Abstract
Objective
To evaluate whether demographic and sonographic factors associated with spontaneous preterm birth (sPTB) among nulliparous women with a cervical length (CL) < 30 mm could be combined into an accurate prediction model for sPTB.
Methods
Secondary analysis of a trial of nulliparous women with a singleton gestation, a CL <30 mm on transvaginal ultrasound between 16 and 22 weeks, and who lacked other risk factors for spontaneous (e.g., prior cervical excisional procedure) or medically-indicated preterm birth (e.g., chronic hypertension), who were randomized to either 17 hydroxyprogesterone caproate or placebo. Risk factors associated with sPTB within the entire cohort were identified using univariable analysis. Factors significantly associated (P < 0.05) with sPTB were included in multivariable logistic regression analyses to determine whether an accurate prediction model could be developed.
Results
Of the 657 randomized patients, 109 (16.6%) had sPTB less than 37 weeks of gestation. Logistic regression analysis revealed only cervical length (OR 1.06 per 1 mm decrease, 95% CI 1.02–1.10) to be associated with sPTB. The area under the ROC curve based on this regression was low (AUC: 0.63, 95% CI 0.58–0.69). Results were similar for the outcome of sPTB < 34 weeks.
Conclusions
An accurate prediction model for sPTB among nulliparous women with a short cervix could not be developed.
Keywords: cervical length, prediction, spontaneous preterm birth
It is well established that the midtrimester sonographic length of the cervix is associated with the chance of preterm birth.1 By convention, the 10th percentile of cervical length for the population has been used to indicate women at “high risk” of preterm birth. At 22–24 weeks gestation, the 10th percentile is approximately 25 mm, although between 16 and 22 weeks (when women typically receive their anatomic survey and cervical length screening) the 10th percentile is 30 mm.1–3 Among nulliparous women, a short cervix is the risk factor with the highest population attributable risk for preterm birth.4
Nevertheless, even though the presence of a short cervix increases the chance of spontaneous preterm birth, many nulliparous women with this finding will still deliver at term. For example, among nulliparous women in the United States, a cervical length less than the 10th percentile in the second trimester conveys a risk of preterm birth of approximately 25%.1,3 That is, the majority of nulliparous women classified as “high risk” will actually deliver at term. These nulliparous women, whose short cervix has been a false positive finding with respect to spontaneous preterm birth, may receive medical treatments (e.g. progesterone), unproven interventions (e.g., bed rest), and experience anxiety because of their high-risk classification.6–8
Some investigators previously have attempted, without success, to elucidate other factors in addition to cervical length that could assist in prediction of preterm birth.9 However, the population examined was not limited to women with a short cervix, and relatively few women with a short cervix were included in the modeling. Thus, whether additional predictive factors can be found specifically among the population of women with a short cervix remains uncertain. Accordingly, a more accurate prediction of preterm birth risk among nulliparous women with a short cervix could be of benefit. Counseling could be improved, therapy could be better targeted, and the subjective experience of pregnancy could be enhanced. At present, however, a more accurate prediction model does not exist. The purpose of this analysis was to determine, among women with a cervix less than the 10th percentile between 16 and 22 weeks of gestation, whether additional factors could be identified that are associated with an increased risk of preterm birth and used to develop an accurate model for preterm birth prediction.
Materials and Methods
The SCAN trial was a randomized placebo-controlled trial in which nulliparous women with a transvaginal sonographic cervical length < 30 mm (i.e., < 10th percentile) between 16 and 22 3/7 weeks of gestation were randomized to receive either weekly intramuscular 17-alpha hydroxyprogesterone caproate (17OHP) or placebo.5 Study injections were initiated by 22 6/7 weeks of gestation and continued until 36 6/7 weeks of gestation or delivery, whichever came first. At enrollment, demographic and transvaginal sonographic characteristics of study participants were collected. The primary outcome of the trial was preterm delivery < 37 weeks. Full details of the study protocol, including the fact that all cervical length measurements were made by trained and centrally certified sonographers, that 10.3% of women screened had a cervical length of < 30 mm, and that those with other risk factors for spontaneous (e.g., prior cervical excisional procedure) or medically-indicated preterm birth (e.g., chronic hypertension) were excluded, have been previously reported.5
The present study is a secondary analysis of data from the SCAN trial. The associations of participants’ demographic factors and transvaginal sonographic findings with spontaneous preterm birth (defined as preterm birth due either to spontaneous labor or premature rupture of the membranes) at less than 37 weeks were estimated in univariable analysis. Factors that were associated with preterm delivery at a significance level of P < 0.05 were then entered into a multivariable binary logistic equation in order to determine which factors were independently associated with spontaneous preterm birth. Treatment group was included in this regression equation. The classification ability of the final multivariable model was assessed by the area under the receiver operating characteristic curve (AUC).
