Approach for Comparative Epidemiology. Neuropsychopharmacology. 2016;41:869–76. doi: 10.1038/npp.2015.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner FA, Anthony JC. From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. Neuropsychopharmacology. 2002;26:479–488. doi: 10.1016/S0893-133X(01)00367-0. [DOI] [PubMed] [Google Scholar]
- Wagner FA, Anthony JC. Male-female differences in the risk of progression from first use to dependence upon cannabis, cocaine, and alcohol. Drug Alcohol Depend. 2007;86:191–198. doi: 10.1016/j.drugalcdep.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. Will increasing alcohol availability by lowering the minimum legal drinking age decrease drinking and related consequences among youths? Am J Public Health. 2010;100:986–992. doi: 10.2105/AJPH.2009.178004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A, Castle IJ, Chen CM, Shirley M, Roach D, Hingson R. Converging Patterns of Alcohol Use and Related Outcomes Among Females and Males in the United States, 2002 to 2012. Alcohol Clin Exp Res. 2015;39:1712–1726. doi: 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- Wilsnack RW, Wilsnack SC, Kristjanson AF, Vogeltanz-Holm ND, Gmel G. Gender and alcohol consumption: patterns from the multinational GENACIS project. Addiction. 2009;104:1487–1500. doi: 10.1111/j.1360-0443.2009.02696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen HU, Behrendt S, Hofler M, Perkonigg A, Lieb R, Buhringer G, Beesdo K. What are the high risk periods for incident substance use and transitions to abuse and dependence? Implications for early intervention and prevention. Int J Methods Psychiatr Res. 2008;17(Suppl 1):S16–29. doi: 10.1002/mpr.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SE, Corley RP, Stallings MC, Rhee SH, Crowley TJ, Hewitt JK. Substance use, abuse and dependence in adolescence: prevalence, symptom profiles and correlates. Drug Alcohol Depend. 2002;68:309–322. doi: 10.1016/s0376-8716(02)00225-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