In order to ensure that prediction ability was not impaired due to the use of “spontaneous preterm birth” as a dichotomous outcome, an additional multinomial regression was performed in which the dependent terms were “spontaneous preterm birth”, “indicated preterm birth”, and “term birth”. The independent associations of demographic and sonographic factors with spontaneous preterm birth were estimated from this multinomial equation as well. All analyses were repeated for the outcome of preterm birth < 34 weeks.
Institutional review board approval for this study was obtained from all participating institutions. In univariable analysis, the Wilcoxon-rank sum test was used to compare continuous variables and the chi-square test or Fisher’s exact test was used to compare categorical variables. Multivariable analyses were performed with both binary and multinomial logistic regression, with odds ratios (OR) and 95% confidence intervals (CI) reported. Alternate definitions for a short cervix (i.e., ≤25mm and ≤20 mm) were evaluated as well. All tests were two-tailed and P < 0.05 used to define statistical significance. No adjustments were made for multiple comparisons. All analyses were performed using SAS Version 9.2 (SAS Institute, Inc, Cary, NC).
Results
Of the 657 women who were eligible for analysis, 109 (16.6%) had a spontaneous preterm birth prior to 37 weeks of gestation, 53 (8.1%) had an indicated preterm birth prior to 37 weeks of gestation, 57 (8.7%) had a spontaneous preterm birth prior to 34 weeks of gestation, and 32 (4.9%) had an indicated preterm birth prior to 34 weeks of gestation. Patient characteristics that were assessed, stratified by spontaneous preterm birth, are presented in Table 1. Few additional characteristics were associated with an increased chance of spontaneous preterm birth. Specifically, two sonographic findings – shorter mean cervical length and the presence of cervical funneling – were associated with an increased risk of preterm birth. Conversely, among this population of women with a short cervix, other characteristics such as race/ethnicity, maternal age, and pre-pregnancy BMI were not associated with spontaneous preterm birth.
Table 1.
Patient characteristics stratified by spontaneous preterm birth
| No sPTB N = 548 |
sPTB N = 109 |
P | |
|---|---|---|---|
| Maternal age (years) | 22.2 ± 4.9 | 22.3 ± 4.8 | 0.87 |
| Pre-pregnancy body mass index (kg/m2) | 25.8 ± 6.7 | 25.6 ± 6.7 | 0.64 |
| GA at short cervix detection (weeks) | 19.9 ± 1.4 | 20.0 ± 1.6 | 0.35 |
| Received 17 OHP | 49.8% | 49.5% | 0.96 |
| Race/ethnicity | |||
| Non-Hispanic white/Asian | 25.2% | 25.7% | 0.24 |
| Non-Hispanic black | 53.3% | 45.9% | |
| Hispanic | 21.5% | 28.4% | |
| Prior spontaneous pregnancy loss | |||
| < 13 weeks | 27.4% | 22.0% | 0.25 |
| 13 – 19 6/7 weeks | 1.8% | 3.7% | 0.27 |
| Any alcohol during pregnancy | 8.2% | 7.3% | 0.76 |
| Any cigarettes during pregnancy | 16.6% | 17.4% | 0.83 |
| Any street drugs during pregnancy | 6.0% | 5.5% | 0.83 |
| Cervical length (mm) | 24.2 ± 5.5 | 21.8 ± 6.2 | < 0.0001 |
| Cervical funnel present | 21.9% | 33.9% | 0.007 |
| If present, funnel length (mm) | 15.3 ± 8.0 | 16.7 ± 9.5 | 0.64 |
| Intra-amniotic debris present | 11.7% | 12.8% | 0.73 |
All data presented as mean ± standard deviation or %
sPTB = spontaneous preterm birth; GA = gestational age: 17 OHP = 17 alpha hydroxyprogesterone caproate
The results of the multivariable analysis are presented in Table 2. In the logistic regression, only cervical length remained significantly associated with spontaneous preterm birth, such that a 1 mm decrease in cervical length was associated with a 6% increased odds of spontaneous preterm birth. This multivariable regression resulted in a receiver operating characteristic curve with an area under the curve of 0.63 (95% confidence interval 0.58 – 0.69, Figure 1), which indicates that the model is poor at classifying who will experience a preterm birth. Binomial logistic regression for the prediction of spontaneous preterm birth prior to 34 weeks, as well as multinomial logistic regression (which categorized the dependent variables as “spontaneous preterm birth”, “indicated preterm birth” and “term birth”) for prediction of preterm birth prior to 37 or 34 weeks, revealed no additional factors other than cervical length to be independently associated with spontaneous preterm birth. As a result, we were unable to develop an expanded prediction model. Similarly, when 25mm (N=309) and 20 mm (N=115) were used to define a cervix as short, no additional factors were found to be associated with preterm birth (data not shown).
Table 2.
Results of binary logistic regression for outcome of spontaneous preterm birth prior to 37 weeks of gestation
| Odds ratio | 95% CI | |
|---|---|---|
| Received 17 OHP | 0.98 | 0.65 – 1.49 |
| Cervical length (1mm decrease) | 1.06 | 1.02 – 1.10 |
| Cervical funnel | 1.19 | 0.68 – 2.05 |
CI = confidence interval; 17 OHP = 17 alpha hydroxyprogesterone caproate
Figure 1.
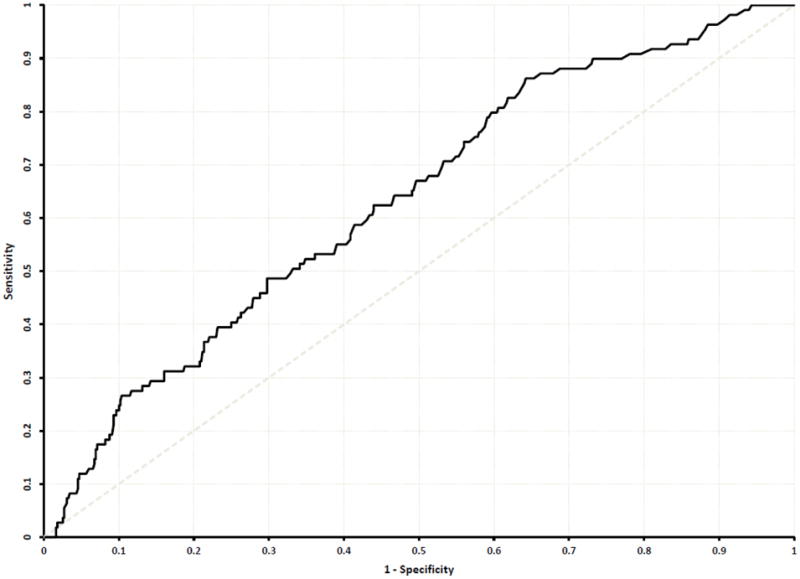
Receiver operating characteristic curve for prediction of spontaneous preterm birth
Discussion
In our study of nulliparous women with a short cervix, patient characteristics were not identified that could be used to create an accurate prediction model for spontaneous preterm birth. This finding seems in contrast to many other studies that have demonstrated multiple other risk factors for preterm birth. For example, among a general population, women who are black, who have a low body mass index, or who have amniotic fluid “sludge” have been found to have an increased risk of preterm birth.10–12 However, such risk factors may be associated with a pathophysiologic cascade that results in a short cervix. Therefore, once the study population is limited to women with a cervical length less than the 10th percentile and the cervical measurement is placed into a regression equation, the apparent association with other risk factors is no longer present or as strong. Thus, we could not derive a prediction model that incorporates factors other than cervical length and accurately predict preterm birth among women with a short cervix.
There are several strengths to this analysis. This study included a large number of women with a cervix less than the 10th percentile in the mid-trimester. Cervical length measurements were performed by sonographers who had undergone a standardized training and certification process. Moreover, the data were collected prospectively in the context of a randomized trial, further enhancing data quality.
It is possible that some factors associated with preterm birth among this population were not captured and thus could not be entered into the prediction model. However, we believe the demographic, historical, and sonographic factors most strongly associated with preterm birth were captured and it is unlikely that additional factors among these women could materially improve spontaneous preterm birth prediction. Also, this study was confined to factors that are available during routine prenatal care and sonographic examination, and did not include additional biomarkers such as serum analytes.13 Nevertheless, at present, no analyte has been demonstrated to significantly enhance prediction of preterm birth in women with a short cervix. Further investigation may elucidate whether other biomarkers are useful in significantly improving preterm birth prediction once a short cervix is identified.13 Lastly, this study was performed using data from nulliparous women and excluded women with certain conditions such as those with prior cervical excisional procedures or prolapsing amniotic membranes at the time of their sonogram. As such, the generalizability of the findings to all women cannot be known.
Although a short cervix is well known to increase the risk of spontaneous preterm birth, many women with this finding will not actually deliver preterm.1–5 Once a “short” cervix is diagnosed, therefore, women and providers are confronted with an anxiety-provoking situation that cannot be fully resolved until delivery occurs. An accurate prediction model among women with a short cervix could allow women and their obstetric providers to gauge their response to an individual’s, rather than a population’s risk. Such a prediction model also could allow better targeting of prophylactic interventions to women at greatest risk of preterm birth. However, our study does not indicate factors other than cervical length that can significantly enhance accurate classification of women with regard to preterm birth, and underscores the need to develop additional biomarkers that can aid in risk stratification.
Acknowledgments
The project described was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) [HD21410, UL1 RR024153; UL1 TR000005; HD27869, HD27915, HD27917, HD34116, HD34208, 5UL1RR025764, HD36801, HD40500, HD40512, HD40544, M01 RR00080, UL1 RR024989 (NCRR), HD40545, HD40560, HD40485, HD53097, HD53118]. Comments and views of the authors do not necessarily represent views of the NICHD.
The authors thank the following Subcommittee members who participated in protocol development and coordination between clinical research centers (Gail Mallett, R.N., B.S.N., C.C.R.C. and Cynthia Milluzzi, R.N.), protocol/data management and statistical analysis (Elizabeth Thom, Ph.D.), and protocol development and oversight (Catherine Y. Spong, M.D.).
References
- 1.Iams J, Goldenberg R, Meis P, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996;334:567–572. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 2.Hibbard JU, Tart M, Moawad AH, et al. Cervical length at 16–22 weeks’ gestation and risk for preterm delivery. Obstet Gynecol. 2000;96:972–978. doi: 10.1016/s0029-7844(00)01074-7. [DOI] [PubMed] [Google Scholar]
- 3.Taipale P, Hiilesmaa V. Sonographic measurement of uterine cervix at 18–22 weeks gestation and the risk of preterm delivery. Obstet Gynecol. 1998;92:902–907. doi: 10.1016/s0029-7844(98)00346-9. [DOI] [PubMed] [Google Scholar]
- 4.Goldenberg RL, Iams JD, Mercer BM, et al. The preterm prediction study: The value of new vs. standard risk factors in predicting early and all spontaneous preterm births. Am J Pub Health. 1998;88:233–238. doi: 10.2105/ajph.88.2.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grobman WA, Thom EA, Spong CY, et al. 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol. 2012;207:390.e1–8. doi: 10.1016/j.ajog.2012.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357:462–469. doi: 10.1056/NEJMoa067815. [DOI] [PubMed] [Google Scholar]
- 7.Grobman WA, Gilbert SA, Iams JD, et al. Activity restriction among women with a short cervix. Obstet Gynecol. 2013;121:1181–6. doi: 10.1097/AOG.0b013e3182917529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vis JY, Kuin RA, Grobman WA, Mol BWJ, Bossuyt PMM, Opmeer BC. Additional effects of the cervical length measurement in women with preterm contractions: a systematic review. Arch Gynecol Obstet. 2011;284:521–6. doi: 10.1007/s00404-011-1892-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mella MT, Mackeet AD, Gache D, Baxter JK, Berghella V. The utility of screening for historical risk factors for preterm birth in women with known second trimester cervical length. J Matern Fetal Neonatal Med. 2013;26:710–5. doi: 10.3109/14767058.2012.752809. [DOI] [PubMed] [Google Scholar]
- 10.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202:335–43. doi: 10.1016/j.ajog.2009.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Savitz DA, Stein CR, Siega-Riz AM, Herring AH. Gestational weight gain and birth outcome in relation to prepregnancy body mass index and ethnicity. Ann Epidemiol. 2010;21:78–85. doi: 10.1016/j.annepidem.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Himaya E, Rhalmi N, Girard M, et al. Midtrimester intra-amniotic sludge and the risk of spontaneous preterm birth. Am J Perinatol. 2011;28:815–20. doi: 10.1055/s-0031-1295638. [DOI] [PubMed] [Google Scholar]
- 13.Menon R, Torloni MR, Voltolini C. Biomarkers of spontaneous preterm birth: An overview of the literature in the last four decades. Reprod Sci. 2011;18:1046–70. doi: 10.1177/1933719111415548. [DOI] [PubMed] [Google Scholar]


